
Establishing the State of Practice about Data Standards in
Monitoring Healthcare Interventions for HIV in Uganda’s
EMR-based Health Information Systems
Achilles Kiwanuka
1a
, Moses Bagyendera
1
, Joseph Wamema
1b
, Andrew Alunyu
1c
,
Mercy Amiyo
1d
, Andrew Kambugu
2e
and Josephine Nabukenya
1f
1
Department of Information Systems, Makerere University, Kampala, Uganda
2
Infectious Diseases Institute, Makerere University Kampala, Kampala, Uganda
{mamiyo, josephine}@cit.ac.ug, akambugu@idi.ac.ug
Keywords: eHealth, Data and Interoperability Standards, Electronic Medical Records, Health Information Systems.
Abstract: Electronic Health Information Systems (EHIS) in Uganda are characterised by inaccessibility to reliable,
timely and integrated data for effectively monitoring and tracking continuity of care for people living with
HIV, exacerbated by disparate, fragmented EHIS in varying health system levels that are not interoperable
and lack common data standards. In order for data to be comparable, there has to be uniformity in terms of
standards that are employed in a uniform manner in all data management processes. In this study, we
established the state of current practice regarding data and interoperability standards in monitoring and
evaluating healthcare interventions for HIV in Uganda’s EMR-based health information systems. The study
findings indicate that there are scanty practices and/or implementation of the eHealth standards (data and
interoperability), and limited to noncompliance of monitoring these standards in the implementation of the
HIV healthcare interventions. Accordingly, our study recommendations point to the need of designing data
and interoperability frameworks to provide for the specific set of standards, protocols, procedures, best
practices and policies for eHealth standardisation in Uganda’s health system.
1 INTRODUCTION
An estimate of 6.7% of Ugandan adult population
have been diagnosed and are currently living with
HIV (Ministry of Health, 2017). Given the magnitude
of the disease, there is a need to use data-driven
approaches to facilitate decision-making ensuring
appropriate interventions are implemented in relevant
populations in the right way (PEPFAR, 2011). In
order for data to be comparable, there has to be
uniformity in terms of standards that are employed in
a uniform manner in all data management processes.
According to the Institute of Electrical and
Electronics Engineers (IEEE), a standard is a
a
https://orcid.org/0000-0003-3352-0312
b
https://orcid.org/0000-0001-6328-7801
c
https://orcid.org/0000-0003-2957-8423
d
https://orcid.org/0000-0002-8172-5382
e
https://orcid.org/0000-0002-3075-0211
f
https://orcid.org/0000-0002-4731-2496
“document that defines the characteristics of a
product, process or service, such as dimensions,
safety aspects, and performance requirements”
(IEEE, 2010). Standards facilitate the consistent and
precise collection and exchange of information across
different services of the health system (World Health
Organization & International Telecommunication
Union, 2012) and are a prerequisite for the smart
healthcare (Chang et al., 2019) .
Uganda’s Ministry of Health has implemented
numerous electronic-based Health Information
Systems (EHIS) including OpenMRS/UgandaEMR,
Integrated Clinic Enterprise (ICEA), and District
Health Information Software 2 (DHIS2) that are used
for reporting, documenting and managing HIV and
200
Kiwanuka, A., Bagyendera, M., Wamema, J., Alunyu, A., Amiyo, M., Kambugu, A. and Nabukenya, J.
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health Information Systems.
DOI: 10.5220/0010264302000211
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 200-211
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

TB patients (Ministry of Health, 2017). Yet the
country’s health system is still challenged with
translation of data into effective use for decision
making and policy development (Henriksson et al.,
2019). This situation is exacerbated by disparate, un-
interoperable fragmented EHIS in varying health
system levels and lack of common data standards to
facilitate sharing data consistently across the health
system (Ministry of Health, 2017; Alunyu and
Nabukenya, 2018; Egwar et al., 2020).
To this end, this study aimed at investigating the
current state of practice regarding data standards for
monitoring healthcare interventions of HIV and TB in
Uganda’s EMR-based health information systems
(EHIS). The choice of these diseases was remitted on
the fact that several global and local efforts, that is,
Uganda government and Health Development
Partners (HDPs) implemented enormous EHIS
investments to accelerate the achievement of the
epidemics control of HIV and TB (Ministry of Health,
2010). Particularly, various duplicated and
disintegrated EHIS have been developed to manage
the HIV and TB epidemic; as such these require
standardising in order to facilitate proper health
information exchange across Uganda’s health system.
2 METHODOLOGY
Study Design: We used the cross-sectional design
since it provides a snapshot of the prevalence of the
study subjects in a single time point (Awaisu & Banan
Mukhalalati, 2019).
Study Area: The study covered four key regions
in Uganda (Kampala, Wakiso, West Nile and Mid-
Western) representing the full spectrum of HIV and
TB prevalence (Ministry of Health, 2017). Kampala
and Wakiso are mainly urban high-HIV prevalence
regions, characterised by high mobility, slum-
dwelling, and limited social support. Mid-Western
comprises some urban/rural populations undergoing
significant socio-economic transformation with an
influx of high-risk groups for HIV transmission like
sex workers). West Nile region is a low-prevalence,
sparsely populated area but prone to the influx of
refugees (currently standing at 1.4 million).
The structure of the health system in Uganda is
decentralised in to six levels, which include: village
health teams, health centre II, health centre III, health
centre IV (district hospital), regional referral hospital,
and national referral hospital. The health facilities
that serve the various levels are referred to as health
centres II, III, IV, and hospitals (district and regional)
(Ministry of Health, Health Systems 20/20 &
Makerere University School of Public Health, 2012).
Data Collection Sites: A stakeholder analysis
was done for all institutions affected by eHealth data
and interoperability standards. The study engaged
stakeholder groups at 4 different health system levels:
national-referral, regional-referral, district hospitals
and HCIVs. The focus on the top 4 levels was due to
the existence of fairly mature but suboptimal EHIS
for data collection and the clear links between those
levels and data use for decision making processes.
Inclusion Criteria: The health facilities that were
included in this study were selected based on the
similarities of the healthcare system in the different
regions in the country, coupled with analogous health
services in health facilities in Uganda. The selected
facilities were health centre IVs in the four key
regions: Central (Kasangati, Namayumba, Ndejje,
Wagagai, Wakiso, Kitebi), Western (Kigorobya,
Emesco, Kibaale, Kakindo, Kakumiro, Kikuube),
Northern (Atiak, Aboke, Amach, Awach) and West
Nile (Adumi, Kuluva, Omugo, River Oli, Pakwach,
Warr). Additionally, data as collected from hospitals
(Kuluva, St Mary’s Lacor, Nebbi and Mulago) and
regional referral hospitals (Entebbe, Hoima, Lira,
Gulu). The combination of health facilities increased
heterogeneity, internal validity and thus
generalizability of the study findings.
