
Clinical Case Study of ABO Hemolytic Disease in Full-term
Newborns with Positive Free Test and Direct Antiglobulin Test
Yan Jin
a
Department of Neonatology, the People’s Hospital of Baise, Baise, Guangxi,China
Keywords: Newborn, ABO Hemolytic dDisease, Free Antibody Test, Free Antibody Test, Direct Antiglobulin Test.
Abstract: ABO hemolytic disease of newborn (ABO-HDN) occurs early and progresses rapidly, which can lead to fetal
or neonatal anemia and neonatal hyperbilirubinemia. Severe intrauterine hemolysis can lead to fetal edema,
which can lead to fetal death or neonatal death. Severe or very severe hyperbilirubinemia can be complicated
with bilirubin encephalopathy, Affect the quality of life of newborns.In this study, full-term children with
ABO-HDN were divided into two groups according to the results of three serological tests of hemolysis.
Group A: single antibody release test (ART) was positive; Group B: ART positive, combined with at least
one hemolysis test positive in direct antiglobulin test (DAT) and free antibody test (FAT). The differences of
minimum hemoglobin, age at onset (h) and incidence of anemia between group A and group B were compared.
1 INTRODUCTION
1
ABO-HDN postpartum diagnosis methods mainly
rely on three hemolysis tests, as follows: ①FAT is
one of the necessary detection methods for the
postpartum diagnosis of ABO-HDN. It can check
whether there is free IgG antibody in the serum of the
newborn and indirectly indicate the concentration of
antibody in the serum of the child. It has guiding
significance for the hemolysis persistence of the child
and the clinical diagnosis and treatment of ABO-
HDN and the progress of the disease.In this test, adult
red blood cells of the same blood group are dropped
into the serum of sick newborns, and then anti human
globulin serum is dropped. Red blood cell
agglutination indicates that the test is positive. ②
DAT is a basic method for the diagnosis of ABO-
HDN. Positive enhancement of DAT is correlated
with the demand for phototherapy, and no false
positive DAT cases have been found (Valsami,
Politou, Boutsikou, et al.2015). DAT is a good
indicator for predicting the development of ABO-
HDN with ABO incompatibility (Aydin, Deveci,
Orman, et al.2016, Ulrich, Ellsworth, Carey 2014). If
there is IgG antibody inconsistent with erythrocyte
membrane surface antigen in newborns, it can
combine with erythrocyte membrane surface antigen
a
https://orcid.org/0000-0002-3465-7057
to form immune complex. However, due to the small
molecular weight of incomplete antibody, it can not
connect the antigen antibody complex well, which
only leads to the sensitization of red blood cells. After
the anti globulin serum is added, it can bind with the
incomplete antibody adsorbed on the red blood cells,
so as to link the sensitized red blood cells and produce
visible agglutination. Direct antiglobulin test (DAT)
can detect the presence of IgG anti-A or anti-B and
C3 on erythrocyte membrane to help identify
hemolysis as immune dependent or immune
independent. In the test, EDTA is best used for blood
samples (Shaz, Hillyer, Gil 2019). Meanwhile, the
neonatal DAT results can well predict their
compliance with the therapeutic indication of
hyperbilirubinemia(Shi, Ma, Zhu, et al 2018). ③
ART uses the reversibility of antigen antibody
reaction to release IgG antibody on sensitized red
blood cells of children with neonatal hemolytic
disease into normal saline through physical or
chemical methods. The released IgG antibody still
has biological activity. Standard type A or type B red
blood cells are added to the release solution, and the
released IgG antibody will sensitize red blood cells,
Subsequently, anti human globulin serum was added,
and the red blood cell aggregation visible to the naked
eye was positive. Among the three detection methods
Jin, Y.
Clinical Case Study of ABO Hemolytic Disease in Full-term Newborns with Positive Free Test and Direct Antiglobulin Test.
DOI: 10.5220/0011163000003444
In Proceedings of the 2nd Conference on Artificial Intelligence and Healthcare (CAIH 2021), pages 47-51
ISBN: 978-989-758-594-4
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
47

of abo-hdn hemolysis, the positive rate of antibody
release test is the highest(Daniel 2019). The
combination of heat release test and acid release test
can improve the positive detection rate of neonatal
ABO hemolytic disease and reduce the risk of missed
detection in release test (Chen, Deng, Huang, et
al.2019). Compare the results of slide test, tube test
and microcolumn gel test. Results the success rate of
ABO blood group identification by microcolumn gel
method was higher than that of slide method + test
tube method (You 2019).
