
Telehealth: A Viable Option for Optimizing Health System
Performance during COVID-19: Call to Action for Future Pandemics
Layal Mohtar
a
and Nabil Georges Badr
b
Higher Institute of Public Health, Saint Joseph University, Beirut, Lebanon
Keywords: Health Care, Quadruple Aim, Covid Pandemic, Scoping Review, Healthcare Services, Health System
Performance.
Abstract: Delve into the 21st century to welcome telehealth! It has taken so long coming, only to be accelerated by the
COVID -19 pandemic. With the advent of telehealth solutions, healthcare systems are on the edge of the
biggest gush in activity in over a century. In this paper, we look for evidence in the literature that treats the
disruption introduced by Telehealth diffusion and the resulting, long awaited, contribution to optimizing
health system performance. In our paper, we attempt to use the scoping review to detect evidence to answer
this question. We performed a search up to April of 2021. Data were extracted on general study characteristics,
clinical domain, technology, setting, category of outcome, and results. We then concluded with a synthesis of
the information and call to action. We then coded the findings through the lens of the quadruple aim, provided
reflections from the scoping review to inform how telehealth can be a dynamic element of system resilience.
Though faced with unintended consequences, telehealth promises to be a viable alternative to in-person care,
optimizing health system performance especially in times of constrained resources during a pandemic.
1 INTRODUCTION
As the pressing need to expand the delivery of
healthcare has surpassed the traditional limits of
implementation, the substantial burden of the
COVID-19 pandemic has placed the provision of
healthcare services under duress. Embracing
telehealth paves the way for all those vigilant in the
work of improving and transforming health care
systems, to usher in the new era of delivering
healthcare services through a reconfiguration of
technology to improve healthcare.
A US study conducted before the COVID-19
Pandemic, shows that the use of telemedicine was in
the most part, to address issues of accessibility and
reach of care to underserved areas (Barnett, 2018).
By January 2020, as COVID-19 was becoming
ostensible, the demand for telehealth services spiked
a 2000% increase in visits before the end of April
2020, and in-person visits declined 80% (Kaplan,
2020). In response to the pandemic, some research
has reported the surge in the use of telehealth services
as an option for clinic appointments, in some cases,
a
https://orcid.org/0000-0003-2771-3169
b
https://orcid.org/0000-0001-7110-3718
83% of the surveyed, cited the COVID-19 pandemic
as the impetus for implementation of such services
(Parisien et al, 2020).
Quick telehealth expansion is an astounding
example of what can happen in a matter of weeks that
was reputed to take a decade. As we explore the
outcomes associated with the implementation of
telehealth technology in healthcare ecosystems, we
are mindful of the challenge in bridging the gap
between the potential for extending healthcare
technology to overcome the disruption in the
provision of health services and the potential impact
on the quality of healthcare services and health
ecosystem performance.
This phenomenon was a worldwide event as
countries moved towards a hurried adoption of
telehealth-based practice to reduce the risk of the
pandemic spread. Health systems have added billing
codes on their schedules that differentiate
Telemedicine based care. Even prehospital telecare
became common, more in Europe than the US
(Winburn et al, 2018). The uptake of telehealth
implementations has been reported in Urgent and Non
Mohtar, L. and Badr, N.
Telehealth: A Viable Option for Optimizing Health System Performance during COVID-19: Call to Action for Future Pandemics.
DOI: 10.5220/0010647400003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 279-288
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
279

Urgent Care (Parisien et al, 2020), clinical
consultations (Smith et al, 2020), for children and
adult care (Tan, 2020) and has accelerated with the
increased restrictions. Even developing countries
reported an increase in video consultations as a
primary means of care (Helou et al, 2020). This is an
indication that Telehealth use came as an urgent,
temporary, alternative care to face – face
consultations, fuelling the reconfiguration of the care
ecosystem (Badr et al, 2021). Technology
implementers have joined the front line of the medical
provider workforce to deploy and maintain the
platforms that make these “at a distance” services
possible. A new level of interaction between the care
team and a new set of sociotechnical complexity
arise.
Have some implementations of telehealth
solutions disrupted the quality of care or were they a
long awaited contribution to optimizing health system
performance? In our paper, we attempt to use the
scoping review to detect evidence to answer this
question.
2 BACKGROUND
2.1 Telehealth: Care at a Distance
Efficiency of healthcare service, effectiveness in
resource usage, and patients’ satisfaction occupy
central attention in the discourse around care at
distance. These sustainability principles are essential
to the optimization of the services that would
otherwise be traditionally with one building and
controlled setting. With telehealth technologies, it has
become possible to extend these principles to distance
care solution such as care at home for instance (Polese
et al., 2018). Hence, telehealth is the delivery of
healthcare services by healthcare professionals using
information and communication technologies, for the
exchange of valid information for diagnosis,
treatment, and injuries and prevention of disease,
evaluation and research, and the healthcare providers’
continuing education (Fisk et al., 2020).
The modes of delivery of telehealth incorporate
technologies such as videoconferencing, mobile
applications, and secure messaging. Furthermore,
telehealth services include provider-to-provider
services with patient presence, provider to provider
without patient presence, tele monitoring, and health
education etc. (Tuckson et al., 2017). In our paper, we
1
http://www.ihi.org/Topics/TripleAim/Pages/Overview.
aspx
refer to telehealth as the overarching term to signify
the service of providing care, which the central notion
of our work.
2.2 Optimizing Health System
Performance
The pandemic has accentuated the focus on distant
care, pushing the limits on telehealth deployments for
safety concerns and for the optimization of the
resources in the healthcare systems. The facilitation
of telemedicine services has made care possible and
accessible. Though in some cases disruptive to the
existing traditional processes and care delivery
models, this new way of mainstream care may
continue to contribute to optimizing the provision of
care. Indeed, practitioners and academics have
advocated leveraging health information technology
to achieve the “triple aim” of healthcare reform
(Bisognano and Kenney, 2012; Sheikh, 2015).
