
Towards an Ambient Support System for Continence Management in
Nursing Homes: An Exploratory Study
Hannelore Strauven
1,2 a
, Ine D’Haeseleer
1 b
, Kristof T’Jonck
3 c
, Hans Hallez
3 d
,
Vero Vanden Abeele
1 e
, Pieter Crombez
4
and Bart Vanrumste
1,2 f
1
e-Media Research Lab, KU Leuven, Andreas Vesaliusstreet 13, Leuven, Belgium
2
imec-Stadius, KU Leuven, Leuven, Belgium
3
imec-DistriNet, KU Leuven, Bruge, Belgium
4
Televic Healthcare NV, Izegem, Belgium
Keywords:
Incontinence, Nursing Home, Ambient Monitoring, Exploratory Study.
Abstract:
Time consuming and costly, continence care management has become one of the main care demands in nurs-
ing homes with potential inadequacy negatively impacting residents’ quality of life. While engineering efforts
in this area are increasing, these mainly focus on wearable innovations. To support continence care in nursing
homes in an unobtrusive manner, we developed an ambient sensor system to continuously monitor inconti-
nence events, e.g., saturated incontinence materials or leakages. In an exploratory study in two nursing homes,
we evaluated an early prototype of the sensor system and built annotated data sets. Implemented annotation
devices included a smart sensor mat, a toilet timing predicting device, and manual data entry of continence
care by care personnel. From our analysis of the preliminary study results based on the first two residents, we
learned how challenging the ambient monitoring and annotation of incontinence events is. On the basis of the
outcomes, we provide suggestions for further research of ambient sensor systems supporting continence care.
1 INTRODUCTION
In long-term care settings, such as nursing homes,
over 50% of the older adults experience incontinence,
i.e., the involuntary leakage of urine or stool (Offer-
mans et al., 2009). Consequently, continence care
has become one of the main care demands (Wagg
et al., 2017). Over 20% of care time is spent on di-
rect continence care management, e.g., toileting as-
sistance, and changing incontinence materials (Ous-
lander and Kane, 1984). In addition, the average cost
for management is about US$15 per day per resi-
dent (Hu et al., 2003). Continence care is thus time
consuming and costly for nursing homes, moreover,
it also negatively impacts the residents’ quality of
life, e.g., by disturbing their sleep (Ouslander et al.,
a
https://orcid.org/0000-0002-7233-8137
b
https://orcid.org/0000-0001-5455-3581
c
https://orcid.org/0000-0003-4150-4144
d
https://orcid.org/0000-0003-2623-9055
e
https://orcid.org/0000-0002-3031-9579
f
https://orcid.org/0000-0002-9409-935X
1998). In a generally ageing society, the prevalence
of incontinence will only increase, resulting in addi-
tional pressure on the already overburdened staff and
institutional costs (Wilson et al., 2001; Mather and
Bakas, 2002). Previous engineering research focused
on wearables, such as the development of smart in-
continence wear (Fish and Traynor, 2013; Lin et al.,
2017). To the best of our knowledge, no studies in-
volve unobtrusive, ambient sensor technology to sup-
port continence care in nursing homes.
We are interested in the potential of an ambient
sensor system to support continence care in nursing
homes. To evaluate the system, this paper describes
an exploratory field study with an early prototype de-
ployed in two nursing homes.
We first elaborate on continence care practices,
and how technology approaches can support them.
We then proceed with the implementation of the pro-
totype, together with the applications and devices for
annotation. Following implementation, a first evalu-
ation of the system is presented through preliminary
results and user feedback. We close by putting for-
ward considerations for further system development
438
Strauven, H., D’Haeseleer, I., T’Jonck, K., Hallez, H., Abeele, V., Crombez, P. and Vanrumste, B.
Towards an Ambient Support System for Continence Management in Nursing Homes: An Exploratory Study.
DOI: 10.5220/0008963404380446
In Proceedings of the 13th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2020) - Volume 5: HEALTHINF, pages 438-446
ISBN: 978-989-758-398-8; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All r ights reserved

Table 1: Overview of Ambient Intelligence (AmI) technologies evaluated in nursing homes to support care management.
Authors Care domain Technology Device
Huion et al. Continence Wearable Smart diaper (WetSens)
Traynor et al. Continence Wearable Smart diaper (SIM)
Wai et al. Continence Wearable Smart diaper (iCMS)
Aloulou et al. Activities of daily living Ambient assistive living Unobtrusive sensors & devices
Hori & Nishida Activities of daily living Ambient assistive living Ultrasonic sensors
Rantz et al. Activities of daily living Ambient assistive livings Unobtrusive sensors & devices
Suzuki et al. Activities of daily living Ambient assistive living Infrared sensors
and associated research studies in nursing homes.
1.1 Background
During the day, over 20% of care tasks are directly re-
lated to continence care, increasing to 70% during the
night. For more interdependent older adults, the esti-
mated time reaches nearly one hour per nursing home
resident per day (Ouslander and Kane, 1984; Borrie
and Davidson, 1992). Continence care practices in-
volve periodic manual check-ups of incontinence ma-
terial, toilet visits and continence assessments. Cur-
rent practices lead to unnecessary controls or delayed
interventions, triggering undesired instances such as
disturbed sleep (O’Dell et al., 2008). These are un-
comfortable situations for care personnel and resi-
dents alike.
