
Evaluation on Risk Factors and Preventative Measures for Breast
Cancer in China
Xiaolu Tang
University of Washington, Seattle, WA, 98105, U.S.A.
Keywords: Breast Cancer, Risk Factors, Screening, Prevention.
Abstract: Breast cancer is one of the leading causes of death among females worldwide. The number of people who
have been diagnosed with breast cancer is increasing rapidly in China. To better understand the current
situation of breast cancer and propose suggestions on reducing the risk of breast cancer, risk factors associated
with breast cancer and measures that can effectively prevent the onset of breast cancer are introduced and
discussed. The research is conducted in the form of a literature review by summarizing, comparing, and
analyzing previous research and proposing constructive suggestions on how breast cancer can be prevented.
The objective of this review is to analyze the risk factors and several preventative measures of breast cancer
and to provide suggestions on future works.
1 INTRODUCTION
Breast cancer is the most commonly diagnosed
cancer in women worldwide and ranks as second-
highest cancer related death among cancers in
women (Fahad Ullah 2019). Breast cancer is a type
of metastatic cancer involving a series of mutations
and can potentially affect other organs including the
brain and liver (Collaborative Group on Hormonal
Factors in Breast Cancer 2002). All women are at risk
of developing breast cancer and a general trend is
observed that the chances increase with age. The
incidence and prevalence rates of breast cancer are
relatively high in developed countries such as North
America and Australia, and relatively low in Eastern
Asia counties including China. However, the
incidence rate and mortality rate of breast cancer of
women in China are rising in recent years with an
increase of about 20–30 % over the past three
decades and an annual growth rate of 3-5% (Fan,
Strasser-Weippl, St Louis, Finkelstein & Goss, etc.
2014). Breast cancer in China is not fully understood
in terms of the causes of breast cancer and effective
prevention and treatment measures lagged far behind
developed countries. Although some risk factors,
which are essential to understand the epidemiology
of breast cancer, have been identified by previous
research, no comprehensive analysis has been
conducted to summarize risk factors associated with
breast cancer. China has made a great effort focusing
on the treatment of breast cancer, but preventative
measures and diagnosis are largely neglected, and
early diagnosis is essential to suppress the growth of
primary tumors and lower the mortality rate
significantly. This review mainly focuses on three
parts. An overview of the current situation of breast
cancer in Chinese women is presented by using
statistics obtained on incidence rate and mortality
rate in recent ten years. Several risk factors closely
related to breast cancer are analyzed. Moreover, the
efficacy of current preventative measures is
evaluated, and new preventative measures are
proposed.
2 CURRENT SITUATIONS OF
BREAST CANCER IN CHINA
The incidence rate of breast cancer in China was low
until the 1990s when the incidence rate rose more
than twice as fast as have global rates. The China
National Cancer Centre reported the incidence rate
by using the age-specific rate from 2004 to 2009. The
highest incidence rate occurred in age groups of 50–
54 for females, with an age-specific rate of 92–108
per 100,000 Chinese women. The slope of the
incidence-age group curve rose with increase in age,
became flat for the age group of 60–69 years, and
gradually decreased from the age of 70. The
Tang, X.
Evaluation on Risk Factors and Preventative Measures for Breast Cancer in China.