Improving care quality while containing costs of
care are the central arguments for the Triple Aim
framework developed by the Institute for Healthcare
Improvement (IHI)
1
for optimizing health system
performance. The framework directs health systems
to pursue three dimensions, simultaneously for
Improving the patient experience of care (including
quality and satisfaction); Improving the health of
populations; and Reducing the per capita cost of
health care. Extending this recommendation, the
Quadruple Aim adds the dimension of improving the
work life of health care providers, including
clinicians and staff (Bodenheimer and Sinsky, 2014).
In our scoping review, we choose the Quadruple
Aim Framework as a lens to evaluate our findings and
synthesize on lessons we can glean from the current
literature.
3 METHODOLOGY
We conducted a scoping review to evaluate the
potential for improvement in the healthcare
ecosystem performance driven by the implementation
of telehealth. A scoping review, in this case, can be
useful to synthesize the relevant evidence in the
literature and identify opportunities for further
research or calls to action (Munn et al, 2018). Our
search involved online databases including Google
Scholar and PubMed, exploring articles from the
Journal of Telemedicine and Telecare, Journal of
HEALTHINF 2022 - 15th International Conference on Health Informatics
280

American College of Surgeons, International Journal
of Medical Informatics, New England Journal of
Medicine, JAMA Dermatology, NEJM Catalyst
Innovations in Care Delivery, JMIR Public Health
Surveillance, International Journal of Environmental
Research and Public Health, and JAMA Intern Med.
The initial search was performed using the search
filter of "Telehealth" AND "Impact on Quality of
Care” in which 209 queries were retrieved.
Then, in a second step, we refocused our lens on
the combined terms "Telehealth" AND "Quadruple
Aim" AND "impact on quality of care" to isolate the
content that would address our research question. We
found limited material (6 papers) on the narrow
subject. In scanning the literature, the terms telehealth
and telemedicine were found to be often used
interchangeably which echoed a primary concern
making the evidence more problematic to evaluate.
Upon review, we found that most telehealth literature
refers to telehealth as the broader practice of the
concept of delivering healthcare services at a distance
and refers to examples from the field of practice for
telemedicine as the term that describes the actual
practice of medicine at a distance. Therefore, we
expanded our narrow search on the combined terms
"Telemedicine" AND "Quadruple Aim" AND
"impact on quality of care" (six papers were also
found).
Thus, our results offered little evidence in the
literature to support the conversation on the potential
of telemedicine for healthcare improvement guided
by principles of the quadruple aim. We found sparse
evidence on how Telehealth and Telemedicine use
would influence the ability of a healthcare ecosystem
to fulfil the quadruple aim. We therefore proceeded
with the initial 209 articles in an attempt to be most
encompassing to yield the subset of articles for our
coding, hoping to develop hidden information in the
direction of our research question. After the
screening, the relevant articles were identified, only
those that were written in the English language were
chosen. Duplicate publications in different journals
were removed and student dissertation excluded.
Articles were read in full to confirm eligibility. The
review was narrowed to 50 articles. After carefully
inspecting the identified articles, we further refined
our synthesis to extract evidence of improvement in
the healthcare system performance. Each author
reviewed findings individually, and then coded using
themes from the four principles of the quadruple aim:
(1) Improving the patient experience of care,
(2) Improving the work life of healthcare
providers,
(3) Reducing the per capita cost of health care;
And
(4) Improving the health of populations.
The coding revealed secondary codes that we
categorized under the main codes, adding depth to our
findings.
4 FINDINGS AND DISCUSSION
Despite the existence of some literature on Telehealth
and Telemedicine to impact on quality of care, few
papers trace the connection between these same
technologies and the context of Quadruple AIM.
The dialogue in the context of telemedicine and
the impact on quality in the context of the goals of the
quadruple aim has been limited to very few
inferences. One paper addressed how telemedicine
and smartphones are enabling more flexible and
mobile work (Nakagawa and Yellowlees, 2019) with
emphasis on continuity of care at home (Helmer-
Smith, et al, 2020). In other examples, healthcare
technology in general has shown evidence of impact
on healthcare quality (Buntin, 2011; Fiani, 2020).
Innovative health technologies such as telehealth can
possibly help improve training, patient centeredness,
access, agreeableness, decency, efficiency, quality,
outcomes, and cost viability (Fund, 2017; Lopo,
2020). Therefore, we found sparse evidence on how
Telehealth and Telemedicine use would influence the
ability of a healthcare ecosystem to fulfill the
quadruple aim; this paper puts the focus on this
context, as our scoping review isolated the concepts
of the quadruple Aim in the context of Telehealth
adoption (Figure 1).
We have identified some works that demonstrate
telehealth as a technology to improve the patient
experience through timeliness of care (Caffery et al,
2016; Gattu et al, 2016; Lum et al, 2020); and better
access (Qureshi et al, 2015; Lurie and Carr, 2018;
Lavin et al, 2020); leading to an improved quality of
life for care seekers (Waibel et al, 2017). Other works
connected a decreased hospitalization and resource
utilization to the implementation of telehealth
solutions (Gattu et al, 2016), lessening the workload
on the care staff (Bashir and Bastola, 2018), thus
improving the work life of health care providers
(Lopo et al, 2020). Our investigation revealed that
Telehealth has the potential of reducing cost of care
(Mehrotra et al, 2013; Liu et al, 2016) and improving
the outcome of care (Flodgren et al, 2015; Snoswell
et al, 2017).
