
MIPHAS: Military Performances and Health Analysis System
Gennaro Laudato
1
, Giovanni Rosa
1
, Simone Scalabrino
1,2
, Jonathan Simeone
2
, Francesco Picariello
3
,
Ioan Tudosa
3
, Luca De Vito
3
, Franco Boldi
4
, Paolo Torchitti
4
, Riccardo Ceccarelli
5
,
Fabrizio Picariello
6
, Luca Torricelli
6
, Aldo Lazich
7
and Rocco Oliveto
1,2
1
STAKE Lab, University of Molise, Pesche (IS), Italy
2
Datasound SRL, Pesche (IS), Italy
3
LESIM lab, University of Sannio, Italy
4
XEOS, Roncadelle (BS), Italy
5
Formula Medicine, Viareggio (LU), Italy
6
TexTech Technologies, Reggio Emilia (RE), Italy
7
Ministero della Difesa, Roma (RM), Italy
{fpicariello, ioan.tudosa, devito}@unisannio.it, {f.picariello, l.torricelli}@textechtechnologies.com,
{franco.boldi, paolo.torchtti}@xeos.it, riccardo.ceccarelli@formulamedicine.com, aldo.lazich@marina.difesa.it
Keywords:
Wearable Devices, Machine Learning, Healthcare, Decision Support System.
Abstract:
In the last few years wearable devices are becoming always more important. Their usefulness mainly lies in the
continuous monitoring of vital parameters and signals, such as electrocardiogram. However, such a monitoring
results in an enormous amount of data which cannot be precisely analyzed manually. This recalls the need of
approaches and tools for the automatic analysis of acquired data. In this paper we present MIPHAS, a software
system devised to meet this need in a well-defined context: the monitoring of athletes during sport activities.
MIPHAS is a system composed of several components: a smart t-shirt, an electronic component, a web
application, a mobile APP and an advanced decision support system based on machine learning techniques.
This latter is the core component of MIPHAS dedicated to the automatic detection of potential anomalies
during the monitoring of vital parameters.
1 INTRODUCTION
Wearables that are able to monitor health parame-
ters, such as electrocardiogram (ECG), are among the
technologies that are going to change the world we
live in. That was stated by Microsoft co-founder and
billionaire Bill Gates at the 18th edition of the MIT
Technology Review’s annual roundup
1
. This feel-
ing is supported also from the scientific literature that
clearly shows an exponential trend in the number of
publications per year with titles including wearable
electronics (Khan et al., 2019). In the recent years
the research community has devoted a lot of effort
to the field of wearable technologies for the health-
care. Park et al. (2002) presented the “Georgia Tech
Wearable Motherboard (GTWM)”, which provides a
versatile framework for the incorporation of sensing,
monitoring and information processing devices. It in-
1
https://cnb.cx/2XxF9XZ
volves the use of optical fibers and special sensors.
The data bus integrated into the structure transmits
the vital signs information to the monitoring devices
such as an ECG Machine, a temperature recorder, a
voice recorder, etc. Paradiso et al. (2005) designed
WEALTHY, a system where breathing pattern, elec-
trocardiogram, electromyogram, activity pattern or
behavior, temperature can be listed as physiological
variables to be monitored. The system is based on a
wearable interface implemented by integrating fabric
sensors, signal processing techniques and telecommu-
nication systems, on a textile platform. Curone et al.
(2010) devised a prototype system, based on a smart
garment, which enables the detection of health-state
signs of the users (heart rate, breathing rate, body
temperature, blood oxygen saturation, position, ac-
tivity, and posture) and environmental variables (ex-
ternal temperature, presence of toxic gases, and heat
flux passing through the garments),to process data
198
Laudato, G., Rosa, G., Scalabrino, S., Simeone, J., Picariello, F., Tudosa, I., De Vito, L., Boldi, F., Torchitti, P., Ceccarelli, R., Picariello, F., Torricelli, L., Lazich, A. and Oliveto, R.
MIPHAS: Military Performances and Health Analysis System.
DOI: 10.5220/0008989401980207
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 198-207
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

and remotely transmit useful information to the op-
eration manager. Villar et al. (2015) introduced Hex-
oskin
2
, a line of cutting-edge smart clothing that in-
clude body sensors into garments for health monitor-
ing. Hexoskin monitors (i) ECG, and derived fea-
tures such as: Heart Rate Variability (HRV), QRS
events, and Heart Rate Recovery, (ii) Breathing Rate
and Minute Ventilation (L/min), (iii) activity inten-
sity, peak acceleration, steps, cadence, positions and
(iv) sleep activity. Balestrieri et al. (2019) recently
introduced ATTICUS, an Internet of Medical Things
(IoMT) system for implementing personalized health
services through the monitoring of ECG, respiration
rate measurement, galvanic skin response estimation,
skin temperature measurements, and activity classifi-
cation and monitoring. Matias et al. (2018) presents
a bracelet able to perform health abnormalities detec-
tion based on both vital signs, and accelerometer data
collection from the user.
All such systems are designed to work in the
health monitoring scenario, where physicians can re-
motely assist patients. However, monitoring vital
signs would be greatly beneficial also when practicing
sports. Indeed, many health problems can arise when
a person is under specific stressful situations, such as
running. Moreover, personal trainers could use the in-
formation acquired through a continuous monitoring
of vital signs to keep track of the improvements of the
athlete.
In this paper, we introduce MIPHAS (Military
Performances and Health Analysis System), a hard-
ware/software system able to detect and analyze the
vital signs of an individual through the use of wear-
able systems when practicing sports. The novelty of
the MiPHAS system lies in the ability to (i) adapt to
the real conditions of the person, modifying the moni-
toring activity; (ii) analyze the data collected through
the use of automatic learning techniques in order to
suggest anomalous and/or critical situations both in
the vital signs or in the performance of the athlete.
The remainder of the paper is organized as fol-
lows. In Section 2 we provide an overview of
MIPHAS, while in Section 3 we describe in details
the core component of MIPHAS, i.e., the decision
support system. Finally, in Section 4 we conclude the
paper and outline directions for future works.
