
Dietary Patterns and Their Effect on the Colorectal Cancer Risk
Hongji Zou
a
University of Liverpool, Liverpool, U.K.
Keywords: Colorectal Cancer, Dietary Patterns, Retrospect, Effect.
Abstract: Colorectal cancer (CRC) the third most commonly diagnosed cancer, excluding skin cancers, worldwide. In
2018 alone, there were close to 2 million new cases all over the globe (World Cancer Research Foundation
International 2019). In 2020, CRC accounted for about 10% of all cancer cases and deaths, recording about
1.9 million new diagnoses and 935,000 fatalities (Sung 2020). In this year, it is projected that there will be an
estimated 104,000 new diagnoses of colon cancer, and about 45,000 new diagnoses of rectal cancer (De
Stefani 2011). There is a 4.3% risk of developing CRC for men, and a 4.0% risk for women (World Cancer
Research Foundation International 2019). Therefore, colorectal cancer has caused a huge burden on social
and economic development worldwide. More and more studies have shown that eating more foods rich in
dietary fiber and dairy products can reduce the incidence of colorectal cancer, while eating more red meat and
processed meat products can increase its incidence (World Cancer Research Fund and American Institute for
Cancer Research 2017).
1 INTRODUCTION
There is evidence that dietary and lifestyle factors
contribute to the risk of developing CRC, and a
number of foods have been studied and reported on in
relation to their associated CRC risk. For instance,
research shows that consuming whole grains, dairy
products, foods high in dietary fibre and taking
calcium supplements lowers CRC risk, while
consuming processed meats, red meat and alcoholic
drinks increases relative CRC risk (World Cancer
Research Fund and American Institute for Cancer
Research 2017). However, the above-named foods
are rarely consumed individually, and instead are
components of a larger dietary pattern. Studying food
and nutrient combinations better elucidates the
dietary patterns of a population and their associated
CRC risk, since chronic diseases usually result from
many interacting variables.
This review looks at studies ranging from 1998 to
2021. We review the literature on the relationship
between different dietary patterns and the relative risk
(RR) for CRC to provide a reference for the public
healthy diet model, and for the primary prevention
strategy of colorectal cancers.
a
https://orcid.org/0000-0003-2771-2748
2 METHOD
PubMed-NCBI was searched for articles up to June
2021 that researched potential correlations between
dietary patterns or foods and the relative risk for
CRC. The search included the following keywords or
phrases: diet, dietary pattern, colorectal cancer, and
epidemiology. Studies that reported risk estimates
(odds ratios [ORs], and RR) of cancer and measures
of variability (SEs or 95% CIs from which these could
be derived) were selected preferably. Primary papers
were selected preferably where possible, but meta-
analyses were not excluded.
3 RESULTS
The papers studied had a number of different
classifications of dietary patterns. While some of the
studies included less popular dietary patterns,
including the traditional and the substitute patterns,
three patterns were consistently found in at least most
of the papers: Western, drinker and prudent. For this
reason, we have focused on the literature on the three
main dietary patterns. Other patterns mentioned in the
Zou, H.
Dietary Patterns and Their Effect on the Colorectal Cancer Risk.
DOI: 10.5220/0011205900003444
In Proceedings of the 2nd Conference on Artificial Intelligence and Healthcare (CAIH 2021), pages 141-145
ISBN: 978-989-758-594-4
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
141
chosen papers have been mentioned briefly in the
final section of the results.
3.1 The Western Dietary Pattern
The Western dietary pattern is described as a
“modern” diet, including a lot of processed foods.
Though the specific elements may vary from study to
study depending on the cultures of origin and the
authors’ research interests, most will be characterized
by red meat and processed meats, eggs, refined
grains. The Western dietary pattern may also include
plenty of processed sugars, fried foods and potatoes,
and low intakes of whole grains, fresh vegetables and
fruits (Tseng 2000). The Western dietary pattern has
shown an association with an increased risk for CRC.