Telehealth: A Viable Option for Optimizing Health System Performance during COVID-19: Call to Action for Future Pandemics
281
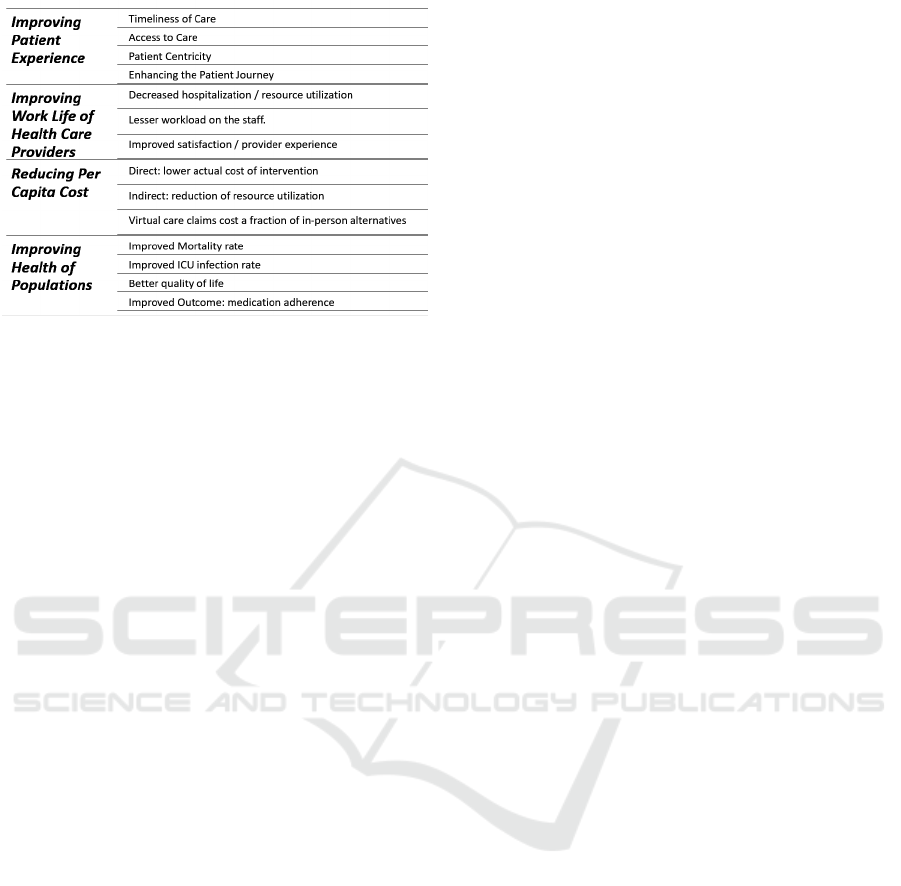
Figure 1: Telehealth & Optimizing Health System
Performance – from our Scoping Review.
4.1 Improving Patient Experience of
Care
Timeliness of Care: Evidence suggests that the
adoption of telehealth has improved timely access to
care, especially for low acuity conditions or serious,
time-sensitive situations; hospitals are adopting
telehealth to improve operational efficiencies and
provide timelier access to specialty care (Lum et al,
2020).
Our review has identified a case, with a
significant (75%) reduction in patient wait times for
urgent care conditions, through a telehealth triage
program (Caffery et al, 2016). In another case, while
chronic pain clinic patients waited for an in person
consultation, they have received useful advice in 86%
of cases, through their telehealth portals, reducing the
negative impact of the long wait times on their day to
day lives. Using virtual visits for low-acuity patients,
reduced the emergency departments wait from 2.5
hours to 40 minutes (Caffery et al, 2016) and timely
diagnosis of minor illnesses in children and
adolescents has improved school attendance (Gattu et
al, 2016).
Access to Care: Our scoping review has
identified instances of improved access to care with
telehealth services, while also recognizing access
barriers of technology reach in some rural populations
of Central Asia (Qureshi et al, 2015) and Africa
(Lurie and Carr, 2018). By placing the technologies
directly in patients' homes or at local clinics near them
(Lavin et al, 2020), patients have reported an
improved quality of life, ameliorating their
experience and almost half strongly disagreed
whether they still must see the provider in person and
most (86%) of them strongly agreed on the use of
telehealth again (Waibel et al, 2017).
Patient Centricity: Consumers are willing to use
telehealth for everything from prescription renewals
to chronic disease management and behavioural
health (Lum et al, 2020). Patients seeking virtual care
rated their satisfaction as “very good” to “excellent”
(Thomas et al, 2020). To note, patients feel in charge
if their records and the levels of care they receive as
their contribution and input through online available
systems, with complete histories, and physical
examinations, contribute to the outcome of correct
diagnoses in 76.5% of the visits (Schoenfeld et al,
2016). Still, one study identified that lab tests may
have been unnecessarily ordered due to a
conservative approach of ordering antibiotics
(Mehrotra et al, 2013).
Enhancing the Patient Journey: Telehealth
implementations have brought the information to the
patients, whereby a decrease in emergency
department’s visits (Wosik et al, 2020), especially in
pediatric visits (DeJong et al, 2014). Patients are
finding their answers with Telemedicine tools and
more digital means of interaction with the care
providers. Case studies have reported a two-fold
improvement in the completeness of documentation
and increase in appropriate antibiotic prescribing
within six months due to the use of telehealth services
(DeJong et al, 2014). This implies a lesser workload
on the care staff and reduction of fatigue. Other cases
have noted a reduction in hospitalizations, length of
stay, and 30-day readmission rate (DeJong et al,
2014), especially among the home based telehealth
patient population (Lum et al, 2020). Video visits
combined with remote patient monitoring enable
healthcare organizations to better monitor patients,
relieve workload and reduce consumption of care
resources.
4.2 Improving Work Life of Health
Care Providers
Decreased Hospitalization / Resource Utilization:
Hospitals are adopting telehealth to improve
operational efficiencies and provide timelier access to
specialty care (Lum et al, 2020). For example, timely
diagnosis, with the use of telehealth for minor
illnesses in children and adolescents decreased
emergency department utilization by 22% (Gattu et
al, 2016). This reduction reflects on lesser workload
on the staff.
Improved Satisfaction / Provider Experience:
Telehealth has improved the quality of the nursing
practice and reflected on the quality of the care
services (Bashir and Bastola, 2018). With the
implementation of telehealth in the model of care,
HEALTHINF 2022 - 15th International Conference on Health Informatics
282

satisfaction levels at the provider experience have
improved (Caffery et al, 2016). Studies in our scoping
review reflected on healthcare practitioner’s morale
affecting workforce engagement and safety such as
workforce burn-out (Sikka et al, 2015). The literature
review has noted provider experience satisfaction in
94% of cases of telehealth implementations (Lopo et
al, 2020).
