
False Alarm: Cutaneous Anthrax Suspicion
in a Case of Bullous Erysipelas - The Clinicopathological
Consideration
Randy Satria Nugraha Rusdy
1*
,Teffy Nuary
1
, Sri Linuwih S. W. Menaldi
1
, Rahadi Rihatmadja
1
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia/
Dr. Cipto Mangunkusumo National CentralGeneral Hospital, Indonesia
Keywords: Bullous Erysipelas, Cutaneous Anthrax, Histopathology
Abstract: Erysipelas is acute superficial infection involving the epidermal and dermal layers, which may feature
bullous formation. Bullous erysipelas lesion can mimic Sweet’s syndrome, pyoderma gangrenosum and
other skin and soft tissue infections (SSTIs). A 42-year-old male presenting with multiple erythematous and
edematous plaques with a large bulla on his left lower leg was first diagnosed clinically with Sweet’s
syndrome or pyoderma gangrenosum. Routine histopathology showed partial epidermal necrosis and
massive dermal edema with neutrophils, lymphocytes and nuclear dust, which might be consistent with the
aforementioned diagnoses. However, taking into account the clinical presentation, the possibility of
cutaneous Anthrax was also raised, especially when the patient was later found to work in areas where
domesticated animals roamed. Further investigation with Gram staining did not demonstrate Gram-positive
bacilli, negating the suspicion. Cefadroxil as prophylaxis which later continued with clindamycin gave
marked improvement. Clinical and histological findings, and response to antibiotics favored bullous
erysipelas as the final diagnosis.
1 INTRODUCTION
Erysipelas is an acute superficial infection and
inflammation of the skin, that features a painful,
warm, erythematous swollen lesion, with sharply
demarcated border. Systemic signs and symptoms
include fever, nausea, vomiting, general weakness,
muscle pain, and lymphedema. (FY Chong et al.,
2008). Usually involving epidermal and dermal
layers, 5% of erysipelas can be complicated by bulla
formation which represents deep seated process,
such as in bullous erysipelas.(S Vichitra et al 2016)
Bullous erysipelas lesions were characterized by
erythematous macules and patches with flaccid
epidermal sterile blister. (S Vichitra et al 2016).
Usually appears on facial areas and legs, they can be
accompanied with necrosis and purpuric hemorrhage
which take longer period of tissue repair.
Not only difficult to treat and related to more
complications, bullous erysipelas with atypical
presentation can mimic other disease, such as
Sweet’s syndrome, pyoderma gangrenosum, and
other skin and soft tissue infections (SSTIs) that are
diagnostically challenging. Histopathology
examination shares many similar features among
erysipelas and those diseases, including cutaneous
anthrax. Therefore, clinical recognition coupled with
knowledge of pathology of diseases contribute
greatly to making sound diagnosis. We present a
case of challenging diagnostic approach in a case of
bullous erysipelas that was nearly mistaken for
cutaneous anthrax.
2 CASE
A 42-year-old male came to our department’s
outpatient clinic presenting with several painful
erythematous lesions on the rightlower leg on March
2017.They had appeared since approximately 10
days before. A blister had appeared some days after
and a tentative aspiration was performed at another
hospital. However, the lesion became ulcerated.The
patient was feverish and his lower leg was swollen.
Previous treatment comprised of amoxycillin-
clavulanic acid and non steroidal anti-inflammatory
drug. History of trauma, skin lesion, or application
Rusdy, R., Nuary, T., Menaldi, S. and Rihatmadja, R.
False Alarm: Cutaneous Anthrax Suspicion in a Case of Bullous Erysipelas - The Clinicopathological Consideration.
DOI: 10.5220/0009986602770281
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 277-281
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
277
of substances was denied, as was history of diabetes
mellitus, hypertension, malignancy, alcohol and
smoking. The patient worked in the municipal
sanitary and environmental department, mostly
behind the desk but regularly supervised workers in
the region.