Efforts have been made to support continence care
management through Ambient Intelligence (AmI)
systems. AmI brings intelligence to physical envi-
ronments and measures them through sensors (Cook
et al., 2009). It has the potential to improve the health-
care domain and mainly consists of two types of tech-
nology (Acampora et al., 2013):
• Body Area Network (BAN): body sensors are at-
tached on clothing or on the body, commonly
known as wearables, or even implanted under the
skin, e.g., to measure body temperature, blood
pressure, or cardiac activity;
• Wireless Mesh Sensor Networks (WMSN): am-
bient sensors are embedded into the environment,
e.g., to measure room temperature, opening doors,
or movement.
Research can be found on the development of smart
incontinence wear, i.e., a BAN with a wearable de-
tecting the saturation level of material via an inte-
grated humidity sensor and alerting care personnel
for required check-ups. Exploratory studies in nurs-
ing home settings evaluated several smart diaper pro-
totypes, identifying and testing technical specifica-
tions (Table 1) (Huion et al., 2019; Traynor et al.,
2014; Wai et al., 2010b). Conducted research to de-
velop an intelligent Continence Management System
(iCMS) for nursing homes via smart incontinence ma-
terials and wetness alert notifications on a smartphone
for care personnel, faced several technical challenges
(Wai et al., 2008; Wai et al., 2010a; Wai et al., 2010b;
Wai et al., 2011). The researchers concluded that de-
sirable features of an intelligent continence care man-
agement system could range from unobtrusive contin-
uous monitoring to odour-based detection, pointing
towards a recommendation to shift continence care
technology from BANs to WMSNs.
In contrast to the technological solutions to sup-
port continence care, WMSN is already thoroughly
researched and evaluated in the care domain of ac-
tivities of daily living (ADLs) by the name of Ambi-
ent Assistive Living (AAL) (Table 1) (Aloulou et al.,
2013; Hori and Nishida, 2005; Rantz et al., 2010a;
Suzuki et al., 2006). To monitor ADLs, research
utilised ambient sensors and devices, ranging from
low cost sensors (e.g., pressure sensors, motion sen-
sors, bed sensors, and vibration sensors) and devices
of interaction (e.g., camera, speakers, and tablets)
(Aloulou et al., 2013; Rantz et al., 2010a) to ultra-
sonic sensors (Hori and Nishida, 2005) or infrared
sensors (Suzuki et al., 2006).
Monitoring via ambient sensors presents an op-
portunity to develop unobtrusive technology for user
groups like nursing home residents. Although, plenty
of AAL research is conducted in nursing home set-
tings, to date and to the best of our knowledge, no
literature can be found in this area on ambient conti-
nence care monitoring.
1.2 Scope of this Work
This paper focuses on the implementation and evalu-
ation of the prototype of an ambient sensor system to
unmask incontinence events through an exploratory
study. Present nursing home technology and techni-
cally validated devices were used to annotate conti-
nence care events and, afterwards, label them. Our
aim is then to avoid these unpleasant incontinence
events in the future. The first results of this study
will enrich further development of the ambient sup-
port system and provide suggestions for future re-
Towards an Ambient Support System for Continence Management in Nursing Homes: An Exploratory Study
439

search studies in nursing home settings.
2 IMPLEMENTATION
The explorative field study was carried out in two
nursing homes to build annotated data sets, necessary
for system evaluation and further technical develop-
ment. Data was acquired via four different sources
(Figure 1):
• The sensor system prototype (blue): a developed
non-obtrusive sensor system that was evaluated;
• Manual data entry by care personnel (red): nurse
calls via the nurse call system (green) and conti-
nence care (Report Inco) via the resident care file
(cyan);
• The Toilet Timing Predicting Device DFree
1
(pur-
ple): validated non-invasive ultrasound technol-
ogy;
• The smart sensor mat Texible Wisbi
2
(brown):
validated wet sheet technology.
Figure 1: Implementation overview of the sensor system
prototype, the manual data entry, and technically validated
devices.
2.1 Sensor System Prototype
The aim was to develop a sensor system to identify in-
continence events. To preserve residents’ comfort, we
wanted the system to be unobtrusive and, therefore, to
include ambient sensors.
We developed a sensor system prototype to be at-
tached to a care bed, monitoring and detecting incon-
tinence events (T’Jonck et al., 2019). The prototype
was designed with commercial off-the-shelf compo-
nents. The chosen sensors were breakout boards, i.e.,
1
dfree.biz/en/
2
www.texible.at/
click boards, from MikroE
3
that use the mikroBUS
TM
specification: Weather click, Temp&Hum 2 click, Ac-
cel 5 click, and Air quality 5 click. The decision
to integrate the Air quality 5 click sensor was based
on research concluding that this sensor is able to de-
tect concentrations of ammonia (NH3) in the range
of concentrations that are present in urine (Strauven
et al., 2019).