Sampling Method and Size: Purposive strategies
guided the sampling process by using individual
judgement to select cases that answer the research
questions (Saunders et al., 2012). The study
population included respondents at health facilities
and national level. The study respondents at health
facilities included: clinicians (medical/clinical
officers) – 32, pharmacists or their assistants – 20,
laboratory technologists or their assistants – 28 and
nurses or their assistants – 51. At the national level,
respondents were from Uganda National Bureau of
Standards (1), Ministry of ICT and National
Guidance (1), National Information Technology
Authority – Uganda (1), Ministry of Health (3),
Central Public Health Laboratory (1), information
system developers (2), research institution (1),
telecommunications company (1) and HDPs (4).
Data Collection and Analysis: Primary data
were collected using semi-structured interviews pre-
programmed on a tablet using Open Data Kit (ODK)
software. Secondary data were collected through
document analysis of the existing data. Data were
collected by 16 research assistants who were trained
and piloted with the data collection tools before the
actual data collection. The interviews were audio
recorded in English, transcribed and then loaded into
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
201

NVIVO software version 12 for analysis.
Quantitative data were analysed using descriptive
statistics and presented using tables and figures.
Qualitative data were analysed using thematic
analysis methods (Maguire & Delahunt, 2017).
Ethical Clearance: Ethical clearance to conduct
the study was obtained from the Makerere University
School of Public Health Research Ethics Committee
(REC) and/or Institutional Review Board (IRB); and
the permission to conduct the research in the
healthcare sites was sought from the Ministry of
Health. Written informed consent was also obtained
from study participants prior to being interviewed.
3 RESULTS
The results are presented in three subsections:
existence and practice of eHealth standards,
standardisation support provided to the Ministry of
Health, and monitoring implementation of eHealth
data and interoperability standards.
3.1 Existence and Current Practice of
eHealth Standards
In this section, we report on the eHealth standards
categorised as medical coding, data exchange and
sharing, communication infrastructure and data
security and privacy standards.
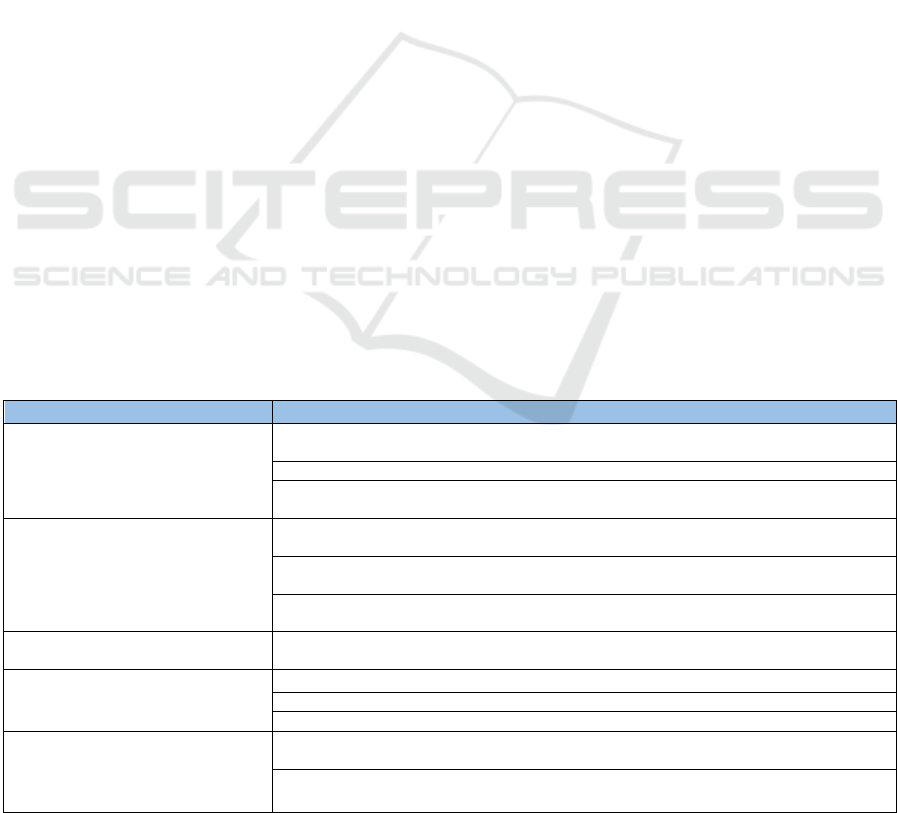
3.1.1 Medical Coding Standards
Medical classifications transform diagnoses or
procedures into standardized codes. Regards
classification of diseases, 81% of the respondents
mentioned that they classify data while providing
services to clients as shown in figure 1. When
providing HIV services, the data is coded using the
Differentiated Service Delivery Models (DSDM) of
HIV Services in Uganda as reported by respondent
HSL2-06: “we do a lot of medical coding and we
always have somewhere where the codes are
explained, for example under DSDM” – HSL2-06.
The International Classification of Diseases (ICD)
standard has been adopted and integrated in the
UgandaEMR, a system that is implemented in many
Uganda health facilities, as mentioned by IP10.
Respondent M01 also noted that the Ministry of
Health had adopted the ICD11 standard for disease
coding and the standard had been integrated in some
of the systems that are used at the Ministry. The
ICD10 standard was also found to be implemented in
Mulago and St Mary’s Lacor hospitals.
In research institutions, it was found that the
Medical Dictionary for Regulatory Activities
(MedDRA) is one of the medical coding standard that
was used in medical research databases.
Management is instrumental in the use of such
standards in the health facilities as 70% of the
respondents mentioned that management supports
them to use classification of diseases and procedures
while performing their duties. Insurance companies
also did require health facilities to report medical
diagnoses using the ICD standard.
3.1.2 Data Exchange and Sharing Standards
Majority (64%) of the respondents were aware of the
presence of data sharing or exchange at the facilities.
Only 16% mentioned that they were not aware while
20% were neutral. Although there were data sharing
or exchange guidelines, 45% of the respondents
disagreed that the existing ICT infrastructure was
good enough to support healthcare processes. A lot of
investments had been made in infrastructure
including hardware, internet infrastructure, power
availability and network infrastructure. At the time of
the study, it was mentioned that the Ministry of
Health was in liaison with Uganda’s National
Information Technology Authority (NITA-U) to
connect most of the healthcare facilities to the
national backbone infrastructure.
