
Matching of Mechanical Properties of Biological Tissues and
Technical Materials for the Fabrication of Anatomical Models by
Material Jetting
Alexander Preis
a
, Hannah Riedle
b
, Elisabeth Benke
c
and Jörg Franke
d
Institute for Factory Automation and Production Systems, Friedrich-Alexander-Universität Erlangen-Nürnberg,
Egerlandstraße 7-9, Erlangen, Germany
Keywords: Surgical Models, Anatomical Models, Surgical Training, Medical Education, Medical Device Evaluation,
Biomechanics, Biomechanical Testing, Additive Manufacturing, 3D Printing, Material Jetting,
Standardization.
Abstract: Realistic, high-fidelity anatomical models with material properties corresponding to those of human tissue
can be used for surgical planning and training, medical education and medical device testing and validation.
Conventional manufacturing of anatomical models is a time consuming, and expensive process, which
nevertheless is not able to fully mimic the complex nature of the human body regarding geometry and
mechanical properties. To create models closer to reality in a fast and cost-effective way, additive
manufacturing, especially the process of material jetting, can be a solution. Utilizing this process, it is possible
to fabricate multi-color, multi-material objects with complex geometries, high resolution, and even gradients
in material properties. To replicate the mechanical properties of biological tissues, they must be matched with
the technical materials or material combinations available for the utilized manufacturing process. Therefore
the authors propose to conduct measurements according to standardized testing procedures like ISO 37 for
tensile and ISO 48-4 for indentation tests, which allows matching to the manufacturing materials and thus
will result in the possibility to create more accurate replicas of the human body that provide realistic haptic
feedback.
1 INTRODUCTION
Anatomical models provide benefits in a multitude of
different fields. In preoperative planning, they
support the familiarization with the patient’s specific
anatomy and provide a hands-on approach of testing
different surgical strategies. Especially in physicians
specialties which require very delicate surgical
procedures, the annual likeliness of a malpractice
claim can be up to 19 % (Anupam et al., 2011), which
shows that accurate planning and preparation is
critical to avoid mistakes during surgery. Here the
field of reconstructive surgery is a good example,
where, for optimal results in the recreation of
appearance and healing of functional losses, a deep
a
https://orcid.org/0000-0003-3469-5982
b
https://orcid.org/0000-0003-1338-2127
c
https://orcid.org/0000-0002-6610-4430
d
https://orcid.org/0000-0003-0700-2028
knowledge of the pathology is needed, which can be
aided by a realistic and tangible representation of the
situation (Chae et al., 2015). Detailed models can be
used to show the planned procedure to the patient,
explain the difficulties and thus support patient
education and informed consent. They even can
support the physician during surgery by providing
information regarding orientation. (Malik et al., 2015)
All of this leads to a reduced duration of the surgery,
less trauma to the patient and overall better results
(Chae et al., 2015). The use of anatomical models can
also aid the understanding of the human body in
general by conducting research activities on additive
manufactured anatomical structures (Birkholz et al.,
2020).
Preis, A., Riedle, H., Benke, E. and Franke, J.
Matching of Mechanical Properties of Biological Tissues and Technical Materials for the Fabrication of Anatomical Models by Material Jetting.
DOI: 10.5220/0010384201890194
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 1: BIODEVICES, pages 189-194
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
189
Studies have shown that additively manufactured
anatomical models are able to represent the human
anatomy and pathologies realistic enough to be used
in medical education (Riedle et al., 2019). Training
by using high fidelity anatomical models providing
haptic feedback was shown to result in a better
performance and more profound understanding than
conventional methods like educational texts, 2D
images, or virtual 3D models (AlAli et al., 2018)
(Ström et al., 2006). Since the use of cadaveric
materials or animal tissue for the teaching of
anatomics has been a controversy regarding ethics
and health since its introduction, issues can be
avoided by using artificial, but realistic
representations of the human body (McMenamin et
al., 2014).
Another important use of anatomical models is
the testing and validation of medical devices. Such a
mock-up does not always have to replicate the
complete anatomy or all the physiological properties
of the intended usage environment (Yoo et al., 2020).
