
Vitiligo on Vogt-Koyanagi-Harada Disease
Meiza
1*
, Irvin Aldikha
1
, Renni Yuniati
1
, Radityastuti
1
, Meira Dewi Kusuma Astuti
2
1
Department of Dermatovenereology, Faculty of Medicine Diponegoro University / Dr. Kariadi General Hospital
5
Department of Pathological Anatomy Faculty of Medicine Diponegoro University / Dr. Kariadi General Hospital
*Telephone: 081360022801; email: meiza.dvjan18@gmail.
Keywords: Vogt-Koyanagi-Harada Disease, vitiligo, poliosis
Abstract: Vogt-Koyanagi-Harada (VKH) disease is a rare granulomatous inflammatory disease that affects the
pigmented structure. The etiopathogenic of this syndrome remains unclear; itis proposed as an autoimmune
disorder. Diagnosis of VKH is made based on least 3 of the following four criteria of The American Uveitis
Society (Bilateral iridocyclitis, posterior uveitis, neurological sign, cutaneous findings of vitiligo, poliosis or
alopecia) and an absence of prior trauma or surgery. Treatment for repigmentation of vitiligo is non-surgical
and/or surgical, which yield good result. This case report is aimed to give more understanding of the
diagnosis and management of vitiligo on VKH. A 47-year-old male with the complaint of white spots
presented previously on the face for three weeks. The patient was referred from the ophthalmology
department with bilateral iridocyclitis and panuveitis. There was no hearing loss. From the physical
examination, hypopigmented macules and poliosis were found on the eyebrows. Histopathological
examination supported the diagnosis of vitiligo. The patient was treated with methylprednisolone tablet 16
mg 2-0-1, and fluticasone propionate cream 0.05% every 12 hours on the affected skin. The prognosis of
this patient was quo ad vitam ad bonam quo ad sanam ad malam and quo ad cosmeticam dubia ad bonam.
In this case, we found 3 of the four criteria of diagnosis is Bilateral iridocyclitis, posterior uveitis, cutaneous
findings of vitiligo, and poliosis. The patient was given high potency topical corticosteroids twice daily and
oral corticosteroid. It showed significant clinical improvement after four months.
1 INTRODUCTION
Vogt Koyanagi Harada Disease is a rare
granulomatous inflammation that can affect
pigmentation structure, where the main target is a
cell which contains melanin on eyes, inner ear, brain
membrane, skin, and hair (Lavezzo et al, 2016;
Sakata et al, 2014; Anstery, 2010). In the beginning,
VKH disease be conceived as an
uveomeningoencephalitis syndrome (Lavezzo et al,
2016).
In 1906, Swiss’s ophthalmologist residency
student Alfred Vogt described the disease as
bilateral subacute iridocyclitis with early bleaching
on eyelashes. In 1926, Einosuke Harada reported 5
cases with posterior bilateral uveitis and retina
exfoliation after the inflammation is decreased.
Close with that time in 1929, Koyanagi published an
article that explained the pathogenesis of the disease,
includes prodromal phase, acute uveitis phase with
the involvement of posterior segment, the recovery
phase followed by hearing and skin manifestation. In
1932, Babel advised this disease is on the same form
with later named Vogt Koyanagi Harada (Lavezzo et
al, 2016; Sakata et al, 2014; Anstery, 2010).
Vogt Koyanagi Harada disease often affects the
individual with darkly pigmented people such as in
Asia, Hispanic, Origin American and Hindian and
Brazilian (Lavezzo et al, 2016; Burkholder, 2015;
Bilgic et al, 2014; Su et al, 2018).
Most of the
research informed that woman affected more than a
man with ratio 2:1 (Lavezzo et al, 2016; Burkholder,
2015; Bilgic et al, 2014; Ng el al, 2014).
Most of the
patients are on the second to fifth decade of the life
with a peak of the event on third and fourth
(Lavezzo et al, 2016; Burkholder, 2015; Bilgic et al,
2014; Bayer, 2016). Elderly and children can be
affected by the disease, and although it is rare, one
author reported that the youngest patient is three
years old girl (Lavezzo et al, 2016; Burkholder,
2015; Bayer, 2016). The prevalence and incidence of
VKH is a rare disease. In the USA the incidence of
VKH is about 1,5 – 6 cases per 1 million patients
while in Japan is about 800 new cases annually
(Lavezzo et al, 2016).
