
The Profile of Diaper Dermatitis in Infants
Cana Rifiza R. S.
1
, Nelva Karmila Jusuf
2*
, Imam Budi Putra
2
, Tri Widyawati
3
,
Nurfida Khairina Arrasyid
4
1
Master Program of Tropical Medicine, Faculty of Medicine, Universitas Sumatera Utara,
2
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Sumatera Utara
3
Department of Pharmacology, Faculty of Medicine, Universitas Sumatera Utara
4
Department of Parasitology, Faculty of Medicine, Universitas Sumatera Utara
Jl. Dr. Mansur No. 5 Medan 20155, Indonesia
*Corresponding author
Keywords: Diaper Dermatitis, Infant
Abstract: Diaper dermatitis is a common condition in infants. The present study aims to describe the profile of diaper
dermatitis in infants. A cross-sectional study was conducted between August and December 2018 in several
hospitals, community health centers and integrated health service in Medan, Indonesia. Age, gender, birth
order, a term or preterm delivery history, feeding history, diaper type used, frequency of diaper changing
and defecation, cleansing agents, diaper cream used, location of rash and skin scraping examination with
10% potassium hydroxide preparation were identified. There were forty infants with diaper dermatitis
included in the study. Of those, 24 infants (60%) were aged 0-6 months, 21 infants (52.5%) were male, and
25 (62.5%) infants were first child. Further, 38 infants (95%) were born a term, 18 infants (45%) were fed
with formula milk, 36 infants (90%) wore disposable diaper, 23 infants (57.5%) had diaper changed <6
times a day, 30 infants (70%) defecated <3 times a day, 17 infants (42.5%) were cleaned with wet wipes,
and 25 infants (62.5%) did not use any diaper cream. Eleven infants (27.5%) had a rash in the inguinal area.
Skin scraping examination with 10% potassium hydroxide preparation showed positive results in 11 patients
(27.5%).
1 INTRODUCTION
Diaper dermatitis is an eruption in the area covered
by the diaper, characterized by erythema, scales, red
plaque, or erosions of skin. It is commonly known as
diaper rash. The covered area includes the lower
abdomen, genital organs, waists, inner thighs,
buttocks and perianal (Stamatas and Tierney, 2014;
Mohamadi et al., 2014).
There are several causes of diaper dermatitis, i.e.
skin friction and irritation, urine and feces, increase
in skin moist and pH, and zinc deficiency (Coughlin
et al., 2014; Blume-peytavi et al., 2014). The three
most common types of diaper dermatitis are chafing
dermatitis, irritant contact dermatitis, and diaper
candidiasis. The prevalence of diaper dermatitis in
general population is 7-35% while among
hospitalized infants and children is 17-43% (Merrill,
2015). The prevalence among countries varied
between 15-84% (Hurdoyal and Pandamikum, 2015;
Li et al., 2012). The incidence of diaper dermatitis is
common in infants aged 3-12 weeks and the peak is
in infants aged 9-12 months. The rate seems to be
similar across male and female (Alonso et al., 2013;
Yaduwanshi and Kumari, 2012).
Infant skin is anatomically and physiologically
different from adults. Although healthy and term
neonates seem to have well-developed skin, the
function of the epidermis is not complete yet (Adam,
2008; Merill, 2015). The epidermis layer of the
infant is characterized by thin stratum corneum and
thin collagen fibers in the dermis layer. A recent
study showed that aterm neonates skin is not
competent and still continues to complete the
maturation process in the first year of life (Agustinus
et al., 2017; Merill, 2015). The epidermis layer as a
skin barrier is not complete yet to prevent water loss
and penetration irritants from the environment.
Further, the infant has a greater tendency to develop
dermatitis. Preterm infant skin has an immature
stratum corneum thus more risky to have an
44
R. S., C., Jusuf, N., Putra, I., Widyawati, T. and Arrasyid, N.
The Profile of Diaper Dermatitis in Infants.
DOI: 10.5220/0009855800440051
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 44-51
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

infection (Agustinus et al., 2017; Atherton et al.,
2016).
Diaper dermatitis can be diagnosed by complete
history taking including the duration, symptoms, risk
factors and appearance of the eruption (Lawton,
2014; Shin, 2014). There are several factors
associated with diaper dermatitis in infants,
including frequency of urination and defecation,
frequency of diaper changes, type of diaper, type of
cleanser, product applied to skin, diet, diarrhea,
recent antibiotic used and any previous diaper
dermatitis (Merill, 2015; Lawton, 2014; Shin, 2014;
Li et al., 2012). Frequent urination and defecation on
covered skin will increase skin pH. Production of
frequent liquid feces means the enzyme is greater
and can act as irritants along with urease enzyme
from the urine. Frequency of urination in neonates is
more than twenty times in 24 hours and will reduce
to around seven times at 12 months of age.
