
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit
Task and Its Analysis based on Heart Rate
Neide Simões-Capela
1,2
, Jan Cornelis
2
, Giuseppina Schiavone
3
and Chris Van Hoof
1,2
1
ESAT, KU Leuven, Kasteelpark Arenberg 10, Heverlee, Belgium
2
IMEC, Kapeldreef 75, Heverlee, Belgium
3
IMEC-NL, High Tech Campus 31, Eindhoven, The Netherlands
Keywords: Health Related Fitness, Cardio-respiratory Fitness, Submaximal Fitness Test, Ruffier-Dickson Task,
PhysioFit Task.
Abstract: Cardio-respiratory fitness (CRF) denotes the health of cardiorespiratory and musculoskeletal systems, thus
being important to evaluate effects of (un)healthy lifestyles. Non-exhaustive submaximal fitness tests enable
simple, fast, and inexpensive CRF assessment, in situations with low accuracy requirements. An example is
the Ruffier-Dickson task (RD), consisting of 30 squats executed within 45 seconds, it estimates a CRF score
from heart rate (HR) during the task. Squats, however, are not straightforward for subjects with poor fitness.
To overcome this limitation, we developed the PhysioFit task (PF). It entails two minutes of stationary
pedaling and employs HR for CRF estimation. PF outcomes were analyzed using RD as benchmark, according
to HR changes during the task; CRF scores estimated with methods based on HR; correlation of CRF scores
to body composition. The analysis relied on data from 28 subjects who executed both tasks. Although, HR
variations during PF were lower relative to RD, PF produced significant changes in HR during pedaling and
allowed for significant recovery after one minute. Significant agreement was found between tasks for two
CRF scores, and both presented strong negative and positive correlations with fat and muscle percentage,
respectively. Preliminary results show that PF is promising towards fast fitness assessments.
1 INTRODUCTION
Physical fitness describes how readily physical
activities can be performed, something that can be
defined in relation to health targets (i.e. health
related) or to a specific athletic skill (i.e. skill related).
The concept of health related fitness is the most
pertinent for the general population as it quantifies
diverse health aspects, namely body composition
(BComp); cardiorespiratory endurance; muscular
strength and endurance; and flexibility (McArdle,
Katch, & Katch, 2015). Nonetheless, accurate fitness
assessment is complex, expensive and has varied
health contraindications, being mainly limited to
athletes and specialized research. Simple and
affordable alternatives exist that can fit a wide range
of individuals, if a suboptimal accuracy is tolerated.
The work hereby presented is aimed at evaluating
the potential of a 2-min pedaling task, the PhysioFit
(PF), towards physical fitness assessment. The PF is
compared to the Ruffier-Dickson (RD) task, a simple
fitness test that relies on the execution of 30 squats to
attain a fitness evaluation, based on heart rate (HR)
during the exercise. The PF task offers an alternative
for situations in which the former is not feasible (e.g.
subjects with low weight or poor fitness). The
analysis methods developed for the RD task are
applied on PF task data, to test whether relevant
fitness information can be extracted. The article is
organized as follows. Chapter 1 introduces relevant
concepts related to fitness and summarizes the state-
of-the-art in data analysis. Chapter 2 details our
methods for data collection and analysis. Chapter 3, 4
and 5 present results, discussion, and conclusion,
respectively.
1.1 Body Composition
Body mass index (BMI) assesses the normalcy of a
person’s weight in relation to height, as in eq.1
(WHO, 2004).
BMI weight/height
(1
)
Analyzing BComp, a domain of health related
fitness, provides a more comprehensive assessment,
Simões-Capela, N., Cornelis, J., Schiavone, G. and Van Hoof, C.
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit Task and Its Analysis based on Heart Rate.
DOI: 10.5220/0010234503770385
In Proceedings of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2021) - Volume 5: HEALTHINF, pages 377-385
ISBN: 978-989-758-490-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
377

quantifying relative amounts of fat, muscle, and bone
in the body. The most convenient measurement
method uses bioimpedance analysis. Normal ranges
for each BComp component vary with age, gender,
ethnicity and measuring device (McArdle et al.,
2015).
1.2 Cardiorespiratory Fitness
Cardiorespiratory fitness (CRF) reflects the health of
the cardiovascular, respiratory, and musculoskeletal
systems. Thus, highly influencing the level to which
everyday aerobic activities can be performed (Arena
et al., 2007). Tough, its major interest lies on the
inverse correlation to morbidity and mortality
(Kodama et al., 2009). Several testing methodologies
and descriptors are available for CRF assessment, and
they are summarized next.
CRF testing comprises maximal and submaximal
fitness tests. In maximal tests the exercise workload
is incrementally increased until the test subject
achieves volitional exhaustion. These tests provide
the most accurate assessments. Though, they have
limited applicability on the general population related
to health contraindications (Thompson, Arena, Riebe,
and Pescatello, 2013). Their widespread use is also
limited by the requirements for specialized medical
supervision, on-site emergency equipment, specific
training, and elaborated protocols requiring
expensive acquisition setups. Submaximal tests, on
the other hand, do not require subjects to reach
exhaustion. With less contraindications, they are
suited for a wider range of individuals (e.g. children,
elderly), and the varied acquisition protocols
available meet different user requirements. Overall,
submaximal tests present a convenient alternative to
the maximal counterparts in situations with low CRF
accuracy requirements (e.g. home, primary care,
general research).
The golden standard for CRF assessment is the
maximal oxygen uptake (VO
2max
), achieved when
consumed oxygen reaches a plateau, despite an
increase in exercise load (i.e. when reaching
exhaustion). It can be directly accessed by ventilatory
gas analysis (Fletcher et al., 2013). CRF categorical
classifications (e.g. very poor, poor, fair...) based on
VO
2max
are provided by the American College of
Sports and Medicine (ACSM) (ACSM, 2014).