It was also reported that the Government of
Uganda had developed several interoperability
Figure 1: Perception of Coding Practices by Health Workers.
9%
10%
39%
10%
20%
20%
81%
70%
41%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90%
I classify health data (diseases, procedures) while providing
services to clients
Management supports me to use classification of diseases and
procedures in performing my duties
I was adequately trained in health data (diseases, procedures)
classification
Agree Neutral Disagree
HEALTHINF 2021 - 14th International Conference on Health Informatics
202
Respondent PM02 reported that “the equipment that
was used in the country was compatible with
interoperability standards like HL7 for laboratories
and DICOM for radiology services.”
Additionally, Health Level Seven (HL7) had been
adopted in the UgandaEMR as reported by
respondent IP10. Another interoperability standard
that had been tested is the Open Health Information
Mediator (OpenHIM). “The openHIM standard was
tested and has worked for the exchange of some of the
viral load data between the EMRs and the viral load
systems” respondent PM01.
Although the HL7, Digital Imaging and
Communications in Medicine (DICOM) and
OpenHIM interoperability standards did exist, only
35% of the respondents mentioned that the adopted
EHIS were compatible with each other.
The Ministry of Health had also developed
systems that were interoperable like mTrac and
DHIS2 which have been adopted at the national level
to manage health information. These were
communicating to each other as described by
respondent IP01. “We have data that is collected
weekly on papers. We also have electronic
components of data collection using SMS and
Android application called mTrac. This data is hosted
on DHIS2 server once it is collected. The data that is
collected from SMS and android application ends up
in DHIS2.” – IP01
Although the Ministry had not explicitly adopted
health information exchange standards, some
interoperability standards were implemented in
isolated EHIS as reported by respondent IP01.
3.1.3 Communication Infrastructure /
Technologies Standards
Regards communication infrastructure/technologies
standards, 46% of the respondents mentioned that the
facility could afford to establish and maintain the
required ICTs, while 39% disagreed. On internet
connectivity, only 11% of the respondents mentioned
that the internet connectivity was very good at the
health facilities, 22% mentioned that it was stable but
slow, whereas over 43% mentioned that they had
variable connectivity (on and off). Besides, only 32%
of the respondents agreed that the facility had
guidelines for communication and access to
electronic health records. The standards for electronic
communication infrastructure, as adopted from
international standards are shown in table 1.
The existing ICT and communication networks in
health facilities were mostly used to support healthcare
processes as mentioned by 53% of the respondents.
The quality of the infrastructure was in question as only
41% reported that it was good enough to support
healthcare processes. Respondent HSL4-15 reported a
constant problem of power and internet challenges to
be affecting the quality of the infrastructure.
Respondent HSL4-07 also mentioned that they still had
limitations in accessing the internet in their health
facility. Adequacy of the hardware and application
technologies was poorly ranked as only 38% agreed
that the facility had adequate hardware and application
technologies to support healthcare processes. Whereas
the adequacy of ICT infrastructure was 38%, more
respondents (46%) mentioned that the facility could
afford to establish and maintain required ICTs.
Table 1: Electronic Communication Infrastructure Standards.
Category Standard
Health Informatics US ISO 17090-1:2013 - Public key infrastructure - Part 1: Overview of digital certificate
services
US ISO 17090-2:2008 Public key infrastructure - Part 2: Certificate Profile
US ISO 17090- 3:2008 - Public key infrastructure - Part 3: Policy management of certification
authority
Data Management and Interchange US ISO IEC 9075-2: 2011 - Information Technology – Database Languages - SQL - Part 2:
Foundation (SQL/Foundation)
US ISO IEC 9075-11: 2011 - Information Technology – Database Languages - SQL - Part 11:
Information and Definition Schemas (SQL/Schemata)
US ISO IEC 9075-14: 2011 Information Technology – Database Languages - SQL - Part 14:
XML –Related Specifications (SQL/XML)
Telecommunications and Information
Exchange between Systems
US ISO IEC 9594-8:2008 - Information Technology - Open Systems Interconnection - The
Directory: Public-key and Attribute Certificate Frameworks
Information and Documentation US ISO IEC 15489-1:2016 - Records Management - Part 1: General
US ISO 13008:2012 - Digital Records Conversion and Migration Process
US 1717:2017 - Implementation Guidelines for Digitization of Records
Information Technology Service
Management
US ISO IEC 20000-1: 2018 - Information Technology – Service Management - Part 1: Service
Management System Requirements
Guidelines and Standards for Acquisition of Information Technology Hardware & Software
for Government Ministries, Departments and Agencies
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
203
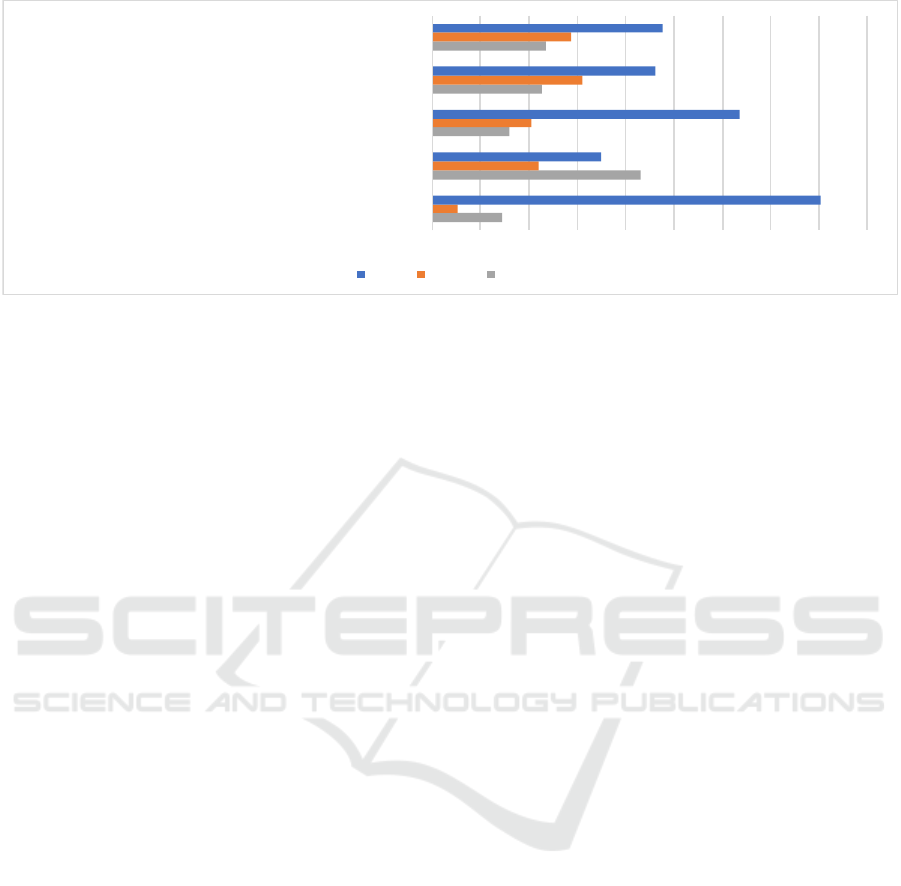
Figure 2: Perception of eHealth Security at Health Facilities.