DOI: 10.5220/0011357100003444
In Proceedings of the 2nd Conference on Artificial Intelligence and Healthcare (CAIH 2021), pages 269-274
ISBN: 978-989-758-594-4
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
269
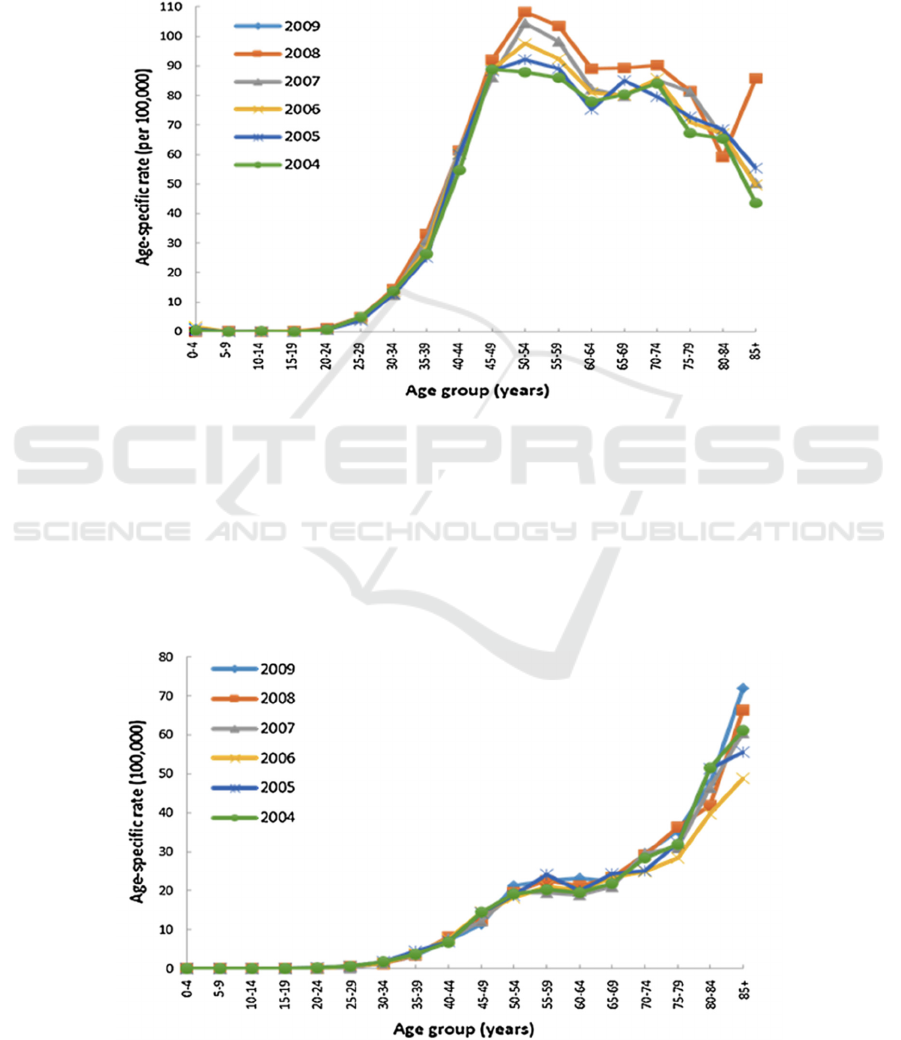
incidence rate generally increased from 2004 to 2009
for almost all age groups and the differences in
incidence rate became significant for people aged
above 50 years old. (Figure 1) The incidence rate also
varied significantly in different geographical
locations in China. Previous studies have
demonstrated that the average age-standardized rate
was 31.3 in urban areas compared to 12.1 per
100,000^2 in rural areas. The difference in incidence
rate can be attributed to factors such as variation in
socioeconomic status, accessibility to health
services, and difference in screening rate (Li, Mello-
Thoms & Brennan 2016).
Figure 1: Age-specific incidence rates of breast cancer in female from 2004 to 2009.
The trend in the mortality rate of breast cancer,
however, was inconsistent with the trend in incidence
rate in China from 2004 to 2009. The incidence rate
was lower for women aged above 60 years old
compared to women aged between 45 and 49, but the
mortality rate showed an increasing trend with age
and rose exponentially for women aged 85 and over.
(Fig. 2) Differences in mortality rates also existed
across geographical regions. Data have suggested
that the mortality rate tripled in urban areas
compared to rural areas with an increase of only 16%
from 2002 to 2008. The discrepancy can be explained
by the availably of sample sizes and limited access to
population-based statistics (Li, Mello-Thoms &
Brennan 2016).
Figure 2: Age-specific mortality rates of breast cancer in female from 2004 to 2009.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
270

Although some trends in the incidence rate and
mortality rate have been analyzed by using data
collected in recent one to two decades, only 13% of
the population has been included in the national
cancer registries in China. The dataset presented is
very limited and hard to reflect the comprehensive
situation of breast cancer through data interpretation
in China. Thus, expansion of cancer registration data
is essential, which would improve the accuracy in
estimating the number and burden of breast cancer
and better the current situation of breast cancer in
China.
3 RISK FACTORS ASSOCIATED
WITH BREAST CANCER
3.1 Genetic Factors
Breast cancer is largely caused by genetic factors and
many genes are associated with the chance of getting
breast cancer, including BRCA1/2, Epidermal
Growth Factor Receptor (EGFR), and HER2.
BRCA1/2 are tumor suppressor genes that suppress
cell growth when tumor cells are been detected. They
have the function of regulating the cell cycle
checkpoint and repairing DNA breaks to make sure
the normal function of cells. When deleterious
mutations happened in BRCA1/2 genes, the genes
lose functions and lead to the growth of tumor cells,
thus greatly increasing the risk of breast cancer.
