
Application of Ultrasound-guided Caudal Block:
Anesthesia in Pediatric Percutaneous Nephrolithotomy
Miao Yang, Hua Fang, Chong Liu and Fang-Xiang Zhang
*
Department of Anesthesiology, Guizhou Province People’s Hospital, Guiyang 550002, China
*
Corresponding author
Keywords: Ultrasound, Anesthesia, Caudal, Percutaneous Nephrolithotomy, Child.
Abstract: Objective: Evaluation of ultrasound-guided caudal block anesthesia in pediatric percutaneous nephrolithotomy.
Methods: Fifty children undergoing percutaneous nephrolithotomy were equally and randomly divided into
general anesthesia group (Group G) and ultrasound-guided caudal block combined with general anesthesia
group (Group C). The recovery time, emergence agitation and postoperative complications of the two groups
were observed. The children in Group G received general anesthesia with tracheal intubation, and the children
in Group C received tracheal intubation general anesthesia after caudal block. The consumption of
intraoperative opioids was compared, the postoperative recovery time, emergence agitation and early
postoperative pain score were observed, and the postoperative complications were recorded. Results: The
number of opioid analgesics in Group C was less than that in Group G (P <0.05). Recovery time in Group C
was shorter than that in Group G, and CHIPPS score in Group C was less than Group G in PACU (P <0.05).
The incidence of emergence agitation in Group C was significantly less than that in Group G (P <0.05). The
incidence of nausea and vomiting in Group C was significantly less than those in Group G (P <0.05).
Conclusions: Ultrasound-guided caudal block can be safely used in pediatric percutaneous nephrolithotomy.
Caudal block can reduce the dosage of opioid analgesics, improves the quality of recovery and the effect of
postoperative analgesia. It is easy to operate and has fewer complications.
1 INTRODUCTION
Urinary calculus is a common and frequently-
occurring disease in urology, while urinary calculus
in children accounts for 2 ~ 3% of total urolithiasis
(Castagnetti 2010). Studies have pointed out that
kidney stones disease has been increasing at all ages
in recent years, which leads to an increasing number
of patients needing corresponding surgical treatment
(Zeng 2018). With the development of urology
endoscopy, most children’s upper urinary tract stones
are treated by endoscopy, with the characteristics of
less injury, high success rate and fewer complications
(Hong 2018). Children need general anesthesia
because it is hard for them to cooperate during
operation, and combined caudal block anesthesia is
gradually paid attention to because of the advantages
of a small amount of general anesthetic, quick
recovery after an operation and so on. Ultrasound-
guided caudal block is simple and safe, giving
attention to both surgical anesthesia and
postoperative analgesia, and has been gradually used
in pediatric surgery (Ecoffey 2010). In this study,
ultrasound-guided caudal block combined with
general anesthesia was used in pediatric percutaneous
nephrolithotomy and compared with general
anesthesia with tracheal intubation alone, and the
recovery time, restlessness during recovery and early
postoperative pain were observed, which remained a
reference for clinical practice.
2 MATERIALS AND METHODS
2.1 General Information
This study was approved by the Medical Ethics
Committee of our hospital, and informed consent was
signed with the parents or legal guardians of the
children. From December 2019 to March 2021, 50
children undergoing elective percutaneous
nephrolithotomy in our hospital were selected, all of
whom were with unilateral kidney calculi, 32 males
and 18 females, aged 3-6 years, with ASA I or II. The
Yang, M., Fang, H., Liu, C. and Zhang, F.
Application of Ultrasound-guided Caudal Block: Anesthesia in Pediatric Percutaneous Nephrolithotomy.
DOI: 10.5220/0011212800003444
In Proceedings of the 2nd Conference on Artificial Intelligence and Healthcare (CAIH 2021), pages 157-161
ISBN: 978-989-758-594-4
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reser ved
157
blood routine and coagulation function were normal
before an operation, and there was no obvious
abnormality in liver and kidney function, no obvious
oropharynx, head and neck deformity or activity
disorder, and no diseases of the central nervous
system and blood system. There was no skin infection
or sacrum deformity in the sacrococcygeal region.
Children were randomly divided into general
anesthesia group (Group G) and ultrasound-guided
caudal block combined general anesthesia group
(Group C), with 25 cases in each group.