A Raspberry Pi
4
was used as room gateway
to send sensor data via an Long Term Evolution
(LTE) network to a secure InfluxDB
5
database. Data
was stored in real-time and could be exported from
Grafana
6
, an open source visualisation application
that supports the direct integration of the InfluxDB
database. The Grafana dashboard monitored the sen-
sor modules remotely and in real-time.
The sensor system prototype recorded sensor data
every second. The temperature, humidity and ammo-
nia sensors were fixated in the middle of the bed bar,
located on the side of the care bed (Figure 2). The ac-
celerometer was positioned between the bottom of the
care bed and the mattress. Sensor data was collected
during the entire study.
Figure 2: Picture of the sensor module at the care bed, in-
cluding the Accel 5 click (left), the Weather click and Air
quality click (middle) and Temp&Hum 2 click (right).
2.2 Manual Data Entry
The manual data entry of the care personnel provided
additional insights in the care needs of participants
and was entered through two nursing home technolo-
gies, the nurse call system (NCS) and the resident care
file (RCF). Care personnel was requested to provide
this data during the entire study. Each annotation was
3
www.mikroe.com/
4
www.raspberrypi.org/
5
www.influxdata.com/
6
grafana.com/
HEALTHINF 2020 - 13th International Conference on Health Informatics
440

Table 2: Timeline of the exploratory field study in the first nursing home for two residents.
Timeline Action
19/07/19 Installation sensor module, NCS application, RCF incontinence report
21/07/19 Start measurement for three weeks with resident 1
29/07/19 Start DFree & Wisbi
12/08/19 End sensor measurement resident 1
14/08/19 Start measurement for three weeks with resident 2
21/08/19 Start DFree & Wisbi
04/09/19 End measurement resident 2
timestamped to link the entry to the sensor data after-
wards.
Residents can call for assistance via the NCS, a com-
munication and management application. If residents
need assistance, they call by pushing an alarm button,
that generates a call at the care personnel’s phone.
For this study, care personnel received smartphones
with the application ‘Call Manager’
7
, designed for
this purpose, and running on the Televic NCS (Figure
1). When a nurse call was triggered, care personnel
could, via the application, first select the reason of the
call from a list and then an appropriate action to assist
the resident from a contextual list.
The RCF is a software application that stores in-
formation about the health and care plan of residents.
Care personnel can obtain all necessary information
about the residents they care for via the RCF. For this
study, additional continence care content was added
to Corilus’ RCF application, ‘Geracc’
8
, to let care
personnel report more extensively about conducted
continence care tasks (Figure 1). The additional tasks
ranged from the check up of incontinence material to
toilet visits. To facilitate the extra input, a Microsoft
(MS) Surface was installed in participants’ room, al-
lowing care personnel to enter the information right
after taking care.
2.3 Validated Technology
The TripleW Toilet Timing Predicting Device DFree
detects bladder size by using harmless, non-invasive
ultrasound technology. The sensor is placed at the ab-
domen in the area of the pubic bone. The main unit,
i.e., another part of the device connected to the sen-
sor, sends data wirelessly to a secured web portal of
TripleW. Participants were asked to wear DFree for
three to four days.
The smart sensor mat Texible Wisbi is a portable
application and consists of an intelligent mattress pad
that detects the humidity level of the fabric. In ad-
7
www.televic-healthcare.com/en/solutions/mobile-
alarming
8
www.corilus.be/en/elderly/careconnect-elderly
dition, Wisbi consists of an occupation detector to
detect presence on the sensor mat. The sensor mat
is attached to an external transmitter that sends the
data through a WLAN network to an application on
a smartphone. The smart sensor mat was placed be-
tween the mattress and sheet of a participant’s care
bed so they lied on the fabric when lying in bed. The
smart sensor mat was used by participants during the
same period as DFree.
2.4 Participants
We recruited ten residents across two Belgian nursing
homes, Sint-Bernardus in Bertem and Biezenheem
in Kortrijk, in collaboration with the nursing home’s
care personnel. Participants’ rooms were provided
with the sensor system prototype for three weeks.
Ethical approval to conduct the research was obtained
from the Social and Societal Ethics Committee of KU
Leuven with protocol number G- 2019 01 1510.
Inclusion criteria for participants were: 65 years
or older, living in one of the two participating nurs-
ing homes, having continence care needs (Katz score
above 1 for Continence (Katz et al., 1963)), and
being able to participate independently, understand-
ing the purpose and involvement and providing con-
sent (Mini-Mental State Examination (MMSE) score
above 18 (Folstein et al., 1975)). An exclusion cri-
terion was when the resident had a separate medical
condition that influences continence.
3 EVALUATION
Measurements were completed in the first nursing
home as the exploratory study was ongoing in the sec-
ond nursing home. Three out of five selected partici-
pants from the first nursing home were excluded: one
removed themselves before the start, one decided to
discontinue during the study, and one was transferred
to another ward. Therefore, this section discusses the
preliminary results from two residents, measured over
a period of three weeks from July to September 2019.