However, developing cancer-related genes like
BRCA1/2 genes does not necessarily mean little
chance to survive through the disease. A meta-
analysis study conducted by Yaning Zhu et. al
examined the relationship between BRCA mutations
and patients’ survival rate, and the results are
summarized here to infer the association between
having BRCA 1/2 genes and breast cancer. The
survival rate of patients with breast cancer was
analyzed by using hazard ratios (HR) and breast
cancer-specific survival (BCSS). By examining the
results of 26 previous research reporting BRCA 1
mutation, BC patients with BRCA1mutation were
associated with worse OS compared to non-breast
cancer patients. The pooled HR was 1.69 (95% CI
1.35 to 2.12, p < 0.001; I2 = 59.1%) No association,
however, was found between BRCA1 mutation and
BCSS (HR = 1.14, 95% CI 0.81 to 1.61, p = 0.448;
I2 = 68.1%) The results were similar when analyzing
the BRCA2 mutations and patients had poor OS.
Also, no association has been found between BRCA2
mutation and BCSS (HR 1.16, 95% CI 0.82 to 1.66,
p = 0.401; I2 = 50.9%). The results might be
counterintuitive to many people but indicated
positive promises. As BRCA1/2 mutation did not
significantly influence the survival rate of patients,
actively and promptly seeking screenings and
treatments may increase the chance of survival for
breast cancer patients (Zhu, Zhang, Liu & Zhang
2016).
3.2 Breastfeeding and Parity
Breastfeeding is another risk factor associated with
breast cancer as breastfeeding and parity are related
to reproductive and hormonal receptors like estrogen
(ER). Parity is defined as the number of times that
women had given birth to a fetus. Previous studies
have confirmed that a 33% association was found
between parity and the increased risk of ER disease
(n = 1252; parous vs. nulliparous, RR = 1.33 [1.11–
1.59]). Women with higher parity who did not
breastfeed also had a higher risk of breast cancer
(e.g., ≥ 4 vs. 1 birth, RR = 1.68 [1.15–2.44]) but
not among women reporting ever breastfeeding (RR
= 1.33 [0.91–1.95]). Consequently, breastfeeding and
number of parity had been confirmed to significantly
influence the chance of whether women would get
breast cancer (Fortner, Sisti, Chai, Collins, Rosner &
Eliassen 2019). The one-child policy was a policy
unique in China implemented at the beginning of the
1980s, and it largely affected the breastfeeding
pattern for pregnant Chinese women. The total
fertility rate had decreased significantly from about
6.0 in 1950 to 1.6 in 2020 (Collaborative Group on
Hormonal Factors in Breast Cancer 2002). Since
women were only legally allowed to have one child,
the number of parity and the time for breastfeeding
declined dramatically. Thus, the risk of breast cancer
would likely increase during those 30 years.
3.3 Dietary Pattern
As economics rapidly developed in China, the
economic status of people have improved and they
could choose more options in terms of eating and
living. The diet of many Chinese people has changed
from a healthy traditional diet based on vegetables,
soybeans, and rice to a modern western diet that
contains too much fat. The Women’s Health
Initiative Randomized Controlled confirmed the
association between low-fat dietary patterns and risk
of breast cancer by examining 48,835
postmenopausal women from 1993 to 1998 at 40 US
clinical centers. The results demonstrated that during
Evaluation on Risk Factors and Preventative Measures for Breast Cancer in China
271

the 8.5 years intervention, the number of deaths had
reduced for breast cancer patients receiving the
dietary intervention, compared to those in the control
group (27 deaths [0.016% per year] v 61 deaths
[0.024% per year]; HR, 0.67; 95% CI, 0.43 to 1.06;
P = .08). A similar trend was found when dietary
intervention lasted for 16.1 years with 3,030 incident
breast cancers. Few deaths were observed in patients
in dietary group in contrast to patients in control
group (111 deaths [0.035% per year] v 185 deaths
[0.039% per year]; HR, 0.91; 95% CI, 0.72 to 1.15)
(Collaborative Group on Hormonal Factors in Breast
Cancer, 2002). When changing to a low-fat dietary
pattern, the risk of breast cancer and death was
significantly decreased. Other than reducing the
frequency of consuming food containing a lot of fat,
eating fiber may help prevent the onset of breast
cancer to some extent because fiber can reduce
cholesterol levels in the blood and even destroy
carcinogens.
