
Functional Connectivity Assessment in Patients with Chronic-type
Tension Headaches after Applying Osteopathic Correction
A. V.
Fokin, M. L Pospelova, G. E. Trufanov, A. A. Medenikov, E. D. Vyshedkevich,
I. A. Mashchenko, T. A.
Bukkieva, D. S. Chegina, E. A. Gorbunova, T. M. Alekseeva and
A. S. Lepekhina
MRI Department, Almazov National Medical Research Centre, Akkuratova str., 2, Saint-Petersburg, Russia Federation
Keywords: Chronic Tension-type Headache, Osteopathic Correction, Functional MRI at Rest, Connectome.
Abstract: Clinical and neuroimaging comparison of the dynamics of changes in the pain connectome against the
background of osteopathic correction in patients with chronic tension-type headaches. We examined 24
patients with chronic tension type headaches, aged 24 to 43 years. Patients underwent resting-state functional
MRI before and after first osteopathic manipulation. Complaints were evaluated and patients were surveyed
to assess the intensity of headache and its impact on different areas of life, quality of life, situational and
personal anxiety before and after therapy. Changes in the functional connectivity of the in patients with tension
headaches after osteopathic manipulation were found to correlate with a positive clinical picture. Changes in
the functional connections of the medial prefrontal cortex with other areas of the brain were detected in
patients with chronic tension-type headaches when using a single osteopathic correction. There was an
improvement in the condition of patients both in the subjective assessment of complaints and in the objective
assessment of their condition on scales. The use of methods for statistical analysis of neuroimaging data, in
particular resting-state functiontional MRI, made it possible to see the differences objectively by mapping
different colors using color scales, which greatly simplifies the entire analytical process. Clinical and
neuroimaging comparison of the dynamics of changes in the pain connectome against the background of
osteopathic correction in patients with chronic tension-type headaches provides potentially new approaches
to the diagnosis and treatment of pain syndrome.
ABBREVIATIONS
DMN – default mode nerwork
CTTH – chronic tension-type headache
FC – functional connectivity
MPFC – medial prefrontal cortex
TTH – tension-type headache
1 INTRODUCTION
Among all types of headaches, the leading role
belongs to tension-type headache (TTH), the
prevalence of which among the population is up to
45-64%, while chronic tension-type headache
(CTTH) accounts for 1,7–4% (Mathew, 2006;
Jensen,
2008). CTTH is a serious medical and social problem
that leads to a decrease in the working capacity and
quality of life of patients. It is proved that the
etiopathogenesis of TTH involves extensive neural
networks that can extend beyond the somatosensory
system (central divisions) (Filatova, 2020). It should
be noted that in the treatment of tension-type
headaches, there is an excessive use of medications.
That is why the approach based on non-drug methods
of influence seems to be relevant.
One of the promising methods of non-drug
correction of tension headaches is osteopathic
correction. There are studies that show a decrease in
Fokin, A., Pospelova, M., Trufanov, G., Medenikov, A., Vyshedkevich, E., Mashchenko, I., Bukkieva, T., Chegina, D., Gorbunova, E., Alekseeva, T. and Lepekhina, A.
Functional Connectivity Assessment in Patients with Chronic-type Tension Headaches after Applying Osteopathic Correction.
DOI: 10.5220/0010390702490254
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 1: BIODEVICES, pages 249-254
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
249

pain sensitivity and pain intensity after treatment
using osteopathic techniques (Bredikhin, 2015;
Miroshnichenko, 2017).
One of the serious problems of modern Algology
is the objectification of pain intensity and the
effectiveness of analgesic treatment. In addition to
subjective assessment using pain scales with low
validity, attempts are being made to develop methods
for objectively measuring the intensity of tension
headaches during treatment – by determining the
concentration of serotonin in the blood plasma of
patients or by studying the latency of P300, but these
approaches are difficult to reproduce and also have
low validity (Rachin, 2005). The most objective and
valid analysis of connections between different areas
of the brain and the assessment of neural networks is
possible using resting-state functional MRI, which is
used to evaluate the effectiveness of evidence-based
medicine methods.