3.1.4 eHealth Data Security and Privacy
71% of the respondents agreed that they were aware
of the guidelines for privacy and personal identifiable
data in their settings whereas only 8% disagreed. Two
information security standards were adopted by
NITA-U: US ISO IEC 27007: 2011 and US ISO IEC
27032: 2012.
The perception of health workers towards eHealth
security was assessed as shown in figure 2. Over 80%
of the respondents noted that the health data that they
were responsible for was valuable, and 64%
mentioned that information security
controls/guidelines were implemented to ensure that
health data were kept secure. Only 35% of the
respondents mentioned that their health facilities
often faced health data security threats, 46% felt that
the security controls/guidelines implemented were
sufficient. 63% of the respondents reported that the
existing ICTs were secure and protected the client’s
privacy and information, and that the available
guidelines fully addressed security issues, access
privileges and or privacy concerns.
53% of the respondents disagreed that there was a
sense of insecurity in using ICT in health. Some of
the security measures that had been implemented
were: each authorised operator had a secret password
that was updated every 3 months and they were held
responsible in case it was used by someone
unauthorized in case they did not report this prior;
various levels of security were deployed, including
authenticating users who attempted to access these
resources, firewalls; some HDPs had their own
security policies and all new staff had to be trained on
them as mentioned by respondent PM07.
3.2 eHealth Standardization Process
The eHealth standardisation process refers to the
process of utilising best practices and principles for
managing eHealth data and processes in a uniform
manner across various levels of the health system
(Kimaro and Twakyondo, 2005). In this sub-section,
we present: eHealth standards adoption, adaptation
and contextualization process; standardisation
support provided to the Ministry of Health; and
challenges affecting the standardisation process.
3.2.1 eHealth Standards Adoption,
Adaptation and Contextualization
Process
Regarding facility assessment for ICTs, only 38% of
the respondents agreed that an assessment was done
for readiness to adopt ICT for healthcare processes.
At the time of study, the Ministry had adopted
eHealth guidelines for provision of its health services.
However, only 35% of the respondents agreed that the
ICT adoption and implementation decision processes
were properly streamlined. The guidelines for
eHealth were specific for health information
exchange, telemedicine and digital health
implementation as mentioned by respondent PM01.
The process of developing and/or reviewing
standards in Uganda is inter-sectorial and involves
various Ministries, Departments and Agencies
(MDAs). This was well elaborated by respondent
PM05, and can be summarised into seven stages as
identification, preparatory, committee discussing
draft, public enquiry, confirmation, approval and
declaration of mandatory standards.
The Ministry of Health developed the eHealth
Policy to guide eHealth standards implementation as
mentioned by respondent PM03: “the Ministry had a
participatory way in which it developed standards,
14%
43%
16%
23%
23%
5%
22%
20%
31%
29%
80%
35%
64%
46%
48%
0% 10% 20% 30% 40% 50% 60% 70% 80% 90%
The health data that I am responsible for is valuable
My health facility often faces health data security threats
Information security controls/guidelines have been implemented to
ensure that health data is kept secure
The security controls/guidelines that have been implemented are
sufficient
I feel sufficiently supported by top management in regard to
information security
Agree Neutral Disagree
HEALTHINF 2021 - 14th International Conference on Health Informatics
204

Figure 3: Perception of eHealth Adoption and Standardisation.
guidelines and Standard Operating Procedures.
There were consultative meetings in the beginning,
development process and a validation process that
took place before adaptation. The guideline had to go
through the bureaucracy of the Ministry. We have
technical working groups that must approve it for use.
It must be presented to the monitoring, evaluation and
budget technical working groups to understand what
the implication will be in terms of resources. Then it
is pushed forward to the HIPA, which is one of the
approving bodies and then to senior management for
final clearance. Once senior management has cleared
it, it can then be put into standard use” – PM03
Only 29% of the respondents at health facilities
agreed that there was team work and collaboration
with the Ministry of Health personnel and
stakeholders drawn from outside the health facility
when developing standards, and only 20% agreed that
the team composition was drawn from all facility
departments as shown in figure 3.
45% of respondents disagreed that the meeting
was structured and could be conducted by any person.
Over 61% mentioned that they did not participate in
determining guidelines for ICT to be used at health
facility. For some who were involved, the
participation was about assessing and acknowledging
draft documents as mentioned by respondent HSL2-
06: “Recently, I was part of the team that came up
with the M&E health plan for the country…...we
basically gave technically support……. They first
make the draft and we come in to assess and
acknowledge what they have done” – HSL2-06
Although the participation at the facility level was
low (14%), a respondent from the Ministry of Health
elaborated that health workers were involved in
consultations and validation of the documents.
3.2.2 Standardisation Support Provided to
the Ministry of Health
Resources for developing guidelines were not
sufficient as mentioned by 40% of the respondents.
HDPs like United Nations Children's Fund and World
Health Organisation (WHO), provided funding
directly to the Ministry of Health to support the
standardisation process. The catalytic funds were
used to facilitate initial scoping to know the extent of
need and make a case for development of standards.
43% of the respondents disagreed that health
workers have the required level of literacy to use ICT
in health. HDPs provided technical support to the
Ministry of Health during the standardisation process
including the provision of standards and guidance
documents as mentioned by respondent IP02:
“provide standards from other settings/countries,
that can be used for benchmarking and best
practice.” – IP02.
Some HDPs had well-established systems that the
Ministry of Health used for benchmarking as reported
by respondent IP07: “Ministry of Health and other
stakeholders already picked interest in Infectious
Diseases Institute’s in-house developed eHealth
platforms - ICEA… The Ministry of Health has on
several occasions engaged Infectious Diseases
Institute teams in discussions aimed at understanding
and possibility adopting some of our eHealth
platforms for nationwide use” – IP07.