A long study of CRC in Montevideo, Uruguay,
spanning from 1996 to 2004, studied 610 cases, with
1220 controls from the same hospitals (Fawehinmi
2012). With the samples and controls divided into
three dietary patterns for women (Western, prudent
and drinker) and four for men (Western, prudent,
drinker and traditional), the study found that the
Western dietary pattern showed an Odds Ratio of 2.62
(95 % CI 1.36-5.08) for colon cancer in men, and 1.95
(95 % CI 1.00-3.78) in women. Rectal cancer was not
found to be associated with the Western diet, which
was defined as consisting of high quantities of total
eggs, red meat and processed meats.
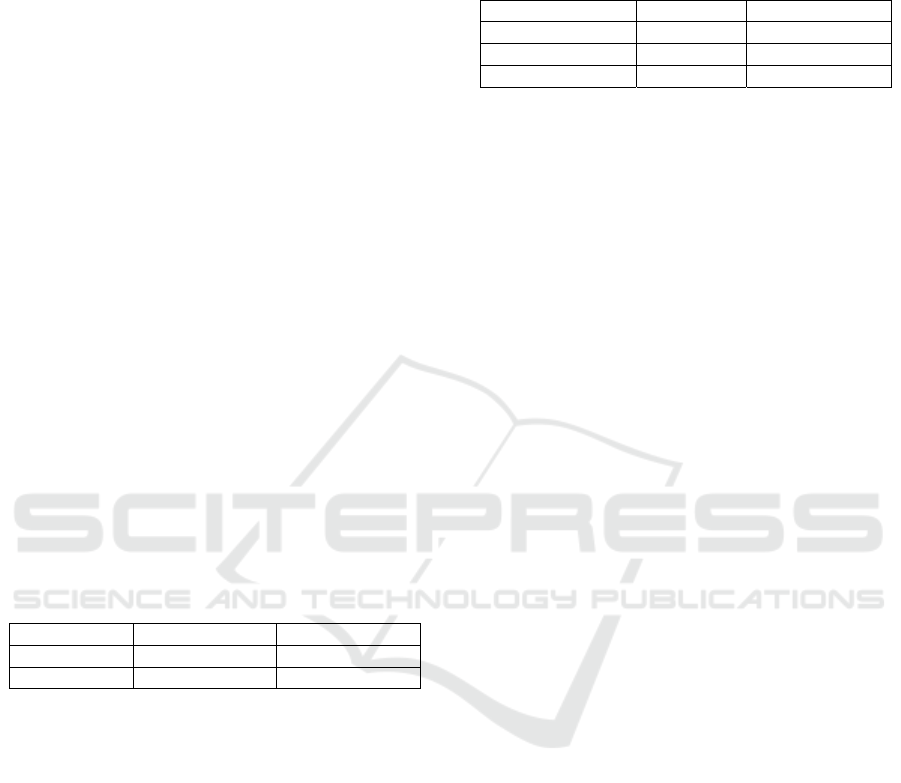
Table 1: Western dietary pattern.
Gende
r
Odds Ratio 95%CI*
Men 2.62 1.36-5.08
Women 1.95 1.00-3.78
*CI confidence interval
A similar study running for 32 years did a follow-
up of 3260 cases of CRC among health professionals
across the US, comparing CRC risk associated with
Western and prudent diets (Mehta 2017). Participants
who had more of the Western dietary pattern showed
an increased risk of CRC, while those who scored
higher in prudent dietary patterns had a lower risk of
CRC. The relative risk for CRC correlated with the
Western diet was also found to have differences in
anatomic subsites. Distal colon and rectal tumors had
a relative risk of 1.55 (95% CI, 1.22–1.96) and 1.35
(95% CI, 1.03–1.77) respectively. Proximal colon
cancers, in contrast, had an RR of 1.11 (95% CI, 0.91–
1.35). Notably, this paper also studied the correlation
between dietary patterns and different molecular
subtypes of CRC. Though the findings still required
further refining, the study found that the Western
dietary pattern was also more strongly correlated with
BRAF- and KRAS-wildtype, and CIMP-
negative/low tumors.
Table 2: The relative risk.