Currently, the issue is devoted to the study of
neuroplasticity in patients with CTTH during the use
of osteopathic correction, and objectively proved the
effectiveness of this method remains poorly
understood. Determining changes in functional
relationships is promising in forming a new view of
the etiology and pathogenesis of CTTH and makes it
possible to develop effective tactics for treating
patients (Patil,2017; Jutzeler, 2015; Baliki 2014,
Lepekhina, 2020).
2 PURPOSE
Сonnectome study in patients with chronic-type
tension headaches with the use of osteopathic
correction.
3 MATERIALS AND METHODS
3.1 Study Population
An open, single-center, uncontrolled study of the
connectome condition was conducted in patients with
tension headaches during a course of treatment with
osteopathic methods.
We observed 24 patients (aged from 24 to 43
years, age - 33±0.5 years) with CTTH, duration of the
disease from 1 year to 18 years (duration - 4.4±0.7 g).
Other causes of headache were excluded.
The diagnosis of CTTH was based on anamnesis
and complaints. All patients complained of
paroxysmal and / or persistent headaches of one - or
two-sided localization of aching (41%), pulsating
character of weak (23%) and moderate intensity
(36%). Headaches were more often of two-sided
localization, were of a pressing/compressing/ non-
pulsating nature, lasting from 60 minutes to several
days, of mild or moderate intensity, which did not
increase with normal physical activity, and were not
accompanied by nausea and vomiting. Patients
reported headache more than 15 days a month, for the
last 6 months. The study was approved by the ethics
committee of the Federal State Budgetary Institution
«National Medical Research Center n.a. V.A.
Almazova» of the Ministry of Health of Russia
(extract from the protocol No. 41 of 02/12/2018).
Criteria for exclusion of patients from the study
were: 1. The presence of a history of psycho-organic
pathology, epilepsy, brain tumors, injuries of the
brain and spinal cord. 2. The presence of severe
concomitant pathology (exacerbation of rheumatism,
acute infections, cirrhosis, alcoholism, drug
addiction, cardiomyopathy with thromboembolism in
the arteries of the brain, acute myocardial infarction,
heart failure 3-4 severity, blood diseases). 3. The
simultaneous administration of drugs that can distort
the results of treatment (anxiolytics, antidepressants,
barbiturates, lithium preparations, narcotic
analgesics, reserpine).
3.2 MR Imaging Protocol
All patients underwent structural MRI with obtaining
T1 and T2 weighted images and FLAIR (Fluid
attenuated inversion) to exclude brain tumors, strokes
and other pronounced pathological changes. All
patients underwent functional resting state MRI at 3
time points – before and after 10 minutes after
applying the first osteopathic technique. Pulse
sequence data of a T1-weighted gradient echo (MP-
RAGE – Magnetization Prepared Rapid Acquired
Gradient Echoes) was collected to combine fMRI
data with anatomical structures of the brain, slice
thickness – 4.5 mm, number of slices – 29, the
number of repetitions – 120, scan time – 6 minutes.
The main feature of this sequence is its high
resolution and 0.8 mm isotropic voxel. BOLD (Blood
Oxygenation Level Dependent) were using with
repetition time (TR) = 3000 ms, echo time (TE) = 50
ms, field of view (FOV) = 230 mm and matrix size
128*128, slice thickness – 4.0 mm, the number of
repetitions – 120, scan time – 6 minutes.
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
250
3.3 Image Analyses
Analyzing the data of functional MRI, when
performing an intergroup statistical analysis (two-
sample t-test, comparing the resting state before
treatment and after osteopathic correction) with the
choice of the medial prefrontal cortex (MPFC) as the
region of interest.
3.4 Statistical Analyses
For statistical analysis, the non-parametric McNemar
test for dependent binary indicators was used.