However, often good representation of the anatomy
as well as the mechanical properties is needed to
conduct meaningful research (Sulaiman et al., 2008).
Conventional manufacturing of individual, high-
fidelity anatomical models is a time consuming, and
expensive process, which nevertheless is not able to
fully mimic the complex nature of the human body
regarding geometry and diversity of mechanical
properties. This problem can be solved by additive
manufacturing, which allows the creation of highly
complex geometries utilizing multiple materials.
(Maragiannis et al., 2015)
2 POSSIBLE PROCESSES FOR
ADDITIVE MANUFACTURING
The process of additive manufacturing was first
presented by Chuck Hull in a 1984 patent. The
presented process of stereolithography is a form of
vat photopolymerization, where the resin is
selectively cured by using a laser scanner (Hull,
1984). Generally speaking, additive manufacturing is
a process where material is, in contrast to subtractive
manufacturing, automatically added, mostly as
layers, to create a physical object based on 3D-data
(DIN EN ISO/ASTM 52900). Important key facts of
the process are:
The geometry is based on 3D-CAD data.
No product specific tools are needed.
No need for fixation of the product.
Complex geometries, like undercuts, can be
manufactured effortlessly. (Gebhardt, 2016)
DIN EN ISO 17296-2 defines the seven different
additive manufacturing processes binder jetting,
directed energy deposition, material extrusion,
material jetting, powder bed fusion, sheet lamination,
and vat photopolymerization, which are described
more closely in table 1. Additionally, the processes
can be differentiated according to the aggregate state
of the raw material into generation from the solid,
liquid or gas phase (Gebhardt, 2016).
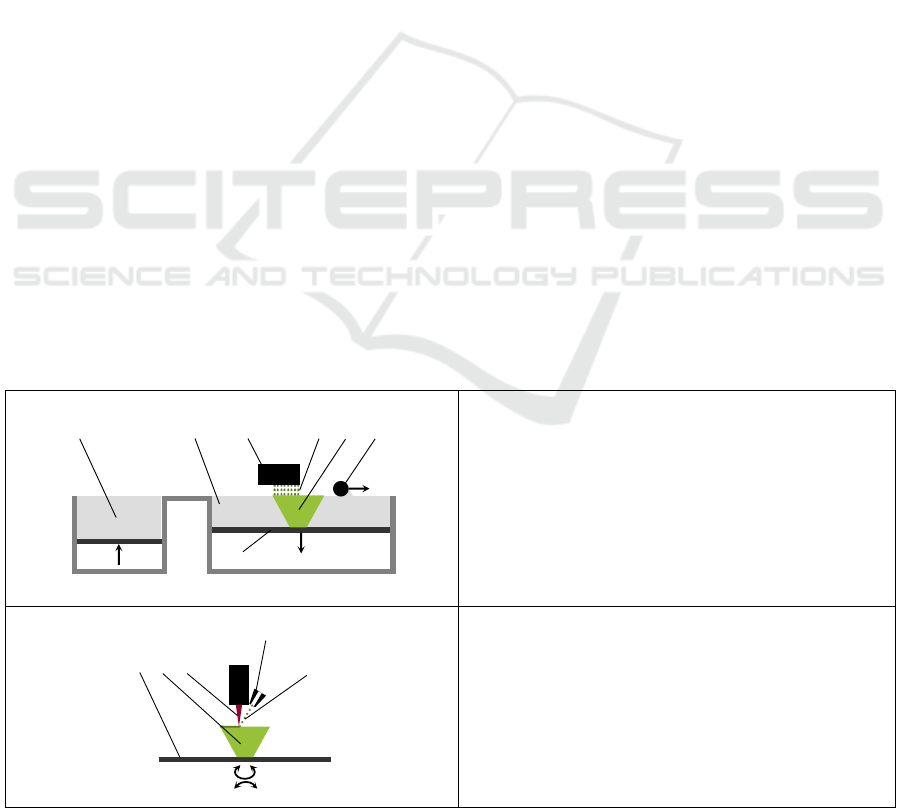
Table 1: Additive manufacturing processes according to DIN EN ISO 17296-2 and Gebhardt et al. 2016.