Gender, age, height, body size/composition, training
status and type of testing protocol all influence the
VO
2max
value (Fletcher et al., 2013). Height is
especially important when the center of mass is
displaced during the test protocol (McArdle, Katch,
and Katch, 2015).
One CRF correlate that is easier to assess is HR.
HR at rest (HR
rest
) is a general indicator of wellness,
while a decline in the HR response to submaximal
exercise represents an enhancement in endurance.
Also, the HR recovery pattern is a mortality predictor
(ACSM, 2014). HR reaches its maximum (HR
max
)
approximately when VO
2max
is achieved. For an
increasing exercise load, HR increases linearly with
oxygen consumption (VO
2
). The relation holds
during light to moderate workloads but may degrade
for high workloads as VO
2
accelerates. The linearity
of the HR-VO
2
relation has been used to predict
VO
2max
in submaximal tasks, by applying a linear
regression to known points and extrapolating the
relation up to a theoretical HR
max
. Due to the
assumptions put into this prediction, the estimated
value is usually
within 10-20% of the actual VO
2max
.
Some authors refer that this accuracy level is
unacceptable for research, but can still be valuable in
lifestyle applications (e.g. screening at the gym)
(McArdle et al., 2015). Likewise, we argue that for
non-fitness specific research, such estimates can be
useful.
VO
2max
has been derived from HR
rest
, HR
max
and
weight as in eq.2 (N. Uth, 2005). The conversion to
relative units (mL/min.kg) is required for comparison
with guidelines and among subjects, which is
achieved by multiplying by 1000/weight. In eq.2 the
proportional factor (pf) takes different values for
women and men: 14.5x10
-3
l/min.kg and 15.3x10
-3
l/min.kg, respectively. Theoretical HR
max
(HR
max,th
)
can be estimated from eq.3 (Tanaka, Monahan, &
Seals, 2001). Variations to this formulation are
available, though no agreement exists on which is
generally preferable (ACSM, 2014).
VO
,
weight pf H
R
H
R
(2
)
H
R
,
208 0.7 age
(3
)
1.2.1 Ruffier-Dickson Task
The RD task is one of the simplest submaximal tasks
found in the literature. It consists on resting for 5 min,
performing 30 squats over a period of 45 s, and
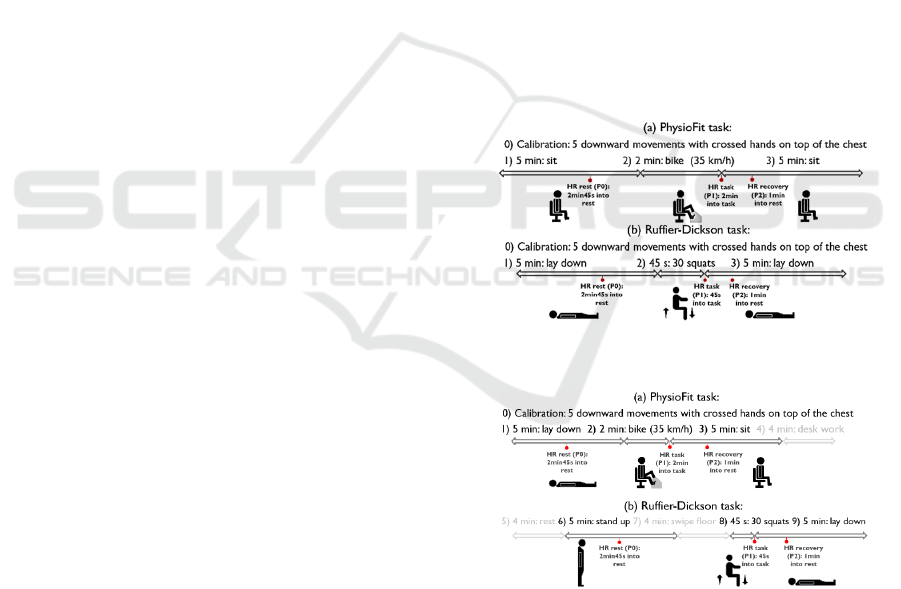
recovering for 5 min (Figure 2 (b)). The basic setup
requires a stopwatch and a mat to lay down during
rest and recovery. Bilateral squatting, involved in the
task, primarily activates lower body musculature, but
spinal and abdominal muscles are also engaged
(Eliassen, Saeterbakken, & van den Tillaar, 2018).
While early literature on the design of this task is not
accessible online, recent studies compared the RD
task results against maximal fitness tests and
HEALTHINF 2021 - 14th International Conference on Health Informatics
378
formulated predictive VO
2max
models.
The RD task analysis traditionally relies on three
discrete HR values: at rest (P0), right after exercise
(P1) and 1 min into recovery (P2). A reference for the
expected values is presented in Table 1. Such values
are employed in calculating numerical fitness scores,
such as the Ruffier index (Ri, eq.4) or the latter
Ruffier-Dickson index (RDi, eq.5). The choice of
factors in Ri and RDi is explained by De Mondernard
et al. (De Mondenard, 1987), showing an ad-hoc
process with weak empirical validation. Numerical
outputs of Ri and RDi can be translated to fitness
categories (e.g. excellent, good, fair...) as described in
previous literature (De Mondenard, 1987)(Dah,
1991)(Sartor et al., 2016), though the classification
ranges vary. The interest of Ri and RDi scores in
fitness evaluation was re-evaluated in recent studies,
that examined their relation to VO
2max
measured
during maximal tasks in healthy individuals.
Table 1: RD task: expected HR at rest, maximum steady
state during exercise and 1 min into recovery (De
Mondenard, 1987).
P0: Rest P1: Ada
p
tion P2: Recover
y
P0<50 bpm: good
Basal endurance.
P0>80 bpm: poor
b
asal endurance.
P1<2P0: good condition.
