Inverse Reinforcement Learning for Healthcare Applications: A
Survey
Mohamed-Amine Chadi and Hajar Mousannif
LISI Laboratory, Department of Computer Sciences, Cadi Ayyad University, Marrakech, Morocco
Keywords: Inverse Reinforcement Learning, Healthcare Applications, Survey.
Abstract: Reinforcement learning (RL) is a category of algorithms in machine learning that deals mainly with learning
optimal sequential decision-making. And because the medical treatment process can be represented as a series
of interactions between doctors and patients, RL offers promising techniques for solving complex problems
in healthcare domains. However, to ensure a good performance of such applications, a reward function should
be explicitly provided beforehand, which can be either too expensive to obtain, unavailable, or non-
representative enough of the real-world situation. Inverse reinforcement learning (IRL) is the problem of
deriving the reward function of an agent, given its history of behaviour or policy. In this survey, we will
discuss the theoretical foundations of IRL techniques and the problem it solves. Then, we will provide the
state-of-the-art of current applications of IRL in healthcare specifically. Following that, we will summarize
the challenges and what makes IRL in healthcare domains so limited despite its progress in other research
areas. Finally, we shall suggest some prospective study directions for the future.
1 INTRODUCTION
In recent years, reinforcement learning (RL) (Richard
S. & Andrew G., 2017) has been very successful at
solving complex sequential decision-making
problems in different areas like video games (K. Shao
et al., 2019), financial market (Halperin, 2017),
robotics (Kober et al., 2013), healthcare domains
(Yu, Liu, & Nemati, 2019), including pathologies like
cancer, diabetes, anaemia, schizophrenia, epilepsy,
anaesthesia, and drug discovery, to mention a few.
However, for RL applications to work correctly, an
explicit reward function should be provided to specify
the objective of the treatment process that clinicians
have in mind. Manually specifying a reward function
may require prior domain knowledge. It also depends
on the clinician’s personal experience, which
undoubtedly differs across all health professionals,
thus leading to a non-representative enough reward
function of a real-world scenario or resulting in
inconsistent learning performance.
The problem of inferring a reward function from
an observed policy is known as inverse reinforcement
learning (IRL) (Russell, 1998), (Ng & Russel, 2000)
and (Pieter & Ng, 2004).
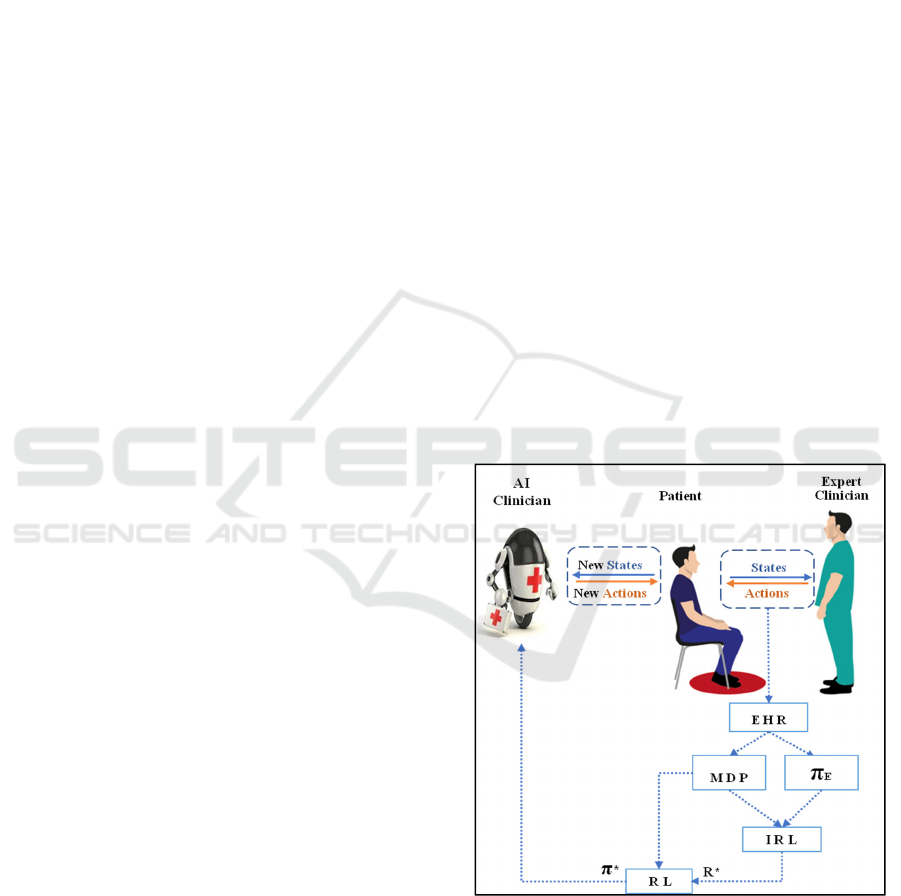
Figure 1: Global view of the RL - IRL framework in
healthcare
During this past decade or so, IRL has been
gaining a lot of attention among researchers in the
artificial intelligence communities, psychology,
control theory, and other domains. For a much
broader discussion of IRL’s progress, its theoretical
Chadi, M. and Mousannif, H.