4 PREVENTATIVE MEASURES
OF BREAST CANCER
4.1 Screening
Early detection and screening are important for
breast cancer prevention because many primary
tumors can be removed by surgery. There are mainly
two types of screening that are currently being used
to screen for breast cancer. Mammography is an
effective screening method that utilizes low-energy
X-rays to obtain high-resolution images of the breast,
but it can lead to problems like overdiagnosis. MRI
is another screening tool that has been widely applied
for breast cancer. The sensitivity of MRI is higher
than mammography, but the specificity of MRI is
much poorer than that of mammography with lower
detection rates (Fan, Strasser-Weippl, St Louis,
Finkelstein & Goss, etc. 2014).
Despite the development of screening technology
that makes early detection of breast cancer possible,
the screening rate is never optimistic in China.
Statistics have shown that the screening rate for
breast cancer was 25.7% for women aged between 35
and 64 years in 2015. Even though the screening rate
increased by 3% from 2013 to 2015, the number was
low compared to developed countries with a
screening rate of above 50%. Moreover, women in
rural areas and with low education levels had
significantly lower screening rates. Some screening
programs had been implemented since 2009 in China
which specifically provide easy access to screening
for rural female residents aged 35-59 years old,
however, the screening rate only increased partially
and there is no nationwide screening program for
breast cancer in China at present (China CDC
Weekly 2021). Therefore, continued efforts should
be made by governments and organizations to give
initiatives and financial support to implement more
screening programs for breast cancer. Also, screening
for breast cancer should be included in the regular
health check-up for women especially those above 35
years old and screening expenditures can be included
in health insurance to alleviate the burden of
financial difficulties especially in rural areas.
4.2 Chemoprevention
Chemotherapy is a primary method used for the
prevention and treatment of breast cancer worldwide.
It is an aggressive form of chemical drug therapy that
destroys the growing cells in the body. The estrogen
receptor is often a major target for chemotherapy
because over of 70% patients have ER-positive
breast cancer. Currently, two major classes of anti-
estrogen drugs are selective estrogen receptor
modulators (SERMs) and aromatase inhibitors (AIs)
(Zhu, Zhang, Liu & Zhang 2016). Although SERMs
and AIs have certain efficacy in treating breast
cancer, their side effects cannot be ignored including
stroke, osteoporosis, and joint pain. Thus,
researching on drugs that can be both effectively
target the disease and with few side effects is of high
priority. Neoadjuvant chemotherapy is a relatively
advanced method in early-stage prevention and
treatment for breast cancer. Neoadjuvant
chemotherapy works by targeting the primary tumors
fixed to the chest wall or skin, decreasing the size of
tumor cells before conducting surgery. Studies
conducted by MD Anderson have shown that the
survival rate of breast cancer patients increased
significantly if neoadjuvant chemotherapy was
implemented, and the size of tumors was reduced by
50% in at least 67% of patients in the study (Redden
& Fuhrman 2013).
In China, neoadjuvant chemotherapy is gradually
being used in the prevention and treatment of breast
cancer and in the stage of continuous development.
With the emergence of various clinical trials and new
treatment concepts, the treatment model has been
transformed from single chemotherapy to current
neoadjuvant chemotherapy based on different breast
cancer molecular subtypes. As new evidence-based
medicine data continue to be enriched, the
differences between various therapeutic concepts
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
272

and clinical practice become more obvious. Thus,
more emphasis should be placed on selecting and
applying neoadjuvant chemotherapy in clinical
practice, optimizing the treatment strategy for
patients, and improving treatment outcomes.
4.3 Changes in Diet Pattern
Another effective preventative measure is to promote
a healthy diet and lifestyle, which could be a risk
factor leading to breast cancer. Evidence has
demonstrated that a diet rich in saturated fat would
increase the risk of breast cancer, so promoting a diet
that includes rice, fresh vegetables, soy, pork would
reduce the risk of breast cancer. Dietary fiber is also
beneficial in preventing breast cancer as it promotes
the growth of probiotics and inhibits the growth of
pathogenic bacteria, which significantly reduces the
risk of breast cancer, especially for postmenopausal
women (Zhao, Zhang, Deng, etc. 2016). China has
implemented some policies in an effort to increase
the awareness of people in pursuing a healthy life.
One of them is The Healthy China Initiative 2019-
2030, which aims to improve national health policies
and provide comprehensive health services for
people. It addresses the urgent need to increase the
awareness of having a healthy diet among people and
to strengthen guidance on nutrition and health works
in schools and institutions. The policies are essential
to solve current health problems such as malnutrition
and excessive intake of high-calorie food, thereby
preventing breast cancer and other cancer diseases.