P1>2P0: insufficient
training.
P2≤P0: very good/good
endurance.
P2>P0+20: insufficient
trainin
g
.
Ri P0 P1 P2 200 10
⁄
(4)
RDi
P1 70
2P2P0 10
⁄
(5)
Sartor et al. (Sartor et al., 2016) shown that RDi alone
should not be used to classify CRF levels in healthy
subjects: the index shown low agreement
(kappa=0.29) to ACSM CRF categorical levels and
explained only 15% of the variability (adjusted
r
2
=0.15, sensitivity for good and fair=61%,
specificity for poor=49%). Including RDi, age,
gender (0=female, 1=male) and height on a
multivariate model (eq.6), enhanced the agreement
with ACSM levels (kappa=0.39) and the explained
variability to 53% (adj. r2=0.53, sensitivity for good
and fair=62%, specificity for poor=63%). These
authors developed other models using HR values
other than P0, P1 and P2. In our view, the increase in
complexity did not justify the performance
enhancement (adj. r
2
=0.59, sensitivity for good and
fair=64%, specificity for poor=62%, kappa=0.42),
thus, those models are not detailed here. The models
were developed on data from 81 healthy subjects (18
F, 63 M), with age ∈[18, 67] years old, height ∈[1.61,
1.88] m, weight ∈[52.5, 100] kg, and BMI ∈[18.8,
33.6] kg/m
2
.
VO
,
3.79 0.56gender
0.03age 4.53heigh
0.09RDi
(6
)
Guo et al. (Guo et al., 2018) developed three models
to predict VO
2max
, respectively based on Ri, RDi and
HR values (P0, P1, P2). Neither Ri (p= 0.06) nor RDi
(p= 0.32) were significant predictors of VO
2max
. The
best model (eq.7) was found using P0, P1, P2, age,
gender (0=female, 1=male,) and height (adj. r
2
=0.64,
sensitivity for good and fair=79%, specificity for
poor=56%, kappa = 0.6). The models were developed
on 40 healthy subjects (22 F, 18 M), age ∈[19, 60]
years old, height ∈[1.57, 1.93] m, weight ∈[49.9,
121.6] kg, BMI ∈[18.6, 41.2] kg/m
2
, P0 ∈[49, 98]
beats per minute (bpm), P1 ∈[101, 184] bpm, and P2
∈[56, 152] bpm.
VO
,
3.014 1.16gender
0.03
P0
height
118.76
P1 P2
age
(7
)
To calculate their performance metrics, both
Sartor et al. (Sartor et al., 2016) and Guo et al. (Guo
et al., 2018) used three CRF classes (i.e. poor, fair and
good), adapted from ACSM’s classification for
VO
2max
during the Balke treadmill protocol (ACSM,
2014).
1.2.2 PhysioFit Task
The PF task is a submaximal task comprising 5 min
of rest while sitting, 2 min pedaling and 5 min of sited
recovery (Figure 1(a)). Pedaling is performed in
upright seated position on a stationary bike with a
fixed gear, with the objective of attaining and
maintaining 35 km/h.
The setup requires a chair, a
stopwatch, and a stationary minibike (i.e. without
upper limb support). The pedaling activity primarily
activates lower body musculature and secondarily
arm, abdominal and back muscles when upper limbs
are used for support (So, Ng, and Ng, 2005). The
muscle activation is a close match to the RD task, an
important factor when comparing both tasks, as
VO
2max
values predicted from upper and lower body
exercises have low correlation (McArdle et al., 2015).
The PF task was thought to cater for varied levels
of fitness, accounting for some individuals being
unable to perform or repeat complex movements (e.g.
squats, step-up/down); while keeping the setup
portable (i.e. excluding treadmills or a bicycle
ergometers) and affordable (minibike prices range
from 20-200 euros, depending on brand); and
excluding tasks requiring the test subject to leave the
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit Task and Its Analysis based on Heart Rate
379
controlled experimental environment to perform
them (e.g. field walk, run tests). This task was first
employed in psychophysiological research related to
eating disorders, as a physical stressor (Simões-
Capela, Schiavone, De Raedt, Vrieze, & Van Hoof,
2019). The aim was to weight the effect of physical
activity on bio signals, when primarily studying the
effects of mental stress on the body.
2 METHODS
2.1 Data
The PF and RD tasks were compared based on data
from two studies, in which volunteers with varied
levels of fitness completed both tasks.
Dataset 1 results from a pilot study designed to
compare both tasks, following standard task
protocols. The study was reviewed and approved by
the medical ethics committee of Ziekenhuis Oost-
Limburg. The study sample consisted of 13 subjects
(7M, 6F) from a working population with
age=30.4±7.2 years and BMI=22.3±4.3 kg/m
2
(mean
± s. dev.). All agreed to voluntarily participate and
consented to the data collection after an explanation
of the study procedures. All subjects were older than
18 years and working on a day desk job (i.e. excluding
physical exertive jobs and shift works). The following
constituted exclusion criteria: sensitive skin or known
allergy to Ag/AgCl electrodes; inability to perform
the protocol (e.g. limited mobility, respiratory illness,
cardiovascular illness); acute illness (e.g. flu);
pregnancy; and carrying implanted devices. The
participants interfaced with three devices: 1) Health
Patch (imec/Biotelemetry), a sensing node attached to
an adhesive chest patch, used to continuously capture
ECG; 2) HBF-516 (Omron), a full BComp monitor,
to measure weight and estimate fat and muscle
percentages based on bio-impedance analysis; 3) low-
cost uncalibrated minibike (crivit, LIDL), used during
the workout. The minibike was compared to a
calibrated device (deskcycle, 3Dinnovations) to attest
the accuracy of its displayed velocity, and an error of
10km/h was found (i.e. 35km/h displayed as
3.5km/h). This was taken in consideration during data
collection. The tasks (Figure 1) were conducted in a
dedicated study room under the supervision of trained
researchers. The tasks were performed at the same
time (between 3h and 5h pm) on consecutive days to
avoid circadian changes. The task order was
randomized. At the first contact the admission criteria
were verified and background information (i.e. age,
gender, height, weight, and BComp parameters) was
collected. After applying the wearable sensors, the
tasks took place as depicted in Figure 1, while a timed
slideshow presentation with directions was shown on
screen for reference. A screen recording was
captured, to document any time diversions and
account for them in the analysis.