2 MIPHAS OVERVIEW
The MiPHAS project provides the monitoring of the
electrical activity of the heart, respiratory activity,
2
https://www.hexoskin.com/
temperature and user “dynamics”, aiming at offering
the following services of detection:
• Cardiac Arrhythmia, through an activity analy-
sis of the electrical system of the heart, with par-
ticular focus on bradyrhythmia, tachyarrhythmia
and on Atrial Fibrillation (AF). The focus on these
specific kinds of disease is due to the fact that car-
diovascular diseases are the leading cause of death
in the world, and, in particular, atrial fibrillation
is one of the most frequent types of cardiac ar-
rhythmia (Fuster et al., 2001; Mathew et al., 2009;
Petrutiu et al., 2006).
• Heat Stress and Heat Stroke, through an ac-
curate estimate of body temperature obtained by
a heat map. Exertional Heat Stroke (EHS) – a
medical emergency defined as life-threatening hy-
perthermia with core body temperature ≥ 40.5
◦
C
and Central Nervous System (CNS) dysfunction
(Navarro et al., 2017) – mainly affects individu-
als performing rigorous physical activities, such
as athletes, soldiers, or laborers (Gaudio and Gris-
som, 2016).
• Falls, through the analysis of the user’s posture
and movements.
MIPHAS is a project based on an innovative tech-
nology designed to monitor the vital signs of individ-
uals during training sessions. Indeed, MIPHAS has
been devised for athletes and specialized trainers, as
final users of the system. The objectives of the sys-
tem are therefore based on an individualistic approach
(e.g., personalized training strategies and techniques),
thanks to the continuous and automatic analysis of
the physical conditions of an athlete. The architecture
turns out to be the composition of a multi-component
technology, which includes:
• A Wearable Sensor Part, in the form of a t-shirt
equipped with innovative sensors able to detect
and acquire vital signs;
• A Hardware Component, capable of transmitting
the signals detected by the wearable sensors. This
component is equipped with a smart hardware,
which is also capable of modifying its behavior
according to the needs identified by the software
component;
• A Firmware and Software Platform, able to an-
alyze the vital signs detected in order to repre-
sent the health status of a person, the performance
level and any information deemed useful in order
to offer significant data for monitoring the physi-
cal activity of the individual;
• An Artificial Intelligence (AI) Module, able to an-
alyze the data obtained from continuous moni-
MIPHAS: Military Performances and Health Analysis System
199
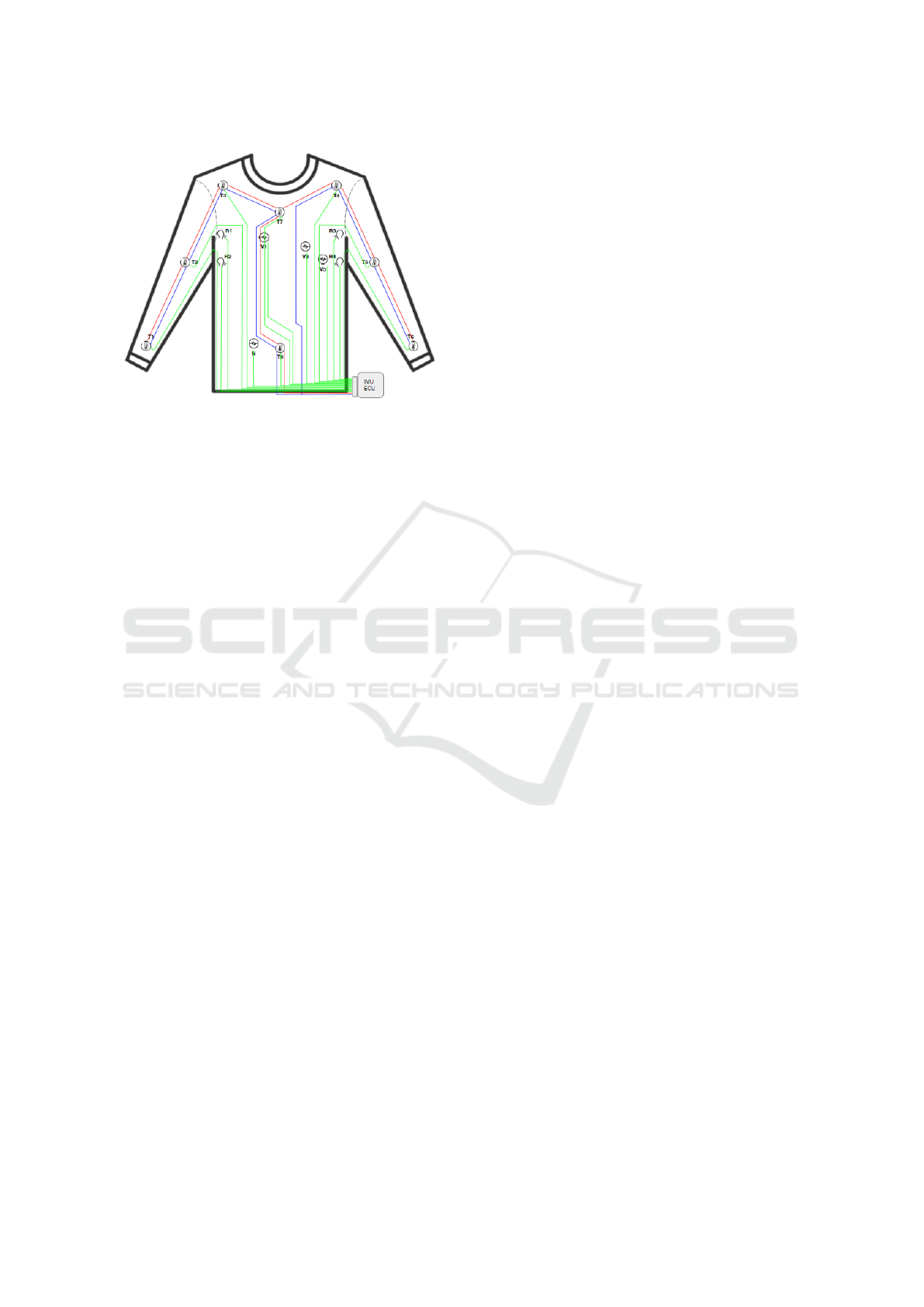
Figure 1: The MIPHAS wearable prototype with the place-
ment of electrodes and sensors to detect vital signs. The
prototype includes eight temperature sensors (from T1 to
T8), four electrodes for the analysis of respiratory activ-
ity (from R1 to R4) and four electrodes for cardiac activity
(from V1 to V5 and N). The IMU/central unit is inside the
ECU (Electronic Control Unit) located at the height of the
belt.
toring and to identify any anomalies, classifying
them according to their criticality level.