Towards an Ambient Support System for Continence Management in Nursing Homes: An Exploratory Study
441
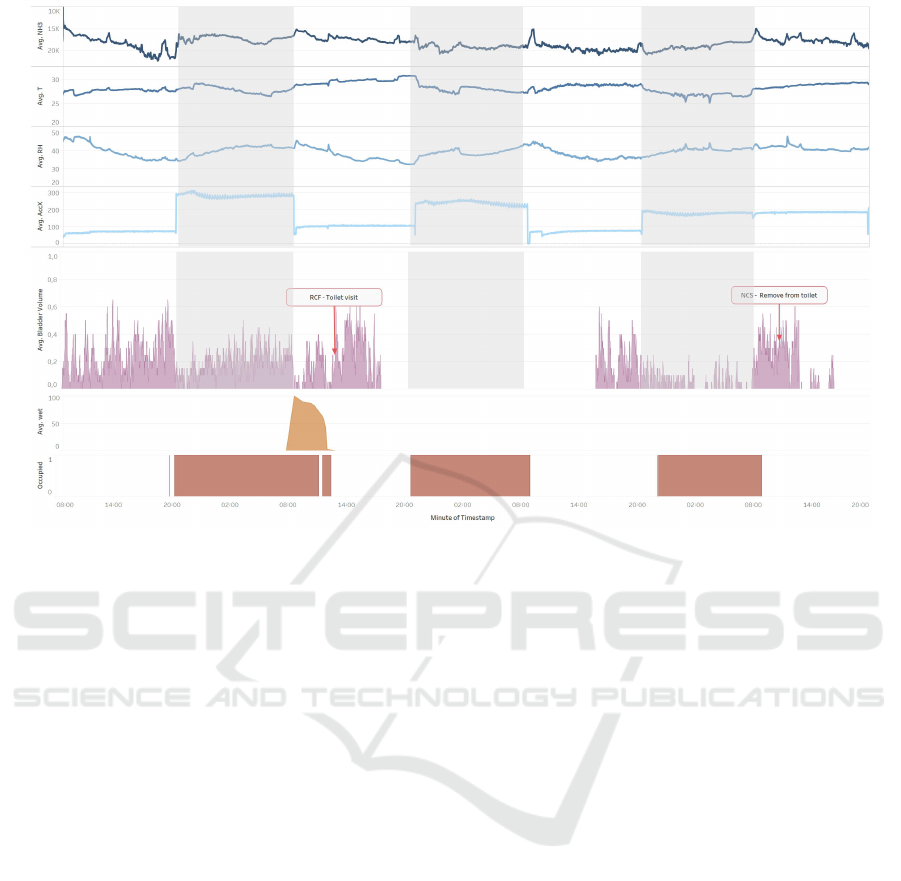
Figure 3: Time series plots of data from Resident 1: the sensor system prototype with the ammonia (NH3), temperature (T)
and humidity (RH) sensor, and the x-axis of the accelerometer (AccX) (top), the DFree (middle), and the Wisbi wetness and
occupation detector (bottom) over a period of 3.5 days.
Table 2 presents a timeline of all systems and appli-
cations used during the study.
3.1 Data Exploration
Data is explored for resident 1 (Figure 3) and resi-
dent 2 (Figure 4) individually by time series plots over
a period of 3.5 days. Resident 1 was a 92-year-old
woman, used a wheelchair due to a physical disability,
and highly dependent on carers. She was also func-
tionally incontinent (i.e., unable to get to a bathroom
for one or more physical or mental reasons). Resident
2 was 88-year-old woman and an active resident who
independently took care of herself. She experienced
urge incontinence (i.e., unable to postpone the desire
to void).
The results of the sensor system prototype are dis-
played at the top of the figures, for the ammonia
(NH3), temperature (T) and humidity (RH) sensor,
and the x-axis of the accelerometer (AccX). For res-
ident 2, the accelerometer lost connection during the
study and is not included in the plot. The y-axis of the
NH3 signal is reversed for better understanding, as the
sensor’s response is inversely proportional to the NH3
concentration. As the sensor module was installed at
the care bed, only periods when a resident was in bed
are relevant for data analysis. To illustrate this time
range, the nights are marked grey. Resident 1 went to
bed around 20:00 and woke up around 08:00. Resi-
dent 2 had a different circadian rhythm and went to
bed around 23:00 and woke up around 09:00.
The NH3 signal varied less in time during the
night, compared to the day. This can be explained
by the difference in motion. During the day, residents
were moving around, opening/closing doors and win-
dows, received care, or had visitors. During the night,
the room was quiet, providing less motion and, there-
fore, a more stable signal. For resident 1, we would
expect an increase of the NH3 signal at night when
she was in bed, wearing incontinence material, and a
decrease in the morning when she was lifted out of
bed. For multiple nights, we could identify a gentle
increase of the NH3 signal over time. After the night,
an elevation was observed which might relate to the
change of the night incontinence material in the morn-
ing. For resident 2, we did not expect the same varia-
tion as she went to the toilet at night as well. Hence,
the NH3 signal remained more stable at night.
We noticed that the temperature raised during the
day and lowered during the night, and how the humid-
ity values related inversely to temperature measures.
Both levels and variances were in accordance with our
expectations for the season and environment.