Dataset 2 was originally dedicated to test the
effect of diverse activities on bio-signal quality, and
its methods include slight variations from Dataset 1.
It was incorporated here to extend the study sample.
The study was reviewed and approved by the medical
ethics committee of Universiteit Ziekenhuis Leuven.
The study sample consists of 15 subjects (5 M, 10 F)
from a working population, with age=34.2±10.3
years and BMI=22.4±3.1 kg/m
2
(mean ± s. dev.). The
admission criteria, the ECG acquisition device and
bike setup were the same as in Dataset 1. The body
analyzer was not employed. All procedures (Figure 2,
with relevant tasks highlighted) were performed on a
single 90 min study session between 8h and 12h am.
In contrast to Dataset 1, there was no randomization
of the task order. Weight and height were self-
reported.
Figure 1: Task protocol for Dataset 1: (a) PF task and (b)
RD task.
Figure 2: Task protocol for Dataset 2: (a) PF task and (b)
RD task. Highlighted time slots were considered in the
analysis.
2.2 Analysis
The analysis entailed: 1) pre-processing; 2)
investigation of HR at P0, P1 and P2; 3) obtention of
CRF scores using HR based models found in previous
literature for the RD task; and 4) comparison of CRF
HEALTHINF 2021 - 14th International Conference on Health Informatics
380
scores to BComp. The previous steps were applied on
data from both task, and results were compared within
and between tasks. The analysis was carried out using
MATLAB 2019b. All correlations were analyzed
considering Cohen’s guidelines (low correlation:
|ρ|≤0.3; moderate correlation: 0.3<|ρ|<0.5; strong
correlation: |ρ|≥0.5).
ECG signals from each subject were truncated to
the interval from start to end of each task. The start of
each task was identified by the acceleration signature
produced by the calibration procedure. Remaining
phases were annotated based on the timings from the
screen recordings. The R-peaks were identified in the
ECG signal using an automatic beat detector
(Romero, Grundlehner, & Penders, 2009). HR was
calculated based on R-R intervals and converted to
bpm. Each 1-min window was assessed for outliers
(i.e. values outside the interval of mean HR ± 2.5 s.
dev.) and these points were excluded.
Each of the relevant HR values was obtained by
calculating the median of 15 seconds following the
P0, P1 and P2 time points (cf. Figur
e
1 and Figure 2).
Median HR values were used to reduce the effect of
outliers. In both tasks it was investigated if changes
in HR from rest to adaption, from adaption to
recovery and from rest to recovery were significant.
Among tasks, the HR values at each phase and the
absolute HR variation from phase to phase were
compared.
For both tasks, CRF scores were estimated based
on 6 indices: Ri (eq.4), RDi (eq.5), VO
2max,sartor
(eq.6),
VO
2max,guo
(eq.7), VO
2max,uth
(eq.2) and VO
2max,uth,th
(eq.2, eq.3). In VO
2max,uth
, the HR
max
was substituted
by P1, in the expectation it would produce a
proportional estimation. All outputs in units of L/min
were translated to relative units of ml/kg.min. In both
tasks the agreement between each pair of CRF indices
was studied. Among tasks, the agreement among CRF
values was tested.
The correlations of HR and CRF scores to BComp
and BMI were investigated. Since only Dataset 1
includes information on BComp this analysis was
limited to those 13 subjects.
3 RESULTS
This section includes results from the comparative
analysis of HR and CRF scores within each task and
among tasks. For most part of the analysis, Dataset 1
and 2 were treated as a single dataset, after visually
verifying that both had a similar HR behavior (Figure
3). Background information of the study sample is
summarized in Table 2.
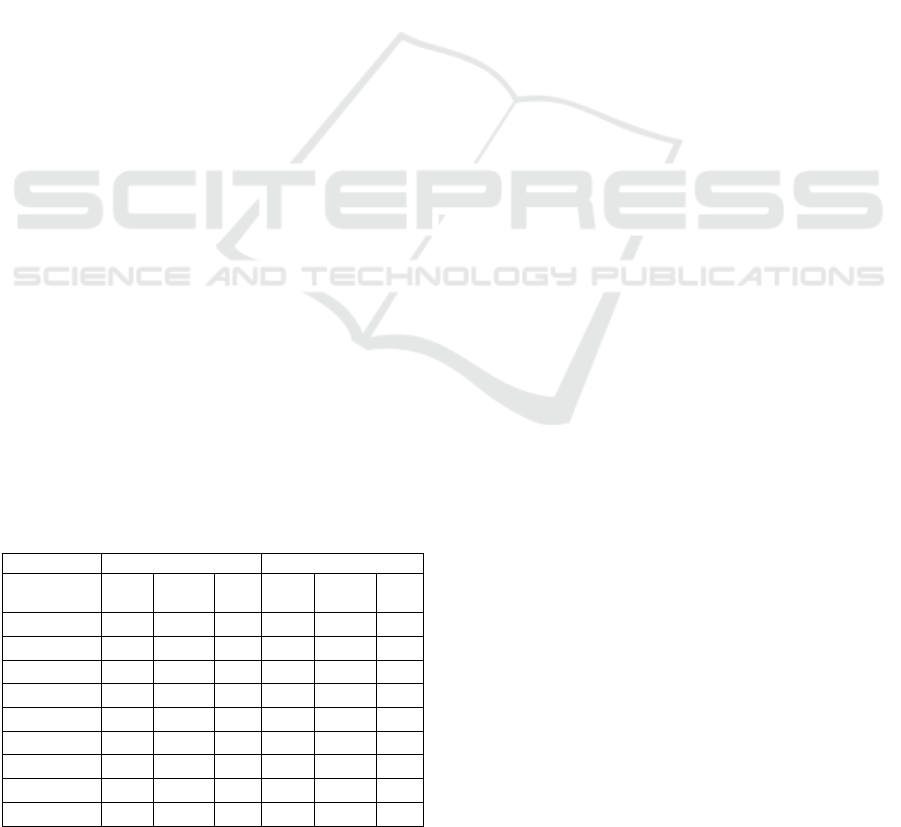
Table 2: Study sample: demographics and anthropometrics
(mean ± s. dev. [max, min]).