52%
66%
61%
42%
45%
33%
40%
45%
28%
23%
25%
37%
35%
38%
45%
40%
20%
11%
14%
20%
20%
29%
15%
14%
0% 10% 20% 30% 40% 50% 60% 70%
I participate in the decision process when planning the facility IT networks
I participate in the design/procurement of IT systems for the health facility
I participate in determining guidelines for ICT to be used at health facility
A team is constituted to develop, select or review guidelines for ICT
The team composition is drawn from all facility departments
The team work in collaboration with MoH personnel and other stakeholders
drawn from outside the facility
The team has adequate time and resources to develop the guidelines
The team meeting is structured and can be conducted by any person including
non-professionals team meeting facilitators
Agree Neutral Disagree
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
205

3.2.3 Challenges of the Standardisation
Process
Insufficient Participation of Key Stakeholders: Only
14% of the respondents at health facilities mentioned
that they participated in determining the guidelines
for ICT to be used at health facility level. Similarly,
at national level, respondent PM05 reported that there
was insufficient participation of key stakeholders
while conducting review meetings or workshops and
proposed vigilance by the Ministry of Health.
Inadequate Technical Expertise: Uganda did not
have adequate technical expertise in the field of
public health informatics. Only 35% of the
respondents agreed that healthcare workers had the
required level of literacy to use ICT in health. Further,
only 47% of the respondents agreed that management
at the health facility was aware of the complexity of
the changes that would result from the adoption of
eHealth in their work practices.
Financial Constraints: Only 15% of the
respondents at health facility level agreed that
standards development or review team had adequate
resources to develop the eHealth guidelines. The
same was echoed by respondent PM05 at national
level that a significant amount of money was needed
for implementing the standards.
Weak Leadership: There was a challenge in the
leadership structure of deciding which innovations
were to be considered or not as mentioned by
respondent IP01. The complexity of multiple
innovations led to having multiple systems with
different standards that could not be interoperable.
There were challenges of individuals or agencies with
interests of moving their agenda forward and not
abiding to the implementation of standards. The weak
leadership resulted into siloed applications as
mentioned by M01: “Our biggest challenge has been
siloed implemented applications at disease level that
are not even speaking to each other…. most of these
solutions are not also sustainable…...this is because
HDPs implement systems without following the
structures put in place for approval.” – M01. The
siloed systems were also facilitated by lack of
monitoring systems in place as noted by respondent
R101. This finding aligns with the fact that only 33%
of the respondents agreed that implementers adhered
to guidelines when implementing ICT in healthcare.
3.3 Compliance to Monitoring
Implementation
3.3.1 Governance Structures
As shown in figure 4, 46% of the respondents
mentioned that there was a strong eHealth governance
at health facility level whereas 29% disagreed.
Regarding eHealth expertise at health facilities,
42% of the respondents mentioned that there is
adequate expertise while 34% disagreed. The
expertise matches with the finding that only 28% of
the respondents reported that they were trained on
how to use the eHealth applications that they used.
The skills gaps are covered by HDPs through training
and mentoring.
Only 36% of the respondents agreed that they
were involved in decision making of eHealth
development whereas over 43% disagreed. In line
with the same issue, only 32% mentioned that the
facility had guidelines for communication and access
to electronic health records. Some facilities had
implemented their own measures as described by one
of the respondents: “We have something which is
quite brief, mainly for guiding the workers on
guarding against misuse of the ICT. We even have a
security system whereby you cannot go to other
websites….” – HSL3-02.
Majority (63%) of the respondents agreed that the
existing ICTs were secure and protected clients’
privacy and information. Physically, there were
security personnel to guard the equipment as
Figure 4: Governance Structure of eHealth at Health Facilities.
43%
34%
29%
21%
23%
25%
36%
42%
46%
0% 5% 10% 15% 20% 25% 30% 35% 40% 45% 50%
I am involved in decision making concerning development of eHealth
There is adequate expertise in eHealth at the health facility
There is a strong eHealth governance at the health facility
Agree Neutral Disagree
HEALTHINF 2021 - 14th International Conference on Health Informatics
206

Figure 5: Compliance to eHealth Standards at Health Facilities.
mentioned by respondent HSL4-24 and M09
respectively: “we have security personnel who are
responsible for guarding the facilities, the rooms are
lockable and access is limited to a few people”-
HSL4-24, “the server environment is securely locked
with only finger print access” – M09. The security
measures that had been put in place were adopted
from the Ministry of ICT. The government also had a
role in ensuring that there was secure exchange of
information by providing a public key infrastructure.
3.3.2 Compliance to eHealth Standards and
Guidelines at the Health Facility and
National Levels
Familiarity of the guidelines that govern ICT was at
39% among respondents as shown in figure 5.
Similarly, only 39% mentioned that there was an
established structure that monitored compliance to
eHealth standards. This showed non-awareness of the
compliance structures as there were monitoring and
evaluation plans in every guideline as mentioned by
respondent PM01: “For each of those guidelines, we
have a monitoring and evaluation plan on how we are
going to implement and monitor compliance with
those guidelines” – PM01.
Only 36% agreed that they were involved in
eHealth planning and decision making. Respondent
HSL4-10 mentioned that no consultations were done
before bringing systems to the facility: “they have to
come to the facility and do an assessment of what is
specifically needed. Most times we find everything
just brought without consulting the facility on what is
needed.” – HSL4-10.
Only 32% of the respondents agreed that there
were guidelines for establishing and implementing
ICT at health facilities. Similarly, only 33% agreed
that there were guidelines for monitoring the use of
ICT and that implementers adhered to the guidelines
when implementing ICT in healthcare. The same
challenge of non-adherence to guidelines when
implementing ICT was reported at national level by
respondent, PM03: “someone goes and develops a
system without consulting us and knowing what
problem we have and then tries to force us to use the
system” – PM03. Some measures for monitoring
compliance had been devised by health institutions.
Access to some sites were be blocked as mentioned
by HSL3-02; “…you are blocked if you try to access
certain sites which you are not supposed to.” –
HSL3-02. The effectiveness of the measures in place
can be backed up by the fact that 64% of the
respondents agreed that information security
controls/guidelines had been implemented to ensure
that health data were kept secure.
Health Development Partners had played a crucial
role in monitoring compliance to standards. In the
absence of an independent arm of monitoring and
evaluation in the government, HDPs support the
Ministry of Health as mentioned by respondent
HSL2-06: “The government does not have an
independent arm attached to monitoring and
evaluation. The health development partners bring in
their M&E systems.” – HSL2-06.
Generally, each of the Ministry guidelines had a
section of monitoring and evaluation, particularly on
implementing and monitoring compliance as
mentioned by respondent PM01: “For each of the
guidelines, we have a monitoring and evaluation plan
on how we are going to implement and monitor
compliance.” – PM01.