Meiza, ., Aldikha, I., Yuniati, R., Radityastuti, . and Astuti, M.
Vitiligo on Vogt-Koyanagi-Harada Disease.
DOI: 10.5220/0009989803890393
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 389-393
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
389

Etiology and pathogenesis of Vogt Koyanagi
Harada suspected to be a systemic autoimmune
disease which clearly unknown (Lavezzo et al, 2016;
Burkholder, 2015; Su et al, 2018). The Vogt
Koyanagi Harada may be systemic autoimmune
disease on melanosis that affects mainly on eyes,
inner ear, and brain membrane and skin (Lavezzo et
al, 2016; Su et al, 2018).
An author has reported a
case that one of the triggers of this disease is an
infectious agent such as Epstein-Barr Virus &
Cytomegalovirus. Trauma on the skin can be one of
the etiology of the disease, even though the
causative relationship between the virus and the
disease have not been established yet (Lavezzo et al,
2016; Burkholder, 2015; Ng et al, 2014).
The diagnosis of VKH disease was based on the
American Uveitis Society (AUS) criteria. The
physical examination also some criteria that have
been made to be diagnostic approachment (Lavezzo
et al, 2016; Sakata et al, 2014).
The diagnosis of
Vogt Koyanagi Harada disease was based on criteria
made by American Uveitis Society (AUS) criteria on
1978 and Sigiura
’
s criteria on 1976 (Lavezzo et al,
2016).
American Uveitis Society recommend,
without history of trauma and eyes surgery
procedure , at least there are 3 or 4 other criteria to
diagnose VKH disease, which are iridocyclitis
bilateral, posterior uveitis, neurology abnormality,
and skin abnormality likes vitiligo, poliosis, or
alopecia. The accurate diagnosis of VKH disease
can prevent complication (Bilgic et al, 2014).
The active and adequate treatment on early phase
can reduce the risk to recurrent. The early treatment
and aggressive corticosteroid are the best treatment
for this disease on acute uveitis phase, and also
corticosteroid treatment on this acute phase can
reduce the risk of lost sight permanently (Lavezzo et
al, 2016; Sakata et al, 2014; Burkholder, 2015; Ng et
al, 2014). The dosage of systemic corticosteroid is
given by oral is prednisone 1-1.5 mg/KgBB/Day, or,
methylprednisolone 1 gr/day for three days.
Treatment with corticosteroid must reduce slowly
and last at least for six months (Lavezzo et al, 2016;
Ng et al, 2014). The treatment for skin
depigmentation is the same with vitiligo treatment
(Bayer, 2016).
2 CASE
A 47 years old man, came with complaint of having
some white spots for three weeks ago. The white
spots appear on the face, It has been starting from
the chin and spreading through cheek, nose, and
forehead, the white spots are not itchy, and the
patient did not apply topical regimen to the spots.
His eyelashes had been starting to bleach when he
came to the hospital. The patient was referred from
the ophthalmology department. One year prior, the
patient suffered from fever, pain on eyes, and blurry
sight, headache without a history of trauma or eyes
surgery. In the ophthalmology department, the
patient is diagnosed with panuveitis and iridocyclitis
bilateral. On that time, there were no hearing
symptoms of ear buzzing and had no white spots on
face. The wound on the Genitalia was denied, no
similar history or symptoms in his family. General
condition was compos mentis, weel nourished with
height 165cm and weight 63kg, blood pressure is
120/80mmHg, respiratory rate 18x/m, and heart rate
is 80x/m, and axilla temperature is 37
0
C. Physical
examination, dermatology status is found
hypopigmented macules on face and poliosis on
dermatologic examination.
On laboratory testing the hemoglobin was 15
gr%; leucocytes 5.500/mm
3
; eritrocytes 4,3
juta/mm
3
; trombocytes 231.000/mm
3
; ureum 15
mg/dl; creatinin 0,8 mg/dl; SGOT 14 U/I; SGPT 45
U/I. VDRL and TPHA are negative.