Male (N=12) Female (N=16) All (N=28)
A
ge, years
32.3 ± 5.6 [25, 44] 32.5 ± 11.2 [18, 52]
32.4 ± 9.1
[18, 52]
H
eight, m
1.83 ± 0.12 [1.69, 2.05] 1.65 ± 0.05[1.57,1.76]
1.73 ± 0.12
[1.57, 2.05]
W
eight, kg
78.6 ± 19.0 [54.6,117.5] 59.7 ± 11.0 [43, 92]
67.8 ± 17.4
[43, 117.5]
B
MI, kg/m
2
23.2 ± 4.3 [18.4, 35.5] 21.7 ± 3.0 [16.4,29.7]
22.4 ± 3.6
[16.4, 35.5]
3.1 HR Intra and Inter-task
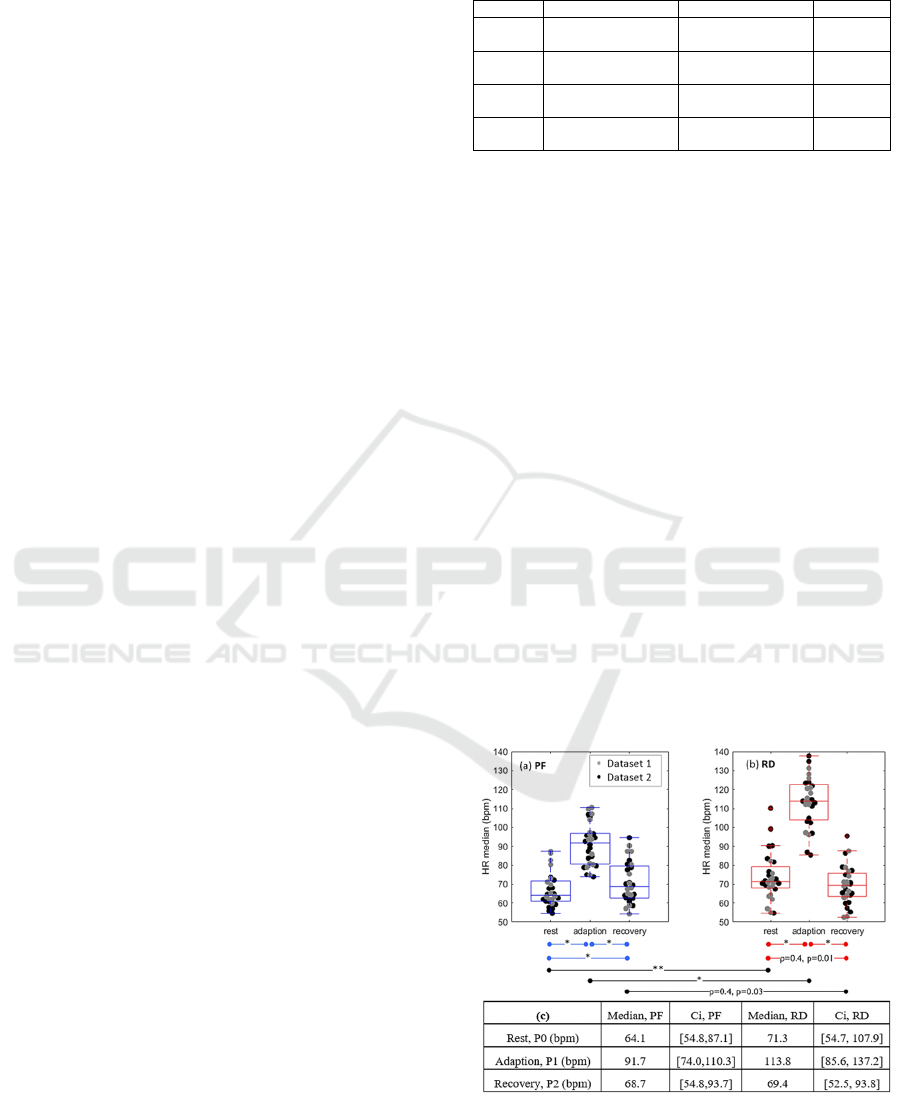
The distributions of P0, P1 and P2 are depicted in
Figure 3, for both tasks. Based on the Kolmogorov-
Smirnov (KS) normality test, all HR distributions are
right-skewed, for such we used non-parametric
statistics in the analysis. Data was not transformed to
a normal distribution in order not to omit outliers. The
Wilcoxon signed-rank test for dependent variables
was employed to find significant differences. For
non-significant differences, the presence of a linear
relation was investigated based on Spearman’s test.
In both tasks, there are significant differences
between rest and adaption (z=-4.6, p<<0.01 for PF
and z=-4.6, p<<0.01 for RD) and between adaption
and recovery (z=4.6, p<<0.01 for PF and z=4.6
p<<0.01 for RD). Differences between rest and
recovery are significant for the PF task (z=-2.9,
p<0.01), but not for RD (z=1.36, p=0.17), in which
case a significant moderate correlation is found
(ρ=0.4, p=0.01). The absolute variations in HR
median
from rest to adaptation are 27.6 bpm and 42.5 bpm,
and from adaption to recovery are 23.0 bpm and 44.4
bpm, respectively for PF and RD task.