5 CONCLUSIONS
Breast cancer is becoming more common in China
with a rising incidence rate and mortality rate.
Identifying risk factors and implementing
preventative measures are important to reduce the
risk of breast cancer. The increase in the number of
Chinese women getting breast cancer is due to the
ignorant of risk factors that potentially lead to breast
cancer, and low awareness and financial difficulties
in conducting preventative measures timely.
Concrete and comprehensive programs and policies,
such as National Screening Program and Health
China Initiative, are necessary to improve
preventative measures and promote awareness of risk
factors associated with breast cancer.
Chinese government and institutions should
make continuous efforts in increasing the awareness
and knowledge of the public, providing more
convenient health services for early diagnosis
especially in rural areas, and improving biomedical
techniques to increase the accuracy of the breast
cancer diagnosis. The paper is subjected to some
limitations. The data used for the incidence rate and
mortality rate of breast cancer might not reflect the
actual situations of breast cancer in China as many
people are not included in the database. Moreover,
only risk factors that have been shown to have a
strong association with the risk of having breast
cancer were included and risk factors such as stress
and mood, which are hard to be analyzed
quantitatively, did not add into consideration. For
future works, more research and analysis can be
conducted on testing whether improving the
implementation of preventative measures of breast
cancer mentioned would decrease the risk of breast
cancer.
ACKNOWLEDGMENT
I would like to thank Prof. Trochim from Cornell
University and teaching assistant Yuanyuan Dong for
teaching me knowledge in public health and cancer-
related areas and provide me guidance with this
research paper.
REFERENCES
Chlebowski, R. T. et al, (2017). Low-Fat Dietary Pattern
and Breast Cancer Mortality in the Women's Health
Initiative Randomized Controlled Trial. Journal of
clinical oncology: official journal of the American
Society of Clinical Oncology, 35(25), 2919–2926.
Collaborative Group on Hormonal Factors in Breast
Cancer (2002). Breast cancer and breastfeeding:
collaborative reanalysis of individual data from 47
epidemiological studies in 30 countries, including
50302 women with breast cancer and 96973 women
without the disease. Lancet (London, England),
360(9328), 187–195.
Fahad Ullah M. (2019). Breast Cancer: Current
Perspectives on the Disease Status. Advances in
experimental medicine and biology, 1152, 51–64.
Fan, L., Strasser-Weippl, K., Li, J. J., St Louis, J.,
Finkelstein, D. M., Yu, K. D., Chen, W. Q., Shao, Z.
M., & Goss, P. E. (2014). Breast cancer in China. The
Lancet. Oncology, 15(7), e279–e289.
Fortner, R. T., Sisti, J., Chai, B., Collins, L. C., Rosner, B.,
Hankinson, S. E., Tamimi, R. M., & Eliassen, A. H.
(2019). Parity, breastfeeding, and breast cancer risk by
hormone receptor status and molecular phenotype:
results from the Nurses' Health Studies. Breast cancer
research: BCR, 21(1), 40.
https://doi.org/10.1186/s13058-019-1119-y
Evaluation on Risk Factors and Preventative Measures for Breast Cancer in China
273

Li, T., Mello-Thoms, C., & Brennan, P. C. (2016).
Descriptive epidemiology of breast cancer in China:
incidence, mortality, survival and prevalence. Breast
cancer research and treatment, 159(3), 395–406.
Redden, M. H., & Fuhrman, G. M. (2013). Neoadjuvant
chemotherapy in the treatment of breast cancer.
Surgical Clinics of North America, 93(2), 493-499.
Zhang, Mei; Zhong, Yijing; Bao, Heling; Zhao, Zhenping;
Huang, Zhengjing; Zhang, Xiao; Li, Chun; Zhou,
Maigeng; Wang, Limin; Wu, Jing; Zheng, Xiaoying;
Wang, Linhong. China CDC Weekly. (2021). Vol.3
(13), p.267-273.
Zhao, P., Zhang, L., Liu, Y., Yu, Q., Deng, Q., & Zhang, K.
(2016). Dietary fibre intake and risk of breast cancer:
A systematic review and meta-analysis of
epidemiological studies. Oncotarget, 7(49), 80980–
80989.
Zhu, Y., Wu, J., Zhang, C., Sun, S., Zhang, J., Liu, W.,
Huang, J., & Zhang, Z. (2016). BRCA mutations and
survival in breast cancer: an updated systematic review
and meta-analysis. Oncotarget, 7(43), 70113–70127.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
274