An overview on each component of MIPHAS will
be described in the following subsections.
2.1 The Wearable Component
The wearable component in MIPHAS has been built
to acquire (i) real-time three-leads ECG, (ii) thoracic
bio-impedance, for the breath wave measurements,
(iii) eight-points body temperature, and (iv) inertial
data, basically used for activity recognition and fall
detection. Figure 1 shows the preliminary prototype
of the wearable.
The sensors positioning configuration follows
these rules:
• Cardiac Activity: The wearable allows the detec-
tion of the electrical activity of the heart through a
three-lead ECG. The electrodes are arranged ac-
cording to a typical standard Holter configura-
tion (Dower et al., 1988), obtaining a continuous
ECG relative to the precordial leads V1, V3, V5.
The fourth electrode, embedded into the wearable,
represents the neutral (N).
• Temperature Acquisition: To obtain a complete
thermal map of the upper body and maintain the
non-invasive constraint, the MiPHAS system has
8 temperature sensors located in 8 distinct areas
of the upper body, according to the model pro-
posed by Wissler (1964) defined for the simula-
tion of the human thermal system. To guaran-
tee the non-invasive constraint, the MIPHAS sys-
tem acquires the skin temperature of the individ-
ual through sensors integrated in the wearable.
• Respiratory Activity: The MIPHAS system ana-
lyzes the patient’s respiratory activity by measur-
ing thoracic bio-impedance, a technique widely
used for long-term monitoring. In fact, impedance
pneumography (IP) signals can be used to assess
respiratory variables such as volume and respi-
ratory rate (Folke et al., 2003; Houtveen et al.,
2003). Wang et al. (2014) carried out a study com-
paring the accuracy of the IP according to four
different configurations (positioning) of the elec-
trodes. From the comparison of the obtained IP
signals it emerged that the most accurate and sta-
ble configuration appears to be the configuration
shown in Figure 1, since being the electrodes far
from the central area of the chest are less sensitive
to the respiratory movement and are able to guar-
antee a better contact with the leather. Moreover,
such a configuration of the electrodes is also less
sensitive, compared to the others, to the assisted
posture.
• Movement Dynamics: The wearable is equipped
with an Inertial Measurement Unit (IMU), aimed
at detecting user activities and potential falls. The
IMU is positioned close to the waist. Such a
spot is largely considered preferable in applica-
tion of automatic fall detection (Mao et al., 2017;
Ranakoti et al., 2018).
The textile part of the wearable prototype shall
meet key requirements. It has to be: (i) comfort-
able in order to fit prolonged activity intervals with-
out affecting negatively the performances, (ii) stable
when worn in order to favourite the stability of sig-
nals acquisition, (iii) customizable for different sizes
as a common ’fashion’ garment. To met these techni-
cal specifications we decided to adopt linear knitting
techniques with three innovative yarns:
• Bioceramic Elastic Yarn: Used as a base for the
wearable due to its technical characteristics, it is a
decisive element for the perceived comfort of the
garment. This material provides a positive side ef-
fect on peripheral circulation due to FIR (Vatan-
sever and Hamblin, 2012) that is supposed to be
part of the subjectively perceived comfort. Fur-
thermore, the material also provides the structure
on which the sensors are applied and the other
functional yarns incorporated;
• High Grip Silicone Yarn: The highly deformable
wire is used to obtain a ”second skin” effect, nec-
essary to keep the motionless sensors in their po-
sition and to minimize movement artifacts on the
HEALTHINF 2020 - 13th International Conference on Health Informatics
200
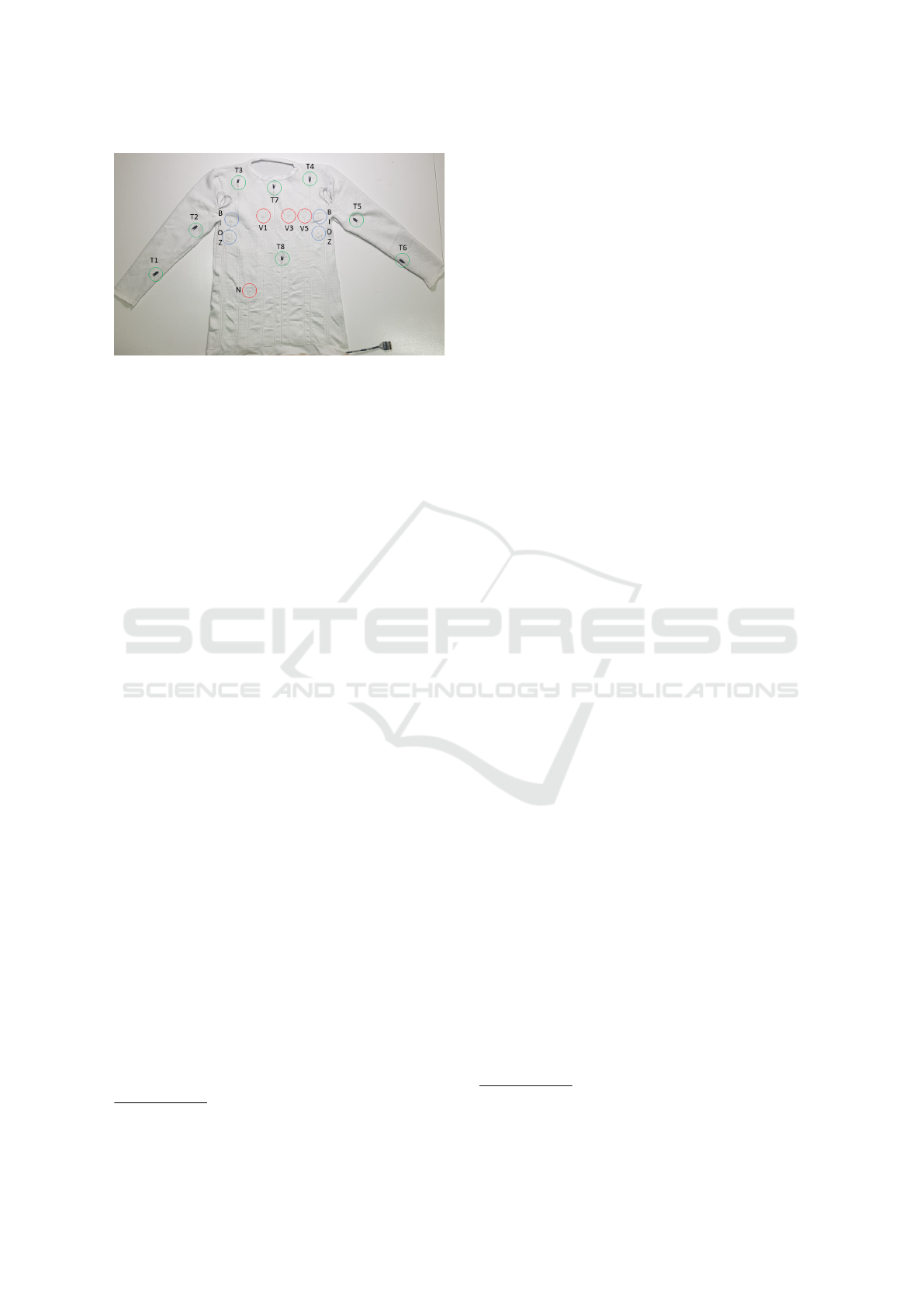
Figure 2: The MIPHAS wearable final prototype.