Binder Jetting
Binder jetting is a process, where a liquid (4) binder is
applied by a print head (3) to selectively bond powdered
raw material (2). New layers of material are added by a
roller (6) out of the material reservoir (1), which is made
possible by lowering the build platform (7). The process
often consists two steps, where the additive manufacturing
is creating a green body (5) which afterwards is infiltrated
or cured. By using different binder colors, a multi-color,
single-material part can be fabricated.
Directed Energy Deposition
Directed energy deposition uses a directed energy beam
(3) to bond the raw material (5), often jetted through a
nozzle (4), via melting to the product (2). The process is
mostly used for the creation of metal parts and often does
not depend on support structures due to the possibility of
5-axis movement of the build platform (1). By using
different raw materials, multi-material or gradient parts
can be fabricated.
23 456
7
1
1
2 3
4
5
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
190
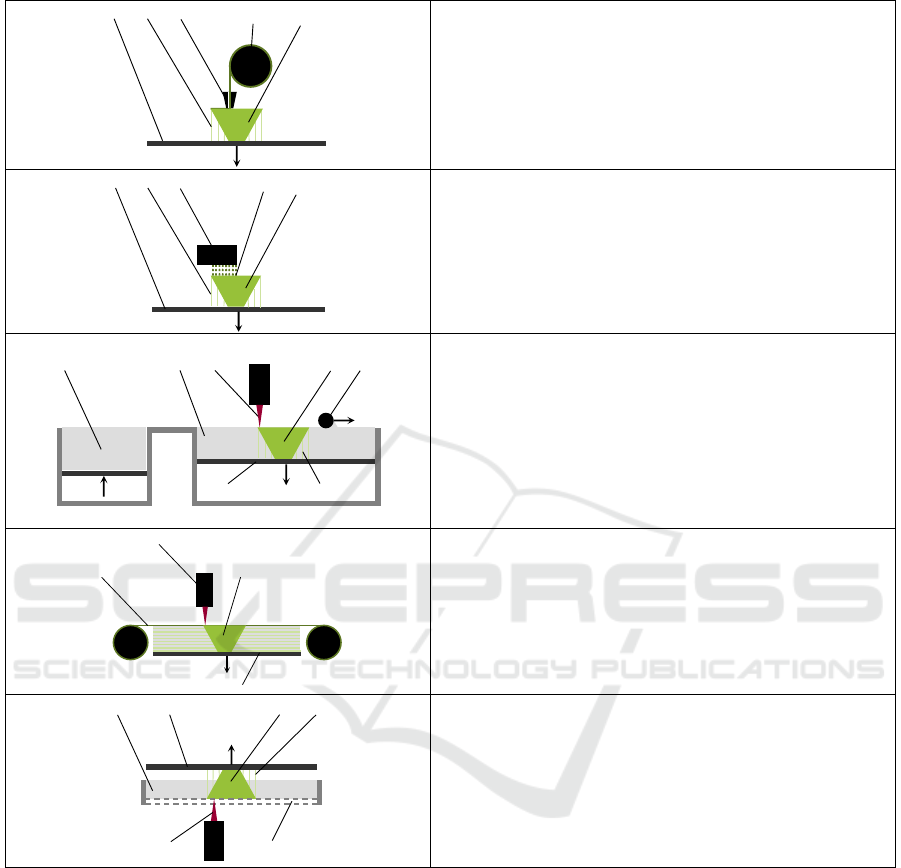
Table 1: Additive manufacturing processes according to DIN EN ISO 17296-2 and Gebhardt et al. 2016 (cont.).
Material Extrusion
One of the most known processes is material extrusion, where
the raw material (4) is extruded through a nozzle (3). Layers
are created by lowering the build platform (1) or raising the
nozzle. Products (5) with complex geometries depend on
support structures (2). By using different raw materials, multi-
material and multi-color parts can be fabricated.
Material Jetting
In material jetting the print head (3) deposits the raw material
(4) in form of droplets. The layers mostly are created by
lowering the build platform (1). For the fabrication of the
product (5), support structures (2) are required most of the
time. Due to the voxel-based approach, multi-material, multi-
color, and gradient parts can be fabricated.