Index RR 95%CI*
Distal colon 1.55 1.22-1.96
Rectal tumors 1.35 1.03-1.77
Proximal colon 1.11 0.91-1.35
*CI confidence interval
Fung et al. found that a Western diet consisting of
large intakes of sweets and desserts, processed and
red meats, refined grains and French fries reported a
high relative risk for colon cancer, at 1.46 (95% CI,
0.97-2.19) (Giovannucci 2002). This paper studied
121,700 women between the ages of 30 and 55 across
11 states, over 12 years of follow-up. Similar to the
aforementioned study by De Stefani et al. in Uruguay,
this study found little to no significant correlation
between the Western dietary pattern and rectal cancer.
This paper reinforces the earlier study by providing
evidence that the impact of the Western diet on
relative CRC risk is generally the same, irrespective
of sex.
Some studies have gone a step further in their
characterizations of dietary patterns. For instance,
Slattery et al. described the Western diet as containing
a higher intake of dietary cholesterol and total energy,
and a greater body mass (Slattery 1998). This diet was
found to be correlated with a higher RR for colon
cancer in both men and women. A meta-analysis of
40 studies investigating the effects of the Western diet
also showed that this dietary pattern may increase the
RR of CRC (Fung 2003). One study included an
analysis of dietary patterns by the duration during
which the participants partook in them. The results
showed that the duration definitely matters (Song
2015). This study found that partaking in a Western
dietary pattern over an extended period of time was
associated with a higher RR for CRC, highlighting
that the prevalent diet during adolescence has a long-
lasting effect, regardless of adult diet. After a CRC
diagnosis, a higher indulgence in the Western diet
further increases the risk of recurrence after
treatment, and mortality.
3.2 The Drinker Dietary Pattern
The drinker dietary pattern, though not as extensively
studied as the Western and prudent patterns, has also
been studied and implicated in an increased relative
risk for CRC. This pattern is characterized by high
quantities of alcoholic beverages, and this is what
most studies focus on. Some studies have suggested
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
142

that the drinker dietary pattern may include poor
nutritional intake, like Fawehinmi et al. that heavy
and moderate drinkers consumed less favorable
loadings of nutritious and healthy foods than non-
drinkers (Feng 2017).
The drinker dietary pattern was consisted mainly
of younger men who consumed wine, beer and hard
liquors, and also smoked heavily in a study by De
Stefani (Salaspuro 2009). This group showed a
positive association with a higher RR for CRC.
Though the sample of women under the drinker
dietary pattern classification featured less intensive
smokers, they also showed poor nutritional intake and
cholesterol consumption, and mirrored the male
sample in CRC risk. The Slattery et al. definition of
the drinker pattern also included smokers, though this
category featured less red meat and more poultry and
fish in this study (Slattery 1998). The drinker pattern
recorded a very weak positive association with colon
cancer in men. The ‘alcohol-consumption’ pattern, as
it was termed in a meta-analysis ty Feng et al. was
reported to potentially increase the relative risk for
CRC, regardless of gender (Fung 2003).
3.3 The Prudent Dietary Pattern
Although the description of the prudent dietary
pattern is determined specifically by the authors of a
paper for their study, there are general features that
apply across the board in many studies. This diet
features an abundance of fresh fruits and green
vegetables, salads and carrots (Salaspuro 2007). Each
of the studies discussed above has slightly different
qualifiers of a “prudent” dietary pattern, but they are
all built on the same basics as listed. These studies
have one other thing in common: they all provide
evidence that the prudent dietary pattern protects
against colon and rectal cancers.
For the study in Montevideo, Uruguay, the
prudent diet was described as having high intakes of
dairy foods, white meat, total fruits and raw
vegetables. This pattern was found to be strongly
effective in preventing rectal cancer (Pietinen 1999).
Mehta et al demonstrated that prudent dietary
patterns, consisting of high quantities of whole grains,
fruits, vegetables and fish, generally have a lower
association with colon and rectal tumors, irrespective
of molecular subtypes and anatomical subsites
(Pöschl 2004). In Fung et al. prudent dietary
patterns including the regular whole grains, fruits and
vegetables plus poultry, legumes and fish, showed an
inverse correlation with colon cancer, but showed
little to no significant correlation with RR for rectal
cancer in women (Cancer.org. 2021).