4.3 Reducing per Capita Cost of Health
Care
Our investigation revealed that Telehealth has the
potential of reducing cost of care. Telehealth
programs can be cost saving for intermediate and
high-risk patients over a 1- to 5-year window (Liu et
al, 2016). The cost reduction can be direct through
actual cost of intervention or consultation and also
indirect through reduction in the consumption of
hospital services (Mehrotra et al, 2013). Service cost
a weighted average of $47.35/case, compared with
$133.60/case for traditional refer (Caffery et al,
2016). In one case, the service cost has decreased to
third for traditional referrals (Caffery et al, 2016) and
virtual care claims have saved the health plan an
average of 30% per claim (Lum et al, 2020).
4.4 Improving Health of Populations
Telehealth consultations contribute to the adherence
to clinical management guideline (Steinman et al,
2015), and the satisfaction of both patients and
providers (Waibel et al, 2019) and showed no
significant difference in adherence to treatment
guidelines across the multiple care modalities
(primary care, urgent care, etc.) of which
telemedicine has become one. There has been some
pleasing news on the decrease in mortality rates in
ICUs (DeJong et al, 2014) and especially concerning
the reduction of risks (30%) of sepsis (Steinman et al,
2015). Telemedicine intervention decreased overall
mortality and length of stay within progressive care
units without substantial cost incurrences (Armaignac
et al, 2018). Additionally, we found evidence of
improved quality of life where participants with
diabetes had a lower glycated hemoglobin (HbA1c
%) levels, a decrease in LDL, and blood pressure
(Flodgren et al, 2015). DeJong et al 2014 elaborated
that uniform transparency about care and referral
protocols would be helpful. Creating a consumer-
dominated regulator, which could compile
information on e-visit websites’ performance, may
improve outcomes. Telehealth tools can aid in
improving medication adherence, thus contributing to
improved patient outcomes, decreased likelihood for
hospital admissions, reduced healthcare cost burden,
and improved mortality in heart failure patients, a
study finds (Broadway, 2021). An interesting article
in our review, noted that by understanding societal
values such as patient preference and willingness-to-
pay, we might be able to quantify the value of new
interventions and extra-clinical outcomes associated
with telehealth more effectively (Snoswell et al,
2017).
5 REFLECTION FROM THE
SCOPING REVIEW
Telehealth implementations are starting to prove
some contributions for optimizing health system
performance, as evidenced by our scoping review.
The literature provides a favourable view on the
potential for Telehealth to improve the patient
experience of care through increasing access to timely
care, focusing more on the needs of care for each
patient. With Telehealth there is a great opportunity
to decrease hospitalization and optimize health
resource utilization. This will also drive an
improvement in the quality of life of the practitioners,
lower the cost of care, improve medication adherence,
etc. leading to improved health of the population. As
a viable alternative to in-person care, Telehealth is
now a dynamic element of care system resilience. The
scoping review has inspired a few calls to action to
reign in and understand the risks incurred while
providing care virtually and how an interruption in
the virtual service may affect the outcome. The
complex care ecosystem with all its actors and
stakeholders must be prepared and the access to latent
information must be ushered to curb likely misuse.
The literature does not reflect on how privacy was
ensured in such visits and what happened when a
breach in privacy and confidentiality took place and
how this affected the satisfaction (Badr et al, 2021,
January). The COVID-19 pandemic coupled with the
rapid explosion of telehealth services grants an
unparalleled opportunity to examine related ethical,
legal, privacy and confidentiality, information
technology infrastructure and social challenges
during a time of crisis in healthcare. Just like the
current and potential benefits, conversely telehealth
has limitations which are essential to address into the
mainstream of telehealth deployment.
Telehealth: A Viable Option for Optimizing Health System Performance during COVID-19: Call to Action for Future Pandemics
283

5.1 Unintended Consequences of
Benefits
Innumerable technologies can be applied through
telehealth to empower patients to have control over
their healthcare, but despite current research, rigorous
investigation needs to be completed to determine all
the possibilities where technology could be beneficial
and useful (fit for use), and also under which
circumstances (fit for purpose). A full understanding
is needed in order to curb the risk of some unintended
consequences.
Fit for Use: Although, one of the benefits of
telehealth implementation is reducing the cost
through providing access to rural areas, reducing
emergency department utilization, and avoiding
hospitalizations; implementing telehealth may not be
cost-effective in the short term due to high
infrastructure and operational cost and capability
building required for the mainstream of practitioners
to use the new technologies. Our review highlighted
the importance of removing financial barriers to use
telemedicine, implementing waivers to purchase
essential devices and internet access, and offering
education and training, could be options in that
direction.
Fit for Purpose: For instance, attention must be
given to avoid risks of unintended consequences.
Examples of such risks are identified in cases of
patient interaction and practitioner satisfaction in
administering care. Studies have persistently shown
that telehealth implementation can improve patient
outcomes due to a timely patient-provider interaction.
Telehealth can encourage more personal encounters
and assist healthcare providers by increasing their
ability to develop improved relationships with
patients, which may lead to better patient compliance
and thus enhance patient outcomes. However, in the
absence of tactile examination, physicians may
perceive the absence of the physical contact with the
patient as inadequate evaluation, incomplete
diagnosis or inappropriate treatment. Thus, a dual
need for evidence-based provision of care along with
easy contextual upskill may be strategically
addressed through a complementary approach
between physical and virtual care. Results of another
study showed that 42.9% of doctors believed that
telemedicine disrupts the doctor-patient relationship
and causes a breach of patient privacy. Cyber related
malpractice insurance would be required for
telehealth practitioners to protect patients from fake
providers and breaches in data security and privacy
(Gogia et al, 2016).
Risks of Technology Fatigue among
Practitioners: Studies in our scoping review
reflected on healthcare practitioner’s morale affecting
workforce engagement and safety such as workforce
burn-out. Telehealth has improved the quality of the
nursing practice which reflected on the quality of the
care services. In addition to reducing the burden of
scheduling, physical and mental exhaustion of the
care providers, telehealth helps lessen transportation
costs for the latter, relieve time lost at work, improves
access to specialists, and promotes continuity in care.