Inverse Reinforcement Learning for Healthcare Applications: A Survey.
DOI: 10.5220/0010729200003101
In Proceedings of the 2nd International Conference on Big Data, Modelling and Machine Learning (BML 2021), pages 97-102
ISBN: 978-989-758-559-3
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
97

foundations, different algorithms, application in
various domains and its inherent challenges, one
might be referred to the work done by (Z. Shao & Er,
2012) and (Arora & Doshi, 2021).
Despite the excellent theoretical progress, one can
easily remark that there is a small amount of work
regarding IRL applications to healthcare domains,
which might be referred to many reasons, as we will
explore in the corresponding sections of this article.
In this respect, this article addresses the following
points:
An introduction to the theoretical foundations
of IRL and the problem that it solves
A state-of-the-art application of IRL in
healthcare domains
The challenges that face the applicability of
IRL in healthcare
Some potential directions for future research
Obviously, a conference article, will not cover
everything. However, we tried to make this survey as
comprehensive as possible.
2 THEORETICAL
FOUNDATIONS OF IRL
To get a proper understanding of IRL, we will
consider the most standard model, “the Markov
Decision Process (MDP)”. There are other models,
such as the partially observable Markov Decision
Process, the hidden-parameter Markov Decision
Process, which we will not go through in this article.
Unlike RL, which gets as input states of the
environment and a well-defined reward function so
that it produces the optimal behaviour that
maximizes the reward function, IRL is the exact
opposite. IRL takes in states of the environment and
information about the behaviour exercised by the
expert to output a reward function.
2.1 Definitions
A Markov Decision Process of {S, A, T, R, γ}
represents an agent's history of interactions, where:
A is the action space, = {a1, a2 . . . ak}.
S is the state space.
T is the transition function, i.e., given state S,
and executing action A. The agent will follow
T to get to another state S’.
γ is the discount factor. It is mainly used for two
goals, first is to prove the convergence of the
algorithm, second is to model the uncertainty
of the agent about the successive decision
instants.
R is the reward received when action A is
performed at state S.
π
E
is an assumedly optimal policy. In the case
of IRL, it is the behaviour performed (or
trajectories followed) by the expert.
2.2 Formulation of the IRL problem
Given rollouts of the expert’s policy π
E
, i.e.,
history of states and actions from the expert’s
interaction process with the MDP.
Identify a set of possible reward functions (R)
so that the policy π recovered from the R is (or
as near as possible as) the policy performed by
the expert π
E
for the given MDP.
Many algorithms were developed to solve this
problem since the first steps taken in 2000 by (Ng &
Russel, 2000) and (Pieter & Ng, 2004) in 2004, such
as Maximum Entropy IRL (Ziebart et al., 2008),
nonlinear representations of the reward function
using Gaussian processes (Levine et al., 2011),
Bayesian IRL (Ramachandran & Amir, 2007), and
many others as discussed in detail in (Z. Shao & Er,
2012) and (Arora & Doshi, 2021).