Microcolumn gel cassette detection (MGCP) is
highly sensitive to serological tests of hemolytic
disease of the newborn by MGCP. It can significantly
improve the detection rate of ABO-HDN positive,
which can effectively reduce the missed diagnosis
rate. Moreover, the MGCP test is convenient and
quick, and easy to operate. It is better than the three
test of ABO-HDN in vitro with the test tube anti
human globulin test (TAT). Some studies also found
that compared with venous blood test, umbilical cord
blood hemolysis serological test is helpful to early
diagnose neonatal ABO-HDN and control the disease
as soon as possible (Hu, Zhang 2019). This study
retrospectively analyzed the clinical data of children
with ABO-HDN who met the diagnosis and treatment
criteria, and discussed the clinical manifestations and
influence of full-term ABO-HDN with positive free
test and direct antiglobulin test.
2 SUBJECTS AND METHODS
2.1 Study Subjects
The subjects selected 127 term neonates who met the
diagnostic criteria for the ABO-HDN.
2.2 Inclusion Criteria
According to the diagnostic criteria in practical
neonatology (4th Edition) for ABO-HDN of the
newborn, the diagnosis of ABO-HDN was confirmed
based on maternal and child ABO blood type (mother
with blood type O, child with blood type A or B, and
both mother and child with Rh blood type positive),
jaundice, and positive serological tests (DAT positive
or ART positive); Received phototherapy,
intravenous human immunoglobulin therapy;
Condition improved discharge; No specific treatment
was given out of hospital.
2.3 Exclusion Criteria
(1) Combined RH hemolytic disease; (2) Preterm
infants; (3) Children discharged automatically,
unable to implement treatment normally; (4)
Readmitted children; (5) Combined G-6-PD
deficiency; (6) Combined severe neonatal asphyxia;
(7) Complicated neonatal sepsis; (8) Children with
clinical symptoms of fever; (9) Comorbid congenital
heart disease.
2.4 Research Methods
SPSS statistics 16.0 software was used for statistical
analysis. The counting data were described by the
number of cases and percentage (n, %). The
measurement data were described by mean±standard
deviation (
SX ±
), and the differences between groups
were compared by independent sample t-test, analysis
of variance and chi square test; According to the
results of correlation factor analysis, the factors with
P<0.05 were included in logistic regression analysis,
and P<0.05 was statistically significant.
3 COMPARISON OF EFFECTS
OF DIFFERENT HEMOLYSIS
TEST GROUPS ON MINIMUM
HEMOGLOBIN, AGE AT
ONSET (H) AND INCIDENCE
OF ANEMIA
In this group of 127 cases, except ART positive, other
results of hemolysis tests were DAT positive in 18
cases (14.2%) and FAT positive in 64 cases (50.4%)
(see Table 1).
According to the different results of three
serological tests of hemolysis, they were divided into
two groups. Group A: ART positive alone; Group B:
ART positive, combined with at least one hemolysis
test of FAT and DAT positive. Independent sample t-
test was used between group A and group B to
compare the differences of minimum hemoglobin and
age at onset (h), and chi square test was used to
compare the differences of anemia incidence. The
results are shown in Table 2.
The lowest hemoglobin in group B was
significantly lower than that in group A (P<0.05), the
age at onset (h) was earlier than that in group A, the
difference was statistically significant (P=0.052), and
the incidence of anemia was higher than that in group
A (P<0.05).
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
48

Table 1: Results of the three hemolysis tests in group A and
group B.
class,(n) ART
p
ositive
FAT
p
ositive
DAT
p
ositive
Group A
(
n=59
)
59 0 0
Group B
(
n=68
)
68 64 18
Table 2: The results of different hemolysis tests were
compared between the lowest hemoglobin, age (h) and
anemia.
class (n) Minimum
Hb(g/ L)
sx ±
1
Age at
disease
onset(h)
sx ±
1
Anemia
incidence2
(%)
Group A
(n=59)
147.39±
18.04
27.44±14.70 40.7%
Group B
(n=68)
130.74±
20.66
21.75±
17.53
72.1%
t value
/
χ
2value
4.80 1.97 12.73*
P value 0.000 0.052 0.000
Note: * Use the chi-square test;1 x refers to the mean, s
refers to the standard deviation; 2 The denominator of the
incidence of anaemia was 127 term ABO-HDN cases
enrolled.