Statistical processing and evaluation of the results of
neuroimaging studies of each patient individually, as
well as their group totality (resting state fMRI data)
were carried out using the CONN v.18 software
package (Functional connectivity toolbox), designed
to determine the relationships between different parts
of the brain, statistical mapping of activation zones,
determining the structure of various resting state
networks and functional networks of the brain.
3.5 Results
According to the results of the study, after the use of
osteopathic manipulations according to resting-state
fMRI data, changes in the functional connectivity
(FC) were observed. When performing osteopathic
correction, there is a functional reorganization of
neural networks involving, first of all, of default
mode network (DMN). The choice of the medial
prefrontal cortex (MPFC) as a region of interest in the
study is due to its importance as one of the central
links in the DMN.
When selecting the MPFC as the region of interest
in the right hemisphere, the positive functional
connection with the right parahippocampal gyrus was
determined to be enhanced. In the left hemisphere,
there was an increase in the positive FC with the
putamen and a decrease in the negative FC with the
upper left parietal region.
Functional MRI data were obtained when
comparing the state at rest before and immediately
after 10 minutes following osteopathic manipulation:
when performing an intergroup statistical analysis
(p<0.005) (two-sample t-test, seed-to-voxel), the
result of an intergroup comparison is presented,
which demonstrates changes in activity (table 1).
Table 1: The degree of activations severity before and after
10 minutes following osteopathic manipulation. Region of
interest - the medial prefrontal cortex.
ROI Statistical indicator, T
The upper parietal
region, left
-3.13
Parahippocampal
gy
rus, ri
g
ht
2.43
Putamen -2.16
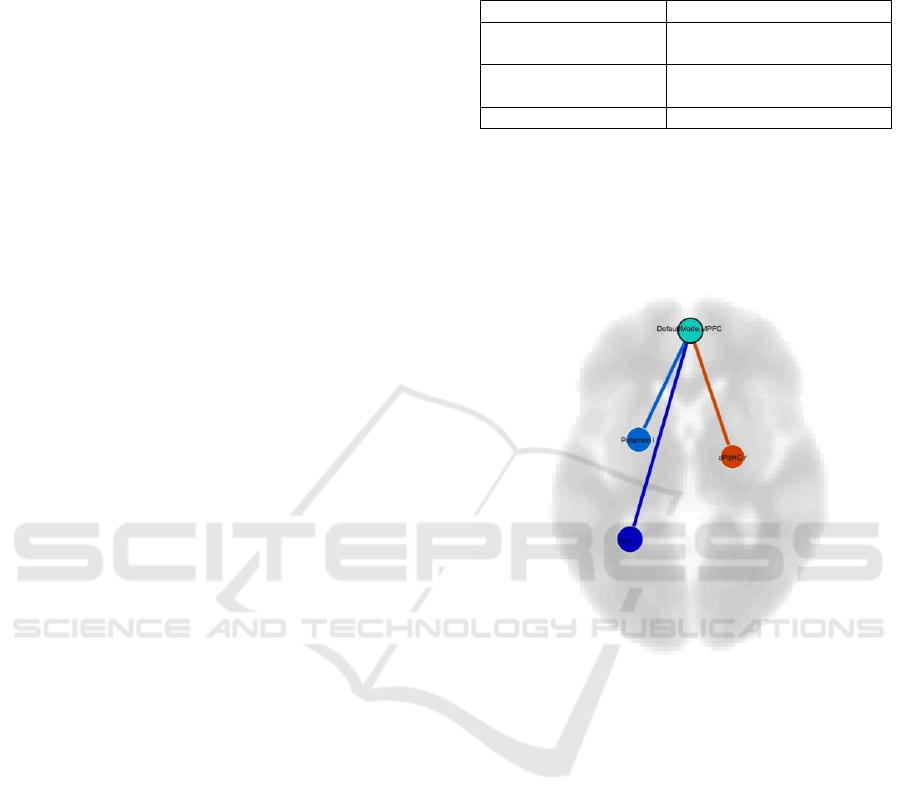
Schematic representation of data from the
intergroup analysis: shows how MPFC is related to
other areas of the study, where more pronounced
activity is observed in the parahippocampal gyrus,
and a decrease in activity in the upper parietal region
and the putamen (Fig. 1).