Powder Bed Fusion
Powder bed fusion uses thermal energy (3) to selectively bond
powdered raw material (2) by melting or sintering. New layers
of material are added by a roller (5) out of the material
reservoir (1), which is made possible by lowering the build
platform (6). Depending on the material used, support
structures (7) can be necessary for heat dissipation to prevent
the product (4) from deforming. Only single material parts can
be fabricated.
Sheet Lamination
Using sheet lamination, the three-dimensional part (3) is
created by bonding sheets of material (1). Here a thermal
energy source (2) can be used, but also a separated system
consisting of a cutter and a lamination tool are common. The
layers are created by lowering of the build platform (4). By
coloring the sheets, multi-color parts can be fabricated.
Vat Photopolymerization
In the process of vat photopolymerization, a liquid
photopolymer (1) is selectively cured inside a vat by a light
source (5), often through a transparent bottom (6) of the vat.
Layers can be created by raising the build platform (2) out of
the photopolymer. Single material parts (3) can be fabricated,
depending on support structures (4) for complex geometries.
3 ADDITIVE MANUFACTURING
OF ANATOMICAL MODELS
For the creation of anatomical models, a wide variety
of direct or indirect additive manufacturing processes
has been used so far with varying degrees of success
(AlAli et al., 2015). To generate high fidelity replicas
of the human anatomy with a realistic haptic behavior
that can possibly be used to replace human or animal
tissue for medical education, surgical training, and
medical device testing, a suitable manufacturing
process is needed. Based on the specifics of the
structure of biological tissues (Fung, 1993), certain
requirements can be derived:
High resolution
Ability to create complex geometries
Ability to replicate different tissues
Ability to manufacture gradients and create
anisotropic material properties
To achieve these, material jetting is the best-
suited process. Because of the voxel-based approach
and multi-material capabilities of typical machines
utilizing this approach (stratasys, 2020), gradients
1 2
3
4
5
1 2
3
4
5
23 45
6
1
7
2
3
4
1
2
34
6
1
5
Matching of Mechanical Properties of Biological Tissues and Technical Materials for the Fabrication of Anatomical Models by Material
Jetting
191
and anisotropic materials can be manufactured.
Additionally, the process has a high resolution and
can create complex geometries using water-soluble
support materials, which allows the removal from
areas inaccessible to conventional tools. The selection
of the proper materials or material mixtures to
accurately resemble the mechanical properties of the
corresponding human tissue is one of the most
important points in the creation of realistic high-
fidelity anatomical models.
4 MATCHING OF BIOLOGICAL
AND TECHNICAL MATERIALS
To be able to match a material or material
combination to the corresponding tissue, the
mechanical properties of that tissue must be known
and be comparable to the technical materials
available. When it comes to mechanical
characterization of tissue, especially soft tissue like
muscle, tendons, ligaments, internal organs, and
vascular tissue, researchers face special challenges. A
lot of the times the desired tissue cannot be isolated
for testing, the size of the specimen is too small for
regular characterization procedures and it is difficult
to keep the tissue in physiological condition. In
addition, soft tissues show nonlinear, history
dependent stress-strain relations, and large
deformations, which leads to complex constitutive
equations. (Fung, 1993) The tissue properties vary
largely depending on sex and age, harvesting site,
pathophysiological condition, environmental and
physical testing conditions, temperature and time
since extraction (Mattei et al., 2016).
To fully be able to predict the mechanical
behavior of these materials, a multitude of different
testing procedures like uniaxial tension tests, uniaxial
ring tests, planar biaxial tests, inflation tests, whole-
body measurements, membrane bulge tests, and many
more where developed (Macrae et al., 2016).