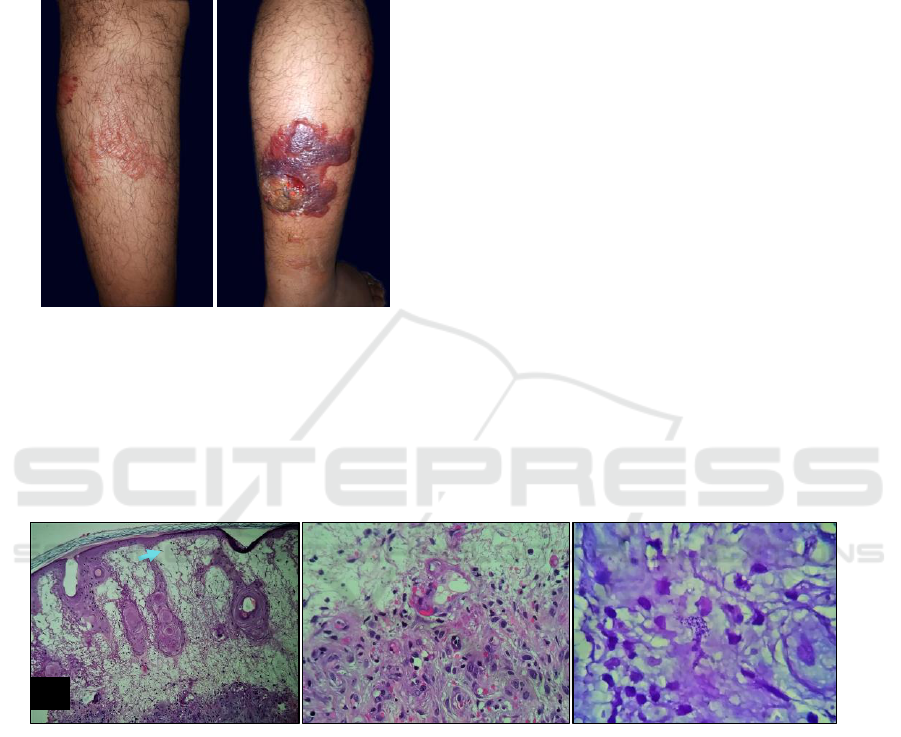
Figure 1.Purpuricand erythematous plaques with a large
hemorrhagic blister on the right lower leg. Swelling was
noted.
There were purpuric and erythematous plaques on
the right lower leg, with extensive edema. A large
hemorrhagic blister was present in the area where a
puncture was previously done. Vital signs and
general physical examination were normal, except
for BMI of 32.92 kg/m
2
. Laboratory result were also
in normal ranges, except increase in erythrocyte
sedimentation rate/ESR (74 mm/hour) and low
eosinophil count (0,9%).Swab from the hemorrhagic
base of the blister showed few Gram-positive cocci
and leukocytes. Aworking diagnosis of Sweet’s
syndrome with differential diagnosis of pyoderma
gangrenosum was made.
Biopsy was performed on two sites, the
erythematous plaque on the anterolateral leg and the
blister margin. Patient received cefadroxil 500 mg
twice a day for a week after biopsy and continued
with clindamycin 300 mg for possible infection.
Hematoxylin and eosin staining from both sites
demonstrated severe upper dermal edema leading to
blister formation, perivascular lymphocytes and
neutrophils, and erythrocyte extravasation. Necrosis
of epidermis and adipocytes in some parts was
noted. These histopathology findings alerted us of
the likelihood of cutaneous anthrax. Patient were
reexamined for possible infection of anthrax. Patient
acknowledged there were many domestic animals
(i.e. goat) where he worked, but no history of direct
contact previously before the lesion appeared. There
was no report of similar casein the environment
where he worked.
Figure 2. A. Marked edema on the upper dermis (blue arrow) and destruction of hair follicles (H&E,100x). B. Infiltrate of
inflammatory cells in dermal layer consisted of neutrophils, lymphocytes, nuclear dusts, and few eosinophils with
endothelial impairment and erythrocytes extravasation (pink arrow) (H&E, 1000x).C. No bacilli were found in Gram stain.
Structures resembled Gram-positive coccus (yellow arrow) sparsely distributed in dermal layer (Gram, 1000x).
Special staining did not reveal Gram-positive
bacilli which did not support diagnosis of cutaneous
anthrax and showed what looked like Gram-positive
cocci, suggesting the more likely cause of infection
for bullous erysipelas.
Ultrasonography by vascular surgeon concluded
lymphedema, although d-dimer and fibrinogen test
result were in normal limits, which did not support
deep vein thrombosis. Patient was suggested to wear
compression stocking. The condition gradually
improved with systemic antibiotics, and additional
treatment with normal saline wet dressing and
sodium fusidic ointment. Clindamycin already given
as prophylaxis and was continued for another two
weeks after biopsy until all lesions resolved and
leaving residual hyperpigmentation. The patient was
finally diagnosed with bullous erysipelas.
A
B
C
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
278

Figure 3. Evaluation after biopsy and receiving antibiotics
revealed marked improvement. Erythema and edema
subsided.