removal of the biomedical signal. This particular
yarn considerably increases friction without elas-
tic compression (elastic force of the thread itself).
The high friction is due to the intrinsic properties
implemented in the material);
• High Conductivity Shielded Stainless Steel Yarn:
For the creation of the electrical circuit, a high-
performance stainless steel yarn made by capil-
laries coated with an insulated polymeric cover-
ing was adopted. This yarn has a high mechanical
strength, good inertia to oxidizing agents and is
suitable for being integrated into the wearable de-
vice as it maintains a softness that is not perceived
as a foreign body. inside the garment;
• Carbon-black based Electrode: a conductive cloth
that acts as dry electrode. Considering the re-
sults obtained in the literature regarding the use of
dry electrodes in electrocardiographic examina-
tions (Chlaihawi et al., 2018; Guo et al., 2016), the
electrodes must be carbon-based and each elec-
trode must cover a surface of at least 2 cm
2
.
• IC Thermal Sensors: specifically designed ac-
tive sensors for superficial skin temperature esti-
mation.
In Figure 2 is presented the first prototype of
the wearable, built according to the above mentioned
specifications.
2.2 The Hardware Component
This section contains the specifications related to the
BIOX, the data acquisition board used to acquire the
signals coming from the several sensors embedded in
the MIPHAS’s wearable. The board is connected to
the internet via the NB-IoT interface and it can also
connect to a local device through a Bluetooth (Low
Energy) interface. A Generic Attribute Profile Server
(GATT
3
) has been implemented with several services
3
https://bit.ly/2hIE3EB
concerning the following measures: eight tempera-
ture measurements, heart rate, respiratory frequency
and thoracic bio-impedance signal, pitch and roll an-
gles and fall detection, SD memory status and battery
level, data streams related to the ECG channels.
The following are the main types of measurements
provided by the various sensors integrated on the data
acquisition board and the minimum/maximum sam-
pling frequencies that are used for the acquisition of:
• Body Temperature: mapping the body tempera-
ture to eight measurement points. The sampling
frequency is approximately 1 Hz, while the ADC
resolution is 12 bits.
Electrocardiogram: acquisition of ECG signals
from three synchronous channels. The sampling
frequency is 320 Hz and the ADC resolution is
equal to 16 bits;
• Respiratory Wave: thoracic bio-impedance mea-
surement at four terminals. Two currents and two
voltages measured with a sampling frequency of
20 Hz. The ADC resolution is equal to 16 bits;
• Dynamics: (1) orientation measurements, ex-
pressed in terms of pitch and roll angles, acquired
with a frequency of 1 Hz. The ADC resolution
is 12 bits; (2) Fall Detection, the event is gen-
erated asynchronously. The accelerometer has a
dedicated event-detection interrupt (fully config-
urable) which allows the identification of a free-
fall episode.
The general architecture of the MIPHAS elec-
tronic component, with all the devices connected to
the microcontroller and the interfaces that have been
used for the data transport and transmission, is listed
below:
• ADS1294
4
, four-channel ADC with integrated
front-end for the ECG signals conditioning; this
device communicated with the microcontroller
via SPI interface;
• MAX30002
5
, chip for the thoracic bio-impedance
measurement with four terminals, two for current
driving and two for voltage reading; this device
communicates with the microcontroller via SPI
interface;
• Micro SD, which communicates with the micro-
controller via SPI interface;
• Three LEDs, one red, one green and one blue,
which are used to define the battery status. The
LEDs are connected to three digital microcon-
troller output pins;
4
https://bit.ly/33J9sgt
5
https://bit.ly/2nY15hX
MIPHAS: Military Performances and Health Analysis System
201
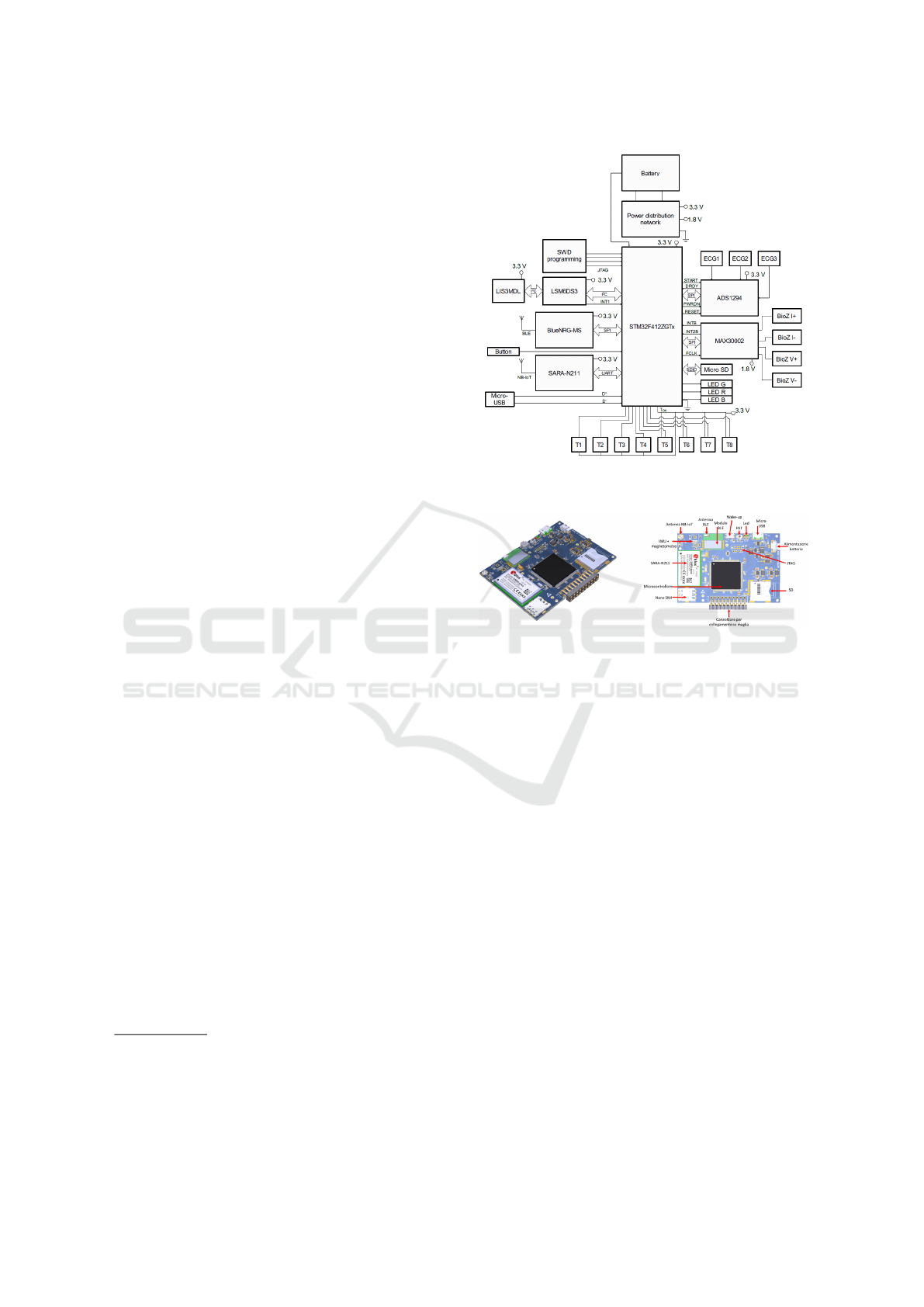
• Eight LMT70
6
temperature sensors, which pro-
vide an output voltage proportional to the mea-
sured temperature. (The signals supplied by these