This is a significant improvement to the work life of
health care providers, leading to a better system
performance overall. Opposing views may see that
when people spend a lot of time virtually, may expose
health care professionals to “zoom fatigue” which
may eventually reflect on their ability to provide care
– A moderation is required with the use of virtual
platforms of communication.
5.2 Telehealth a Dynamic Element of
System Resilience
Resilience is commonly portrayed as a positive
capability that allows actors in a system to thrive in
dynamic contexts, adapting, reconfiguring and
developing sustainability (Pisano, 2012). A resilient
healthcare system exhibits an ability to overcome the
disruption in healthcare services the latest
experiences provide evidence that telehealth is no
more the cherry on top but has become an essential
component of care delivery. Telehealth aids the
healthcare system in achieving healthcare equity by
closing care gaps that have been created by current
care models and hence ensuring continuity of care.
After decades of measured implementation of
telemedicine and telehealth (Flores et al, 2020), the
COVID-19 pandemic has dramatically changed not
only the frequency of patient-clinician visits
conducted via technology across a distance, but also
the urgency to practice at a distance, in order to
prevent the spread (Turer et al, 2020). Telehealth
became a component of the personal protective
equipment gear, designated as Electronic PPE
(ePPE), in the medical practice (Wosik et al, 2020),
giving this new interaction experience a mainstream
(Vilendrer et al, 2020; Li et al, 2020). Thus, bridging
the digital divide for a tranche of the population, and
creating new challenges for others vulnerable sectors
of society (Ramsetty and Adams, 2020). Clinicians
now could practice from the hospital and from home.
While practitioners used teleconferencing equipment
and connected remote devices to collect their patients
vitals and provide a remote assessment (Badr et al,
HEALTHINF 2022 - 15th International Conference on Health Informatics
284

2021), patients were able to access their information
through their mobile app, interfaced with the health
record. (Munn et al, 2020). Although extending
healthcare engagement into the patient home was
pursued out of necessity, it is evolving around easier
access to care and timely patient-provider interaction.
While Telehealth can facilitate swift and
successful reconfiguration of care, it also creates
tensions among the complex health system that
require careful consideration (Cho and Robey, 2007).
A call to action is indispensable now, as we embark
on this untethered diffusion of telehealth innovations.
Firstly, when evaluating the literature, we found
lack of evidence in studies that shown the impact of
technology interruption on the care provided. The
literature did not depict whether any adverse events
took place while providing care virtually and how an
interruption in the virtual service affected the
outcome. Providers may potentially become more
frustrated and stressed out of dealing with patients
who delay treatment.
Secondly, when scoping to the future, healthcare
organizations shall assess the organization readiness,
put the policies in places, provide education and
continuous support, check financial reimbursements,
consider IT breakdowns, consider laws of physician
provision of services within the boundaries, and most
importantly, consider privacy and confidentiality. All
these factors shall be sought when determining the
future of telehealth.
Thirdly, access to telemedicine software shall be
escorted with simple guidelines on its proper use and
what to do in case an interruption happens. A
continuous evaluation and monitoring model shall be
put in place to unceasingly assess the system.
Finally, decision-makers still lack adequate
information on comparing the effects of telemedicine
applications to alternative health care strategies. They
also lack good evaluation of the infrastructure
implications and financial requirements for
sustaining telemedicine post COVID. Telemedicine
shall be included as a part of regional disaster health
care systems and provide some of the needed
protections for patients and providers. Disaster
planners and telehealth clinicians shall leverage
technology to improve health care delivery and
prevent the disruption of services during such times
(Gogia et al, 2016).
5.3 Telehealth – Viable Alternative to
In-person Care
The former year has brought the vital nature of virtual
care to the vanguard. Mitigating the spread of the
COVID -19 pandemic has linked isolated patients,
provided care for non-COVID-19 patients, and led to
the accelerated diffusion of telehealth services.
During the COVID-19 pandemic, we have seen the
perceptual cycle of ineffective/absent public
healthcare processes compounded by lack of access
to healthcare services. The provision of health care
services through telehealth technologies has revealed
a reassuring effect in the lives of patients.
The public is increasingly in need to access
personalized advice with ease, which will lead to
better quality of healthcare services and, particularly,
improving the overall patient experience. In this era
of Netflix, Uber, Amazon, Zoom, mobile banking,
and a technology facility that enables a 3-year-old to
log in to online classes, unaided, it will not be proper
for the healthcare sector to tumble behind. An average
consumer finishes nearly all aspects of their life
online; healthcare shall be just as convenient,
reachable, and innocuous as online banking.
Leveraging telehealth may produce a higher level
of access and new ways for patients and providers to
participate in the care system resulting in increased
satisfaction for both patients and providers.
Telemedicine while evolving and changing the
current landscape of healthcare, can in a way take us
back to a time when home visits were a part of normal
practice; however, it is now virtually (Shockley,
2020). Immunocompromised, homebound or patients
who live in remote areas, for example, could receive
uninterrupted access to healthcare services.
Furthermore, other patients who want to save time
and cost by reducing travel may continue to seek
virtual care if it is available.
Progressively, for telehealth to become a more
viable alternative to in-person care, research
recommends that healthcare leaders must be less
reactive and more adaptive in the development and
implementation of telehealth solutions (Shockley,
2020) in order to face the challenges in this complex
healthcare ecosystem,. Henceforth, the authors offer
a few recommendation, as calls to action, motivated
by of the findings of this review
Firstly, as we look forward, virtual care will
persist to build the needed foundation to provide safe
and effective care with the right clinician, at the right
time, and at the convenience of the patient. Remote
patient care should be provisioned virtually to
improve effectiveness and enhance patient outcomes.
It offers instantaneous communication with the
healthcare provider at the convenience of the patient
(according to his or her time schedule, saving travel
time for those in rural areas). With the rapid
expansion of telemedicine in the light of the COVID-
Telehealth: A Viable Option for Optimizing Health System Performance during COVID-19: Call to Action for Future Pandemics
285
19 pandemic, ensuring that remote care reaches
diverse, low-income patients and promotes health
equity rather than exacerbating health disparities is
critical. One important aspect to take into deliberation
is that telemedicine may not be accessible to specific
individuals with disabilities and older adults, and
hence affects the treatment delivery via telehealth
technology; the odds of leveraging telemedicine will
be those aged 64 or younger. As mental health
problems are more prevalent in older adults, tele-
mental health services are urgently needed, especially
during the pandemic, for this age category.