The histopathologic examination found flat
sprained epithelial, creatine, follicular plugging, and
melamine pigment is not equal, stroma subepithelial
plain, contain sebaceous gland that suitable of
vitiligo. Diagnosis of this patient was Vogt
Koyanagi Harada disease. The treatment of vitiligo
to this patient is active potential topical
corticosteroid fluticasone 0,05 % applied every 12
hours on the face, and a systemic corticosteroid is
metilprednisolon 16 mg tab 2-0-1.
Repigmentation was found in the first month of
observation. Good clinical improvement was
observed after four-month.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
390
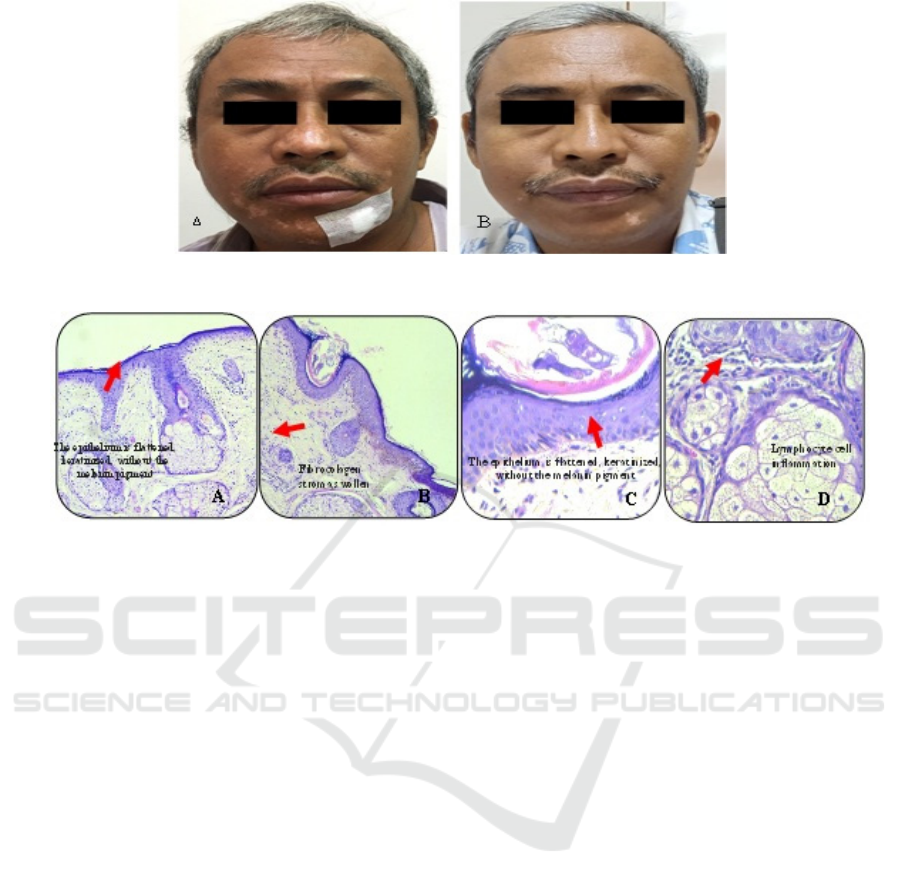
Figure 1. (A) Examination on
the first
month (B) Examination on
the fourth
month
Figure 2. Microscopic histopathology
3 DISCUSSION
Vogt Koyanagi Harada (VKH) disease shows some
manifestation, in clinical side VKH disease, has 4
phases, an early phase is a prodromal phase or called
meningoencephalitis phase, which happens for 3-5
days with a flu-like syndrome, fever, headache,
orbital pain, hearing problems, tinnitus and
neurology symptoms. On this phase, the
cerebrospinal fluid test will show limonitic
pleocytosis that happens for some weeks.