4 THE INFLUENCING FACTORS
OF MODERATE AND SEVERE
ANEMIA WERE ANALYZED BY
BINARY LOGISTIC
REGRESSION
4.1 Univariate Analysis of Moderate
and Severe Anemia in ABO-HDN
A total of 127 full-term ABO-HDN cases included in
the study were subjected to univariate analysis based
on the occurrence or absence of moderate to severe
anemia, using different hemolysis serology results as
independent variables, and the relevant assignments
are presented in table 3.
Table 3: Assignment table of relevant factors.
p
roject assignment
The hemolysis test
results were grouped
Group A =1
Group B =2
Table 4: Univariate analysis of moderate and severe anemia in term infants with ABO-HDN.
project classify No moderate or
severe anemia
occurred (n=104)
Moderate and
severe anemia
occurred (n=23)
χ2value P value
Different hemolysis
test results were
grouped
Group B 49 19 9.54 0.002*
Note: * P <0.05 has statistical differences
4.2 Binary Logistic Regression
Analysis of Moderate and Severe
Anemia in ABO-HDN
Table 4 shows that group B with ART positive and at
least one positive hemolysis test result of DAT and
FAT is P= 0.002, which is statistically significant (P
< 0.05). It is included in the binary logistic regression
analysis model, P < 0.05 is statistically significant,
and the results are shown in Table 5.
The results in Table 5 showed that the incidence
of moderate to severe anemia in ABO-HDN patients
with ART positive and at least one positive for DAT
and FAT was 5.33 times higher than that of ABO-
HDN patients with ART positive alone.
Table 5: Binary logistic regression analysis of related factors of moderate and severe anemia in ABO-HDN.
analytical factor B S.E. Wals P OR OR of 95% C.I.
lower
limit
superior
limit
Hemolysis test results
group B
1.67 0.58 8.21 0.004 5.33 1.70 16.75
Clinical Case Study of ABO Hemolytic Disease in Full-term Newborns with Positive Free Test and Direct Antiglobulin Test
49
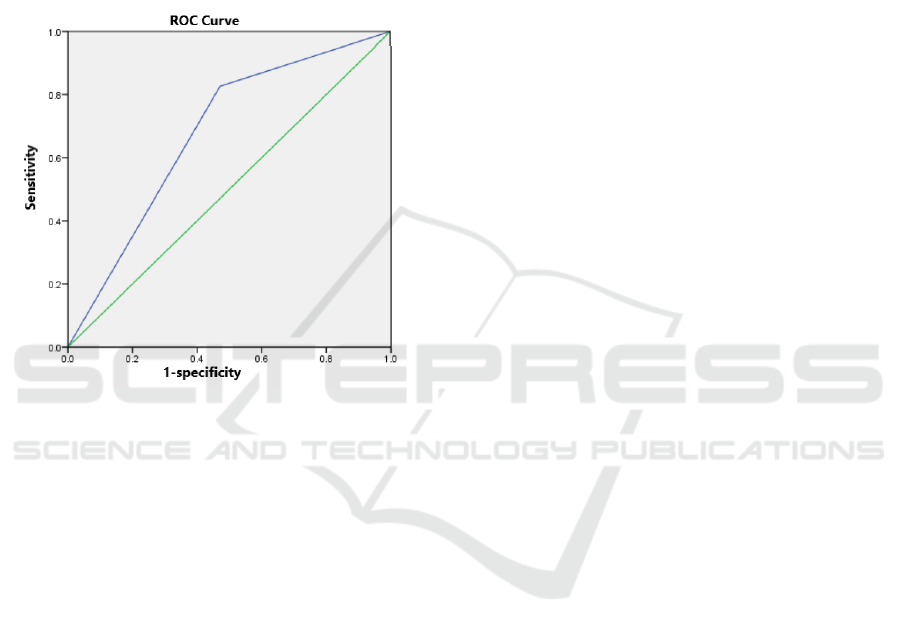
According to the results of logistic regression, the
ROC curve was drawn. With the occurrence of
moderate and severe anemia as the reference, the area
under the ROC curve (AUC) of group B was 0.677,
indicating that there was a certain reference value for
predicting the occurrence of moderate and severe
anemia according to the results of hemolysis test. The
sensitivity of clinical prediction was 82.6% and the
specificity was 52.9%. It shows that the model has a
high accuracy in predicting the occurrence of
moderate and severe anemia (see Figure 1).