3 DISCUSSION
There was slight difficulty in assessing the condition
that we believe was due to non-classical clinical
presentation that might be interpreted as non-
infectious in origin, such as Sweet’s syndrome and
pyoderma gangrenosum. Sweet’s syndrome (SS)
lesion is characterized by tender, glistening
erythematous plaque that gives the impression of
vesiculation, while pyoderma gangrenosum (PG)
may have several variances, including ulceration
with violaceous border. (Cohen PR et al., 2016;
Cowell FC et al., 2008).However, disease history
and clinical data did not support the two entities.
Initially, infection was not considered because
there was no known trauma preceding the lesion.
The lesions appeared abruptly and accompanied by
fever and pain which was first thought to be clinical
manifestation of Sweet’s syndrome. There was
history of blister aspiration which later exacerbated
lesion. Moreover, there was no history of
malignancy, systemic infection, medication, or
inflammatory bowel disease which were usually
found in SS.(Cohen PR et al., 2016).
Pyodermagangrenosum usually occurred in older
people, with various underlying morbidity, that was
still doubtful in our case. Nevertheless, it was
diagnosis of exclusion that required ruling out other
diseases.(Cowell FC et al., 2008).
Regional lymph node enlargement and edema,
however, might suggest underlying infection.
Laboratory result did not support leukopenia and
neutropenia, although there was higher result of
erythrocyte sedimentation rate.(Cohen PR et al.,
2016). Our case showed low neutrophil count which
was not consistent with infection and SS.
Bullous formation, along with abscess,
hemorrhagic purpura and necrotic lesion are major
local complications usually found in erysipelas.
Local complication occurred around 31-52%
patients with erysipelas. It is associated with several
risk factors, including age ≤ 50 years, female gender,
obesity, smoking, history of diabetes mellitus,
hypertension, heart disease, and prior treatment with
non-steroidal anti-inflammatory drug. (Krasagais KI
et al., 2006). A comparison study in 2015 between
erysipelas patients with localized complication and
without showed history of antibiotic before
admission (OR = 5.15) and accelerated erythrocyte
sedimentation rate (OR = 5) as independent risk
factors. (Montravers P et al., 2016). Our case was
obese and had history of short-course amoxicillin-
clavulanic acid and anti-
inflammatorymedication.Possible sources of
infection in erysipelas including leg ulcer,
excoriating skin disease, and ascending infection
from distal limb inoculation, which usually follow
toe-web fungal infection. (Jendoubi F et al., 2019).
Since we did not find any signs mentioned above in
our case, we assumed the more likelihood of
microtrauma as the source of inoculation. As we
could not ascertained the origin of infection in our
case, the diagnosis of Sweet’s syndrome was
considered. The ulceration had confused the
diagnosis of erysipelas with pyodermagangrenosum.
Histopathological evaluation unfortunately did
not give conclusive result. The main findings, heavy
neutrophilic infiltrates corresponding with epidermal
necrosis and stark dermal edema, suggestive of
infection, but might also support the provisional
diagnoses.(Johnston RB et al., 2012). Striking
edema and epidermal necrosis combined with
description of blister formation and subsequent
ulceration also alerted us of cutaneous anthrax
possibility. .(Johnston RB et al., 2012). Gram-
positive bacilli, however, was not found.
Blood cultures in bullous erysipelas usually
produce negative result. Culture can be performed
by bacterial swab from the blister or ulcer, even
though there are still more possibilities of negative
finding. (Krasagais KI et al., 2006). performed
culture of bullous erysipelas and find 4 out of 7
patients were sterile. We did not perform it since he
initially was diagnosed as SS and PG.
Reexamination of the patient did not confirm
history of direct contacts with domesticated animals
(i.e. goats) or their products, even though he
acknowledged some of those animals wandered
False Alarm: Cutaneous Anthrax Suspicion in a Case of Bullous Erysipelas - The Clinicopathological Consideration
279

around the neighborhood where he sometimes came
to inspect. To his knowledge, there was no similar
ailment reported from the area or by his co-workers.
Moreover, cutaneous anthrax lesion usually starts
with papule and vesicles distributed on the face or
upper extremities that rapidly breaks down to
necrotic painless ulcer with brawny edges, unlike in
our case. Antigen detection by tissue polymerase
chain reaction (PCR) is highly recommended to
perform if cutaneous anthrax is still suspected.(Titou
H et al., 2012) Suspicion of cutaneous anthrax can
also be excluded by immunohistochemistry,
although it was not available.
Finally, a favorable response toward antibacterial
monotherapy and leg compression as adjuvant
without the need to add systemic corticosteroid has
greatly supported diagnosis of bullous erysipelas.