2.2 Methods
Children were routinely fasted and forbidden to drink
before surgery, and dexmedetomidine was dripped
intranasally at 1 ug/kg, alternately dripped into
bilateral nostrils, and gently rubbed the nasal wings
on both sides for 2 ~ 3 times. After entering the
operating room, the peripheral venous access was
opened, oxygen was inhaled with a conventional
mask, HR, BP, ECG and SpO2 were monitored, and
the corresponding type of endotracheal tube was
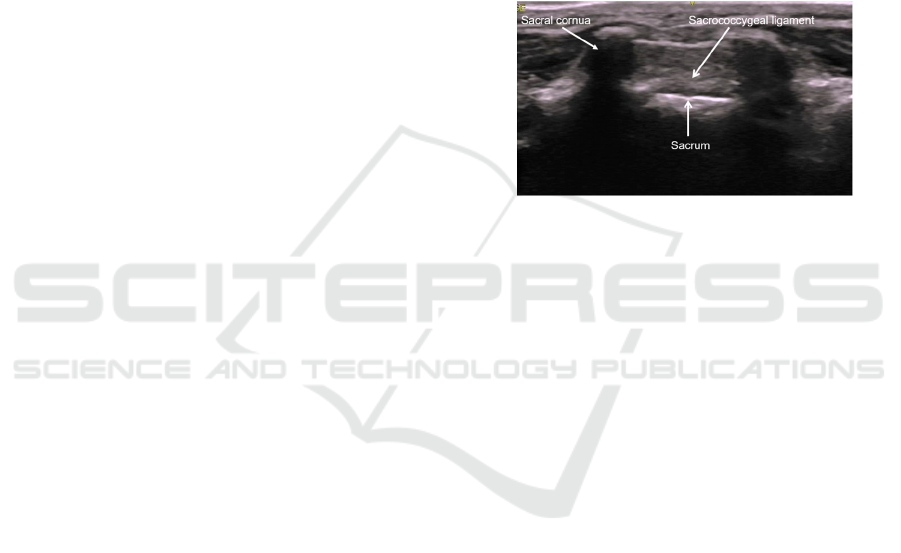
selected according to the age. In Group C, the
children were given ultrasound-guided caudal block
anesthesia, and the children were in the left lateral
position. After routine disinfection and towel laying,
the local anatomical structure of sacral hiatus was
observed with a 10 ~ 15 MHz linear array probe using
a color Doppler ultrasound instrument (GE Venue
50). The probe was placed in a sterile plastic sleeve,
perpendicular to the long axis of the body (cross-
section), and gradually moved upward from the
tailbone until a typical sacral hiatus image appeared
(Fig. 1). The puncture needle was inserted at the
midpoint of the probe using the out-of-plane
technique. After a sense of breakthrough appeared or
when the cross-section of the needle shaft in the sacral
hiatus was seen under ultrasound, the bloodless or
cerebrospinal fluid was pumped back, and then 0.2%
ropivacaine was injected 1ml/kg (Wang 2015).
During caudal solution injection, ultrasound showed
that the sacral hiatus was dilated (the sacrococcygeal
ligament was lifted), which indicated that the caudal
solution was injected into the sacral hiatus.
Anesthesia intubation was performed after nerve
block took effect and no adverse reactions such as
local anesthetic poisoning or total spinal anesthesia
were confirmed.
Two groups of children were given an intravenous
injection of propofol medium/long-chain fat
emulsion injection 3 ~ 3.5 mg/kg, fentanyl citrate
injection 2 ug/kg and rocuronium bromide injection 1
mg/kg for anesthesia induction. After mechanical
ventilation with the Omeda anesthesia machine, the
operation was started, continuous monitoring of end
tidal carbon dioxide Pressure (P
ET
CO
2
) was
maintained at 35 ~ 45 mmHg. During the operation,
remifentanil hydrochloride was injected
intravenously for 5 ~ 10 ug kg
-1
h
-1
, and sevoflurane
was inhaled for 2% ~ 3% to maintain anesthesia, with
an end-tidal concentration of 0.8 ~ 1.0 MAC. After
the operation, remifentanil hydrochloride and
sevoflurane were stopped, and the children were sent
to PACU after spontaneous breathing returned to
normal, swallowing and cough reflex became active,
and the endotracheal tube was pulled out, oxygen was
inhaled through the mask, and vital signs were stable.