Figure 3: HR at rest (P0), adaption (P1) and recovery (P2):
(a) PF task, (b) RD task, (c) statistics. Significant
differences indicated with * (p<0.01) or ** (0.01≤p-
value<0.05), otherwise Spearman’s ρ and p-value are
shown. Ci: 95% confidence interval.
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit Task and Its Analysis based on Heart Rate
381
Across tasks, the HR is significantly different during
rest (z=-2.4, p=0.02) and adaption (z=-4.6, p<<0.01),
but not during recovery (z=1.0, p=0.3), presenting a
significant moderate correlation in this case (ρ=0.4,
p=0.03).
3.2 CRF Intra and Inter-task
All CRF scores’ distributions are right skewed
according to the KS normality test, hence non-
parametric statistics were used in the analysis. The 6
CRF indices have different scales, and vary
differently with an increasing level of fitness: Ri and
RDi tend to -∞, while VO
2max,sartor
,
VO
2max,guo
,
VO
2max,uth
and
VO
2max,uththeory
tend to +∞. In this case a
test to compare medians is not appropriate. Thus, the
relation among CRF indices’ output was investigated
using regression.
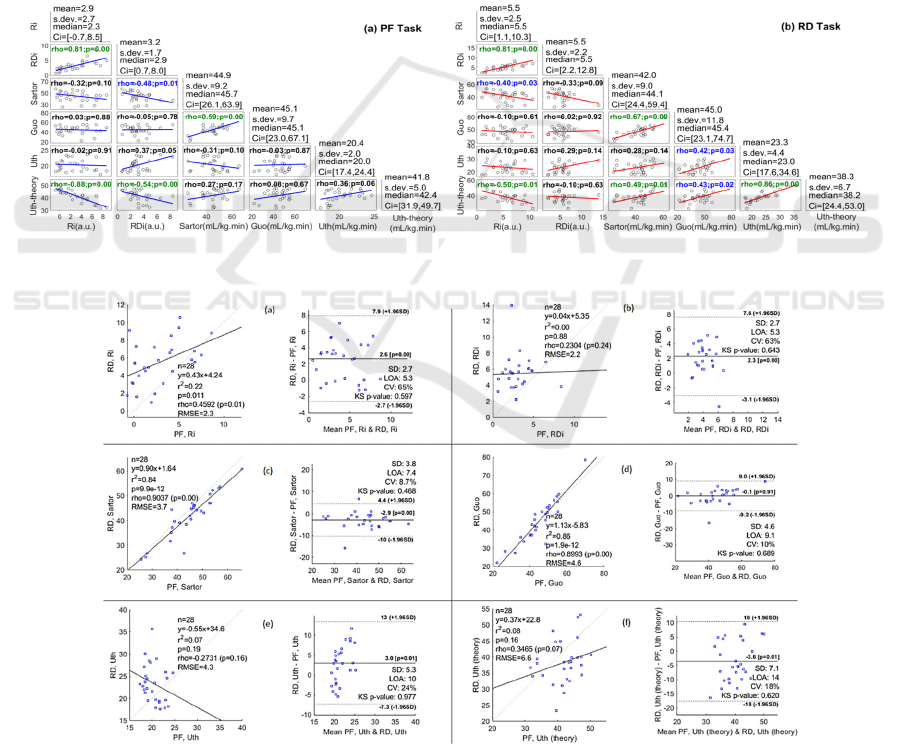
The linear regression between each pair of CRF
indices (i.e. Ri-RDi, Ri-VO
2max,sartor
, Ri-VO
2max,guo
...)
was calculated (Figure 4). For the PF task, four pairs
of algorithms presented significant strong correla-
tions: Ri-RDi (ρ=0.81, p>>0.01), Ri-VO
2max,uththeory
(ρ=-0.88, p>>0.01), RDi-VO
2max,uththeory
(ρ=-0.54,
p>>0.01) and VO
2max,sartor
-VO
2max,guo
(ρ=0.59,
p>>0.01). For the same task, a moderate correlation
was found for RDi-VO
2max,sartor
(ρ=-0.48, p=0.01). For
the RD task, a significant strong correlation was
found for five pairs: Ri-RDi (ρ=0.81, p>>0.01), Ri-
VO
2max,uththeory
(ρ=-0.5, p=0.01), VO
2max,sartor
-
VO
2max,uththeory
(ρ=0.49, p=0.01), VO
2max,sartor
-
VO
2max,guo
(ρ=0.67, p>>0.01) and VO
2max,uth
-
VO
2max,uththeory
(ρ=-0.86, p>>0.01). For the same task,
Figure 4: Linear relations between CRF indices for (a) PF task; (b) RD task. rho: Spearman’s ρ, p: p-value, s. dev: standard
deviation, Ci: 95% confidence interval. Significant correlations marked in green (p<0.01) or blue (0.01≤p-value<0.05).
Figure 5: Linear regression of CRF scores from PF task against RD task and differences’ plot for: (a)Ri, (b) RDi, (c)
VO
2max,sartor
, (d)VO
2max,guo
, (e)VO
2max,uth
and (f)VO
2max,uth theory
. n: number of points, y: regression formula, r
2
: coef. of
determination, p: Pearson’s correlation p-value, rho (p): Spearman’s ρ and p-value, RMSE: root mean squared error, SD: s.
dev., LOA: limits of agreement (±1.96 s. dev.), presented as dashed lines, CV: coef. of variation (s. dev./mean in %), KS p-
value: p-value for Kolmogorov-Smirnov test.