3 IRL FOR HEALTHCARE:
STATE-OF-THE-ART
APPLICATIONS
In most cases, IRL is just a step towards making a
more robust approach to solve a healthcare-related
decision-making problem using RL, where providing
the reward function to the RL algorithm is not trivial,
exploiting IRL techniques might be of massive
benefit in solving many issues that RL faces when
used in clinical settings, for a more detailed
discussion on the use of RL in healthcare, the survey
conducted in (Yu, Liu, & Nemati, 2019) is a good
resource.
Despite being widely used, nearly every RL
application assumes that a reward function is
provided or easy to program manually, which is often
not the case, calling for new robust ways such as IRL.
After working on modelling medical records of
diabetes as an MDP in this first article (Asoh, Shiro,
Akaho, Kamishima, et al., 2013), and utilizing the
doctors’ opinions for defining the reward for each
treatment, Asoh et al. then developed a new method
based on Bayesian-IRL to infer the reward function
that doctors were considering for the treatment
BML 2021 - INTERNATIONAL CONFERENCE ON BIG DATA, MODELLING AND MACHINE LEARNING (BML’21)
98

process (Asoh, Shiro, Akaho, & Kamishima, 2013),
in the conclusion of their work, Asoh et al. reported
that the results they have achieved thus far are
somewhat preliminary and still some difficulties that
must be addressed, such as introducing the
heterogeneity of doctors and patients using
hierarchical modelling, applying the multitasks
inverse reinforcement learning algorithm by
(Dimitrakakis & Rothkopf, 2012), extending the
MDP to POMDP which implicates a proper design of
the state and the action spaces, and finally taking into
account longer examinations histories and treatments.
Next, is the work done in (Li & Burdick, 2017)
and (Li et al., 2018) regarding clinical motion
analysis of both physicians and patients. They worked
on the problem of inverse reinforcement learning in
large state space and solved it using function
approximators approaches (e.g., a neural network)
that do not necessarily need to go through the RL
problems when learning the reward function. They
reported that the proposed approach showed more
accuracy and scalability when compared to traditional
methods. A clinical application was also presented as
a test for the proposed method, where it was applied
to evaluate robot operators according to three surgical
activities: tying knots, passing needles and suturing.
And in their later work (Li & Burdick, 2020), the
suggested technique was tested in two simulation
settings. They used ground-truth data for comparing
alternative configurations and extensions and then
applied it to a clinician skill assessment and the
analysis of a patient motion therapy.
Following the above, the authors in (Yu, Liu, &
Zhao, 2019) applied the Bayesian IRL method and
modelled the sequential decision-making problem of
a ventilator weaning as an MDP, and used a batch RL
approach, fitted-Q-iterations with a gradient boosting
decision tree, to infer an appropriate strategy from
actual trajectories in historical data in ICU. In their
results, they concluded that the IRL approach could
extract significant indications for prescribing
extubation readiness and sedative dosage. This makes
it clear that patient’s physiological stability received
greater importance by clinicians, rather than
oxygenation criteria. In addition, new successful
treatment procedures can be proposed when
determining optimum weights. They also emphasized
that although the results have confirmed the viability
of inverse reinforcement learning techniques in
complex medical environments, there are still many
concerns that must be properly addressed before these
approaches might be meaningfully applied.
In even more recent work, (Yu, Ren, & Liu, 2019)
Yu et al. proposed a new model that incorporates the
advantages of mini trees and Deep IRL. As reported
in their conclusion, this approach can adequately
address the problems of identifying factors that have
to be taken into consideration when evaluating the
decision-making performance, and the different roles
these factors can play in treating sepsis.
4 IRL FOR HEALTHCARE:
CHALLENGES
The previous section has summarized the state-of-
the-art applications of IRL in healthcare domains over
the past decade. While notable success has been
obtained, IRL applications in healthcare still manifest
some limitations. Most of these limitations are
inherent to the RL framework in general and to the
complexity of clinical data, which was exhaustively
discussed in (Yu, Liu, & Nemati, 2019) and
(Gottesman et al., 2018) and (Gottesman et al., 2019).