In this case, patient had suffered from prodromal
phase such as fever, pain in eyes, headache for 1
week, afterward patient had the second phase which
was acute uveitis generally happens on the 3th days
until 5th days from prodromal phase and occurs for
some weeks until several months, with blurry vision,
photophobia, pain on eyes, loss of vision in one or
both of eyes. The patient was diagnosed with
panuveitis, and iridocyclitis bilateral by the
ophthalmologist with clinical symptoms is a blurry
vision, but the patient has no dysacusis, tinnitus, or
other hearing problem. The 3rd phase or
convalescence phase occurs some weeks after acute
uveitis phase. This phase started with
depigmentation, progressive tissue; on this stage,
there is skin involvement with vitiligo appearance,
poliosis, and alopecia. The clinical symptoms on the
skin occur for some months or even some years.
(Lavezzo et al, 2016;Sakata et al,2014; Burkholder,
2015; Bilgic et al, 2014)
Vitiligo develops on 19-90% cases, vitiligo
usually symmetrical and can occur in every area of
the body likes on face and back area are the most
common. The histopathologic finding showed there
was no melanosis. Poliosis occurs most on
eyebrows, eyelashes, and scalp. Alopecia can occur
as areata alopecia or diffuse hair loss (Burkholder,
2015; Bilgic et al, 2014;Ng JY et al,2014) On the
third phase, and this patient had vitiligo that was
spreading, followed by poliosis on eyebrows.
The diagnosis of Vogt Koyanagi Harada was
based on clinical symptoms. Some criteria have been
made to achieve the diagnostic, include America
Uveitis Society on1978, Sugiura on 1976. On 1999,
an international workshop for some expert made
diagnosis revision, the criteria published on 2001
which has three categories such as Complete Vogt
Koyanagi Harada disease, Incomplete Vogt
Koyanagi Harada, and suspect Vogt Koyanagi
Harada. (Lavezzo et al, 2016;Sakata et
al,2014;Anstery et al,2010)
Vitiligo on Vogt-Koyanagi-Harada Disease
391

From these three categories, there are absolute
requirements: bilateral eyes problem, no history of
trauma or eyes surgery.(Burkholder, 2015)
Revised Diagnosis Criteria on the international
workshop I in 2001
2
Complete disease (Criteria 1-5 must be found)
1. There is no history of ocular trauma or surgery
before the initial onset of uveitis
2. There is no clinical evidence that shows other eye
diseases
3. The involvement of both eyes
a. Rapid disease manifestations
- Diffuse choroiditis
- Alternatively, the characteristics of
fluorescein angiography and echography
findings are diffuse choroidal
thickening
b. Slow disease manifestations
- History of previous uveitis with the
characteristics described above
Ocular depigmentation (fundus sunset
glow, Sugiura sign)- and other ocular signs
(nummular chorioretinal scar, pigmented
epithelial clots or recurrent or chronic
anterior uveitis)
4. Symptoms of nerves and symptoms of hearing
5. Integumentary symptoms (alopecia, vitiligo, or
poliosis)
Incomplete disease (Criteria 1 to 3 plus one of 4 or 5
must be found)
Possible disease (Isolated eye disease, criteria 1 to 3
must be found)
This patient was suitable with the incomplete
Vogt Koyanagi Harada disease are met. This patient
has no history of penetrating ocular trauma and
surgery at the onset of uveitis and no laboratory
results that support other eye diseases.
Differential diagnosis with Alezzandrini's
syndrome can be ruled out. Alezzandrini syndrome
is characterized by ipsilateral facial vitiligo, with
unilateral taporetinal regeneration of the eyes, white
hair, poliosis, and hearing loss. Vitiligo facials and
poliosis in the eyebrows and eyelashes usually occur
after several years of abnormalities in the eye.
(Anstery et al,2010;Bilgic et al,2014;Bleue,2016)
.
In
this patient found facial vitiligo accompanied by
poliosis in the eyebrows and panuveitis with
bilateral iridocyclitis.
Treatment of vitiligo in Vogt
Koyanagi Harada disease can be treated according to
vitiligo.(Bayer,2016) The main goal of vitiligo
therapy is repigmentation, while the secondary goals
include stabilization of the disease to stop the loss of
functional melanocytes, and ensure adequate
psychosocial care and quality of life. (Bleue,2016)
Specific therapy for vitiligo repigmentation can be
done surgically and non-surgical.