Figure 1: The results of the intergroup analysis of resting-
state functional MRI, before and after 10 minutes following
osteopathic manipulation. Schematic data.
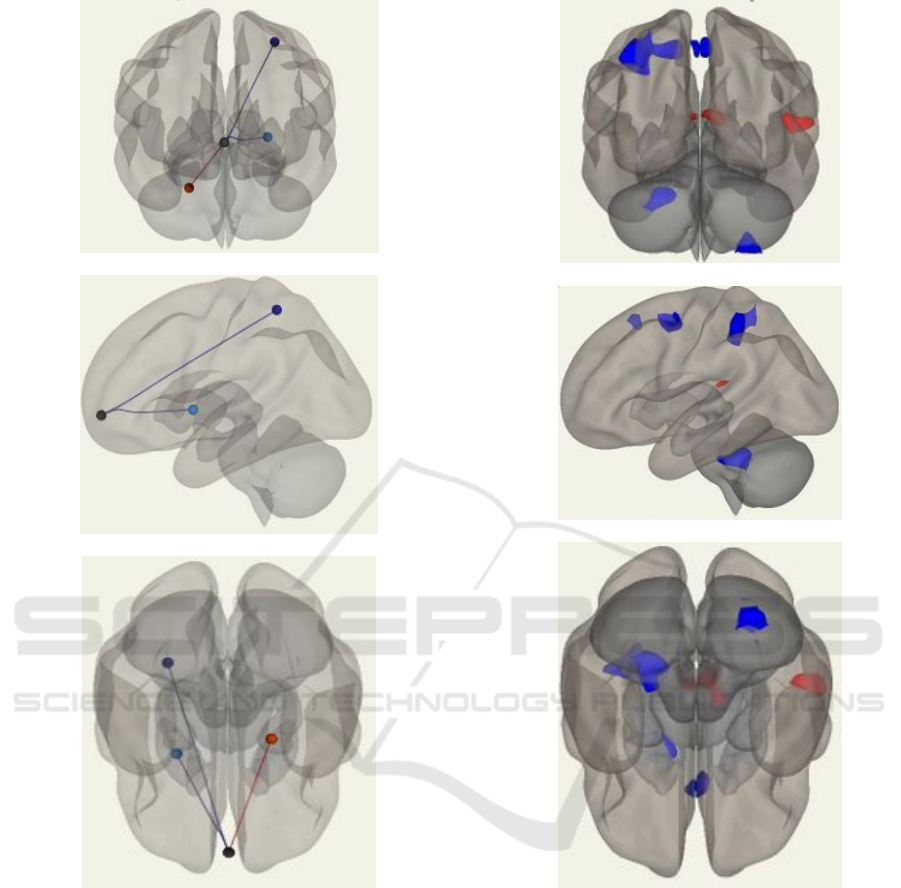
For the most convenient visualization, we
combined fMRI data with anatomical structures of the
brain T1-weighted gradient echo MP-RAGE
(Magnetization Prepared Rapid Acquired Gradient
Echoes-gradient echo with magnetization preparation
and rapid data collection) (Fig. 2, 3). When selecting
the MPFC as the zone of interest in the right
hemisphere, the positive FC with the right
parahippocampal gyrus was determined to be
enhanced. In the left hemisphere, there was an
increase in the positive FC with the putamen and a
decrease in the negative FC with the upper left
parietal region.
Functional Connectivity Assessment in Patients with Chronic-type Tension Headaches after Applying Osteopathic Correction
251
a
b
c
Figure 2: (a - axial, b - sagittal, c - coronal). The results of
the inter-group analysis of the resting-state functional MRI
(roi-to-roi). 3-D reconstruction. Region of interest: MPFC.