In the present work, however, we will concentrate on
the challenges encountered when using IRL in
healthcare and what makes the literature as limited as
we explored.
4.1 Data in Healthcare Settings
As shown in Figure 1, the primary sources of data for
an IRL algorithm in healthcare are states of the
patients and actions performed by clinicians
accordingly. Thus, the main challenge here is how to
collect useful data given that:
Patients may fail to complete the treatment
regime.
Devices in clinical settings can be changed, and
each device is subject to many inherent biases.
For some complicated diseases, clinicians are
still confronted with inconsistencies in
selecting precise data as the state in each case
(Vellido et al., 2018).
States and actions -by credit assignment-
should contain sufficient information for a
clear distinction of different patients.
States and actions must be causal, meaning
they must have either direct or indirect effects
on the task to learn or reward to achieve.
4.2 IRL for an Eventual RL
Application
Let us consider that the IRL algorithm did well and
gave us the reward function perfectly. The RL
algorithm now have two choices, either: (one) learn
using trial and error or (two) learn from another
Inverse Reinforcement Learning for Healthcare Applications: A Survey
99

policy, i.e., that of the expert clinician, also known as
the off-policy evaluation problem. Learning via
method one implicates executing the policy directly
on the patients, this is impossible because of the large
trial costs, uncontrolled treatment hazards, or just
illegal and unethical humanistic considerations.
Method two on the other hand (the off-policy
evaluation), estimates the performance of the learned
policies on retrospective data before testing them in
clinical environments. Using sepsis management as
an illustration, (Gottesman et al., 2019) discussed the
reasons that make the assessment of policies on
historical data a difficult problem, as any improper
handling of the state representation, variance of
importance-sampling-based statistical estimators, and
confounders in more ad-hoc measurements, would
result in inaccurate or even deceptive values of the
treatment quality.
4.3 the Black Box Problem
This problem, which is the lack of clear
interpretability (Lipton, 2018) is inherent to the RL
eventual application after an IRL usage. As illustrated
in figure 1, most IRL applications are just a bridge
(extracting the reward function) for an eventual RL
application, and RL algorithms take-in some input
data and directly output a policy, that is hard to
interpret. Despite the tremendous success achieved in
solving challenging problems like learning games
such as Atari and Go, autonomous driving, etc.
Adopting RL policies in medical applications might
get strong resistance given the fact that clinicians are
not expected to try any new treatment without
laborious validation accuracy, safety, and robustness.
5 POTENTIAL DIRECTIONS
FOR FUTUR RESEARCH
Since the very first introduction of IRL, a good
number of remarkable improvements have enabled it
to be integrated in more practical applications.
However, IRL applications in healthcare are still very
limited given the challenges manifested in current
IRL applications in healthcare domains discussed
above. Addressing these challenges would certainly
be of enormous benefit in improving clinical decision
making.
In this section, we will discuss some future
perspectives that we believe are among the most
important ones, mainly focusing on the following
four axes:
5.1 The Missing Data
As concluded in (Yu, Liu, & Zhao, 2019), the
learning accuracy will undoubtedly be affected by the
errors brought in by the data collection and
preprocessing phase. They proposed that IRL
methods must be able to directly work on the raw,
noisy, and incomplete data.
On the other hand, Asoh et al. believe that next
time they should consider longer histories of
examinations and treatments to introduce complex
decision-making processes of doctors (Asoh, Shiro,
Akaho, & Kamishima, 2013).
While enough available training samples are
currently scarce in many healthcare domains (e.g.,
few retrospective data for new or rare diseases).
Excellent solutions were proposed in other fields of
research that might mitigate the effect of missing data
immensely if exploited in healthcare applications, for
example, using data augmentation techniques
(Salamon & Bello, 2017) or GANs (Goodfellow et
al., 2020) to increase the number of samples. Another
solution is the application of knowledge distillation
(Hinton et al., 2015), or meta-learning (Lake et al.,
2017), or even knowledge transfer (Killian et al.,
2019) from a well-known patient to another relatively
similar patient to overcome the problem of
insufficient data.
