
Generalized Pustular Psoriasis in Childhood
Milka Wulansari Hartono
1
*, Ernawati Hidayat
1
, Buwono Puruhito
1
, Asih Budiastuti
1
,
Meira Dewi Kusuma Astuti
2
1
Department of Dermatovenereology, Faculty of Medicine, Diponegoro University /
Dr. KariadiGeneral Hospital
2
Department of Pathological Anatomy, Faculty of Medicine, Diponegoro University /
Dr. Kariadi General Hospital
*
Corresponding auhtor
Keywords: Childhood generalized pustular psoriasis, cyclosporine
Abstract: A Generalized pustular psoriasis is a rare form of psoriasis in children. The prevalence of psoriasis in
children is ≈0.71%, the pustular type occurring in 0.6-7%.It is more severe in children and characterized by
a generalized pustule, forming the lake of pus, on an erythematous base.A 9-year-old boy presented with
fever and sudden onset of pustules eruption on erythematous base over the face, trunk, and extremities.
There was no past or family history of psoriasis. The laboratory result was leucocyte count 14.000/ µL,
CRP1,43 mg/L, qualitative ASTO (+). Histopathologic examination revealed skin lesions with psoriasiform
reactions, microabscess munro (+), dermis contained adnexa of the skin, stroma hyperemia with
lymphocytes, histiocytes, PMN leucocytes, supporting the diagnosis of generalized pustular psoriasis.
Patient was treated with cyclosporine tablet 3 mg/kgbw/day, desoximetasone cream 0,25% twice
daily,loratadine tablet 10 mg/day, paracetamol tablet3x500 mg.Generalized pustular psoriasis often requires
systemic and topical therapy because of the severity of the disease.Cyclosporin is recommended as a first-
line drug for pediatric generalized pustular psoriasis. Cyclosporin acts by inhibiting T-cell and IL-2.
Treatment using oral cyclosporin gave a good outcome in this patient. The eruptions markedly improved
after administration of oral cyclosporine 3 mg/kgbw/day for seven days.Topical treatment using a potent
corticosteroid, which has antiinflammatory and antiproliferative properties were co-administered to
increase the efficacy.Prognosis quo ad vitam ad bonam, quo ad sanam dubia ad bonam dan quo ad
kosmetikamad bonam.
1 INTRODUCTION
Psoriasis is a chronic inflammatory skin
disease,characterized by complex alterationsin
epidermal growth and differentiation (Gudjonsson et
al, 2012; Griffi et al, 2010).
The exact etiology and
pathogenesis is unknown but immunologic
drivenmediated primarily by T cells in the dermis,
genetic andenvironmental factors also are implicated
in the development of the disease (Gudjonsson et al,
2012; Griffi et al, 2010; Voorhees et al, 2019).
Psoriasis is universal in occurrence, affecting 2
to 4% of the world’s population, equally common in
males and females, may begin at any age, but it is
uncommon under the age of 10 years (Saikaly et al,
2016).
The prevalence of psoriasis in children is ≈
0.71%.Many subtypes of childhood psoriasis have
been described, including generalized pustular
psoriasis (GPP), which is arare form, affecting 0,6-
7% of psoriasis patients (Gupta et al, 2015; Bhuiyan
et al, 2017).
Generalized pustular psoriasis is a rare type of
psoriasis first described in 1910 by Von Zumbusch,
and it is the most severe type and can be potentially
life-threatening. It presents abruptly
withconstitutional symptoms and diffuse
erythematous lesions, followed by yellow-colored
sterile pustules.The etiology of pustular psoriasis is
uncertain. Its onset has been associated with
triggering factors such as trauma, infections,
emotional stress, vaccinations, sunlights, metabolic
factors, alcohol and smoking, drugs, and HIV. The
abrupt withdrawal of systemic and topical
corticosteroids and the withdrawal of cyclosporin
have also been implicated (Gudjonsson et al, 2012;
352
Hartono, M., Hidayat, E., Puruhito, B., Budiastuti, A. and Astuti, M.
Generalized Pustular Psoriasis in Childhood.
DOI: 10.5220/0009988603520356
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 352-356
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Griffi et al, 2010; Voorhees et al, 2019; Saikaly et al,
2016; Hoegler et al, 2018).