The AccX signal was low during the day and
HEALTHINF 2020 - 13th International Conference on Health Informatics
442
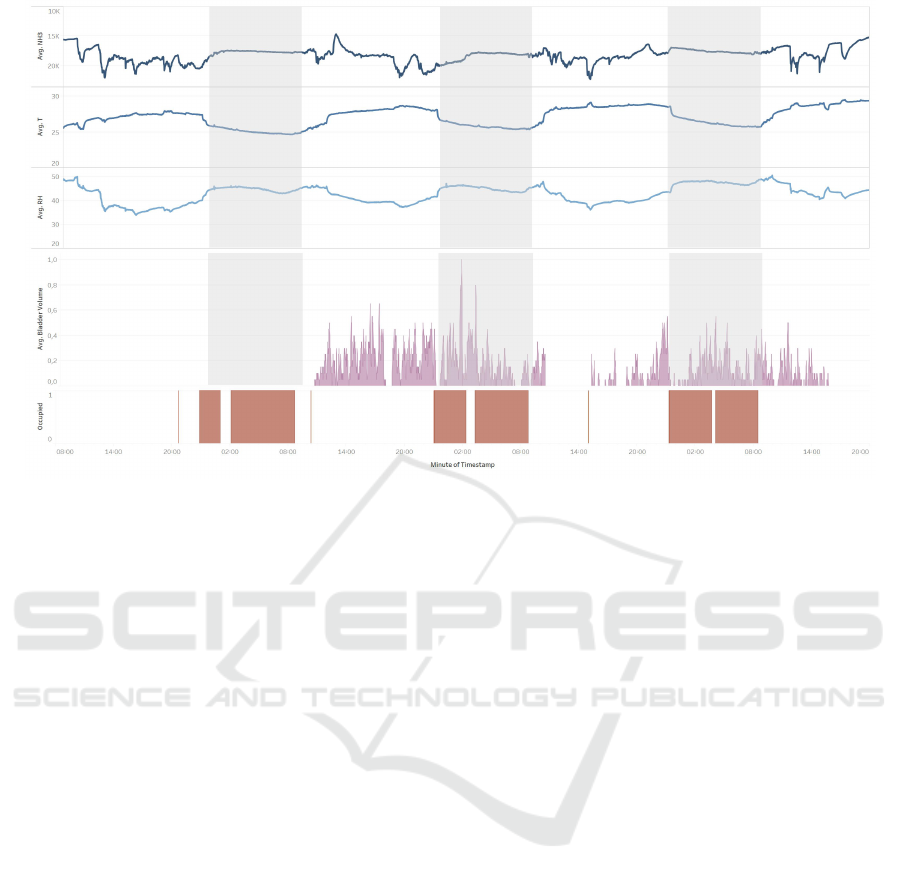
Figure 4: Time series plots of data from Resident 2: the sensor system prototype with the ammonia (NH3), temperature (T)
and humidity (RH) sensor (top), the DFree (middle), and the Wisbi occupation detector (bottom) over a period of 3.5 days.
high during the night, following resident 1’s day/night
regime. Therefore, the accelerometer can be consid-
ered an out-of-bed detector.
The AccX signal remained high after the third night,
when we would expect it to turn low. The reason for
this alteration was uncertain as, for example, it was
possible resident 1 stayed in bed that day, or care per-
sonnel made up the bed and changed the position of
the sensor.
The figures’ middle sections display the output of
TripleW DFree by the average bladder volume per
minute. The signal was continuously spiking, and
harder to be examined visually in time than foreseen.
In addition, DFree had a short battery lifetime of ca.
24 hours so the device had to be charged periodically,
which explains the gaps in the plots.
The output of Texible Wisbi is visualised at the fig-
ures’ bottom. For resident 2, Wisbi did not detect any
wetness; subsequently only the occupation plot is in-
cluded. When the occupation signal was high, this
largely corresponded with the marked night times, ex-
cept for some disparities. For resident 2, we observed
low occupation periods during the night. The resident
mentioned she went to the toilet at night, so we could
assume these low signal periods coincide with these
instances. To define the resting night times, the Wisbi
was more accurate as the predefined ranges based on
the habitual times. We could see one wetness peak
for resident 1 at the second morning. The DFree plot
showed a low bladder volume at the same time and
the NH3 signal increased. This means it was possible
that the incontinence material became oversaturated
or leaked. On the other hand, the AccX signal was
low, and in contrast, the occupation detector of Wisbi
high. Since the accelerometer was located behind the
upper part of the care bed and the sensor mat under
the bottom, it was possible the resident was sitting on
the bed. For resident 1, the same unexpected high sig-
nal for the occupation detector was not noticed as for
AccX after the third night. Therefore, it was more
likely that the position of the accelerometer changed,
for example, after making up the bed.
In the window of 3.5 days, one annotation was
made via Geracc, where care personnel assisted resi-
dent 1 at the toilet, and one via Call Manager, where
resident 1 called to be taken off the toilet. We would
expect the bladder volume to decrease before these
annotations, which was observed for the first annota-
tion but not visible for the second.