sensors is acquired using the 12-bit ADC inte-
grated on the microcontroller. Moreover, they are
powered by an output pin of the microcontroller
in order to reduce the energy consumption of the
device);
• Micro-USB, for interfacing the board to a PC via
USB;
• SARA N211
7
, NB-IoT module; this module com-
municates via UART interface with the microcon-
troller;
• BlueNRG-MS
8
, Bluetooth module this module
communicates via SPI with the microcontroller;
• LSM6DS3
9
, sensor containing triaxial accelerom-
eter and gyroscope, which communicates via I2C
with the microcontroller;
• LIS3MDL
10
, triaxial magnetometer, which com-
municates via I2C with the LSM6DS3 module;
• JTAG interface, for microcontroller programming
and firmware debugging;
• The PDN (Power Distribution Network), which
supplies the power to the microcontroller and to
all the devices connected to it, based on the volt-
age supplied by the battery. The voltage supplied
by the battery is measured by the microcontroller
via ADC in order to estimate its state of charge.
The schematic is depicted in Figure 3.
In Figure 4 is depicted the preliminary hardware
prototype of the BIOX board.
The schematic of the BIOX is depicted in Figure 3,
while Figure 4 shows the preliminary hardware pro-
totype. Figure 5 shows the 3D rendering of the case
designed to house the BIOX board. In addition to the
case, it is also shown the design of the sled housing
to anchor the BIOX to the wearable of the MiPHAS
system and to allow a reliable connection of the elec-
trodes and sensors to the electronics.
The MIPHAS firmware implements a GATT pro-
file server Bluetooth Low Energy (BLE) with services
and features according to the working principle de-
picted in Table 1.
We show in Figure 6 the system which integrates
the MIPHAS’s wearable, hardware and firmware.
Moreover, it is shown how, with this configuration, it
6
https://bit.ly/2oSRsl3
7
https://bit.ly/2iBsZsK
8
https://bit.ly/2J1Nspi
9
https://bit.ly/2Mq2Huf
10
https://bit.ly/2J0rcMm
Figure 3: General architecture of the MIPHAS hardware
component.
Figure 4: The preliminary prototype of MIPHAS hardware
component.
is possible to acquire a real-time multi-channel elec-
trocardiogram.
2.3 The Software Component
Figure 7 shows the architecture of the MIPHAS’ sys-
tem. The server is mainly composed by three compo-
nents:
• Application Server: in the the MIPHAS system, it
is the component that provides the infrastructure,
the support and execution functions;
• Decision Support System (DSS): it is the compo-
nent that implements the decision support system
of the MIPHAS system. Based on machine learn-
ing techniques, it has the task of making a first
assessment of the alarms received;
• Alert Manager: it is the component that is in-
volved in the process of notifying the medical spe-
cialists on the alarms received and confirmed by
the DSS. The notification of the alarm is made
only to the sport medical specialists who are in
charge of the athlete for whom an anomalous sit-
uation has been found.
HEALTHINF 2020 - 13th International Conference on Health Informatics
202

Table 1: List of services implemented by the MIPHAS’s firmware.
Feature Transmission Frequency (via BLE) Source
Measurement of body temperature Sent every 1 s Eight points located on the shirt
Measurement of the user’s Heart Rate Sent every 1 s Evaluated on one of the three ECG signals acquired
Electrocardiogram Sent every 31 ms, 10 samples per channel Three ECG channels acquired through the electrodes in V1, V3, V5
Measurement of the user’s Respiratory Rate Sent every 1 s Evaluated on the thoracic bio-impedance signals
Respiratory Wave (thoracic bio-impedance signal) Sent every 500 ms, 10 samples Acquired through the electrodes in R1, R2, R3, R4
Pitch and Roll angles Sent every 1 s Inertial Measurement Unit
Identification of falls Sent in asynchronous mode Inertial Measurement Unit
Estimation of the state of the battery [%] Sent every 1 s BIOX
SD memory occupied in percentage [%] Sent every 1 s BIOX
Figure 5: MIPHAS hardware case 3D Rendering.
Figure 6: The preliminary test of MIPHAS and an example
of the acquired ECG signals.