Additionally, technical working groups approve
information systems in Uganda before they are
deployed: “The technical working group of the
25%
25%
22%
28%
26%
26%
43%
42%
45%
37%
39%
39%
32%
33%
33%
35%
35%
35%
0% 5% 10% 15% 20% 25% 30% 35% 40% 45% 50%
There are guidelines for establishing/implementing ICT at the health facility
There are guidelines for monitoring use of ICT at the health facility
Implementers adhere to guidelines when implementing ICT in healthcare
There is an established structure that monitors compliance to eHealth
standards
This facility collaborates with other facilities in monitoring compliance to
standards
Users of ICT at the facility are familiar with guidelines that govern its use
Agree Neutral Disagree
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
207

Ministry of Health has sub-committees that sit and
evaluate these systems before they (systems) are
approved and implemented for the case of monitoring
ICD-11” – PM01.
The NITA-U conducts assessments of
implemented systems as part of monitoring to ensure
that they complied with standards as mentioned by
respondent PM04: “NITA-U also conducts
assessment to compliance to standards once systems
have been implemented.” PM04.
3.3.3 Challenges of Monitoring Compliance
Inadequate Resources: Only 15% of the respondents
agreed that the standards development team had
adequate time and resources to develop standards or
guidelines. Besides, only 35% of the respondents
agreed that health service providers had the required
level of literacy to use ICT in health. Respondent
IP02 supplemented by saying that ICT skills related
to eHealth are inadequate, both in terms of the
numbers and skills mix/set. Respondent PM04 also
commented about the eHealth skills of the health
workers and mentioned that there was inadequate
integration of eHealth skills into existing health
professional training curricula. Moreover, only 41%
of health workers mentioned that they were
adequately trained in health data classification.
Financial Constraints: Only 38% agreed that
health facilities and Ministry of Health had adequate
financial capacity to support ICT, yet it was
expensive to hire consultants as mentioned by
respondent M05.
Non-Involvement of Stakeholders: At the health
facility level, only 36% of the respondents agreed that
they were involved in eHealth decision making. At
the national level, the technical MDAs would only
provide support; however, the Ministry of Health had
not taken the lead in enforcing compliance as reported
by respondent PM04. Moreover, only 52% agreed
that management takes an active role in preparing
plans for implementing eHealth.
Non-operational Regulatory Frameworks:
Although health facilities had guidelines with quality
parameters to regulate implementation as mentioned
by 76% of the respondents, implementation was a
challenge because of the lack of regulatory frame-
works as mentioned by respondent PM05: “once the
National Standards Council has declared a Ugandan
Standard, at that stage, it is still voluntary to use the
standard because of the regulatory framework that
we have in this country.” PM05. Respondent R101
also noted the inability to operationalise the
regulatory framework currently in place.
4 DISCUSSION
4.1 Existence and Current Practice of
eHealth Standards
In health facilities, it has been reported that the ICD
standard has been used to a lesser extent to record
morbidity and mortality statistics (Ministry of Health,
2014). In our study, 81% of the respondents noted that
they classified health data while providing services to
clients. The ICD standard is the foundation for the
identification of health trends and statistics globally,
and the international standard for reporting diseases
and health conditions (WHO, 2020).
One of the standards that is used to code health
research data is MedDRA). This is a clinically
validated international terminology for medical
products used by regulatory authorities (MedDRA,
2015). One advantage of the MedDRA standard is
that it can be mapped to SNOMED (Banda et al.,
2016; Bousquet et al., 2019; Yuksel et al., 2016).
Inefficient EHIS for public health surveillance are
partly as a result of inability of lack of interoperability
(Celi et al., 2017; Greenwell and Salentine, 2018).
Yet poor coding processes can damage also
information quality (Teixeira et al., 2013).
Information systems in public health should ensure
greater quality and efficiency, not only in the
management of health institutions, but also in
patients’ treatment (Carvalho et al., 2016). Efforts are
in place to have a comprehensive approach to an
integrated and efficient data collection process
important to public health (Health Enabled, 2017;
(Kuperman et al., 2013; WHO, 2015).
Data is a major challenge in the information
security (Aggarwal et al., 2013). Data security refers
to the assurance of data and its important assets like
tools and equipment for its gathering, data storage and
the transmission process (Whitman &Mattord 2009).
Standards decrease health workers’ concerns over
patient data safety and professional liability
(Benavides-Vaello et al., 2013; Jennett et al., 2004)
and thus enabling ease of work.
Although many of the electronic communication
infrastructure standards are not direct for public
health informatics, they can still be adopted or
customised for the health sector. This is exemplified
by NITA-U in Uganda adopting international ICT
standards. NITA-U also has national guidelines and
standards for acquisition of information technology
hardware and software for government MDAs that
can be readily adopted for the health sector and most
especially HIV services.
HEALTHINF 2021 - 14th International Conference on Health Informatics
208

Interoperability of national information systems
ensures sharing of valuable information across the
government systems (Mandl & Kohane., 2012;
Terhune et al., 2009) to collectively support online
improved service delivery (McDonnell, 2012). A
number of international certification and standards
bodies work towards developing standards to address
interoperability issues including; International
Standards Organization (ISO), European Committee
for Standardization (CEN), HL7, OpenEHR and
IEEE 11073-20601-2008 (Trigo et al., 2013).
Opportunities to improve healthcare by reusing data
are often missed due to the limited interoperability of
eHealth solutions (Beerenwinkel et al., 2018). An
interoperability framework provides for the specific
set of standards, protocols, procedures, best practices
and policies to improve digital solutions (Barbabella
et al., 2017; Lamine, 2017).
In order for information management to have
meaning across health systems, there has to be a
common language and format across all facilities
(Braa et al., 2017). For health facilities transitioning
from paper to electronic systems, the common format
provides an opportunity to move from errors in paper-
based record-keeping that can affect the delivery of
safe quality care (The Joint Commission, 2011).
Standards have to be implemented in health
information systems to achieve interoperability,
portability and data exchange. Yet, systems that
conform to different standards cannot communicate
with one another (Hammond & Cimino, 2006).
Oderkirk (2017) also noted multiple standards as a
challenge to standardisation. This can be caused by
siloed systems having different standards.
Information technology standards, including
standards for messaging, content and coding,
networks, electronic data interchange, and electronic
health records, are important to healthcare
information systems.
4.2 eHealth Standardization Process
and Compliance to Monitoring
Implementation
Uganda made advancement in utilizing information
technology to report aggregated data at national level
in 1997 through the introduction of electronic Health
Management Information System (MoH, 2017).