The red color indicates a positive FC, and the blue color
indicates a negative FC.
a
b
c
Figure 3: (a - axial, b - sagittal, c - coronal). The results of
the inter-group analysis of the resting-state functional MRI
(seed-to-voxel). 3-D reconstruction. Region of interest:
MPFC. The red color indicates a positive FC, and the blue
color indicates a negative FC.
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
252

The study was the first to identify changes in the
FC of the brain after a single procedure of osteopathic
correction in patients with CTTH. The use of methods
for statistical analysis of neuroimaging data, in
particular resting-state fMRI, made it possible to see
the differences objectively by mapping different
colors, which greatly simplified the entire analytical
process.
There were no adverse reactions due to
osteopathic correction, as well as deterioration of the
condition of patients with CTTH during the
treatment.
The possibilities of modern visualization methods
expand the understanding of the mechanisms of
neurological diseases by studying connectome of the
brain. Using resting-state fMRI allows you to
objectively assess neuronal activity and study
changes in CTTH.
When performing osteopathic manipulations, the
functional reorganization of neural networks occurs
with the involvement of the network of the DMN. The
study examined changes in the FC of the medial
prefrontal cortex with other parts of the brain. The
choice of the medial prefrontal cortex as a region of
interest in the study is due to its importance as one of
the central links in the DMN. The MPFC connects
large areas that include the orbitofrontal cortex and
structures such as the central gray matter of the
midbrain, amygdala, and hypothalamus, while
playing an important connecting role in transmitting
somatosensory information to structures that are
responsible for motor and visceral responses,
participating in the internal reward system and
responsible for decision-making. According to recent
data, the parahippocampal gyrus is an intermediate
link in the DMN, which connects the MPFC with the
limbic system, and participates in the processes of the
internal reward and memory system (Ward, 2014).
The increase in the positive FC of MPFC with the
parahippocampal gyrus in the right hemisphere in
patients with CTTH after performing osteopathic
manipulation revealed in our study may indicate
activation of the functional pathway associated with
a positive emotional response in the reward system.
In the left hemisphere, there was a weakening of
the negative FC with the upper left parietal region and
an increase in the positive FC with the putamen. The
upper parietal cortex is part of the vast preclinical
zone, which, along with the MPFC, is one of the
important links in the DMN, which are involved in
the processing of sensory-motor signals and attention.
Changes in the FC between the upper parietal region
and the MPFC may indicate a decrease in activity in
this area DMN. The putamen is a subcortical structure
that belongs to the significance determination
network, and the strengthening of links between this
area and the MPFC may indicate activation of DMN.
So, changes in the FC of the MPFC with other
areas of the brain were detected when applying a
single osteopathic correction in patients with CTTH.
4 CONCLUSIONS
To date, the number of full-fledged studies on
changes in the FC of the brain in patients with CTTH
is limited, which makes this area even more relevant.
The current study showed the importance of
evaluating the FC that ensure the interaction of brain
structures. Changes in the FC of the DMN were
identified in patients with CTTH after the use of
osteopathic correction, which require further study.
The results of the study of FC of the brain in patients
with CTTH expand the understanding of the
pathogenesis of this type of headache and improve the
treatment regimens used in patients.
CONFLICT OF INTERESTS
The authors declare no conflict of interest
REFERENCES
Bredikhin A.V., Bredikhin K.A., Chekha O.A. Headache as
a dysfunction of cranial sutures. Medical news. 2015;
11 (254): 23-27 (in Russian).
Baliki M.N., Mansour A.R., Baria A.T., Apkarian A.V.