HEALTHINF 2021 - 14th International Conference on Health Informatics
382
a moderate correlation was found for three pairs: Ri-
VO
2max,sartor
(ρ=-0.40, p=0.33), VO
2max,guo
-
VO
2max,uththeory
(ρ=-0.43, p=0.02) and VO
2max,guo
-
VO
2max,uththeory
(ρ=0.42, p=0.03). Only three pairs of
algorithms correlate well in both PF and RD tasks.
Regression analysis was used to investigate
proportionality among CRF scores from different
tasks. To understand if the relations found were
significant the analysis of differences (Bland &
Altman, 1999) was performed on the residuals
(Figure 5), which is more robust to compare different
acquisition methods than simple correlation. Three
CRF indices shown significant agreement between
tasks: Ri with moderate correlation (ρ=0.4, p=0.01);
VO
2max,sartor
(ρ=0.9, p<<0.01) and VO
2max,guo
(ρ=0.9,
p<<0.01) with strong correlation. All residuals
arenormal (KS p-value>0.05), hence the results from
regression are trustworthy. There is a systematic error
between PF and RD for 5 CRF indices, as illustrated
by the significant proportional bias on Ri (bias=2.6,
p>>0.01), RDi (bias=2.3, p>>0.01), VO
2max,sartor
(bias=-2.9, p>>0.01), VO
2max,uth
(bias=3.0, p=0.01),
and VO
2max,uththeory
(bias=-3.6, p=0.01). As for
VO
2max,guo
(bias=-0.1, p=0.91) the bias is not
significant. Ri and RDi have similar limits of
agreement, both indicating a wide variability of the
residuals. The VO
2max,sartor
(in comparison to
VO
2max,guo,
VO
2max,uth
and VO
2max,uththeory
) presented
the narrowest limits of agreement for the differences
between tasks (LOA=7.4). The models with least
dispersion of the residuals are VO
2max,sartor
(CV=8.7%) followed by VO
2max,guo
(CV=10%).
3.3 BMI and Body Composition
For Dataset 1 (N=13), correlations of P
0,1,2
and CRF
scores to BMI, muscle and fat percentages were
investigated based on Spearman’s correlation test.
Significant correlations are highlighted in Table 3.
Table 3: Correlation among CRF indices and
anthropometrics for: (a) PF task, (b) RD task. Significant
correlations marked with *(p<0.01) or **(0.01≤p-
value<0.05).
(a) PF task (b) RD task
BMI Muscle
%
Fat % BMI
Muscle
%
Fat %
0 0.29 -.12 0.12 0.20 -.63** 0.48
P1 0.27 -.57** 0.46 -.35 -.02 -.15
P2 0.42 -.19 0.24 0.52 -.38 0.59
Ri 0.28 -.36 0.27 0.30 -.59** 0.54
RDi 0.31 -.48 0.43 0.07 -.18 0.20
VO
2max,sartor
-.56 0.92* -.92* -0.52 0.90* -.90*
VO
2max,guo
-.66** 0.64** -.84* -.60** 0.66* -.83*
VO
2max,uth
0.08 -.05 0.03 -.24 0.43 -.39
VO
2max,uththeory
-.22 0.26 -.19 -.16 0.70* -.51
4 DISCUSSION
All HR distributions are right-skewed, which is a
common find in HR literature, occurring whenever
the sample as a subgroup of tachycardic subjects
(Palatini, 1999).
For the intra-task comparison, we found that both
tasks produce statistically and physiologically
significant changes in HR from rest to adaption and
both show significant recovery after adaption. In the
RD task, HR at rest and HR during recovery have a
significant moderate correlation. As for the PF task
HR at rest and during recovery are significantly
different.
For the HR inter-task comparison only HR during
recovery agrees across tasks, presenting a significant
moderate correlation. HR at rest can naturally change
across measurements related to diet and activity prior
to the measurement and acute changes in emotional
state. Nonetheless, HR at rest is systematically higher
for the RD task. In the current work, it is difficult to
evaluate if body position (McArdle et al., 2015) is the
reason for the difference, as Dataset 1 and Dataset 2
present varied resting positions. It is also possible that
recovery is insufficient as the resting phase in Dataset
2 takes place after other activities. During adaption it
is noted that pedaling leads to a significantly lower
peak HR (less 22.1 bpm) than the squats, each
producing a median variation in HR from rest to
adaption of 27.6 bpm and 42.5 bpm, respectively.
Such difference is unlikely due to body position, as
this can only account for HR in PF (sitting) being
systematically lower than RD (standing) by 1 bpm
(McArdle et al., 2015) (Figure 3). During recovery
there is a significant moderate correlation in HR
across tasks, which could mean that the HR braking
system acts to bring HR back to a baseline level,
independently of the intensity of the physical stressor.
Related to different body positions during recovery,
HR in PF (sitting) should be systematically higher
than RD (laying down). This should not invalidate the
correlation found, though the ~1 bpm systematic error
was not accounted in the calculation.
In the CRF intra-task comparison, we verified that
not all models are consistent in the CRF score
obtained for the same task (
Figure 4). This does not
appear to be a problem specific of the PF task: only 5
and 8 out 15 pairs of models agree for PF and RD,
respectively. The discrepancies can be attributed to
the different variables and their weight in each model.
For CRF inter-task comparison, two models
shown to be consistent across tasks: VO
2max,guo
with
no significant bias and VO
2max,sartor
systematically
estimating higher fitness levels for the PF task (
Figure
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit Task and Its Analysis based on Heart Rate
383

5). Unsurprisingly Ri and RDi shown poor agreement,
as expected from their low rating as CRF predictors
in previous literature (Sartor et al., 2016)(Guo et al.,
2018). Finally, we verified that outputs from both
VO
2max,guo
and VO
2max,sartor
agreed with other fitness
indicator. With both presenting strong positive
correlation with muscle percentage, and strong
negative correlation with fat percentage (Table 3).