Secondly, a deployment of a digital health
strategy that includes telehealth can be effective to
decrease service costs, improve satisfaction, and
improve the entire experience as the hospital rooms
will be extended outside of the physical facility and
into patients’ homes. Such strategy will move us in
the direction of optimizing health system
performance. Nevertheless, in the implementation of
telehealth, we shall acknowledge the perilous role of
the workforce in the healthcare revolution (Fiks et al.,
2021). To ensure that the service that is delivered to
the patient is a service of superior quality, some
aspects of the patient journey are still to be evaluated.
Improvement programs in telehealth technology must
seek the participation of practitioners as important
ambassadors for programmatic success (Smith et al,
2020).
Thirdly, for the near future, Telehealth ought to be
first, an extension, not a replacement of traditional
care services where we shall monitor for those
potentially negative effects and mitigate them. A
quality improvement system is needed to ensure that
services are being provided within best practice
guidelines, demanding quality of the care monitoring
across all levels regardless of location; by monitoring
compliance to standardized treatment protocols, data
collection procedures, and professional behaviour.
5.4 Summary and Calls to Action
Telehealth endures to advance in both developed and
developing countries within the all-embracing setting
of information technology. The former year has
brought the vital nature of virtual care to the
vanguard. Mitigating the spread of the COVID -19
pandemic has linked isolated patients, provided care
for non-COVID-19 patients, and led to the
accelerated diffusion of telehealth services. During
the COVID-19 pandemic, we have seen the
perceptual cycle of ineffective/absent public
healthcare processes compounded by lack of access
to healthcare services. The provision of health care
services through telehealth technologies has revealed
a reassuring effect in the lives of patients, especially
during constraints imposed by the pandemic
response.
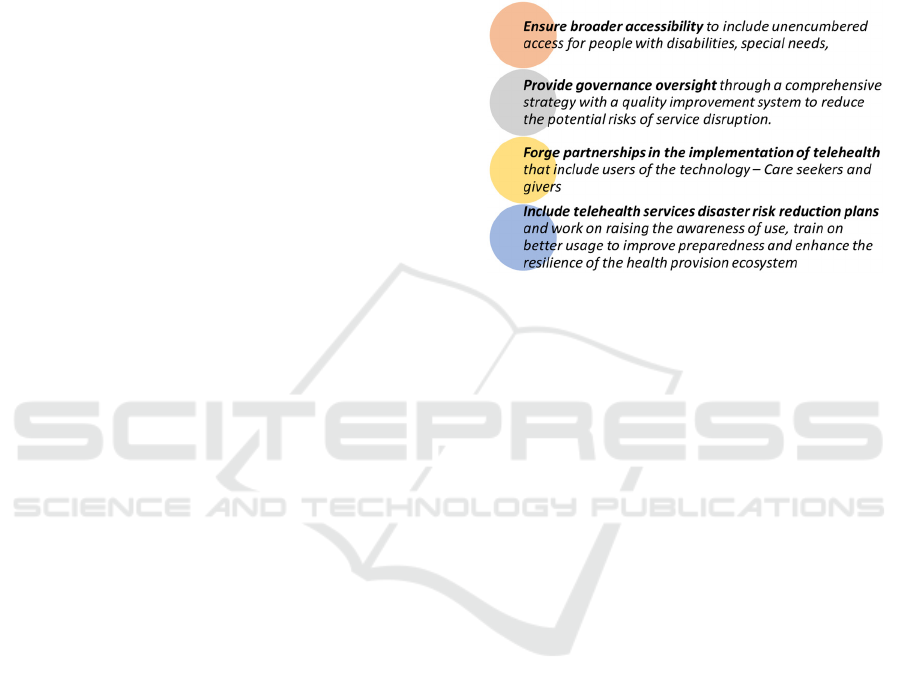
Our review is valuable in producing calls to action
to improve the performance of the healthcare
ecosystem through Telehealth, in response to
pandemics (Figure 2).
Figure 2: Calls to action to improve the performance of the
healthcare ecosystem through Telehealth during
pandemics.
Hence, designers and implementers of the
telehealth solutions must ensure broader accessibility
to include unencumbered access for people with
disabilities, special needs, and provide governance
and oversight through a comprehensive deployment
strategy with a quality improvement system to reduce
the potential risks of service disruption.
Moreover, technology developers must forge
partnership in the implementation of telehealth that
include users of the technology experience (care
seekers and givers) for value co-creation to
complement the existing complex care ecosystem.
Finally, we call on disaster planners to include
telehealth services disaster risk reduction plans and
work on raising the awareness of use, train on better
usage to improve preparedness and enhance the
resilience of the health provision ecosystem.
6 CONCLUSION
The scoping review provides a few lessons from the
literature. Telehealth has crossed the stage of
disillusionment in the technology hype cycle (Fenn
and Raskino, 2008). The technology’s potential for
mainstream application has become more broadly
understood. Telehealth, a mode of providing care at a
distance has entered the mainstream largely gated by
the latest pandemic needs. We have learned how
HEALTHINF 2022 - 15th International Conference on Health Informatics
286

Telehealth become a significant mediator for the
resilience of the care system during the COVID-19
Pandemic.
REFERENCES
Alami, H., Lehoux, P., Gagnon, M. P., Fortin, J. P., Fleet,
R., & Ahmed, M. A. A. (2020). Rethinking the
electronic health record through the quadruple aim:
time to align its value with the health system. BMC
medical informatics and decision making, 20(1), 1-5.
Armaignac, D. L., Saxena, A., Rubens, M., Valle, C. A.,
Williams, L. S., Veledar, E., & Gidel, L. T. (2018).
Impact of Telemedicine on Mortality, Length of Stay,
and Cost Among Patients in Progressive Care Units:
Experience From a Large Healthcare System. Critical
care medicine, 46(5), 728–735.