Functional reorganization of the default mode network
across chronic pain conditions. PLoS One. 2014; 9 (9):
e106133. DOI: 10.1371/journal.pone.0106133
Jensen R, Stovner LJ. Epidemiology and comorbidity of
headache. Lancet Neurol. 2008; 7: 354–361. DOI:
10.1016/S1474-4422(08)70062-0
Filatova E.G., Merkulova D.M. Tension-type headache as
most frequent and often erroneous diagnosis. Medical
alphabet. 2020; 1 (11): 5-9 (in Russian). DOI:
10.33667/2078-5631-2020-11-5-9
Jutzeler C.R., Curt A., Kramer J.L. Relationship between
chronic pain and brain reorganization after
deafferentation: A systematic review of functional MRI
findings. Neuroimage Clin. 2015; 9: 599‐606. DOI:
10.1016/j.nicl.2015.09.018
Koreshin, E., Efimtsev, A.Yu, Gulko, A., Popov, S., Orlov,
I., Trufanov, G., Zubkov, M. Design of a RF-resonant
set improving locally the B1+ efficiency. Applications
for clinical MRI in andrology and urology. Journal of
Functional Connectivity Assessment in Patients with Chronic-type Tension Headaches after Applying Osteopathic Correction
253

Magnetic Resonance, 2020, 317, 106774 DOI:
10.1016/j.jmr.2020.106774
Lepekhina A.S., Efimtsev A.Y., Pospelova M.L., et al.
Possibilities of neuroimaging when using non-drug
therapies in patients with tension headaches. Modern
problems of science and education. 2020; 4: 616-857
(in Russian). DOI: 10.17513/spno.29984
Mathew N.T. The prophylactic treatment of chronic daily
headache. Headache. 2006; 46 (10): 1552‐1564. DOI:
10.1111/j.1526-4610.2006.00621.x
Miroshnichenko D.B., Rachin A.P., Mokhov D.E.
Osteopathic algorithm of treatment for chronic tension
headaches. Practical medicine. 2017; 1 (102): 114-118
(in Russian).
Patil U.D. Role of functional MRI in identifying network
changes in chronic pain syn-dromes. Neurol India.
2017; 65 (2): 255‐256. DOI: 10.4103/0028-
3886.201853
Petrenko, T.S., Kublanov, V.S., Retyunskiy, K., Dolganov,
A., Efimtcev, A. The effect of multichannel
electrostimulation of neck nervous structures on the
brain connectivity of patients with depressive disorders
(2020) Zhurnal Nevrologii i Psihiatrii imeni S.S.
Korsakova, 120 (1), pp. 51-54. DOI:
10.17116/jnevro202012001151
Shamrey, V., Odinak, M., Trufanov, G., Abritalin, E.,
Litvintsev, B., Goncharenko, A., Tarumov, D.,
Korzenev, A., Fokin, A., Boykov, I., Efimtsev, A.
Neuroimaging diagnosis of depressive and addictive
disorders (2016) Psychiatry, Psychotherapy and
Clinical Psychology, 7 (1), pp. 30-40.
Trufanov, A.G., Litvinenko, I.V., Yurin, A.A., Trufanov,
G.E., Buriak, A.B. Modern possibilities of magnetic
resonance imaging in the diagnosis of parkinsonian
syndrome (2018) Russian Electronic Journal of
Radiology, 8 (1), pp. 52-65. DOI: 10.21569/2222-7415-
2018-8-1-52-65
Rachin A.P., Sergeev A.V., Yudelson Ya.B. Method for
determining the intensity of tension headache. Pat. RU
2311121 Russian Federation: IPC A61B 5/0484.
Ward A.M., Schultz A.P., Huijbers W., Van Dijk K.R.,
Hedden T., Sperling R.A. The parahippo-campal gyrus
links the default-mode cortical network with the medial
temporal lobe memory system. Hum Brain Mapp. 2014;
35 (3): 1061‐1073. DOI: 10.1002/hbm.22234
NDNSNT 2021 - Special Session on Non-invasive Diagnosis and Neuro-stimulation in Neurorehabilitation Tasks
254