Slattery et al described the prudent dietary pattern
as being associated with smaller body size, rigorous
leisure physical activity and higher quantities of
dietary folates and fibers (Pietinen 1999). This study
included age variations in the subjects, and found that
the prudent diet was correlated with a decreased RR
for colon cancer, particularly in younger individuals.
These results were further confirmed by a meta-
analysis by Feng et al (Fung 2003), which showed
that the ‘healthy’ dietary pattern, with the same
features as the prudent dietary pattern, may reduce the
RR for CRC. Song, Garrett and Chan showed that the
prudent pattern is protective against CRC, especially
when the diet is adhered to from adolescence (Song
2015). This study also showed that following a
diagnosis of CRC, the prudent dietary pattern is
recommended to prevent recurrence and to improve
disease prognosis.
3.4 Other Dietary Patterns
Although the three dietary patterns discussed above
are the most commonly studied in the literature, some
studies include less common patterns. De Stefani et al
studied the traditional dietary pattern but only in men
(Salaspuro 2009). It was described as having high
quantities of cooked vegetables, desserts, legumes
and tubers. This diet shared many similarities with the
Western diet, but was classed separately considering
the geographical location and cultural background of
the area under study. Most of the men who reported
under the traditional pattern were poorly educated and
lived in the rural areas of Uruguay. The traditional
dietary pattern was found to have an inverse
association with both colon and rectal cancers.
Slattery et al had five dietary patterns: prudent,
drinker, Western, substituters and high fat/sugar dairy.
The first three have been discussed above (Pietinen
1999). Substituters switched out butter, red meat, high
fat dairy products and refined grains in favor of
margarine, poultry, low fat dairy products and whole
grains, respectively. This pattern is perceived as
healthier than the Western pattern. However, this
study showed that this substitution did not
significantly reduce the RR for colon cancer. The high
fat/sugar dairy pattern contained high quantities of
yogurt and dairy products rich in fat and sugar. This
dietary pattern was not studied for relative risk of
colorectal cancer.
4 DISCUSSIONS
Most of the papers studied for this review found that
Dietary Patterns and Their Effect on the Colorectal Cancer Risk
143

dietary patterns have an association with the relative
risk for CRC in both men and women. The exception
was Pietinen et al which studied the relative risk for
CRC of different diet components rather than dietary
patterns, and found that high intake of calcium, milk
products and milk protein had an inverse correlation
with the RR for CRC, while high intake of fat, dietary
fiber, fried meats, vegetable and fruits had no
significant association with risk for CRC (Pöschl
2004). The food components found to have no
association with CRC risk cut across both the prudent
and Western dietary patterns, by the general
characterizations of both patterns. Extrapolating the
results of this study to our model of dietary patterns,
Pietinen et al. found that dietary patterns in general
have no correlation to the relative risk of CRC, and
rather it is specific foods, especially dairy products
and other calcium-rich foods that have an impact on
CRC relative risk.
The main tentative conclusion of this review is
that the Western and drinker dietary patterns show a
positive correlation with an increased relative risk for
colon cancers, but this association is much less
definite in rectal cancers.
This review highlights the differences in the
constitutions of different dietary patterns, as well as
the differences in classifications, to different
researchers. Though these differences may seem
subtle (the difference is usually only in a few food
groups), when considered as forming a daily diet that
spans decades of an individual’s life, individual foods
make a significant difference in the overall effect of a
diet. This consideration thus has us wondering
whether it is in fact effective to study the effect of
broad dietary patterns rather than isolated foods.