Badr, N. G., Carrubbo, L., & Ruberto, M. (2021).
Responding to COVID-19: Potential Hospital-at-Home
Solutions to Re-configure the Healthcare Service
Ecosystem.
Badr, N., Drăgoicea, M., Walletzký, L., Carrubbo, L., &
Toli, A. M. (2021, January). Modelling for Ethical
Concerns for Traceability in Time of Pandemic “Do no
Harm” or “Better Safe than Sorry!” In Proceedings of
the 54th Hawaii International Conference on System
Sciences (p. 1779).
Barnett, M. L., Lau, A. S., & Miranda, J. (2018). Lay health
worker involvement in evidence-based treatment
delivery: a conceptual model to address disparities in
care. Annual review of clinical psychology, 14, 185-
208.
Bashir, A., & Bastola, D. R. (2018). Perspectives of nurses
toward telehealth efficacy and quality of health care:
pilot study. JMIR medical informatics, 6(2), e35.
Bisognano, M., & Kenney, C. (2012). Pursuing the triple
aim: seven innovators show the way to better care,
better health, and lower costs. John Wiley & Sons.
Bodenheimer, T., & Sinsky, C. (2014). From triple to
quadruple aim: care of the patient requires care of the
provider. The Annals of Family Medicine, 12(6), 573-
576.
Broadway, D. M. (2021). Implementation of Telephone-
based Medication Adherence Conferences to Improve
Health Outcomes of Heart Failure Patients.
Buntin, M. B., Burke, M. F., Hoaglin, M. C., & Blumenthal,
D. (2011). The benefits of health information
technology: a review of the recent literature shows
predominantly positive results. Health affairs, 30(3),
464-471.
Caffery, L. J., Farjian, M., & Smith, A. C. (2016).
Telehealth interventions for reducing waiting lists and
waiting times for specialist outpatient services: A
scoping review. Journal of telemedicine and telecare,
22(8), 504-512.
Cho, S., Mathiassen, L., & Robey, D. (2007). Dialectics of
resilience: a multi–level analysis of a telehealth
innovation. J. Inf. Technol, 22(1), 24-35.
Chuo, J., Macy, M. L., & Lorch, S. A. (2020). Strategies for
Evaluating Telehealth. Pediatrics, 146(5).
DeJong, C., Santa, J., & Dudley, R. A. (2014). Websites
that offer care over the Internet: is there an access
quality tradeoff?. JAMA, 311(13), 1287-1288.
Fenn, J., & Raskino, M. (2008). Mastering the hype cycle:
how to choose the right innovation at the right time.
Harvard Business Press.
Fiani, B., Quadri, S. A., Farooqui, M., Cathel, A., Berman,
B., Noel, J., & Siddiqi, J. (2020). Impact of robot-
assisted spine surgery on health care quality and
neurosurgical economics: a systemic review.
Neurosurgical review, 43(1), 17-25.
Fiks, A. G., Jenssen, B. P., & Ray, K. N. (2021). A defining
moment for pediatric primary care telehealth. JAMA
pediatrics, 175(1), 9-10.
Fisk, M., Livingstone, A., & Pit, S. W. (2020). Telehealth
in the context of COVID-19: changing perspectives in
Australia, the United Kingdom, and the United States.
Journal of medical Internet research, 22(6), e19264.
Flodgren, G., Rachas, A., Farmer, A. J., Inzitari, M., &
Shepperd, S. (2015). Interactive telemedicine: effects
on professional practice and health care outcomes.
Cochrane Database of Systematic Reviews, (9).
Flores, A. P. D. C., Lazaro, S. A., Molina-Bastos, C. G.,
Guattini, V. L. D. O., Ump-ierre, R. N., Gonçalves, M.
R., & Carrard, V. C. (2020) Teledentistry in the
diagnosis of oral lesions: A systematic review of the
literature. JAMIA, 27(7), 1166-1172.
Fund, M. M. (2017). The Impact of Primary Care Practice
Transformation on Cost, Quality, and Utilization.
Gattu, R., Teshome, G., & Lichenstein, R. (2016).
Telemedicine applications for the pediatric emergency
medicine: a review of the current literature. Pediatric
emergency care, 32(2), 123-130.
Gogia, S. B., Maeder, A., Mars, M., Hartvigsen, G., Basu,
A., & Abbott, P. (2016). Unintended consequences of
tele health and their possible solutions: contribution of
the IMIA working group on telehealth. Yearbook of
medical informatics, (1), 41.
Helmer-Smith, M., Fung, C., Afkham, A., Crowe, L.,
Gazarin, M., Keely, E., & Liddy, C. (2020). The
feasibility of using electronic consultation in long-term
care homes. Journal of the American Medical Directors
Association, 21(8), 1166-1170.
Helou, S., El Helou, E., Abou-Khalil, V., Wakim, J., El
Helou, J., Daher, A., & El Hachem, C. (2020). The
effect of the COVID-19 pandemic on physicians’ use
and perception of telehealth: The case of Lebanon.
International journal of environmental research and
public health, 17(13), 4866.
Kaplan, B. (2020). Revisting Health Information
Technology Ethical, Legal, and Social Issues and
Evaluation: Telehealth/Telemedicine and COVID-19.
International journal of medical informatics, 104239.
Lavin, B., Dormond, C., Scantlebury, M. H., Frouin, P. Y.,
& Brodie, M. J. (2020). Bridging the healthcare gap:
Building the case for epilepsy virtual clinics in the
current healthcare environment. Epilepsy & Behavior,
111, 107262.
Telehealth: A Viable Option for Optimizing Health System Performance during COVID-19: Call to Action for Future Pandemics
287

Li, G., Fan, G., Chen, Y., & Deng, Z. (2020) What patients
“see” doctors in online fever clinics during COVID-19
in Wuhan?. JAMIA, 27(7), 1067-1071.
Liu, S. X., Xiang, R., Lagor, C., Liu, N., & Sullivan, K.
(2016). Economic modeling of heart failure telehealth
programs: when do they become cost saving?.
International journal of telemedicine and applications,
2016.