The users can interact with the system in two dif-
ferent ways:
• Active: Regards the interaction between the
MIPHAS system and the all the actors. Espe-
cially, the “Personal trainer” and the “Manager”
access to a web-based platform while the “Ath-
lete” to a application for mobile devices;
• Passive concerns the interaction between the
MiPHAS system and the “Athlete” during a train-
ing session. These do not have access to any fea-
tures of the MIPHAS system; they only supply
data to the system thanks to the combined use of
the wearable component and the BIOX. The wear-
able deals with the detection of vital signs, while
the BIOX deals with its acquisition and sending,
via Bluetooth Low Energy (BLE) protocol to a
personal gateway. It is then the task of the per-
sonal gateway to send data, via the HTTPS proto-
col, to the MiPHAS server.
The sending of personal gateway data to the
MiPHAS server is done online, i.e., the vital signs
of the individual are streamed every second during a
training session.
Specifically, the structured data, i.e., personal and
clinical data of the athlete are stored in a relational
database. The vital signs automatically monitored, in-
stead, are stored in a document DBMS. The choice
to store this data in a no-SQL database is motivated
by two factors: (i) scalability, because given the large
amount of data to be managed, a document database
offers performances that are certainly superior to a re-
port database as regards information retrieval and (ii)
flexibility, because although the structure of a report
has been defined to send the monitored vital signs, the
latter could be modified, for example by changing the
sampling frequency of a data (e.g., the ECG) or by
adding new sensors to the wearable. In this scenario,
a document database offers greater flexibility than a
relational database.
2.3.1 The Mobile Application
The MIPHAS app is designed for the profile “Ath-
lete”. In the home there are two buttons (Figure 8 A)
that allow, respectively, to start a new training session
and to view the history of the workouts already per-
formed. In case the athlete wishes to perform a new
training session, she has to be submitted to a relax-
ation session, lasting one minute, in order to record
MIPHAS: Military Performances and Health Analysis System
203

Figure 7: The architecture of MIPHAS.
Figure 8: MIPHAS Mobile App: (A) Home section (B) re-
cap of the assigned training session (C) record of the com-
pleted training session.
and store her baseline heart rate and respiratory rate
values. After the minute, the athlete displays a re-
port of her baseline heart rate and respiratory rate val-
ues and the assigned training program (Figure 8 B).
At this point the athlete can start the actual training
session. When completed the training, the system re-
quires the athlete to perform a new relaxation session,
always lasting 1 minute, so as to be able to monitor
the basal heart rate and respiration rate values again.
After the post-workout relaxation time, the app shows
the athlete a screen with the report of the training ses-
sion just ended (Figure 8 C).
2.3.2 The Web Platform
The web platform has been devised for the other two
profiles of the MIPHAS system: (i) the “Gym man-
ager”, responsible for managing personal and clinical
data of athletes, (ii) the “Personal trainer”, who takes
care of the athlete’s training and is interested in mon-
itoring vital signs during a training session in order
to assess how the athlete is responding to the training
protocol.
When accessing the homepage (Figure 9, the sys-
tem shows a mask divided into 3 sections, the first two
sections are displayed both to the “Personal trainer”
and to the “Gym manager”, the third section is shown
Figure 9: The Home section in MIPHAS web platform.
Figure 10: The Heart Rate comparison graph.
only to the “Personal trainer”. In the first section, the
system shows four information boxes containing: (i)
the number of total athletes registered, (ii) the number
of red alarms in the last 30 days, (iii) the number of
yellow alarms in the last 30 days and (iv) the number
of white alarms in the last 30 days. In the second sec-
tion a histogram is shown on the left with the alarms
recorded in the last 30 days and to the right a pie chart
containing the distribution of the alarms in the last 30
days. In the histogram for each day the system reports
3 different colored rectangles: red, yellow and white,
representing respectively the number of red, yellow
and white alarms occurred in the last 30 days.
The third section “Athletes” is visible only to the
personal trainer and shows the list of all the athletes
assigned to the personal trainer. The system gives also
the possibility to view the progress and the details of
the current training session (if any).
A very useful feature is represented by the Com-
pare Workouts section. Here, the personal trainer can
compare the training sessions obtained by an athlete
on different days or compare the sessions carried out
by two different athletes. Through this feature, the
personal trainer can evaluate the progress and results
of the athletes and choose whether to modify certain
training sessions for particular athletes. The compari-
son is based on the data monitored during the train-
ing sessions. The Data Summary section displays
some descriptors of the trainings, such as: (i) the
HEALTHINF 2020 - 13th International Conference on Health Informatics
204

effective duration, in minutes (ii) the average Heart
Rate and Respiratory Rate during the relaxation be-
fore the training (iii) the average Heart Rate and Res-
piratory Rate obtained during relaxation after com-
pleting the training session (iv) the Cardiac, Respi-
ratory and Thermal activity during the entire training
session. Furthermore, in the Details section, the Per-
sonal Trainer has the possibility to check the graphs
with the Heart Rate (an example in Figure 10, Respi-
ratory Rate and Temperature waveforms based on the
data acquired during the training sessions.
3 ARTIFICIAL INTELLIGENCE
IN MIPHAS
The Decision Support System (DSS) is the core soft-
ware for the automatic detection of potential critical
situations. Intelligent decisions are made at different
levels: part of the DSS is embedded in the personal
gateway, while another part is deployed as a stan-
dalone service. The mobile gateway integrates - what
we have defined - a MIPHAS Local DSS (MLDSS),
considering that the data, automatically analyzed by
this component, are related only to one athlete. On the
other hand, we have defined as MIPHAS Global DSS
(MGDSS) the one installed on the server because it is
enriched with the data from all the MIPHAS system
users.
When the electronic component detects an
anomaly, the DSS is warned. Depending on the
source of the warning (e.g. Heart, Respiration, etc.), a
specific component of the - Global or Local - DSS
is triggered. The DSS now can confirm or reject
the warning. In case it is confirmed, an alarm (with
a severity information) is forwarded to the personal
trainer. The personal trainer can analyze in near real-
time the anomaly and decide whether to confirm or re-
ject the anomaly. The decision of the personal trainer
is provided to the DSS that can use the (positive or
negative) feedback to enrich its knowledge base.