Even so, the majority of the papers studied for this
review showed that the prudent dietary pattern is the
healthiest and the most protective, with the highest
negative association with colorectal cancers,
regardless of gender, age, molecular subtypes and
anatomical subsites. The prudent dietary pattern
notably contains fresh green vegetables (some papers
specify that the green vegetables have to be eaten raw
to qualify under the prudent pattern). Fresh green
vegetables are high in dietary fiber. Fruits and cereals,
which may also be indicated as part of this diet are
also sources of fiber. It was demonstrated in a
screening trial that participants who regularly
consumed higher quantities of dietary fiber had a
lower risk of colorectal adenomas (Mehta 2017).
Further, the components of the prudent dietary pattern
are also high in antioxidants, which would confer
protection, not just from colorectal cancers, but from
other cancers as well.
The Western dietary pattern, in all its versions in
the papers studied for this review, included high
loadings of processed meats and red meat, and it has
been shown definitively to have an increased relative
risk for CRC. These results are consistent with the
findings of the International Agency for Research on
Cancer (IARC) (Cancer.org. 2021), which reported
that consumption of red meat and processed meats is
mutagenic and carcinogenic to humans. Though red
meat contains high quantities of important proteins
and micronutrients like iron and vitamin B, it also
contains haem iron which when broken down, forms
N-nitroso-compounds (NOC) are released, which are
carcinogenic. Meat processing and cooking can also
result in the formation of NOC and polycyclic
aromatic hydrocarbons (PAH), particularly with high-
temperature preparations such as barbecuing or
grilling. It is therefore no wonder that diets featuring
high loadings of these meats would show a higher RR
for CRC and other cancers (Aykan 2015).
The drinker dietary pattern has been consistently
shown to increase the risk of CRC by the papers in
this study, even though it is more consistently
associated with colon cancers than with rectal
cancers. These results are backed up by research that
shows that alcohol consumption has a causal
relationship with an increased risk of digestive system
cancers, including those of the colon and rectum, and
also of the breast in women (Bouvard 2015). The
exact mechanism of the association of alcohol
consumption and colorectal cancer is still under
study. One epidemiological study suggested that this
action is because alcohol affects the metabolism of
dietary folates, where folates are thought to reduce the
relative risk of CRC and other cancers (Kunzmann
2015). A more substantial explanation for the
correlation between CRC and alcohol consumption is
that ethanol metabolism releases acetaldehyde and
reactive oxygen species (ROS). Acetaldehyde has
been shown to be mutagenic and carcinogenic, and
has been implicated as a common denominator in the
development of many alimentary tract cancers
(Salaspuro 2009). It binds to proteins and DNA and
disrupts folate. Research has also shown that
acetaldehyde can be produced by oral bacteria. The
fact that the drinker dietary pattern is commonly
characterized by moderate to heavy smoking may
also be a factor in the results seen. Smoking is known
to alter the flora of oral bacteria, which may impact
the production of acetaldehyde (Pöschl 2004).
Cigarettes also contain acetaldehyde (Salaspuro
2007).
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
144

5 CONCLUSIONS
The study of dietary patterns and their disease
association has become popular as a way to better
understand the impact of combining well studied and
documented individual foods. The literature shows
multiple classifications of dietary patterns, but the
three most common are the “Western” diet, the
“drinker” diet and the “prudent” diet. Of the three, the
Western diet has consistently shown the highest
positive association with an increased relative risk for
CRC, though the association is stronger with colon
cancers than with rectal cancers. This is presumably
because of the high intake of carcinogenic meats, and
the low intake of beneficial vitamins and
antioxidants. The drinker dietary pattern has shown a
less consistent association with an increased risk for
CRC, but it has not shown a negative correlation in
any of the studies reviewed in this paper. The prudent
dietary pattern has consistently shown to be the
healthiest, even when other patterns such as the
substitute pattern are considered. This pattern
provides high quantities of beneficial nutrients and
antioxidant, and contains low quantities of
carcinogenic foods. Even so, the vast differences in
how each of these dietary patterns is characterized in
the literature could be a potential avenue for
confusion. The research shows that perhaps
recommending an increase in some foods and a
reduction of others may be more beneficial in creating
guidelines for healthy living and the prevention of
CRC, than recommending a larger dietary pattern
whose details are left to interpretation.