The pathogenesis of GPP is only partially
understood. GPP can present in patients with
existing or prior psoriasis Vulgaris or in patients
without a history of psoriasis Vulgaris. More than
half of the GPP individual cases are caused by
recessive mutations in IL36RN. IL36RN encodes
interleukin-36-receptor antagonist (IL-36Ra), which
antagonizes three interleukin cytokines (IL-1F6, IL-
1F8, and IL-1F9) that are involved in the activation
of pro-inflammatory signaling pathways (Hoegler et
al, 2018).
The clinical presentation of generalized pustular
psoriasis usually presents with 2-3 mm sterile
pustules overlying painful, erythematous skin.
Patients are visibly ill, with high-grade fever,
malaise, leucocytosis, elevated C-reactive protein
levels (Hoegler et al, 2018). Diagnostic criteria
proposedby Umezama et al. are consisted of 1)
multiple sterile pustules overlying erythematous
skin, 2) fever, malaise and other systemic symptoms,
3) Kogoj spongiform pustules on histopathological
analysis, 4) laboratory abnormalities including left
shift leucocytosis, elevated erythrocyte
sedimentation rate, elevated CRP, elevated ASTO
levels, elevated IgG or IgA levels, hypoproteinemia,
hypocalcaemia, 5) recurrence of these
clinical/histopathological features. (Hoegler et al,
2018) The differential diagnosis of pustular psoriasis
is with acute generalized exanthematous pustulosis
(AGEP), but AGEP tends to occur and resolve more
quickly and is particularly associated with antibiotic
use (Hoegler et al, 2018).
For the diagnostic examination, we can do a
biopsy for a histopathology examination. The
histopathology findings in pustular psoriasis consist
of confluent parakeratosis, hyperkeratosis,
neutrophils in stratum corneum (Munro
microabscesses) and in spinous layer (spongiform
pustules of Kogoj), hypergranulosis,sub-
parapapillary thinning of the epidermis, regular
acanthosis, often with clubbed rete ridges, dilated
capillaries in dermal papillae, perivascular
lymphocytes (Rapini, 2012).
A broad spectrum of antipsoriatic treatments,
both topical and systemic, is available for the
management of psoriasis (Gudjonsson et al, 2012).
In patients with erythrodermic and pustular
psoriasis, treatments with acitretin, methotrexate, or
short-course cyclosporine are the treatments of the
first choice (Gudjonsson et al, 2012).
For children
with GPP, first-line treatment is similar to that
inadults.As retinoids can cause premature epiphyseal
closure,skeletal hyperostosis, and extraosseous
calcification, it maynot be ideal first-line therapy.
Cyclosporine has fewer knownsideeffects and is
often the first treatment used before
retinoids.Methotrexate is not approved in children
under the age of 2 years.Both methotrexate and
cyclosporine must be used with cautionbecause of
the long-term oncogenic potential.A recent
retrospective chart review assessed the efficacy of
cyclosporine in pediatric patients having extensive
plaquetype, erythrodermic, and pustular psoriasis.
Excellent efficacy (>75% reduction in PASI) was
observed in all but three patients (Gudjonsson et al,
2012; Rapini, 2012; Dogra et al, 2017; James et al,
2016; Dogra et al, 2018). Corticosteroids shouldbe
utilized with caution, especially in patients with
concomitantpsoriasis Vulgaris because of the
potential to initiate flares.Combination therapies are
employed in almost 50% of the children with
generalized pustular psoriasis in order to provide
optimum disease control. Pustular psoriasis in
children has a more favorable course as compared to
adults. The response to treatment is good, and
remission lasts longer as compared to adults (Dogra
et al, 2018).
2 CASE
A nine-year-oldboy, Indonesian people, Javanese,
was brought by her parents to the dermato-
venereology clinic in Karyadi General Hospital on
August 10
th
, 2018 with a chief complaint ofsudden
onset of pustules eruptions on an erythematous
baseover the face, trunk, and extremities.
The lesions were developed within 24 h after the
patient got vaccinated in his school. The lesion was
initially on his face then became more generalized
with the involvement of the face, trunk, and
extremities. The symptoms were alsoaccompanied
by fever and pain on his body.Then his parents
brought him to a dermatologist. There he received
treatment with topical cream and oral capsule, but
the lessons did not improve, so he was referred to
Karyadi Hospital.