Figure 1: Ultrasound image of sacral hiatus.
2.3 Observation Indicators
The dosage of opioid analgesics during the operation
was recorded in the two groups, and the recovery time
and the occurrence of restlessness during the recovery
period were observed. The recovery time was from
the end of operation to the time of pulling out the
endotracheal tube. After entering PACU, the agitation
was evaluated by five-point scale: 0: drowsiness,
wakefulness; 1: Quiet, sober and cooperative; 2:
Crying, need appeasement; 3: Crying and fidgeting
are serious, unable to comfort, but do not need
braking; 4: dysphoria, disorientation, need to press
and brake, 3 points or 4 points mean restlessness. 15
minutes after being sent to PACU, the postoperative
pain of children was evaluated by the CHIPPS
scoring method, and the behaviors such as crying,
facial expression, trunk posture, leg posture and
restlessness were scored. Each item was subdivided
into three levels, and the scores were recorded as 0, 1
and 2 points step by step, with a total score of 10
points. The higher the total score, the higher the
degree of pain. The CHIPPS score ≥ 4 points
suggested the need for joint analgesic drugs. The
postoperative complications such as nausea,
vomiting, hypoxemia, laryngeal spasm and reflux
aspiration were recorded. All operations were
performed in the same operating room, and all
children were graded by anesthesiologists in PACU.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
158
2.4 Statistical Analysis
Data were analyzed using the SPSS19.0 software
(SPSS Inc., Chicago, IL, USA). Data were presented
as mean ± standard deviation (SD). Comparisons
among multiple groups were performed using a one-
way analysis of variance. Data within groups were
analyzed using analysis of variance with repeated
measurements. P < 0.05 was considered statistically
significant.
3 RESULTS
3.1 Comparison of General Data of
Children between the Two Groups
There is no significant difference in sex composition,
age, body weight and operation time between the two
groups (P >0.05), as shown in Table 1.
Table 1: Comparison of general information between two groups.
Group C (n=25) Group G (n=25)
Gender (Male/Female) 15/10 17/8
Age (years) 4.2±2.5 4.5±2.7
Body mass (kg) 15.8±3.6 16.3±4.2
Operation time (min) 82.5±30.1 96.3±37.4
3.2 Comparison of the Number of
Opioid Analgesics Used in the
Operation between the Two Groups
The amount of opioid analgesics used in the operation
of Group C is less than that in Group G, and the
difference is statistically significant (P <0.05), as
shown in table 2.
Table 2. Comparison of consumption of intraoperative opioids between two groups
Group C (n=25) Group G (n=25)
Remifentanil (ug) 126.5±31.8* 224.6±47.2
Fentanyl (ug/kg) 2.5±0.3* 3.4±0.7
Compared with Group G: *P <0.05.
3.3 Comparison of Recovery Time and
Postoperative CHIPPS Score
between the Two Groups
The recovery time in Group C is shorter than that in
Group G, and the CHIPPS score in Group C is smaller
than that in Group G, the difference is statistically
significant (P <0.05), as shown in table 3.
Table 3. Comparison of recovery time and CHIPPS scores between two groups.
Group C (n=25) Group G (n=25)
Awaking time (min) 10.3±4.5* 16.7±5.2
CHIPPS score (points) 2.5±0.7* 4.3±1.1
Compared with Group G: *P <0.05.
3.4 Comparison of Restlessness and
Postoperative Complications
between the Two Groups
The children in Group C were mostly quiet after
tracheal extubation, and the incidence of restlessness
in Group C was significantly less than that in Group
G (P <0.05), and the incidence of nausea and
vomiting in Group C was less than that in Group G (P
<0.05). There was no hypoxemia, laryngospasm and
reflux aspiration in both groups, as shown in table 4.
Table 4: Comparison of emergence agitation and complication between two groups.
Group C (n=25) Group G (n=25)
Nausea and Vomiting 2 (8.0)* 5 (20.0)
emergence agitation 3 (12.0)* 12 (48.0)
Compared with Group G: *P <0.05.
. .