During the measurement period of three weeks,
18 nurse calls were recorded via Call Manager: 16
for resident 1 and two for resident 2. The number
of entries seemed low as resident 1 needed assistance
for each toilet visit and used the NCS to alert care
personnel when ready. For this reason, we would ex-
pect at least two calls per day (i.e., 42 calls for three
weeks). Although the total number of entries was
rather low, Figure 5 gives some insight in the type
of nurse calls. It appeared that resident 1 called more
than resident 2, and mostly for toilet assistance and
Towards an Ambient Support System for Continence Management in Nursing Homes: An Exploratory Study
443

Figure 5: Result of manual data entry by care personnel via
Call Manager for resident 1 and resident 2.
movement. This can be associated with her physi-
cal impairments, whereby she needed more assistance
with ADLs compared to resident 2.
Via Geracc, three continence care records were gener-
ated for resident 1 and none for resident 2. In relation
to the nurse call records, the number of annotations in
Geracc was remarkably low, as there should be at least
a continence care record for each toilet assistance. On
the basis of the three records, we could only identify
that all records entered were toilet visits and that in-
continence material was changed during each toilet
visit, even if the material was not yet saturated.
3.2 User feedback
When we finished the study in the first nursing home,
we obtained user feedback. Residents who partici-
pated were asked how they experienced their partici-
pation in a one on one conversation with a researcher.
Care personnel of the ward was asked for their feed-
back in group by two researchers during their daily
ward meeting.
Both residents were unfamiliar with the devices
and applications installed in their room for this study.
It was an adjustment of their environment which felt
uncomfortable. However, after a few days, they
adapted to the changes. One resident enjoyed to be
involved and notified care personnel when a device
was not working properly (i.e., when the lights were
not blinking). Wearing the sensor of DFree was per-
ceived tolerable, at least for a few (ca. four) days. The
level of tolerance depended mostly on the mobility of
the resident. For example, resident 2 walked around
during the day and had to think about the clothes she
could wear when wearing DFree, so others would not
see the device. The use of Wisbi went largely unno-
ticed by the residents.
Care personnel found it difficult to recommend
residents as suitable participants. In a nursing home,
only a limited number of residents have a MMSE
score above 18 and are able to understand the purpose
of and involvement in a research study.
The sensor system attached to the care bed might be
designed more robust or cased for care personnel to
ease making the bed or cleaning underneath. Largely,
care personnel had little experience with smart elec-
tronic devices, e.g., smartphones. This made anno-
tating challenging for them as they were learning to
operate a new device as well as a new application.
DFree was perceived as easy to use, once they found
the proper sensor location on the abdomen of the res-
ident. They preferred a longer battery lifetime as they
had to remove and reload the device daily. At last,
they experienced Wisbi as straightforward to use.
4 DISCUSSION AND
CONCLUSION
As mentioned before (see Table 1), technical inno-
vations to support continence care in nursing homes
are predominantly wearable systems. After conduct-
ing several trials, including exploratory studies, re-
searchers (Wai et al., 2010b) stressed the importance
of an unobtrusive system and odour-based detection.
When looking at other care domains, e.g., ADLs, us-
ing AmI to design unobtrusive technology is already
further explored. On the basis of the need to support
continence care by ambient monitoring, a first proto-
type was developed.
Through the implementation and evaluation of the
prototype via an exploratory study, we evaluated the
preliminary results from two participants of the first
nursing home. They provided us with sensor data
from the prototype, together with data from devices
for annotation purpose to obtain a reliable ground
truth. In this paper, we analysed and compared data
from all devices in a window of 3.5 days. Patterns
were found that illustrated the alteration of the en-
vironment among day and night, and indicated that
the accelerometer can be used for out-of-bed (or oc-
cupation) detection. The NH3 signal was highly in-
fluenced by an environment in motion. During the
night, the signal was smoother as the environment was
more steady. The visual identification of incontinence
events appears to be challenging. To lower the influ-
ence of motion, we suggest to locate the NH3 sensor
at a position on the care bed where less motion oc-
curs, e.g., under the sheets, and to integrate the sensor
system in a robust case.
Finding and providing an appropriate annotation
method in exploratory studies to label ground truth
is known to be challenging, but also incredibly valu-
able for further qualitative, in-depth data analysis (Al-
HEALTHINF 2020 - 13th International Conference on Health Informatics
444

shammari et al., 2017).
Once initiated, a trial could not be repeated, as
nursing home residents are frail elderly and would not
have the resilience for a second try. Every day with-
out annotation can be seen as an expensive loss (Hein
et al., 2017). Common practice for annotating AmI
studies is to videotape the recording session and to
label the data based on the video footage afterwards
(Plotz et al., 2012). Although this technique provides
an accurate labelling, it is ethically inappropriate to
videotape in real-life situations due to privacy reasons
(Aicha et al., 2017). Our sensor setup was in nursing
home residents’ rooms for three weeks and would in-
terfere with the privacy of the residents as well as their
relatives and nursing home staff, who all enter the
room during the study. In addition, it is uncertain that
incontinence events occurring under a sheet, would be
noticed on video footage. For this reason, we opted
for a combination of manual data entry and techni-
cally validated devices (DFree and Wisbi) to enable
ground truth labelling. The obtained data of Wisbi
was straightforward, however, the data from DFree
turned out to be harder to interpret than expected.