Although it is still early, significant progress has
been made in the “small sample learning” research in
recent years (Carden & Livsey, 2017). Building on
these achievements and address the issue of IRL with
little data in healthcare domains, is a calling area for
future research.
5.2 Modelling Complex Clinical
Settings
Most of the current IRL applications in healthcare
assume that the agent operates in tiny domains with a
discrete state space, which in contrast to the
healthcare domains, that often involve continuous
multi-dimensional states and actions. Learning and
planning across such large-scale continuous models
is a great challenge.
The authors in (Yu, Liu, & Zhao, 2019) reported
that their future investigations would focus on
applying IRL methods that can estimate the reward
and the model-dynamics simultaneously (Herman et
al., 2016). Because usually, IRL methods rely on the
availability of an a precise MDP model, which is
either given or estimated from data. Asoh et al. also
faced a similar issue (Asoh, Shiro, Akaho, &
Kamishima, 2013) regarding the over simplicity of
BML 2021 - INTERNATIONAL CONFERENCE ON BIG DATA, MODELLING AND MACHINE LEARNING (BML’21)
100

MDPs in a healthcare setting. Thus, they decided that
the following works will consider some extensions of
the MDP to POMDP and introducing the
heterogeneity of doctors and patients by hierarchical
modelling.
5.3 IRL or Apprenticeship Learning
Apprenticeship learning via IRL (Pieter & Ng, 2004)
is learning a reward function using IRL from
observed behaviour and using the learned reward
function in reinforcement learning. While most
studies use IRL as a bridge for an eventual RL
application, just like in apprenticeship learning, in the
case of healthcare where safety is of paramount
importance, it might be helpful to consider using IRL
alone for the sake of extracting the reward function.
Because all it does is inferring the reward function of
presumably optimal treatment policy and extracting
information about the essential variables to consider
and recommend for clinicians. Thus, unless we can
provide a sophisticated and realistic simulation of the
healthcare setting for RL algorithms to be trained and
create interpretable RL solutions to improve the
safety, robustness, and the accuracy of learnt policies
in healthcare-domains which is currently an
unresolved topic that necessitates more research, IRL
can safely help improve clinician’s decision-making.
6 CONCLUSIONS
Inverse reinforcement learning (IRL) presents a
theoretical, and in lots of cases, a practical solution to
infer the reward function or the objective behind a
given policy. Usually, in healthcare domains, the
policy is performed by a clinician (i.e., the expert).
This paper aims to provide a brief comprehensive
survey of state-of-the-art applications of IRL
techniques in healthcare, the challenges faced, and
some potential directions for future research.
Although tremendous progress has been made in
recent years in the field of IRL in a lot of other areas,
clinical settings are uniquely critical and high risk-
sensitive, thus the limited literature regarding these
IRL applications in healthcare.
Nevertheless, IRL can be safely and efficiently
exploited to extract meaningful indicators associated
with the learned reward function. This can help to
recommend new effective treatment protocols and
therefore improving clinician’s decision making.
However, the risks of IRL in healthcare
applications is manifested highly when it is used as a
bridge for an eventual RL application where the
patient’s health is becoming between the hands of an
algorithm usually functioning as a non-interpretable
black-box making clinicians unlikely to trust it. Also,
most RL algorithms in healthcare learn either by trial
and error, which is obviously unfeasible/unethical, or
through another policy given as retrospective
treatment data, which -as we discussed- is still not
reliable enough and needs more improvement.
Finally, the hope is that more researchers from
different disciplines exploit their domain-expertise
and collaborate to produce more reliable solutions to
improve the decision-making in the healthcare
domains.
REFERENCES
Arora, S., & Doshi, P. (2021). A survey of inverse
reinforcement learning: Challenges, methods and
progress. Artificial Intelligence, 297, 103500.
https://doi.org/10.1016/j.artint.2021.103500
Asoh, H., Shiro, M., Akaho, S., & Kamishima, T. (2013).