Application of Ultrasound-guided Caudal Block: Anesthesia in Pediatric Percutaneous Nephrolithotomy
159

4 DISCUSSION
Caudal block is commonly used in children’s inguinal
region surgery, urinary system surgery and lower limb
surgery, and it is combined with general anesthesia in
clinical practice. The anesthesia effect is exact, which can
reduce the number of general anesthetics during operation,
exert ideal muscle relaxation and analgesic effect,
effectively block the stress response induced by surgical
stimulation, reduce the use of opioid analgesics after the
operation, prolong the postoperative analgesia time,
promote postoperative recovery and further reduce the
average hospitalization days (Schloss 2015). Conventional
caudal block is a safe method, complications may be
observed especially in children. Complications such as
subcutaneous and intraosseous injection, local anesthetic
toxicity or spinal anesthesia are related to inaccurate
placement of the puncture needle (Afshan 1996). With the
improvement of high-resolution portable ultrasound
equipment and probe technology, ultrasound technology
has been more and more used in nerve block anesthesia,
which broadens the role of ultrasound in clinical anesthesia.
Ultrasound-guided caudal insert can see the sacral hiatus,
sacrococcygeal ligament and sacral lumen, and can observe
the liquid flow produced by the injected local anesthetic
drug in the sacral lumen in real-time. The sensitivity and
specificity of ultrasonic monitoring of the correct position
of puncture needle during ultrasound-guided caudal block
are 96% and 100%, which is feasible and practical for
clinical application (Schwartz 2008). Because the structure
of sacral hiatus and local anesthetic injection can be
observed in real-time under ultrasound, the drug injection
position can be accurately judged, the puncture difficulty
can be reduced, and the success rate of blocking can be
improved.
In this study, 0.2% ropivacaine was used for sacral
canal block, which had little toxicity, no local
anesthetic poisoning reaction or total spinal
anesthesia, and produced a good anesthetic effect.
The recovery time of Group C was shorter than that
of Group G and the CHIPPS score after PACU was
lower than that of Group G which indicated that the
sacral canal block under ultrasound guidance was
effective and the circulation was stable, which
reduced the dosage of opioid analgesics during
operation, effectively shortened the recovery time of
children, and provided perfect postoperative
analgesia, which was beneficial to rapid recovery and
early postoperative pain relief.
Emergence agitation refers to a mental state in
which children’s consciousness and behavior are
separated during the awakening period after general
anesthesia, which is characterized by stubbornness,
irritability and inability to comfort, even crying,
hands and feet moving and disorientation, etc., and it
is impossible to identify familiar people or things in
the past (Mihara 2015, Hijikate 2016). The incidence
of restlessness during the awakening period is mainly
related to factors such as operation type, unfamiliar
environment, urinary catheter, quick awakening after
anesthesia and postoperative pain degree (Kim 2013).
In this study, the incidence of emergence agitation in
Group C was significantly lower than that in Group
G. It is considered that caudal block can reduce the
stimulation of urinary catheter, improve the analgesia
and prolong the postoperative analgesia time, thus
reducing the circulation fluctuation caused by general
anesthesia drugs and pain induced emergence
agitation and reducing the incidence of nausea and
vomiting. Postoperative canal block has a good long-
term analgesic effect, which also has a good effect on
the operation and psychological recovery of children,
and improves the satisfaction of their families to the
operation, thus increasing the safety factor of
anesthesia (Wang 2015).
Our study has several obvious limitations. It may
be difficult to display the needle using the out-of-
plane technique in some children. We did not have a
comparative group with conventional caudal block,
so we cannot comment on the efficiency and success
rate of placement using ultrasound-guidance. In
addition, the incidence of complications may not be
correctly determined in groups with small sample
size. Therefore, studies should be conducted on
groups with larger sample sizes. Finally, this study
did not compare the analgesic effect and duration of
local anesthetics with different concentrations.
5 CONCLUSIONS
Ultrasound-guided caudal insert can see the sacral
hiatus, sacrococcygeal ligament and sacral lumen,
and can observe the liquid flow produced by the
injected local anesthetic drug in the sacral lumen in
real-time. Ultrasound-guided caudal block can
produce a good anesthetic effect. Compared with
general anesthesia alone, it reduces the dosage of
opioid analgesics, improves the quality of anesthesia
recovery and provides perfect postoperative
analgesia. Ultrasound-guided canal block in children
can achieve accurate positioning, reduce puncture
difficulty and the complications, improve the success
rate of a block. It is convenient to operate, has few
complications, is safe and effective, is satisfactory to
parents and children, and is worthy of clinical
application.