The patient did not suffer from any other
diseases or use any topical or systemic medication
before. He had no food or drug allergy. Therewas no
past and family history of dermatosis, including
psoriasis. The patient was the first child, and he has
a healthy 5-year-old little brother. He was in 2
nd
-
grade junior high school, and his academic status
was functional. His parents worked as an employee.
Generalized Pustular Psoriasis in Childhood
353
The payment method was using BPJS insurance, and
the economic status impression was low.
On the initial physical examination, the patient
was looked ill-appearance, body height: 120 cm and
body weight: 17 kg. He had a fever, t = 38
0
C. He
also had difficulty to walk because of the pain on his
leg. On the dermatology, examination showedtypical
widespreadpustules that developed on an
erythematous base on his face, trunk, and
extremities. (figure 1).
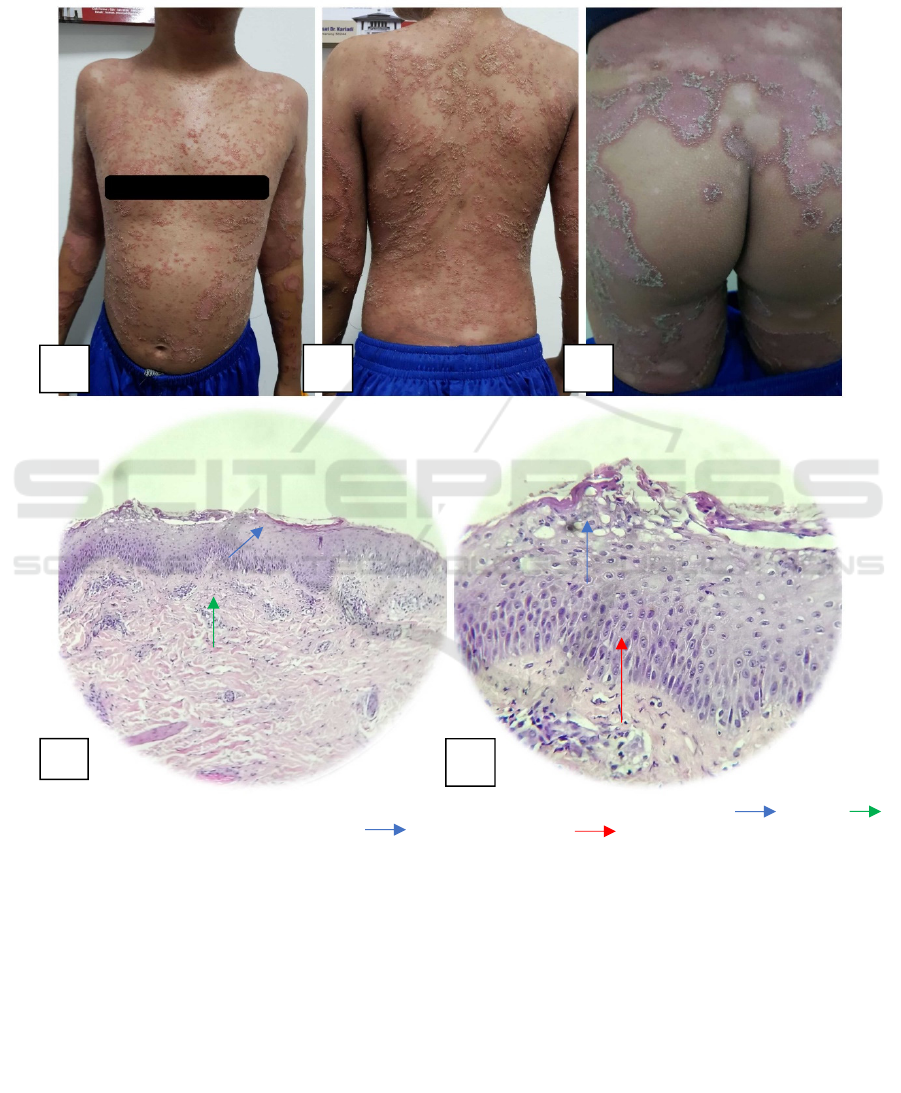
Figure 1. A&B&C. The clinical appearanceof the lesion. D. (i) Histopathology examination showed: parakeratosis,
dermis with lymphocytes and PMN leucocytes E. Munro’s microabsces sAcanthosis
Then we did the laboratory examination, and
there were some abnormality including, leucocyte
count 14.000/ µL, CRP 1,43 mg/L, qualitative
ASTO (+). Histopathologic examination revealed
skin lesions with psoriasiform reactions, Munro's
microabscess (+), dermis contained adnexa of the
skin, stroma hyperemia with lymphocytes,
histiocytes, PMN leucocytes, supporting the
diagnosis of generalized pustular psoriasis. (figure 1)
Based on history taking, physical and
dermatology examination, laboratory and
histopathology examination, the diagnosis of
generalized pustular psoriasis was made. Differential
diagnosis with drug reaction was eliminated.