10
Grafting can be done surgically such as punch
grafts, blister grafts, split-thickness skin grafts, and
hair follicle grafts. Surgical therapy is only
recommended for patients with a stable history of
the disease for the past 6-24 months and should only
be used for small size lesions. The surgical
procedure is generally followed by a 3-4 week
phototherapy procedure. (Bleue,2016;Stanca et
al,2012)
Topical treatments can be given, including
corticosteroids topical, calcineurin inhibitors,
calcipotriol, topical vitamin D analogs. Physical
therapy with UVB, PUVA, laser excimer. Systemic
therapy with corticosteroid use. (Bayer, 2016;Bleue,
2016;Stanca et al,2012).
Corticosteroids are the first-line therapy for
localized vitiligo and are highly recommended for
faces or small size lesions, and for children, the
benefit of corticosteroid is easy to use low cost
compared to PUVA. PUVA has proven to be less
effective and has more side effects compared to
UVB. (Bleue,2016;Stanca et al,2012)
The prognosis of this patient was quo ad vitam
ad bonam, quo ad sanam dubia ad malam, quo ad
cosmetikam dubia ad malam. Inadequate treatment
is the main factor associated with worse prognosis.
2
Improvements in visual impairment depend on the
rapid and precise management, and ocular symptoms
are usually right. Disorder of the skin may be
permanent last longer. (Bilgic et al,2014;Stanca et
al,2012)
4 CONCLUSION
A case of patient vitiligo in Vogt Koyanagi Harada
disease was reported in a 47-year-old male patient,
and Physical examination found hypopigmented
macules on the face and poliosis on the eyebrows.
Histopathologic examination was suitable with
vitiligo. Vogt Koyanagi Harada disease Therapy
with systemic and topical corticosteroid after four
months gave good clinical result. The prognosis of
the patient was quo ad vitam ad bonam, quo ad
sanam dubia ad malam, quo ad cosmetikam dubia ad
malam
REFERENCES
Anstery AV. 2010. Disorders of skin colour. In: Burns T,
Breatnach S, Cox N, Griffith C, editors. Rook
’
s
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
392

Textbook Of Dermatology, 8
th
edition. Weat Sussex:
Blackwell Publishing.. p.58.45-46
Bayer ML. 2016. Successful Treatment of Vitiligo
Associated with Vogt–Koyanagi. 1-2
Bilgic O. Abuzer G. Kaya K. 2014. Vogt-Koyanagi-
Harada Disease in an Adolescent Boy. Pediatric
Dermatology. 99–101.
Bleue R, Eberlein B. 2018. Therapeutic management of
vitiligo. Deutsche Dermatologische Gesellschaft
(DDG). 1-5
Burkholder MB. 2015. Vogt–Koyanagi–Harada disease.
Curr Opin Ophthalmol. 26:506–11.
Lavezzo MM, Sakata VM, Morita C, et.al. 2016. Vogt-
Koyanagi-Harada disease: review of a rare
autoimmune disease targeting antigens of
melanocytes. Orphanet J Rare Dis.11(29):1-21.
Ng JY, Luk OJ, Lai YY, et.al. 2014. Influence of
molecular genetics in Vogt-Koyanagi-Harada disease.
Journal of Ophthalmic Inflammation and Infection.
4(20):1-12
Sakata VM, Silva FT, Hirata CE, et.al. 2014. Diagnosis
and classification of Vogt–Koyanagi–Harada disease.
Autoimmunity Reviews. 1-6.
Stanca AB, Richard AS, David AN. 2012. Vitiligo. In:
Wollf, K, et.al. Gold Smith L, Katz S, Gilchrest, Palle
A, Editors. Fitzpatrick’s Dermatology In General
Medicine.8
th
edition. New York: Mc. Graw Hill. p.
792-803
Su E, Oza. SV, Latkany P. 2018. A case of recalcitrant
pediatric Vogt-Koyanagi-Harada disease successfully
controlled with adalimumab. Journal of the Formosan
Medical Association. 1-6
Vitiligo on Vogt-Koyanagi-Harada Disease
393