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
160

ACKNOWLEDGMENTS
Funding
This research was supported by the Foundation of
Science and Technology Department of Guizhou
Province (Qiankehe LH zi [2014]7027). and the
Youth Foundation of Guizhou Provincial People’s
Hospital (No. GZSYQN [2019]03). The funders had
no role in study design, data collection and analysis,
decision to publish, or preparation of the manuscript.
Availability of Data and Materials
The datasets used and analyzed during the current
study are available from the corresponding author on
reasonable request.
Declarations
Consent for Publication
Not applicable.
Competing Interests
All authors declare no conflicts of interest
REFERENCES
Afshan,G., &Khan, F.A. (1996).Total spinal anaesthesia
following caudal block with bupivacaine and
buprenorphine. Paediatr Anaesth.6(3):239–42.
Castagnetti, M., & Rigamonti,W.(2010).Extracorporeal
shock wave lithotripsy for the treatment of urinary
stones in children. Arch Ital Urol Androl.82(1):49-50.
Ecoffey, C., Lacroix, F., Giaufre,E., Orliaguet,g., &
Courreges, p. (2010). Epidemiology and morbidity of
regional anesthesia in children: a follow-up one-year
prospective survey of the French-Language Society of
Paediatric Anaesthesiologists (ADARPEF). Paediatr
Anaesth.20(12): 1061-1069.
Hijikata,T., Mihara,T., Nakamura,N.,Miwa,T.,Ka,K.,
&Goto, T. (2016).Electrical stimulation of the heart 7
acupuncture site for preventing emergence agitation in
children: A randomized controlled trial. Eue J
Anaesthesiol.33(7): 535-542.
Hong, Y., Xu,Q.Q., Huang, X.B.,Zhu,Z.J., Ye,H.Y.,Yang,
Q.Y., An,L.Z., Zhang, F.S., &Xu, T. (2018).
Outcome of percutaneous nephrolithotomy in the treatment
of pediatric patients under14 years old with upper
urinary calculi. J Clin Urology (China). 33(7):246-249.
Kim, M.S., Moon,B.E., Kim, H., &Lee,J.R. (2013).
Comparison of propofol and fentanyl administered at
the end of anesthesia for prevention of emergence
agitation after sevoflurane anesthesia inchildren. Br J
Anaesth.110(2): 274-280.
Mihara, T., Nakamura,N., Ka,K.,Oba,M.S., &Goto,T.
(2015).Effects of melatonin premedication to prevent
emergence agitation after general anesthesia in
children: A systematic review and meta-analysis with
trial sequential analysis. Eue J Anaesthesiol.32(12):
862-871.
Schloss, B., Martin,D., Tripi,J., Klingele,K., &Tobias,J.D.
(2015).Caudal epidural blockade for major orthopedic
hip surgery in adolescents. Saudi J Anaesth.9(2): 128-
131.
Schwartz, D., Raghunathan,K., Dunn,S., &Connelly,N.R.
(2008).Ultrasonography and pediatric caudals. Anesth
Analg.106(1): 97-99.
Wang, H., Liu,G., Fu,W., &Li,S.T. (2015).The effect of
infraorbital nerve block on emergence agitation in
children undergoing cleft lip surgery under general
anesthesia with sevoflurane. Pediatric
Anesthesia.25(9): 906-910.
Wang, W.K., Guo, W.B., Liu,H., Xu,G.C., &Yang,Q.G.
(2015).Comparison of postoperative analgesia between
transversus abdominis plane block and caudal block for
Hirschsprung’s disease. J Clin Anesthesiol, 2015,
35(2):194-196.
Zeng, G.H., Zhu, W., &Lam, W. (2018). Miniaturised
percutaneous nephrolithotomy: Its role in the treatment
of urolithiasis and our experience. Asian J Urol.
5(4):295-302.
Application of Ultrasound-guided Caudal Block: Anesthesia in Pediatric Percutaneous Nephrolithotomy
161