The patient was treated withcyclosporine tablet 3
mg/kgbw/day, desoximetasone cream 0,25% twice
daily, loratadine tablet 10 mg/day, paracetamol
tablet 3x500 mg. The patient experienced rapid
improvement of his skin lesion. At one week follow
up, the skin had markedly improved. (figure 2)Then
the dosage of cyclosporine was tapered off.
A
B C
D
E
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
354

Figure 2. Clinical improvement after one-week administration of cyclosporine and topical desoximetasone Discussion
Diagnosis ofgeneralized pustular psoriasiswas
made based onhistory taking, physical and
dermatology examination, laboratory, and
histopathology examination.
From history-taking, a 9-year-old boy had suddenly
developed widespread pustules on an erythematous
base, 24 hr after he got vaccinated in his school.
There was no past and family history of dermatosis,
including psoriasis, and he also admitted that he did
not use any topical or systemic medication before.
According to the theory, psoriasis is a complex
inflammatory skin condition with abnormal
epidermal keratinocyte differentiation and
hyperproliferation.It is universal in occurrence,
equally common in males and females, may begin at
any age, but it is uncommon under the age of 10
years. The exact etiology and pathogenesis is
unknown but immunologic, genetic, and
environmental factors with triggering factors such as
trauma, infections, emotional stress, vaccinations,
sunlights, metabolic factors, alcohol and smoking,
drugs and HIValso are implicated in the
development of the disease. (Gudjonsson et al, 2012;
Griffi et al, 2010; Voorhees et al, 2019;Saikaly et
al,2016).
From the physical examination, the patient
presented typical widespread pustules that developed
on an erythematous base on his face, trunk, and
extremities, accompanied by constitutional
symptoms such as fever and tenderness on the
lesion. Psoriasis has many clinical patterns of skin
presentation, such as psoriasis vulgaris, guttate
psoriasis, small plaque psoriasis, inverse psoriasis,
erythrodermic psoriasis, pustular psoriasis. Several
clinical variants of pustular psoriasis exist
generalized pustular psoriasis (von Zumbusch type),
annular pustular psoriasis,impetigo herpetiformis,
and two variants of localized )and acrodermatitis
continua of Hallopeau.Generalized pustular psoriasis
is a distinctive acute variant of psoriasis. It is
characterized by fever, and sudden generalized
eruption of pustules arise on erythematous skin. This
form of psoriasis is usually associated with
prominent systemic
signs and can potentially have life-threatening
complications. (Gudjonsson et al, 2012)
A laboratory and histopathological examination
were done. Findings revealed some abnormalities
such asleucocyte count 14.000/ µL, CRP 1,43 mg/L,
qualitative ASTO (+). Histopathologic examination
revealed skin lesions with psoriasiform
reactions,Munro's microabscess (+),dermis
contained adnexa of the skin, stroma hyperemia with
lymphocytes, histiocytes, PMN leucocytes. It is
consistent with generalized pustular psoriasis’
histopathology findings.
The treatment in this patient were usingcyclosporine
tablet 3 mg/kgbw/day(tapered-off after 1 week),
desoximetasone cream 0,25% twice daily, loratadine
tablet 10 mg/day, paracetamol tablet 3x500
mg.According to the theory, combination therapies
are employed in almost 50% of the children with
generalized pustular psoriasis in order to provide
optimum disease control. An initial daily oral
regimen of 2.5 mg/kg cyclosporine equally divided
in two doses has been recommended. Improvement
may be seen within days, but if this does not occur
within two weeks, the dosage may be increased
gradually to a maximum of 5 mg/kg/day.