An Application of Inverse Reinforcement Learning to
Medical Records of Diabetes. European Conference on
Machine Learning and Principles and Practice of
Knowledge Discovery in Databases (ECML/PKDD
’13), 1–8.
Asoh, H., Shiro, M., Akaho, S., Kamishima, T., Hasida, K.,
Aramaki, E., & Kohro, T. (2013). Modelling Medical
Records of Diabetes. Proceedings of the ICML2013
Workshop on Role of Ma- Chine Learning in
Transforming Healthcare, 6.
Carden, S. W., & Livsey, J. (2017). Small-sample
reinforcement learning: Improving policies using
synthetic data. Intelligent Decision Technologies,
11(2), 167–175. https://doi.org/10.3233/IDT-170285
Dimitrakakis, C., & Rothkopf, C. A. (2012). Bayesian
multitasks inverse reinforcement learning. Lecture
Notes in Computer Science (Including Subseries
Lecture Notes in Artificial Intelligence and Lecture
Notes in Bioinformatics), 7188 LNAI, 273–284.
https://doi.org/10.1007/978-3-642-29946-9_27
Goodfellow, I., Pouget-Abadie, J., Mirza, M., Xu, B.,
Warde-Farley, D., Ozair, S., Courville, A., & Bengio,
Y. (2020). Generative adversarial networks.
Communications of the ACM, 63(11), 139–144.
https://doi.org/10.1145/3422622
Gottesman, O., Johansson, F., Komorowski, M., Faisal, A.,
Sontag, D., Doshi-Velez, F., & Celi, L. A. (2019).
Guidelines for reinforcement learning in healthcare.
Nature Medicine, 25(1), 16–18.
https://doi.org/10.1038/s41591-018-0310-5
Gottesman, O., Johansson, F., Meier, J., Dent, J., Lee, D.,
Srinivasan, S., Zhang, L., Ding, Y., Wihl, D., Peng, X.,
Yao, J., Lage, I., Mosch, C., Lehman, L. H.,
Komorowski, M., Komorowski, M., Faisal, A., Celi, L.
A., Sontag, D., & Doshi-Velez, F. (2018). Evaluating
Inverse Reinforcement Learning for Healthcare Applications: A Survey
101

Reinforcement Learning Algorithms in Observational
Health Settings. 1–16. http://arxiv.org/abs/1805.12298
Halperin, I. (2017). Inverse Reinforcement Learning for
Marketing. SSRN Electronic Journal, 1–18.
https://doi.org/10.2139/ssrn.3087057
Herman, M., Gindele, T., Wagner, J., Schmitt, F., &
Burgard, W. (2016). Inverse reinforcement learning
with simultaneous estimation of rewards and dynamics.
Proceedings of the 19th International Conference on
Artificial Intelligence and Statistics, AISTATS 2016, 51,
102–110.
Hinton, G., Vinyals, O., & Dean, J. (2015). Distilling the
Knowledge in a Neural Network. 1–9.
http://arxiv.org/abs/1503.02531
Killian, T., Daulton, S., Konidaris, G., & Doshi-Velez, F.
(2019). Robust and Efficient Transfer Learning with
Hidden Parameter Markov Decision Processes.
Physiology & Behavior, 176(3), 139–148.
Kober, J., Bagnell, J. A., & Peters, J. (2013). Reinforcement
learning in robotics: A survey. International Journal of
Robotics Research, 32(11), 1238–1274.
https://doi.org/10.1177/0278364913495721
Lake, B. M., Ullman, T. D., Tenenbaum, J. B., &
Gershman, S. J. (2017). Building machines that learn
and think like people. Behavioural and Brain Sciences,
40(2012), 1–58.
https://doi.org/10.1017/S0140525X16001837
Levine, S., Popović, Z., & Koltun, V. (2011). Nonlinear
inverse reinforcement learning with Gaussian
processes. Advances in Neural Information Processing
Systems 24: 25th Annual Conference on Neural
Information Processing Systems 2011, NIPS 2011,
May.