Consequently, the eHealth framework was put in
place including the ICT Policy (Ministry of ICT,
2011), eHealth Policy (MoH, 2016) and the five-year
eHealth Strategic Plan. These policies are
instrumental in shaping the eHealth governance in
Uganda’s health system.
Successful EHIS interoperability depends on the
presence and use of widely adopted data exchange,
security, and messaging standards (Measure
Evaluation, 2019). A standard should be approved by
a recognized standards development organization, or
it should have been accepted by the industry like
International Telecommunications Union (ITU), ISO,
WHO or a national standards body (Celi, et al., 2017).
True data interoperability requires the development
and implementation of standards and clinical-content
models and frameworks (Begoyan, 2007; Goossen et
al., 2010) for the unambiguous representation and
exchange of clinical meaning (Knaup et al., 2007).
The findings indicate that there are scanty
practices and/or implementation of the eHealth
standards. The same was also found out in Tanzania
where Mukasa et al (2017) noted absence of health
information system standards control mechanisms to
be the cardinal challenge of standardizing
information systems for integrated TB/HIV services.
Insufficient participation of key stakeholders and
inadequate resources as reported in this study were
also identified as challenges to the standardisation
process by Mukasa et al., (2017). During the design
of EHIS, a holistic service perspective can leverage
the full potential to health information systems.
5 CONCLUSIONS
This study investigated the state of current practices
and challenges to data and interoperability standards
in monitoring HIV healthcare interventions in
Uganda’s EMR-based health information systems.
The key data standards practices included MedDRA,
DSDM, ICD and HL7 which positively impacted on
the monitoring of HIV data management and
exchange among healthcare interventions in various
EHIS. The study also identified challenges to data and
interoperability standards compliance monitoring that
included insufficient participation of key
stakeholders, inadequate technical expertise,
financial constraints and weak leadership or
governance. These challenges are barriers that
adversely affect successful eHealth standards
implementation in EHIS. As such our future work is
to progress with designing of contextual data and
interoperability frameworks to provide for the
specific set of standards, protocols, procedures, best
practices and policies that can be used to improve
monitoring of HIV healthcare interventions for
Uganda’s EMR-based health information systems.
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
209

ACKNOWLEDGEMENTS
The authors acknowledge the Government of the
Republic of Uganda through Makerere University
Research and Innovation Fund for sponsoring the
study; as well as the study participants at national and
sub-national level in Uganda’s health system.
REFERENCES
Aggarwal, N., Tyagi, P., Dubey, B.P., Pilli, E.S.: Cloud
computing: data storage security analysis and its
challenges. Int. J. Comput. Appl. 70, 33–37 (2013)
Alunyu, A., and Nabukenya, J. (2018). A Conceptual
Model for Adaptation of eHealth Standards by Low and
Middle-Income Countries. Journal of Health
Informatics in Africa, Vol. 5(2), 10-16
Awaisu, A., & Banan Mukhalalati, M. I. M. I. (2019).
Research designs and methodologies related to
pharmacy practice. Encyclopedia of Pharmacy Practice
and Clinical Pharmacy, 7.
Banda, J. M., Evans, L., Vanguri, R. S., Tatonetti, N. P.,
Ryan, P. B., & Shah, N. H. (2016). A curated and
standardized adverse drug event resource to accelerate
drug safety research. Scientific data, 3(1), 1-11.
Barbabella, F., Melchiorre, M. G., Quattrini, S., Papa, R.,
Lamura, G (2017): How can eHealth improve care for
people with multimorbidity in Europe? World Health
Organization, Regional Office for Europe (2017).
Beerenwinkel, N., Fröhlich, H., Murphy, S., A.:(2018)
Addressing the Computational Challenges of
Personalized Medicine (Dagstuhl Seminar 17472). In
Dagstuhl Reports (Vol. 7, No. 11).
Begoyan, A. (2007). An overview of interoperability
standards for electronic health records. USA: society for
design and process science.
Benavides-Vaello, S., Strode, A., & Sheeran, B. C. (2013).
Using technology in the delivery of mental health and
substance abuse treatment in rural communities: A
review. The Journal of Behavioral Health Services &
Research, 40(1), 111-120.
Bousquet, C., Souvignet, J., Sadou, E., Jaulent, M. C., &
Declerck, G. (2019). Ontological and non-ontological
resources for associating MedDRA terms to SNOMED
CT concepts with semantic properties. Frontiers in
Pharmacology, 10, 975.
Braa, J., Sahay, S., Lewis, J., & Senyoni., W. (2017). Health
information systems in Indonesia: Understanding and
addressing complexity. IFIP Advances in Information
and Communication Technology. ISSN 1868-4238.
504, s 59- 70
Carvalho, J.V., Rocha, A., & Abreu, A. (2016). Maturity
models of healthcare information systems and
technologies: A literature review. Journal of Medical
Systems, 40 (6), 131.
Celi, L. A., Fraser, H. S., Nikore, V., Osorio, J. S., & Paik,
K. (Eds.). (2017). Global health informatics: Principles
of eHealth and mHealth to improve quality of care.
Cambridge, MA: The MIT Press. Available from
https://mitpress. mit.edu/books/global-health-
informatics.
Chang, V., Cao, Y., Li, T., Shi, Y., & Baudier, P. (2019,
May). Smart healthcare and ethical issues. In 1st
International Conference on Finance, Economics,
Management and IT Business (pp. 53-59). SciTePress.
Egwar, A., Ssekibuule, R. and Nabukenya, J. (2020). Status
of Resources for Information Technology to Support
Health Information Exchange in Resource-constrained
Settings: Case study of Uganda. 13th International Joint
Conference on Biomedical Engineering Systems and
Technologies, HEALTHINF, Vol 5: 463-471, ISBN:
978-989-758-398-8
Goossen, W., Goossen-Baremans, A., & Van Der Zel, M.
(2010). Detailed clinical models: a review. Healthcare
informatics research, 16(4), 201-214.
Greenwell, F., & Salentine, S. (2018). Health information
system strengthening: Standards and best practices for
data sources. Chapel Hill: MEASURE Evaluation,
University of North Carolina, 58-63.
Hammond, W., & Cimino, J. (2006). Biomedical
informatics. In E. Shortliffe & J. Cimino (Eds.),
Standards in biomedical informatics (pp. 265–311).
New York: Springer-Verlag.
Health Enabled. (2017). The global health digital health
index. Available at http://healthenabled.org/wordpress/
the-global-digital-health-index/. Accessed on
September 25, 2020
Henriksson, D. K., Peterson, S. S., Waiswa, P., &
Fredriksson, M. (2019). Decision-making in district
health planning in Uganda: does use of district-specific
evidence matter? Health research policy and systems,
17(1), 57.