As the two different fitness tasks agree on the
CRF scores obtained from two models that have been
independently developed, and those scores agree with
other fitness indicator (BComp), we illustrate the
potential of our task for rough CRF estimation.
Nonetheless, these are preliminary results and we are
aware of the limitations of the current work. Dataset
2 presents design flaws related to the objectives this
investigation, such as the incongruence of body
positions with Dataset 1. We compare our task results
to another submaximal task, while the correct
approach towards validation is the comparison
against a golden standard. Submaximal tests are
especially useful for intra-subject comparison, over
repeated measurements, which excludes
reproducibility issues that are present across subjects.
Our datasets present cross-sectional designs,
preventing this analysis. Also, test-retest variability
was not addressed. These limitations constitute points
for further investigation.
5 CONCLUSIONS
We propose the PhysioFit, a simple 2-min pedaling
task for fitness assessment, suited for subjects with
low fitness level. We show that it induces a
significant change in HR. We identify two models
from previous literature (Sartor et al., 2016) (Guo et
al., 2018) that can be used to analyze it, and obtain
fitness scores based on HR during the task. CRF
scores obtained from both models shown strong
agreement with body composition indices. We reckon
that this task is no match for settings requiring high
accuracy assessments. Though, it has potential for
rough fitness indexation in lifestyle and wellbeing
applications (e.g. routine health checkups, tracking
training progress or diet) or in non-fitness specific
research studying human physiology (e.g.
psychophysiology). With this work we intend to
inspire the periodical monitoring of fitness levels in
individuals who only casually engage in physical
activity, be it in research studies, in the general
practitioner’s office, at home or in the work
environment.
ACKNOWLEDGEMENTS
The authors acknowledge their gratitude to Emma
Laporte for a preliminary literature review on fitness
tasks; Erika Lutin and Christophe Smeets for
reviewing the study materials; Luc Hons and Pieter
Vandervoort for clinical supervision; and Leen
Tordeurs for data management.
REFERENCES
ACSM. (2014). ACSM’s Guidelines for Exercise Testing
and Prescription 9th Ed. 2014.
Arena, R., Myers et al. (2007). Assessment of Functional
Capacity in Clinical and Research Settings.
Circulation, 116(3), 329–343.
Bland, J. M., & Altman, D. G. (1999). Measuring
agreement in method comparison studies. Statistical
Methods in Medical Research, 8(2), 135–160.
Dah, C. (1991). Evaluation de l’aptitude physique. Intérêt,
méthodes et application pratique. Médecine d’Afrique
Noire, 38(10), 681–687.
De Mondenard, J. J. (1987). Test des flexions de Ruffier-
Dickson. Ann. Kinésithér., (14), 381–388.
Eliassen, W., Saeterbakken, A. H., & van den Tillaar, R.
(2018). Comparison of Bilateral and Unilateral Squat
Exercises on Barbell Kinematics and Muscle
Activation. International Journal of Sports Physical
Therapy, 13(5), 871–881.
Fletcher, G. F. et al. (2013). Exercise standards for testing
and training. Circulation, 128(8), 873–934.
Guo, Y. et al. (2018). A 3-minute test of cardiorespiratory
fitness for use in primary care clinics. PLoS ONE,
13(7), 1–11.
Kodama, S. et al. (2009). Cardiorespiratory fitness as a
quantitative predictor of all-cause mortality and
cardiovascular events in healthy men and women: A
meta-analysis. Journal of the American Medical
Association, 301(19), 2024–2035.
McArdle, W. ., Katch, F. I., & Katch, V. L. (2015). Exercise
Physiology: Energy, Nutrition and Human
Performance, 8th edition.
Palatini, P. (1999). Need for a Revision of the Normal
Limits of Resting Heart Rate. Hypertension, 33(2),
622–625.
Romero, I., Grundlehner, B., & Penders, J. (2009). Robust
beat detector for ambulatory cardiac monitoring.
Proceedings of the 31st Annual International
Conference of the IEEE Engineering in Medicine and
Biology Society: Engineering the Future of
Biomedicine, EMBC 2009, 950–953.
Sartor, F. et al. (2016). A 45-second self-test for
cardiorespiratory fitness: Heart rate-based estimation in
healthy individuals. PLoS ONE, 11(12).
Simões-Capela, N., Schiavone, G., De Raedt, W., Vrieze,
E., & Van Hoof, C. (2019). Toward Quantifying the
Psychopathology of Eating Disorders From the
HEALTHINF 2021 - 14th International Conference on Health Informatics
384

Autonomic Nervous System Perspective: A
Methodological Approach. Frontiers in Neuroscience,
13(JUL), 1–12.
So, R. C. H., Ng, J. K.-F., & Ng, G. Y. F. (2005). Muscle
recruitment pattern in cycling: a review. Physical
Therapy in Sport, 6(2), 89–96.
Tanaka, H., Monahan, K. D., & Seals, D. R. (2001). Age-
predicted maximal heart rate revisited. Journal of the
American College of Cardiology, 37(1), 153–156.
Thompson, P. D., Arena, R., Riebe, D., & Pescatello, L. S.
(2013). ACSM’s New Preparticipation Health
Screening Recommendations. Current Sports Medicine
Reports, 12(4), 215–217.
Uth, N. (2005). Gender difference in the proportionality
factor between the mass specific V
̇
O2max and the ratio
between HRmax and HR rest. International Journal of
Sports Medicine, 26(9), 763–767.
WHO. (2004, June 26). Body mass index. Retrieved June
26, 2020, from https://www.euro.who.int/en/health-
topics/disease-prevention/nutrition/a-healthy-lifestyle/
body-mass-index-bmi
A 2-minute Fitness Test for Lifestyle Applications: The PhysioFit Task and Its Analysis based on Heart Rate
385