Lopo, C., Razak, A., Maidin, A., Rivai, F., Mallongi, A., &
Sesa, E. (2020). Technology impact on healthcare
quality of the hospital: A literature review. Enfermería
Clínica, 30, 81-86.
Lum, H. D., Nearing, K., Pimentel, C. B., Levy, C. R., &
Hung, W. W. (2020). Anywhere to anywhere: use of
telehealth to increase health care access for older, rural
veterans. Public Policy & Aging Report, 30(1), 12-18.
Lurie, N., & Carr, B. G. (2018). The role of telehealth in the
medical response to disasters. JAMA internal medicine,
178(6), 745-746.
Mehrotra, A., Paone, S., Martich, G. D., Albert, S. M., &
Shevchik, G. J. (2013). A comparison of care at e-visits
and physician office visits for sinusitis and urinary tract
infection. JAMA internal medicine, 173(1), 72-74.
Munn, Z., Peters, M. D., Stern, C., Tufanaru, C., McArthur,
A., & Aromataris, E. (2018). Systematic review or
scoping review? Guidance for authors when choosing
between a systematic or scoping review approach. BMC
medical research methodology, 18(1), 1-7.
Nakagawa, K., & Yellowlees, P. M. (2019). The
physician’s physician: the role of the psychiatrist in
helping other physicians and promoting wellness.
Psychiatric Clinics, 42(3), 473-482.
Parisien, R. L., Shin, M., Constant, M., Saltzman, B. M., Li,
X., Levine, W. N., & Trofa, D. P. (2020). Telehealth
utilization in response to the novel coronavirus
(COVID-19) pandemic in orthopaedic surgery. JAAOS
Pisano, U. (2012). Resilience and Sustainable
Development: Theory of resilience, systems thinking.
European Sustainable Development Network (ESDN),
26, 50.
Polese, F., Carrubbo, L., Caputo, F., & Sarno, D. (2018).
Managing healthcare service ecosystems: Abstracting a
sustainability-based view from hospitalization at home
(HaH) practices. Sustainability, 10(11), 3951.
Qureshi, I. A., Raza, H., Whitty, M., & Abdin, S. Z. U.
(2015). Telemedicine implementation and benefits for
quality and patient safety in Pakistan. Knowledge
Management & E-Learning: An International Journal,
7(3), 367-377.
Ramsetty, A., & Adams, C. (2020) Impact of the digital
divide in the age of COVID-19. JAMIA, 27(7), 1147-
1148.
Schoenfeld, A. J., Davies, J. M., Marafino, B. J., Dean, M.,
DeJong, C., Bardach, N. S., & Dudley, R. A. (2016).
Variation in quality of urgent health care provided
during commercial virtual visits. JAMA internal
medicine, 176(5), 635-642.
Sheikh, A., Sood, H. S., & Bates, D. W. (2015). Leveraging
health information technology to achieve the “triple
aim” of healthcare reform. JAMIA, 22(4), 849-856.
Shockley, T. (2020). Telehealth and Achieving the
Quadruple Aim in Rural communities: A Vision for the
21st Century. Health Science Journal, 14(6), 1-3.
Sikka, R., Morath, J. M., & Leape, L. (2015). The quadruple
aim: care, health, cost and meaning in work.
Smith, W. R., Atala, A. J., Terlecki, R. P., Kelly, E. E., &
Matthews, C. A. (2020). Implementation guide for
rapid integration of an outpatient telemedicine program
during the COVID-19 pandemic. Journal of the
American College of Surgeons, 231(2), 216-222.
Snoswell, C., Smith, A. C., Scuffham, P. A., & Whitty, J.
A. (2017). Economic evaluation strategies in telehealth:
obtaining a more holistic valuation of telehealth
interventions. Journal of telemedicine and telecare,
23(9), 792-796.
Steinman, M., Morbeck, R. A., Pires, P. V., Abreu Filho, C.
A. C., Andrade, A. H. V., Terra, J. C. C., ... &
Kanamura, A. H. (2015). Impact of telemedicine in
hospital culture and its consequences on quality of care
and safety. Einstein (Sao Paulo), 13(4), 580-586.
Tan, L. F. (2020). Ho Wen Teng V, Seetharaman SK, Yip
AW. Facilitating telehealth for older adults during the
COVID-19 pandemic and beyond: strategies from a
Singapore geriatric center. Geriatr Gerontol Int, 20,
993-995.
Thomas, E. E., Haydon, H. M., Mehrotra, A., Caffery, L. J.,
Snoswell, C. L., Banbury, A., & Smith, A. C. (2020).
Building on the momentum: Sustaining telehealth
beyond COVID-19. Journal of telemedicine and
telecare, 1357633X20960638..
Tuckson, R. V., Edmunds, M., & Hodgkins, M. L. (2017)
Telehealth. NEJM, 377(16), 1585-1592.
Turer, R. W., Jones, I., Rosenbloom, S. T., Slovis, C., &
Ward, M. J. (2020) Electronic personal protective
equipment: a strategy to protect emergency department
providers in the age of COVID-19. JAMIA, 27(6), 967-
971.
Vilendrer, S., Patel, B., Chadwick, W., Hwa, M., Asch, S.,
Pageler, N., & Sharp, C. (2020) Rapid deployment of
inpatient telemedicine in response to COVID-19 across
three health systems. JAMIA, 27(7), 1102-1109.
Waibel, K. H., Cain, S. M., Hall, T. E., & Keen, R. S.
(2017). Multispecialty synchronous telehealth
utilization and patient satisfaction within Regional
Health Command Europe: a readiness and recapture
system for health. Military medicine, 182(7), e1693-
e1697.
Winburn, A. S., Brixey, J. J., Langabeer, J., & Champagne-
Langabeer, T. (2018). A systematic review of
prehospital telehealth utilization. Journal of
telemedicine and telecare, 24(7), 473-481.
Wosik, J., Fudim, M., Cameron, B., Gellad, Z. F., Cho, A.,
Phinney, D., & Tcheng, J. (2020). Telehealth
transformation: COVID-19 and the rise of virtual care.
JAMIA, 27(6), 957-962.
HEALTHINF 2022 - 15th International Conference on Health Informatics
288