Manual data entry by care personnel, e.g., via log
sheets or questionnaires, was similarly part of our pro-
tocol as previously mentioned by AmI research (Table
1) (Aloulou et al., 2013; Rantz et al., 2010b; Suzuki
et al., 2006). However, in our study, we encoun-
tered multiple difficulties to let care personnel anno-
tate. Care personnel was inexperienced with the use
of smartphones, which caused insecurity in using the
device and generated issues directly related with the
smartphone, instead of the application use. These is-
sues eventually resulted in frustrations and a reduced
usage of the devices. As a result, the number of an-
notations were limited. To obtain an enriched set of
manual data entries for exploratory studies in real-life
settings, such as nursing homes, we suggest to extend
the information about the use of the annotation appli-
cations with an explanation of the used device or en-
abling annotation through devices that have already
been used by the annotators prior to the study.
We will continue our research with an in-depth
analysis of all acquired data and ground truth la-
belling to deconstruct this complex data and identify
incontinence events, e.g., the saturation level of the
incontinence material or leakages. Further research
of an ambient monitoring system supporting conti-
nence care should consider the altering environment
and monitor at places with the lowest impact. In ad-
dition, care personnel should be assisted more thor-
oughly and consistently in the annotation process.
ACKNOWLEDGEMENTS
The imec.icon project DISCRETE runs from Octo-
ber 1, 2018 to September 30, 2020 and joins forces
of commercial partners Televic Healthcare, Corilus,
Distrac Group and the knowhow of Zorg Kortrijk and
WZC Sint-Bernardus, with the scientific expertise of
researchers from van imec-KU Leuven-DISTRINET,
imec-KU Leuven-STADIUS and KU Leuven-HCI.
The project is funded by Flanders Innovation & En-
trepreneurship. We would like to thank the nursing
homes’ care personnel and residents for their partici-
pation during the exploratory field study, and our col-
league, Katta Spiel, for their feedback that greatly im-
proved the paper.
REFERENCES
Acampora, G., Cook, D. J., Rashidi, P., and Vasilakos, A. V.
(2013). A survey on ambient intelligence in health-
care. Proceedings of the IEEE, 101(12):2470–2494.
Aicha, A. N., Englebienne, G., and Kr
¨
ose, B. (2017). Un-
supervised visit detection in smart homes. Pervasive
and Mobile Computing, 34:157–167.
Aloulou, H., Mokhtari, M., Tiberghien, T., Biswas, J., Phua,
C., Kenneth Lin, J. H., and Yap, P. (2013). Deploy-
ment of assistive living technology in a nursing home
environment: methods and lessons learned. BMC
Medical Informatics and Decision Making, 13(1):42.
Alshammari, N., Alshammari, T., Sedky, M., Champion, J.,
and Bauer, C. (2017). Openshs: Open smart home
simulator. Sensors, 17(5):1003.
Borrie, M. J. and Davidson, H. A. (1992). Incontinence
in institutions: costs and contributing factors. CMAJ:
Canadian Medical Association Journal, 147(3):322–
328.
Cook, D. J., Augusto, J. C., and Jakkula, V. R. (2009).
Ambient intelligence: Technologies, applications, and
opportunities. Pervasive and Mobile Computing,
5(4):277–298.
Fish, P. and Traynor, V. (2013). Sensor technology: a smart
way to manage continence.
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975).
“Mini-mental state”: A practical method for grading
the cognitive state of patients for the clinician. Journal
of Psychiatric Research, 12(3):189–198.
Hein, A., Kr
¨
uger, F., Bader, S., Eschholz, P., and Kirste,
T. (2017). Challenges of Collecting Empirical Sensor
Data from People with Dementia in a Field Study.
Hori, T. and Nishida, Y. (2005). Ultrasonic Sensors for
the Elderly and Caregivers in a Nursing Home. pages
110–115.
Hu, T.-W., Wagner, T. H., Bentkover, J. D., LeBlanc, K.,
Piancentini, A., Stewart, W. F., Corey, R., Zhou, S. Z.,
and Hunt, T. L. (2003). Estimated economic costs
of overactive bladder in the United States. Urology,
61(6):1123–1128.
Towards an Ambient Support System for Continence Management in Nursing Homes: An Exploratory Study
445

Huion, A., Decalf, V., Kumps, C., Witte, N. D., and Ev-
eraert, K. (2019). Smart diapers for nursing home
residents with dementia: a pilot study. Acta Clinica
Belgica, 74(4):258–262.
Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A.,
and Jaffe, M. W. (1963). Studies of Illness in the
Aged: The Index of ADL: A Standardized Measure
of Biological and Psychosocial Function. JAMA,
185(12):914–919.
Lin, S. H., Kajiyama, K., and Wu, T. (2017). Smart Di-
aper: How It Works. In Proceedings of the 2017
ACM International Joint Conference on Pervasive and
Ubiquitous Computing and Proceedings of the 2017
ACM International Symposium on Wearable Comput-
ers, UbiComp ’17, pages 129–132, New York, NY,
USA. ACM. event-place: Maui, Hawaii.