Erysipelas in general has rapid and favorable
response to antibacterial treatment. Although many
guidelines has been established, treatment of SSTIs
including erysipelas with local complication is still
challenging because there were many variants,
degree and different etiologic agents which
associated with various pathomechanisms of
infections and clinical manifestation.(E Silvano et
al., 2016) Because SSTIs in general usually due to
Gram-positive microorganism, first line
recommended treatment are usually broad spectrum
antibiotics with more susceptibility towards Gram-
positive bacteria, such as β-lactams, cephalosporin
and clindamycin.(Edwards J et al., 2006). However,
many guidelines available do not consider target
population and its geographical differences, which is
related to epidemiology of various bacterial strains
and susceptibility toward certain antibiotics.
7
Clindamycin was chosen to treat this patient due to
its broad-spectrum activity since the infection
covered deeper structures of the skin and its
underlying structures. Clindamycin and several
antibiotics have its antitoxin property that is
beneficial to reduce early release of exotoxins from
Gram-positive microorganism, since toxin
production is associated with streptococcal and
staphylococcal infections. (Montravers P et al.,
2016).Guideline for SSTIs management from
Infectious Diseases Society of America (IDSA)
recommends the use of clindamycin for mild to
moderate erysipelas and other non-purulent
SSTIs.(Stevens DL et al., 2014). Dosage option and
adjustment should be considered based on specific
clinical condition such as renal insufficiency.
4 CONCLUSION
Bullous erysipelas is a skin and soft tissue infection
characterized by blistering and is not an uncommon
entity. However, it may still be unrecognizable if the
source and mode of infection cannot be identified.
Its clinical presentation could mimic other entities,
such as Sweet’s syndrome, pyoderma gangrenosum,
and cutaneous anthrax, each with its own
characteristics (e.g. pseudo vesiculation, brawny
edges) and underlying condition that should not be
overlooked. Histopathology may at times show
findings that are indistinguishable so that correlation
with clinical information should always be sought.
REFERENCES
Cohen PR, Honigsmann H, Kurzroc R. Acute febrile
neutrophilicdermatosis (Sweet Syndrome). Goldsmith
LA, Katz SI, Gilchrest BA, Paller A, Leffell D, Wolff
K, eds. 2008. In: Fitzpatrick’s Dermatology in General
Medicine. 8th ed. New York: McGraw Hill;. p. 362-
70.
Cowell FC, Hackett BC, Wallach D.
Pyodermagangrenosum. Goldsmith LA, Katz SI,
Gilchrest BA, Paller A, Leffell D, Wolff K, 2008. eds.
In: Fitzpatrick’s Dermatology in General Medicine.
8th ed. New York: McGraw Hill;. p.371-9.
E Silvano, Bassetti M, Bonnet E, Bouza E, Chan M,
Simone GD, et al. 2016. Hot topics in the diagnosis
and management of skin and soft-tissue infections. Int
J of Antimicrob Agents.; 48(1): 19-26.
Edwards J, Green P, Haase D. 2006. A blistering disease:
bullous erysipelas. CMAJ.; 175 (3): 247.
FY Chong, T Thirumoorthy. Blistering erysipelas: not a
rare entitiy. Singapore Med J. 2008; 49(10): 809-13.
Jendoubi F, Rohde, M, Prinz JC. 2019. Intracellular
streptococcal uptake and persistence: a potential cause
of erysipelas recurrence. Front Med., 6(6): 1-15
S Vichitra, Senanayeke S. 2016. Bacterial skin and soft
tissue infections.AistPrescr.. 39: 159-63.
Krasagakis K, Samonis G,Maniatakis P, Georgala S,
Tosca A. 2006. Bullous erysipelas: clinical
presentation, staphylococcal involvement and
methicillin resistance. Dermatology.; 212(1): 31-5.
Montravers P, Snauwaert A, Welsch C. 2016. Current
guidelines and recommendations for the management
of skin and soft tissue infections. Curr Opin Infect
Dis.; 29(2): 131-8.
Stevens DL, Bisno AL, Chambers HF, Dellinger EP,
Goldstein EJC, Gorbach SL, et al. 2014. Practice
guidelines for the diagnosis and management of skin
and soft tissue infections: 2014 update by the
Infectious Diseases Society of America. Clin Infect
Dis.; 59(2): e10-52.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
280

Titou H, Ebongo C, Bouati E, Bouil M. 2017. Risk factors
associated with local complications of erysipelas: a
retrospective study of 152 cases. Pan Afr Med J.;
26(66): 1-7
Vesiculobuloous. 2012. reaction pattern.Johnston RB, ed.
In: Weedon's skin pathology essentials. 4th ed.
Elsevier.. p. 129
False Alarm: Cutaneous Anthrax Suspicion in a Case of Bullous Erysipelas - The Clinicopathological Consideration
281