Institute of Electrical and Electronics Engineers (2010).
IEEE Standard Computer Dictionary: A Compilation of
IEEE Standard Computer Glossaries. New York: The
Institute of Electrical and Electronics Engineers.
Jennett, P. A., Scott, R. E., Affleck Hall, L., Hailey, D.,
Ohinmaa, A., Anderson, C., ... & Lorenzetti, D. (2004).
Policy implications associated with the socioeconomic
and health system impact of telehealth: a case study
from Canada. Telemedicine Journal and E-health,
10(1), 77-83.
Kimaro, H.C. and Twaakyondo, H.M. (2005). Analyzing
the Hindrance to the Use of Information and
Technology for Improving Efficiency of Health Care
Delivery Systems in Tanzania. Tanzania Health
Research Bulletin 7, 189-197.
Knaup, P., Bott, O., Kohl, C., Lovis, C., & Garde, S. (2007).
Electronic patient records: moving from islands and
bridges towards electronic health records for continuity
of care. Yearb Med Inform, 2007, 34-46.
Kuperman, G. J., Gardner, R. M., & Pryor, T. A. (2013).
HELP: a dynamic hospital information system.
Springer Science & Business Media.
Lamine, E., Guédria, W., Rius Soler, A., Ayza Graells, J.,
Fontanili, F., Janer‐García, L., Pingaud, H. (2017). An
Inventory of Interoperability in Healthcare Ecosystems:
HEALTHINF 2021 - 14th International Conference on Health Informatics
210

Characterization and Challenges. Enterprise
Interoperability: INTEROP‐PGSO Vision, 1, 167-198
(2017).
Maguire, M. & Delahunt, B. (2017). Doing a Thematic
Analysis: A Practical, Step-by-Step Guide for Learning
and Teaching Scholars. AISHE-J, 3, 3351. Accessed at
http://ojs.aishe.org/index.php/aishe-
j/article/viewFile/335/553 on 25th January 2019.
Mandl, K. D., & Kohane, I. S. (2012). Escaping the EHR
trap—the future of health IT. N Engl J Med, 366(24),
2240-2242.
McDonnell, B. (2012) ACCF 2012 Health Policy Statement
on Patient-Centered Care in Cardiovascular Medicine.
A Report of the American College of Cardiology
Foundation Clinical Quality Committee
Measure Evaluation, (2019). Health Information Systems
Interoperability Maturity Toolkit: Users’ Guide
Version 1.0. Available at: https://www.measure
evaluation.org/resources/tools/health-information-
systems-interoperability-toolkit . Accessed August 15,
2020
MedDRA, M. S. S. O. (2015). MedDRA. Medical
Dictionary for Regulatory Activities.
Ministry of Health Uganda, (2014). The Health
Management Information System: Health Unit and
Community Procedure Manual 2014. 2014;1. Available
from: https://nutrition.opm.go.ug/wpcontent/
Ministry of Health, (2010). Uganda, The Second National
Health Policy: Promoting People’s Health to Enhance
Socio-Economic Development, 2010.
Ministry of Health, (2016). Uganda, Uganda National
eHealth Strategy 2016/2017-2020/202
Ministry of Health, (2017). Uganda, Uganda Population-
Based HIV Impact Assessment UPHIA 2016–2017,
2017.
Ministry of Health, Health Systems 20/20, Makerere
University School of Public Health. (2012) Uganda
Health System Assessment 2011. Kampala, Uganda
and Bethesda: MD: Health Systems 20/20 project, Abt
Associates Inc.
Ministry of Health, Uganda. (2017). Uganda National
eHealth Strategy 2016/2017—2020/2021.
Ministry of Health. (2016) Uganda eHealth Policy,
Kampala, Uganda.
Ministry of ICT (2011). Uganda ICT Policy. Uganda
Mukasa, E., Kimaro, H., Kiwanuka, A., & Igira, F. (2017).
Challenges and strategies for standardizing information
systems for integrated TB/HIV services in Tanzania: a
case study of Kinondoni municipality. The Electronic
Journal of Information Systems in Developing
Countries, 79(1), 1-11.
Oderkirk, J. (2017), "Readiness of electronic health record
systems to contribute to national health information and
research", OECD Health Working Papers, No. 99,
OECD Publishing, Paris, https://doi.org/10.1787/
9e296bf3-en.
PEPFAR, Data for Impact, 07-Jan-2011. Available:
https://www.pepfar.gov/priorities/data/index.htm. .
[Accessed: 10-September 10, -2019].
Saunders, M., Lewis, P. & Thornhill, A. (2012). Research
Methods for Business Students. 6
th
edition. Pearson
Education Limited
Teixeira, J. G., Patrício, L., Nóbrega, L., Constantine, L., &
Fisk, R. P. (2013, October). Healthcare professionals as
customers: A service perspective on Portuguese
primary care health information systems. In 2013 IEEE
15th International Conference on e-Health Networking,
Applications and Services (Healthcom 2013) (pp. 377-
381). IEEE.
Terhune, C., Epstein, K., & Arnst, C. (2009). The dubious
promise of digital medicine. Business week.
The Joint Commission. (2011). Comprehensive
accreditation manual for hospitals (updated September
2011). Oakbrook Terrace, IL: Author.
Trigo, J. D., Kohl, C. D., Eguzkiza, A., Martínez-
Espronceda, M., Alesanco, A., Serrano, L., ... & Knaup,
P. (2013). On the seamless, harmonized use of
ISO/IEEE11073 and openEHR. IEEE journal of
biomedical and health informatics, 18(3), 872-884.
Whitman, M. and Mattord, H. (2009), Principles of
Information Security, 3rd ed., Course Technology,
Boston, MA.
WHO, (2015) Measurement and Accountability for Results
in Health Summit, 9–11 June 2015. World Bank
Headquarters, Washington DC, USA
WHO, 2020. As accessed from https://www.who.int/
classifications/icd/en/. Accessed on 21
st
August 21,
2020.
World Health Organization & International
Telecommunication Union (2012). National eHealth
Strategy Toolkit. Geneva: WHO Press.
Yuksel, M., Gonul, S., Laleci Erturkmen, G. B., Sinaci, A.
A., Invernizzi, P., Facchinetti, S., ... & De Roo, J.
(2016). An interoperability platform enabling reuse of
electronic health records for signal verification studies.
BioMed Research International, 2016.
Establishing the State of Practice about Data Standards in Monitoring Healthcare Interventions for HIV in Uganda’s EMR-based Health
Information Systems
211