However, it has been shown, that complex testing
protocols are probably not necessary for the
acquisition of mechanical data with the intention to
match a tissue to a technical material. The well-
established process of preconditioning biological
tissues before mechanical characterization might not
be suitable for the creation of anatomical models as
the behavior of human tissue during surgery does not
correspond to a preconditioned state (Cotin et al.,
2004). It also was shown that a long relaxation time
between loads "resets" the materials behavior to pre-
preconditioning state (Sacks, 2000). Because of this,
it is recommended to characterize the mechanical
properties of the tissues using industry standard
testing procedures for technical materials to get
matchable parameters (Riedle et al., 2018). Here
especially the measurement of the stress-strain
relation using tensile tests and the measurement of the
tissues hardness using indentation tests will deliver
meaningful results (McKee et al., 2011) and allow the
comparison to technical materials usable for additive
manufacturing ( Riedle et al., 2019).
5 HOW TO CREATE REALISTIC
ANATOMICAL MODELS
As shown in the previous sections, the demand for
realistic and high-fidelity anatomical models utilizing
different materials to replicate the complex tissue
structures of the human body is high. Currently the
most promising way to achieve this in a fast and cost-
effective manner is the fabrication by additive
manufacturing. Here especially the material jetting
process is a good choice, since it has a high resolution
and can utilize multiple materials, which allows the
production of multi-color and multi-material models.
Even gradients of material properties can be
produced. The ability to use soluble support
structures makes the creation of complex geometries,
like those occurring in anatomy, possible.
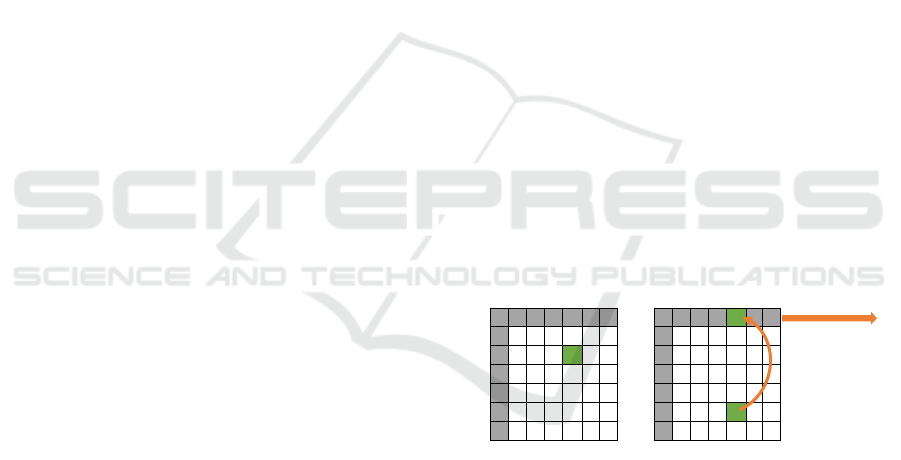
Figure 1: Matching different tissues to available materials
or material combinations, the creation of highly detailed
anatomical models with realistic mechanical properties will
be possible.
The goal of future research is now to compare the
mechanical properties of materials available for
processing via material jetting with those of
biological tissues. To utilize a standardized testing
process increases comparability between biological
and technical materials and seems to be suitable for
the usage in production of anatomical models. Here
especially the execution of uniaxial tension tests
according to ISO 37, which mostly corresponds to
DIN 53504 available for the authors, and indentation
tests according to ISO 48-4 should be conducted.
Tissue
Mechanical properties
Material /
material combination
Mechanical properties
Application in
anatomical models
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
192

While doing this, the general considerations
regarding the mechanical characterization of
biological tissue, like respecting its anisotropic
properties, and keeping it as close to physiological
condition as possible, still have to be made.
By matching the different tissues to the available
technical materials for the material jetting process, as
shown in Figure 1, it will be possible to create highly
detailed anatomical models with realistic mechanical
properties, which can be used for surgery planning
and training, medical education and medical device
testing without raising concerns about health or
ethical issues.