Mather, K. F. and Bakas, T. (2002). Nursing assistants’
perceptions of their ability to provide continence care.
Geriatric Nursing, 23(2):76–81.
O’Dell, Katharine, K., Jacelon, C., and Morse, A. N.
(2008). ’I’d Rather Just Go On as I Am’ - Pelvic Floor
Care Preferences Of Frail, Elderly Women in Residen-
tial Care. Urologic Nursing, 28(1):36–47.
Offermans, M. P. W., Moulin, M. F. M. T. D., Hamers, J.
P. H., Dassen, T., and Halfens, R. J. G. (2009). Preva-
lence of urinary incontinence and associated risk fac-
tors in nursing home residents: A systematic review.
Neurourology and Urodynamics, 28(4):288–294.
Ouslander, J. G., Buxton, W. G., Al-Samarrai, N. R., Cruise,
P. A., Alessi, C., and Schnelle, J. F. (1998). Nighttime
Urinary Incontinence and Sleep Disruption Among
Nursing Home Residents. Journal of the American
Geriatrics Society, 46(4):463–466.
Ouslander, J. G. and Kane, R. L. (1984). The Costs of Uri-
nary Incontinence in Nursing Homes. Medical Care,
22(1):69–79.
Plotz, T., Chen, C., Hammerla, N. Y., and Abowd,
G. D. (2012). Automatic Synchronization of Wear-
able Sensors and Video-Cameras for Ground Truth
Annotation–A Practical Approach. pages 100–103.
IEEE.
Rantz, M., Skubic, M., Alexander, G., Aud, M., Wake-
field, B., Galambos, C., Koopman, R., and Miller, S.
(2010a). Improving Nurse Care Coordination With
Technology. Computers, informatics, nursing : CIN,
28:325–32.
Rantz, M., Skubic, M., Alexander, G., Popescu, M., A Aud,
M., J Wakefield, B., Koopman, R., and J Miller, S.
(2010b). Developing a Comprehensive Electronic
Health Record to Enhance Nursing Care Coordina-
tion, Use of Technology, and Research. Journal of
gerontological nursing, 36:13–7.
Strauven, H., Hallez, H., Vanden Abeele, V., and Vanrum-
ste, b. (2019). The Design and Development of an
Ambient Sensor System to Detect Incontinence.
Suzuki, R., Otake, S., Izutsu, T., Yoshida, M., and Iwaya,
T. (2006). Monitoring Daily Living Activities of
Elderly People in a Nursing Home Using an In-
frared Motion-Detection System. Telemedicine and
e-Health, 12(2):146–155.
T’Jonck, K., Strauven, H., Vankeirsbilck, J., Hallez, H., and
Boydens, J. (2019). Design and implementation of
an unobtrusive sensor system to support incontinence
care of elderly in nursing homes. Sozopol, Bulgaria.
Traynor, V., Yu, P., Hailey, D., and Fleming, R. (2014). An
exploration of the effects of introducing a telemoni-
toring system for continence assessment in a nursing
home. Journal of Clinical Nursing, 23:3069–3076.
Wagg, A., Kung Chen, L., Johnson II, T., Kirschner-
Hermanns, R., Kuchel, G., Markland, A., Orme, S.,
Ostaszkiewicz, J., Szonyi, G., and Wyman, J. (2017).
Incontinence in frail older persons. Incontinence : 6th
International Consultation on Incontinence, Tokyo,
September 2016, pages 1309–1442.
Wai, A. A. P., Foo, S. F., Jayachandran, M., Biswas, J., Nu-
gent, C., Mulvenna, M., Zhang, D., Craig, D., Pass-
more, P., and Lee, J.-E. (2010a). Towards develop-
ing effective Continence Management through wet-
ness alert diaper: Experiences, lessons learned, chal-
lenges and future directions. pages 1–8. IEEE.
Wai, A. A. P., Foo, S. F. V., Jayachandran, M., Biswas, J.,
Nugent, C., Mulvenna, M., Zhang, D., Craig, D., Pass-
more, P., and Lee, J.-E. (2010b). Technical develop-
ment and clinical evaluation of intelligent continence
management system at nursing home. pages 345–352.
IEEE.
Wai, A. A. P., Fook, F. S., Jayachandran, M., Song, Z.,
Biswas, J., Nugent, C., Mulvenna, M., Lee, J.-E., and
Yap, L. K. P. (2008). Smart wireless continence man-
agement system for elderly with dementia. pages 33–
34. IEEE.
Wai, A. P., Foo, S., Biswas, J., Donnelly, M., Parente, G.,
Nugent, C., and Yap, P. (2011). Smart phone reminder
system for managing incontinence at nursing home.
pages 254–259. IEEE.
Wilson, L., Brown, J. S., Shin, G. P., Luc, K.-O., and Subak,
L. L. (2001). Annual direct cost of urinary inconti-
nence. Obstetrics & Gynecology, 98(3):398–406.
HEALTHINF 2020 - 13th International Conference on Health Informatics
446