3.1 Local Decision Support System
The local DSS has the duty to perform the automatic
analysis of:
• Fall Detection. The process of fall detection in
MIPHAS is managed in such a way that the elec-
tronic component, according to an algorithm in-
ternal to the sensor, detects (optimistically) a free
fall event. Once a potential fall has been identi-
fied, the DSS of MIPHAS system has the task of
rejecting a potential False Positive or confirming
the episode, through a more specific elaboration
than the one implemented by the electronic com-
ponent. Specifically, for an accurate identification
of falls, in MIPHAS it is integrated the method
proposed by Mao et al. (2017). Basically, the au-
thors propose a method based on the evaluation
of a generalized instantaneous Root Mean Square
(RMS) of the triaxial acceleration. To discrim-
inate better a fall event from other rapid move-
ments, in addition to considering the RMS of the
acceleration of the human body, the authors also
analyze the individual posture after the increase
in acceleration. Posture is analyzed through an al-
gorithm that uses the Euler angle, a quantity that
represents the spatial orientation of a body;
• Heat Stress & Heat Stroke. Thanks to a continu-
ous temperature analysis, the DSS needs to iden-
tify a particular situation of heat stress that could
lead to a fatal heat stroke. This is done through
the procedure described by Palma et al. (2017):
an alarm is generated if the patient’s heart rate is
higher than a threshold f (in MIPHAS, the default
is 100 bpm) and there is a change in body tem-
perature at least equal to 0.1° C per minute for a
defined period of time t (in MIPHAS, the default
is 20 minutes).
3.2 Global Decision Support System
We have designed the global DSS in order to perform
these automatic analyses:
• Atrial Fibrillation. When alerted, the MIPHAS
DSS acquires a consistent portion of 3-leads ECG
data. On these signals a well-known QRS detec-
tion method is applied, the Pan-Tompkins algo-
rithm, according to the work of Pan and Tomp-
kins (1985). The outcome of this last step, is used
to trigger the detection algorithm. In MIPHAS,
the algorithm embedded to automatically detect
Atrial Fibrillation is the one proposed by Zhou
et al. (2015). This method is one of the best ap-
proaches in the state of the art, showing highly
precise results in the classification metrics (Sensi-
tivity = 97.37%, Specificity = 98.44%, Accuracy
= 97.89%).
• Respiratory Disorders. When alerted, the
MIPHAS DSS buffers a consistent portion of the
bioimpedance signal. The offset is removed from
the signal, by removing the mean. After this op-
eration, a zero-crossing algorithm has been ap-
plied in order to derive the respiration frequency
from the bioimpedance waveform. Once obtained
a pattern of respiration frequencies, an algorithm
MIPHAS: Military Performances and Health Analysis System
205

Figure 11: The MIPHAS MGDSS modular architecture.
inspects the presence of potential anomalous val-
ues in the pattern;
• Human Activity Recognition (HAR). The HAR
component in MIPHAS is crucial because it al-
lows the system to reject possible False Positive.
If the respiration rate increases, it does not cer-
tainly indicate a respiratory disease if the athlete is
running. Thus, the HAR is an information which
helps the DSS to do a bivariate analysis, before
confirming an anomaly. The algorithm works on
a consistent section of the generalized RMS accel-
eration data: first, the method operates to remove
the DC component from the accelerometer data.
Once deleted, the FFT is computed. The funda-
mental frequency, resulting from FFT, provides
the frequency range where the Human Activity
belongs. At the moment, we have experimented a
3-classes identification (Standing, Walking, Run-
ning) method.
The MGDSS is designed to be reliable, safe and
easily extensible. The MGDSS system defines a se-
ries of detectors, that are, components capable of de-
tecting specific problems based on the measurements
available. MGDSS is structured in different modules
(see Figure 11). Some are basic modules, while others
are plug-ins. There are two basic modules:
• Core Module: contains all the entities of the sys-
tem and defines the abstract class Detector, which
represents a generic pathology detector;
• Main Module: the entry point of MGDSS. It con-
tains all the classes that allow you to manage the
detectors, starts the system and provides services
outside.
The plug-in modules currently defined are the fol-
lowing (see Figure 11): (i) Atrial Fibrillation mod-
ule which contains the detector of atrial fibrillation
and all the classes necessary for the identification of
the pathology, (ii) Breath Problems module as con-
tainer of the detector of respiratory diseases and all
the classes necessary for the identification of such dis-
orders and (iii) Arrhythmia module which contains the
generic cardiac arrhythmia detector and the classes
necessary for the identification of this pathology; (iv)
Activity Recognition module: contains all the classes
that allow to recognize the activity that the athlete is
doing (e.g., running or resting).
When the intervention of MGDSS is requested for
a given athlete, all concrete detectors related to the
warning are instantiated. For example, if the warning
concerns the fall, the heat stroke detector will not be
started in order to optimally allocate the available re-
sources. An instance of a detector refers to a specific
athlete: in other words, if several athletes are mon-
itored simultaneously, it is possible that several in-
stances of the same detectors are running at the same
time. MGDSS periodically checks for new data for
the patient in question and provides this data to all the
detectors installed for it.
The detectors access a patient’s data and, based on
these, they decide if there is any anomaly. If at least
one of the detectors reports an anomaly, it is registered
and sent back to the MiPHAS backend, which, in turn,
alerts the physician. Some of the detectors can be just
a support for other detectors: they are not intended to
report anomalies, but to provide additional informa-
tion to help the other detectors to take a decision. At
the moment, the only support detector implemented is
the Human Activity Recognition (HAR) detector. Pe-
riodically, such a detector is called in order to update
patient activity. Like the other detectors, the HAR de-
tector also has an instance for each patient.
Finally, a Detector Manager (DM) orchestrates all
the detectors. This component provides operations
that allow data to be forwarded to all the detectors
of an athlete and to perform a global detection in a
transparent way (without necessarily know which de-
tectors have been instantiated and in which moment).
4 CONCLUSIONS
In this paper we have presented MIPHAS, a tele-
monitoring system aimed at continuously monitor-
ing athletes during their training sessions and offer-
ing support to the trainers in their decision-making
processes. MIPHAS is basically composed of three
components: a smart t-shirt, an electronic device,
called BIOX, and several software components.
The wearable - made of specific fabrics for the
tele-healthcare applications - embeds several sensors.
The electronic device is the component dedicated to
the data acquisition of vital parameters. This unit is
also in charge of transmitting data in real-time to the
software components. These are mainly composed of
a web application, a mobile app and a DSS.
HEALTHINF 2020 - 13th International Conference on Health Informatics
206

We have an interesting agenda for future works.