Figure 1: Logistic ROC Curve of regression Model.
5 CONCLUSIONS
In this study, the results of three postpartum
hemolysis tests for term ABO-HDN were divided
into two groups, A and B, to explore whether term
ABO-HDN with different positive serological test
results (ART, FAT, DAT) had differences. The
results showed that patients with ART positive,
combined with FAT and DAT at least one hemolysis
test positive group had significantly lower lowest
hemoglobin than the ART positive group alone, and
the results were statistically significant (P<0.05). It
was significantly earlier than the cases in the ART
positive group alone, and the result was statistically
significant (P < 0.05), and the incidence of anemia
was significantly higher than that in the ART positive
group alone (P < 0.05).
In the logistic regression analysis of the risk
factors for predicting the occurrence of moderate and
severe anemia, the case group with positive ART and
at least one of DAT and FAT was positive, compared
with the ART positive group alone, the risk of
moderate and severe anemia increased by 5.33 times.
The results were statistically significant
(P<0.05).DAT is a confirmed test of neonatal ABO
hemolysis, which has a lower positive rate in ABO
than in RH hemolysis, Although FAT cannot be used
as a decisive criterion for the diagnosis of neonatal
ABO hemolysis, it can detect whether there are free
IgG antibodies in neonatal serum and indirectly
reflect the degree and persistence of ABO, which is
of guiding significance for the clinical diagnosis and
treatment of ABO-HDN and disease
progress.Clinically, children with positive ABO-
HDN combined with at least one positive DAT and
FAT should be actively treated, so as to minimize the
incidence of children complicated with anaemia,
severe hyperbilirubinemia, and bilirubin
encephalopathy.In conclusion, in full-term ABO-
HDN cases, the serological hemolysis test was
positive for ART, combined with DAT and at least
one positive case with an increased moderate and
severe risk of FAT anemia.
REFERENCES
Aydin M, Deveci U, Orman A, et al. (2016). Is the
Antiglobulin Test a Good Marker for Predicting the
Development of Hemolytic Disease of the Newborn in
ABO Incompatibility?[J].Pediatrics & Neonatology,
57(5):449-450.
Chen Zhuoyao, Deng Qiulian, Huang Yinghong, et al.
(2019). The significance of the two release tests for the
diagnosis of neonatal ABO hemolysis [J].Laboratory
Medicine and Clinical Medicine, 2019,16 (18): 2660-
2662.
Daniel. (2019).Explore the three detection methods and
clinical significance of neonatal hemolysis [J].Chinese
Guidelines, 17 (19): 119-120.
Hu Jiting, Zhang Xin. (2019).Value of umbilical cord blood
and venous blood testing in neonatal ABO hemolysis
[J].Experimental and Laboratory Medicine, 37 (03):
499-500.
Shaz BH, Hillyer CD, Gil M R. (2019). Transfusion
Medicine and Hemostasis [M].Third Edition,
Amsterdam: Elsevier, 127-130.
Shi Jingli, Ma Huimin, Zhu Weiyan, et al. (2018). Study of
direct anti-human globulin test to predict Rh blood
incompatibility [J].Chinese Journal of Health
Inspection, 28 (18): 2177-2179.
Ulrich T, Ellsworth M, Carey W. (2014).5ICCN_012:
Direct antiglobulin test as a sensitive and specific
marker for development of hemolytic disease of the
newborn in at-risk infants[J]. Early Human
Development, 90 (2):S 66-S66.
Valsami S, Politou M, Boutsikou T. (2015), et al.
Importance of Direct Antiglobulin Test (DAT) in Cord
CAIH 2021 - Conference on Artificial Intelligence and Healthcare
50

Blood: Causes of DAT (+) in a Cohort Study[J].
Pediatrics & Neonatology,56(4):256-260.
You bi jun. (2019). Role of the microcolumn gel method in
the identification of neonatal ABO blood type
[J].Journal of Clinical Rational Drug Use,12 (31): 155-
156.
Clinical Case Study of ABO Hemolytic Disease in Full-term Newborns with Positive Free Test and Direct Antiglobulin Test
51