6 CONCLUSIONS
This paper shows that there is a demand for realistic,
high-fidelity anatomical models for surgical planning
and training, medical education, and medical device
testing. Since conventional manufacturing of
anatomical models is a time consuming, and
expensive process, which is not able to fully mimic
the complex nature of the human body regarding
geometry and mechanical properties, the creation of
such models by additive manufacturing, especially
the process of material jetting, is proposed. By
utilizing this process, it is possible to fabricate multi-
color, multi-material objects with complex
geometries, high resolution, and even gradients in
material properties. To be able to generate
appropriate mechanical properties, which resemble
those of biological tissues, the conduction of
biomechanical measurements according to
standardized testing procedures for technical
materials like ISO 37 for tensile and ISO 48-4 for
indentation tests is proposed, since it eases the
matching to the manufacturing materials and thus will
result in the possibility to create more accurate
replicas of the human body, which provide realistic
haptic feedback.
REFERENCES
DIN EN ISO 17296-2: Additive Fertigung - Grundlagen -
Teil 2: Überblick über Prozesskategorien und
Ausgangswerkstoffe.
DIN EN ISO/ASTM 52900: Additive Fertigung –
Grundlagen – Terminologie.
Ahmad B. AlAli; Michelle F. Griffin; Peter E. Butler
(2015): REVIEW Three-Dimensional Printing Surgical
Applications.
AlAli, Ahmad B.; Griffin, Michelle F.; Calonge, Wenceslao
M.; Butler, Peter E. (2018): Evaluating the Use of Cleft
Lip and Palate 3D-Printed Models as a Teaching Aid.
In: Journal of surgical education 75 (1), S. 200–208.
DOI: 10.1016/j.jsurg.2017.07.023.
Birkholz, Peter; Kürbis, Steffen; Stone, Simon; Häsner,
Patrick; Blandin, Rémi; Fleischer, Mario (2020):
Printable 3D vocal tract shapes from MRI data and their
acoustic and aerodynamic properties. In: Scientific data
7 (1), S. 255. DOI: 10.1038/s41597-020-00597-w.
Chae, Michael P.; Lin, Frank; Spychal, Robert T.; Hunter-
Smith, David J.; Rozen, Warren Matthew (2015): 3D-
printed haptic "reverse" models for preoperative
planning in soft tissue reconstruction: a case report. In:
Microsurgery 35 (2), S. 148–153. DOI:
10.1002/micr.22293.
Charles W. Hull (1984): Apparatus For Production of
Three-dimensional Objects By Stereolthography am
08.08.1984. Anmeldenr: 638,905. Veröffentlichungsnr:
4,575,330.
Dimitrios Maragiannis, M. D.; Matthew S. Jackson, MSc;
Stephen R. Igo, BSc; Robert C. Schutt, M. D.; Patrick
Connell, PhD; Jane Grande-Allen, PhD et al. (2015):
Replicating Patient-Specific Severe Aortic Valve
Stenosis With Functional 3D Modeling.
DIN ISO 48-4: Elastomere oder thermoplastische
Elastomere – Bestimmung der Härte – Teil 4:
Eindruckhärte durch Durometer-Verfahren (Shore-
Härte).
Gebhardt, Andreas (2016): Additive Fertigungsverfahren.
Additive Manufacturing und 3D-Drucken für
Prototyping - Tooling - Produktion. 5. Aufl. 1 Band.
München: Carl Hanser Verlag.
Gebhardt, Andreas; Kessler, Julia; Thurn, Laura (2016):
3D-Drucken. Grundlagen und Anwendungen des
Additive Manufacturing (AM). 2., neu bearbeitete und
erweiterte Auflage. München: Hanser (Hanser-
eLibrary).
Hannah Riedle; Barbara Mukai; Pirmin Molz; Jorg Franke
(2018): Determination of the Mechanical Properties of
Aortic Tissue for 3D Printed Surgical Models. In:
BMWiCON-2018.
Hannah Riedle; Kim Braunias; Barbara Mukai; Jorg Franke
(2019): Experimental Mechanical Examination of
Artificial 3D Printed and Post Processed Vascular
Silicone Models
*
.
Jena Anupam B.; Seabury Seth; Lakdawalla Darius;
Chandra Amitabh (2011): Malpractice Risk According
to Physician Specialty.
Macrae, R. A.; Miller, K.; Doyle, B. J. (2016): Methods in
Mechanical Testing of Arterial Tissue: A Review. In:
Strain 52 (5), S. 380–399. DOI: 10.1111/str.12183.