First of all, we plan to exhaustively experimenting
MIPHAS. The experimentation will involve profes-
sional athletes. We also plan to enrich the DSS with
more refined algorithms, in order to reach a fully
functioning phase of Continuous Learning. Finally,
we also plan to reduce the invasiveness of the elec-
tronic component by dividing it in distinct physical
modules.
REFERENCES
Balestrieri, E., Boldi, F., Colavita, A. R., De Vito, L.,
Laudato, G., Oliveto, R., Picariello, F., Rivaldi, S.,
Scalabrino, S., Torchitti, P., and Tudosa, I. (2019). The
architecture of an innovative smart t-shirt based on the
internet of medical things paradigm. In Proc. of 2019
IEEE Int. Symp. on Medical Measurements and Appli-
cations.
Chlaihawi, A., Narakathu, B., Emamian, S., Bazuin, B., and
Atashbar, M. (2018). Development of printed and flex-
ible dry ECG electrodes. Sensing and Bio-Sensing
Research, 20, 9–15.
Curone, D., Secco, E. L., Tognetti, A., Loriga, G., Dud-
nik, G., Risatti, M., Whyte, R., Bonfiglio, A., and Ma-
genes, G. (2010). Smart garments for emergency op-
erators: the ProeTEX project. IEEE Transactions on
Information Technology in Biomedicine.
Dower, G., Yakush, A., Nazzal, S., Jutzy, R., and Ruiz, C.
(1988). Deriving the 12-lead electrocardiogram from
four (EASI) electrodes. Journal of Electrocardiology.
Folke, M., Cernerud, L., Ekstrom, M., and Hok, B. (2003).
Critical review of non-invasive respiratory monitoring
in medical care. Medical & Biological Engineering &
Computing, 41(4), 377–383.
Fuster, V., Ryden, L., Asinger, R., Cannom, D., Crijns,
H., and et al., R. F. (2001). ACC/AHA/ESC Guide-
lines for the Management of Patients With Atrial Fib-
rillation: Executive Summary A Report of the Amer-
ican College of Cardiology/American Heart Associa-
tion Task Force on Practice Guidelines and the Eu-
ropean Society of Cardiology Committee for Practice
Guidelines and Policy Conferences (Committee to De-
velop Guidelines for the Management of Patients With
Atrial Fibrillation) Developed in Collaboration With
the North American Society of Pacing and Electro-
physiology. Journal of the American College of Car-
diology, 38(4):1231–1265.
Gaudio, F. and Grissom, C. (2016). Cooling Methods in
Heat Stroke. The Journal of Emergency Medicine,
50(4), 607–616.
Guo, S., Han, L., Liu, H., Si, Q., Kong, D., and Guo, F.
(2016). The future of remote ECG monitoring systems.
Journal of Geriatric Cardiology, 13(6):528-30.
Houtveen, J., Groot, P., and de Geus, E. (2003). Valida-
tion of the thoracic impedance derived respiratory sig-
nalsusing multilevel analysis. International Journal of
Psychophysiology, 59(2):97–106, 2006.
Khan, S., Ali, S., and Bermak, A. (2019). Recent de-
velopments in printing flexible and wearable sens-
ing electronics for healthcare applications. Sensors,
19(5):1230.
Mao, A., Ma, X., He, Y., and Luo, J. (2017). Highly
Portable, Sensor-Based System for Human Fall Moni-
toring. Sensors, 17(9), 2096.
Mathew, S., Patel, J., and Joseph, S. (2009). Atrial fibrilla-
tion: mechanistic insights and treatment options. Eu-
ropean Journal of Internal Medicine, 20(7):672–681.
Matias, I., Pombo, N., and Garcia, N. (2018). Towards a
fully automated bracelet for health emergency solu-
tion. In Proceedings of the 3rd International Con-
ference on Internet of Things, Big Data and Security,
pages 307–314. INSTICC, SciTePress.
Navarro, C., Casa, D., Belval, L., and Nye, N. (2017). Exer-
tional Heat Stroke. Current Sports Medicine Reports,
16(5), 304–305.
Palma, O. A., Ceballos, M., Rocio, R. V., Basto, C., and
Barzallo, B. (2017). Heat stroke detection system
based in iot. In Proc. of 2017 IEEE Second Ecuador
Technical Chapters Meeting.
Pan, J. and Tompkins, W. J. (March 1985). A real-time qrs
detection algorithm. IEEE Transaction on Biomedical
Engineering, bme-32(3).
Paradiso, R., Loriga, G., Taccini, N., Gemignani, A., and
Ghelarducci, B. (2005). Wealthy-a wearable health-
care system: new frontier on e-textile. Journal of
Telecommunications and Information Technology.
Park, S., Mackenzie, K., and Jayaraman, S. (2002). The
wearable motherboard:a framework for personalized
mobile information processing (pmip). In 39th Annual
Design Automation Conference (ACM).
Petrutiu, S., Jason, N., Nijm, G., Al-Angari, H., Swiryn, S.,
and Sahakian, A. (2006). Atrial fibrillation and wave-
form characterization. IEEE Engineering in Medicine
and Biology, 25(6): 24–30.
Ranakoti, S., Arora, S., Chaudhary, S., Beetan, S., Sandhu,
A., Khandnor, P., and Saini, P. (2018). Human Fall
Detection System over IMU Sensors Using Triaxial
Accelerometer. Advances in Intelligent Systems and
Computing, 495–507.
Vatansever, F. and Hamblin, M. R. (2012). Far infrared radi-
ation (fir): its biological effects and medical applica-
tions. Photonics & lasers in medicine, 1(4):255–266.
Villar, R., Beltrame, T., and Hughson, R. L. (2015). Vali-
dation of the hexoskin wearable vest during lying, sit-
ting, standing, and walking activities. Applied Physi-
ology, Nutrition, and Metabolism, 40(10):1019–1024.
Wang, H., Yen, C., Liang, J., Wang, Q., Liu, G., and
Song, R. (2014). A Robust Electrode Configuration
for Bioimpedance Measurement of Respiration. Jour-
nal of Healthcare Engineering, 5(3), 313–328.
Wissler, E. (1964). A mathematical model of the human
thermal system. The Bulletin of Mathematical Bio-
physics, 26(2), 147–166.
Zhou, X., Ding, H., Wu, W., and Zhang, Y. (2015). A real-
time atrial fibrillation detection algorithm based on the
instantaneous state of heart rate. In Plos One Journal.
MIPHAS: Military Performances and Health Analysis System
207