Maintenance dosage should be reduced to the
minimum that allows adequate control A systematic
review of therapies for severe psoriasis concluded
that ‘cyclosporine is a well-tested treatment for
severe psoriasis and in the short term, ideally 3-4
months, is probably more effective than other forms
of systemic therapy's (Griffi et al, 2010)
Topical corticosteroidwas used in adjunct to
systemic cyclosporine as local therapyto increase the
efficacy, but the duration and the dosage should be
monitored carefully because of the potential
Generalized Pustular Psoriasis in Childhood
355

induction of pustules. The paracetamol and
loratadine herewere used as symptomatic
therapy.(Fujita et al,2018).
In this case report,the patient experienced rapid
improvement of his skin lesion. At one week follow
up, the skin had markedly improved. Prognosis quo
ad vitam ad bonam, quo ad sanam dubia ad bonam
dan quo ad kosmetikamad bonam.
3 CONCLUSION
Generalized pustular psoriasis is a rare form of
psoriasis, and onset at children is even rarer. In this
case report, combination therapies using systemic
cyclosporine and topical desoximetasone, gave a
good outcome. There are many factors influence the
remission and relapse/worsening of this disease, so
despite the therapy, we also provided education for
the patient and her family that his disease was a
chronic disease, and could be triggered with various
factors and to maintain the remission, it needed
cooperation between patient, doctors, and parents.
REFERENCES
Bhuiyan MSI, Zakaria ASM, Haque AKMZ, Shawkat SM,
Sultana A. 2017. Clinico-epidemiological study of
childhood psoriasis. Bangabandhu Sheikh Mujib Med
Univ J. 10(2):119.
Dogra sunil, Bishnoi Anuradha. 2018. Childhood
Psoriasis: What is New and What is News. Indian
Journal of Paediatric Dermatology. 308-14
Dogra S, Mahajan R, Narang T, Handa S. 2017. Systemic
cyclosporine treatment in severe childhood psoriasis:
A retrospective chart review. J Dermatolog Treat.
28(1):18–20.
Fujita H, Terui T, Hayama K, Akiyama M, Ikeda S,
Mabuchi T, et al. 2018. Japanese guidelines for the
management and treatment of generalized pustular
psoriasis: The new pathogenesis and treatment of
GPP. J Dermatol. 45(11):1235–70
Griffi th CEM, Camp RDR HI, Baker J. 2010. Psoriasis.
In: Burn T, Breathnach S, Cox N, Griffi th C, editors.
Rook’s textbook of dermatology. 8th ed.
Massachussets: Blackwell Publishing. p.351- 69.
Gudjonsson JE, Elder JT. 2012. Psoriasis. In: Wolff K,
Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leff
el DJ, editors. Fitzpatrick’s dermatology in general
medicine. 8th ed. New York: McGraw-Hill
Companies Inc. p.197-231.
Gupta S, Deo K, Wadhokar M, Tyagi N, Sharma Y. 2015.
Juvenile generalized pustular psoriasis in a 10-year-
old girl. Indian J Paediatr Dermatology. 0(0):0
Hoegler KM, John AM, Handler MZ, Schwartz RA. 2018.
Generalized pustular psoriasis: a review and update
on treatment. J Eur Acad Dermatology Venereol.
32(10):1645–51
James WD, Elston DM, G.Berger T, editors. 2016.
Seborrheic Dermatitis, Psoriasis, Recalcitrant
Palmoplantar Eruptions, Pustular Dermatitis, and
Erythroderma. In: Andrew’s Diseases of The Skin
Clinical Dermatology. twelfth ed. Philadelphia:
Elsevier Inc. 187-95
Rapini RP. 2012. Eczematous and Papulosquamous
Diseases. In : Practical Dermatopathology. 2nd
edition. London: Elsevier Saunders. 52-4
Saikaly SK, Mattes M. 2016. Biologics and Pediatric
Generalized Pustular Psoriasis: An Emerging
Therapeutic Trend. Cureus.8(6).
Voorhees AV, Wanat Karolyn. 2019.
Psoriasis:Erythrodermic and Pustular Variants.
Clinical Advisor Dermatology.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
356