REFERENCES
Aykan, N.F. (2015). Red meat and colorectal cancer.
Oncology reviews, 9(1).
Bouvard, V., Loomis, D., Guyton, K.Z., et al. (2015).
Carcinogenicity of consumption of red and processed
meat. The Lancet Oncology, 16(16), pp.1599-1600.
Cancer.org. (2021). Colorectal Cancer Statistics-How
Common Is Colorectal Cancer?. [online]Available at:
<link> [Accessed 26 July 2021].
De Stefani, E., Deneo-Pellegrini, H., Ronco, et al. (2011).
Dietary patterns and risk of colorectal cancer: a factor
analysis in Uruguay. Asian Pac J Cancer Prev, 12(3),
pp.753-759.
Fawehinmi, T.O., Ilomäki, J., et al. (2012). Alcohol
consumption and dietary patterns: the FinDrink study.
PloS one, 7(6), p.e38607.
Feng, Y.L., Shu, L., Zheng, P.F., et al. (2017). Dietary
patterns and colorectal cancer risk: a meta-analysis.
European Journal of Cancer Prevention, 26(3), pp.201-
211.
Fung, T., Hu, F.B., Fuchs, C., et al. (2003). Major dietary
patterns and the risk of colorectal cancer in women.
Archives of internal medicine, 163(3), pp.309-314.
Giovannucci, E., (2002). Epidemiologic studies of folate
and colorectal neoplasia: a review. The Journal of
nutrition, 132(8), pp.2350S-2355S.
Kunzmann, A.T., Coleman, H.G., Huang, W.Y., et al.
(2015). Dietary fiber intake and risk of colorectal
cancer and incident and recurrent adenoma in the
Prostate, Lung, Colorectal, and Ovarian Cancer
Screening Trial. The American journal of clinical
nutrition, 102(4), pp.881-890.
Mehta, R.S., Song, M., Nishihara, R., et al. (2017). Dietary
patterns and risk of colorectal cancer: analysis by tumor
location and molecular subtypes. Gastroenterology,
152(8), pp.1944-1953.
Pietinen, P., Malila, N., Virtanen, M., et al. (1999). Diet and
risk of colorectal cancer in a cohort of Finnish men.
Cancer causes & control, 10(5), pp.387-396.
Pöschl, G. & Seitz, H.K., (2004). Alcohol and cancer.
Alcohol and alcoholism, 39(3), pp.155-165.
Salaspuro, M., (2007), April. Interrelationship between
alcohol, smoking, acetaldehyde and cancer. In Novartis
Foundation symposium (Vol. 285, p. 80). Chichester;
New York; John Wiley; 1999.
Salaspuro, M., (2009). Acetaldehyde as a common
denominator and cumulative carcinogen in digestive
tract cancers. Scandinavian journal of gastroenterology,
44(8), pp.912-925
Slattery, M.L., Boucher, K.M., Caan, B.J., et al. (1998).
Eating patterns and risk of colon cancer. American
journal of epidemiology, 148(1), pp.4-16.
Song, M., Garrett, W.S. , Chan, A.T., (2015). Nutrients,
foods, and colorectal cancer prevention.
Gastroenterology, 148(6), pp.1244-1260.
Sung, H., Ferlay, J., Siegel, R.L., et al. (2021). Global
cancer statistics 2020: GLOBOCAN estimates of
incidence and mortality worldwide for 36 cancers in
185 countries. CA: a cancer journal for clinicians,
71(3), pp.209-249.
Tseng, M. & DeVillis, R.F., (2000). Correlates of the
“western” and “prudent” diet patterns in the us. Annals
of epidemiology, 10(7), pp.481-482.
World Cancer Research Foundation International. (2019).
Colorectal cancer statistics. [online]Available at:
<link> [Accessed 26 July 2021].
World Cancer Research Fund and American Institute for
Cancer Research, (2017). Food, nutrition, physical
activity, and the prevention of cancer: a global
perspective (Vol. 1). Amer Inst for Cancer Research.
Dietary Patterns and Their Effect on the Colorectal Cancer Risk
145