Malik, Hammad H.; Darwood, Alastair R. J.; Shaunak,
Shalin; Kulatilake, Priyantha; El-Hilly, Abdulrahman
A.; Mulki, Omar; Baskaradas, Aroon (2015): Three-
dimensional printing in surgery: a review of current
surgical applications. In: The Journal of surgical
research 199 (2), S. 512–522. DOI: 10.1016/j.jss.2015.
06.051.
Matching of Mechanical Properties of Biological Tissues and Technical Materials for the Fabrication of Anatomical Models by Material
Jetting
193

Mattei, Giorgio; Ahluwalia, Arti (2016): Sample, testing
and analysis variables affecting liver mechanical
properties: A review. In: Acta biomaterialia 45, S. 60–
71. DOI: 10.1016/j.actbio.2016.08.055.
McKee, Clayton T.; Last, Julie A.; Russell, Paul; Murphy,
Christopher J. (2011): Indentation versus tensile
measurements of Young's modulus for soft biological
tissues. In: Tissue engineering. Part B, Reviews 17 (3),
S. 155–164. DOI: 10.1089/ten.TEB.2010.0520.
McMenamin, Paul G.; Quayle, Michelle R.; McHenry,
Colin R.; Adams, Justin W. (2014): The production of
anatomical teaching resources using three-dimensional
(3D) printing technology. In: Anatomical sciences
education 7 (6), S. 479–486. DOI: 10.1002/ase.1475.
Michael S. Sacks (2000): Biaxial Mechanical Evaluation of
Planar Biological Materials.
DIN 53504: Prüfung von Kautschuk und Elastomeren –
Bestimmung von Reißfestigkeit, Zugfestigkeit,
Reißdehnung und Spannungswerten im Zugversuch.
Riedle, Hannah; Burkhardt, Andrea E.; Seitz, Vera; Pachaly,
Bernd; Reid, Russell R.; Lee, Justine C.; Franke, Jörg
E. (2019): Design and fabrication of a generic 3D-
printed silicone unilateral cleft lip and palate model. In:
Journal of plastic, reconstructive & aesthetic surgery:
JPRAS 72 (10), S. 1669–1674. DOI: 10.1016/j.bjps.
2019.06.030.
Stéphane Cotin; Dimitris Metaxas (Hg.) (2004): Medical
Simulation. International Symposium, ISMS 2004.
Berlin, Heidelberg: Springer.
stratasys (2020): J750 Digital Anatomy. Online verfügbar
unter https://www.stratasys.com/de/3d-printers/j750-
digital-anatomy, zuletzt geprüft am 20.11.2020.
Ström, P.; Hedman, L.; Särnå, L.; Kjellin, A.; Wredmark,
T.; Felländer-Tsai, L. (2006): Early exposure to haptic
feedback enhances performance in surgical simulator
training: a prospective randomized crossover study in
surgical residents. In: Surgical endoscopy 20 (9), S.
1383–1388. DOI: 10.1007/s00464-005-0545-3.
Sulaiman, Abdulrazzaq; Boussel, Loîc; Taconnet, Frédéric;
Serfaty, Jean Michel; Alsaid, Hasan; Attia, Cherif et al.
(2008): In vitro non-rigid life-size model of aortic arch
aneurysm for endovascular prosthesis assessment. In:
European journal of cardio-thoracic surgery : official
journal of the European Association for Cardio-
thoracic Surgery 33 (1), S. 53–57. DOI:
10.1016/j.ejcts.2007.10.016.
Yoo, In Seong; Preis, Alexander; Franke, Jörg E. (2020):
Development of a test bench for the urodynamic
simulation of the lower urinary tract. In: IEEE Xplore,
S. 2337–2341. DOI: 10.1109/EMBC44109.2020.91
76198.
Yuan-Cheng Fung (1993): Biomechanics. Mechanical
Properties of Living Tissues. 2. Aufl. New York:
Springer.
BIODEVICES 2021 - 14th International Conference on Biomedical Electronics and Devices
194