Li, K., & Burdick, J. W. (2017). A Function Approximation
Method for Model-based High Dimensional Inverse
Reinforcement Learning.
http://arxiv.org/abs/1708.07738
Li, K., & Burdick, J. W. (2020). Human motion analysis in
medical robotics via high dimensional inverse
reinforcement learning. International Journal of
Robotics Research, 39(5), 568–585.
https://doi.org/10.1177/0278364920903104
Li, K., Rath, M., & Burdick, J. W. (2018). Inverse
Reinforcement Learning via Function Approximation
for Clinical Motion Analysis. Proceedings - IEEE
International Conference on Robotics and Automation,
December, 610–617.
https://doi.org/10.1109/ICRA.2018.8460563
Lipton, Z. C. (2018). The mythos of model interpretability.
Communications of the ACM, 61(10), 35–43.
https://doi.org/10.1145/3233231
Ng, A. Y., & Russel, S. (2000). Algorithms for Inverse
Reinforcement Learning. 0.
Pieter, A., & Ng, A. Y. (2004). Apprenticeship Learning via
Inverse Reinforcement Learning. 21 St International
Confer- Ence on Machine Learning, Banff, Canada,
2004
, 346, 1–2.
https://ai.stanford.edu/~ang/papers/icml04-
apprentice.pdf
Ramachandran, D., & Amir, E. (2007). Bayesian inverse
reinforcement learning. IJCAI International Joint
Conference on Artificial Intelligence, 2586–2591.
Richard S., S., & Andrew G., B. (2017). Reinforcement
Learning: An Introduction. In The MIT Press (Vol. 3,
Issue 9).
Russell, S. (1998). Learning agents for uncertain
environments (extended abstract). Conference on
Computational Learning Theory (COLT), 1–3.
Salamon, J., & Bello, J. P. (2017). Deep Convolutional
Neural Networks and Data Augmentation for
Environmental Sound Classification. IEEE Signal
Processing Letters, 24(3), 279–283.
https://doi.org/10.1109/LSP.2017.2657381
Shao, K., Tang, Z., Zhu, Y., Li, N., & Zhao, D. (2019). A
Survey of Deep Reinforcement Learning in Video
Games. 61573353, 1–13.
http://arxiv.org/abs/1912.10944
Shao, Z., & Er, M. J. (2012). A review of inverse
reinforcement learning theory and recent advances.
2012 IEEE Congress on Evolutionary Computation,
CEC 2012, 10–15.
https://doi.org/10.1109/CEC.2012.6256507
Vellido, A., Ribas, V., Morales, C., Ruiz Sanmartín, A., &
Ruiz Rodríguez, J. C. (2018). Machine learning in
critical care: State-of-the-art and a sepsis case study.
BioMedical Engineering Online, 17(S1), 1–18.
https://doi.org/10.1186/s12938-018-0569-2
Yu, C., Liu, J., & Nemati, S. (2019). Reinforcement
Learning in Healthcare: A Survey.
http://arxiv.org/abs/1908.08796
Yu, C., Liu, J., & Zhao, H. (2019). Inverse reinforcement
learning for intelligent mechanical ventilation and
sedative dosing in intensive care units. BMC Medical
Informatics and Decision Making, 19(Suppl 2).
https://doi.org/10.1186/s12911-019-0763-6
Yu, C., Ren, G., & Liu, J. (2019). Deep inverse
reinforcement learning for sepsis treatment. 2019 IEEE
International Conference on Healthcare Informatics,
ICHI 2019, 1–3.
https://doi.org/10.1109/ICHI.2019.8904645
Ziebart, B. D., Maas, A., Bagnell, J. A., & Dey, A. K.
(2008). Maximum entropy inverse reinforcement
learning. Proceedings of the National Conference on
Artificial Intelligence, 3(January), 1433–1438.
BML 2021 - INTERNATIONAL CONFERENCE ON BIG DATA, MODELLING AND MACHINE LEARNING (BML’21)
102