Therefore, frequent diaper changes are important to
do for at least every 3-4 hour (Li et al., 2012).
Improvement of diaper technology associated with
the decrease of the severity of diaper dermatitis. The
absorbent gel makes it possible for a disposable
diaper to keep skin to be dry and maintain the
normal moisture. Cleanser used to cleanse out the
rain and feces is also important because it will
remove the lipid and feces residue from the stratum
corneum (Atherton, 2004; Odio and Thaman, 2014).
The use of barrier cream every diaper change aim to
reduce friction, wetting and contact with urine and
feces. The ideal barrier cream will provide a
longlasting lipid shield which protects the skin from
irritants. (Atherton, 2004; Merill, 2015).
Treatment of diaper dermatitis varies depending
on the severity and etiology. Current practice
including the most recent guideline on neonatal skin
care from the Association of Women's Health,
Obstetric and Neonatal Nurses (AWHONN, 2013)
recommends five approaches for prevention and
treatment of diaper dermatitis. The approaches are
nonpharmacologic solutions easily summarizes into
the "ABCDE" that include air, barrier, cleansing,
diapering, and education. The first is to expose the
diaper area frequently to air as much as possible.
Apply barrier cream to skin for infants at risk of
diaper dermatitis or whenever diaper dermatitis is
present. The skin should be cleansed gently with
water and soft cloth or wipes at every diaper change.
Use of superabsorbent diaper is recommended and
the diaper should be changed as soon as the diaper is
soiled at least every 3 hours during the day and once
during the night. Parents must be educated for diaper
hygiene and good skin practices (Merill, 2015;
Pogacar et al., 2018; Serdaroglu and Ustunbas,
2010).
Diaper dermatitis can improve in a couple of
days with good skin practices. A skin infection may
develop if diaper dermatitis is not managed well.
One of the most common infection occurred is
caused by fungal. Candida is fungal that often
infects skin with diaper dermatitis. When it is
suspected, the skin scraping examination with 10%
potassium hydroxide can be done to identify the
fungal structure such as hyphae, pseudohyphae or
spore (Bonifaz et al., 2016). If it is confirmed,
topical antifungal can be given as the choice for
treatment for diaper dermatitis.
Several studies in Indonesia has been conducted
to evaluate parents knowledge about diaper
dermatitis (Ullya et al., 2018; Kusumastuti and
Alfiyanti, 2017; Jahidin, 2015) however studies on
the profile of diaper dermatitis in infants and skin
scraping examination with 10% potassium
hydroxide to find fungal infection are still limited.
The aim of this study is to describe the profile of
diaper dermatitis in infants at health service centers
in Medan, Indonesia. The health service centers
included in this study are the hospital, community
health center (known as Puskesmas) and integrated
health service center (known as Posyandu).
2 METHODS
This cross-sectional study was conducted between
August and December 2018 at one General Hospital,
one Hospital Women and Children, two community
health centers and integrated health service centers
(Posyandu in the two Puskesmas area) in Medan,
Indonesia. Subjects were infants who were inpatient
at the two hospitals, and infants who were attending
the two Puskesmas and Posyandu. Inclusion criteria
included infants aged 0-24 months, wore a diaper
and had diaper dermatitis at the time of the study.
Exclusion criteria included infants who used the
antifungal topical cream on skin covered by the
diaper and had oral antibiotics at the time of the
study. Forty patients who were fulfilled the selection
criteria participated in the study.
Parents or guardians were given written informed
consent before enrolment of the children to the
study. The required information was being asked to
the parents or guardians and then the diaper rash was
observed carefully. Skin scrapping was collected
with a sterile pot and analyzed at the clinical
microbiology laboratory in the General Hospital.
Samples were labeled with name, age, and gender.
The Profile of Diaper Dermatitis in Infants
45
Skin scraping sample was prepared with 10%
potassium hydroxide preparation and examined
under a microscope. Microscopic findings were used
to identify the presence of fungi, i.e. hyphae, and
spore they were confirmed as a positive result.
Data processing using Statistical Package for the
Social Science (SPSS) version 22.0 was presented
descriptively to see the percentage of profile diaper
dermatitis in infants in the present study.
The protocol of this study has been approved by
the Ethics Committee of Faculty of Medicine,
Universitas Sumatera Utara with ethical clearance
No: 446/TGL/KEPK FK USU-RSUP HAM/2018.
3 RESULTS
A total of 40 patients were included in this study. Of
those, 13 patients were enrolled at the General
Hospital (8 male, 5 female), 6 patients were at
Women and Children’s Hospital (3 male, 3 female),
2 patients were at the Puskesmas (2 male), and 19
were at the Posyandu (8 male, 11 female).
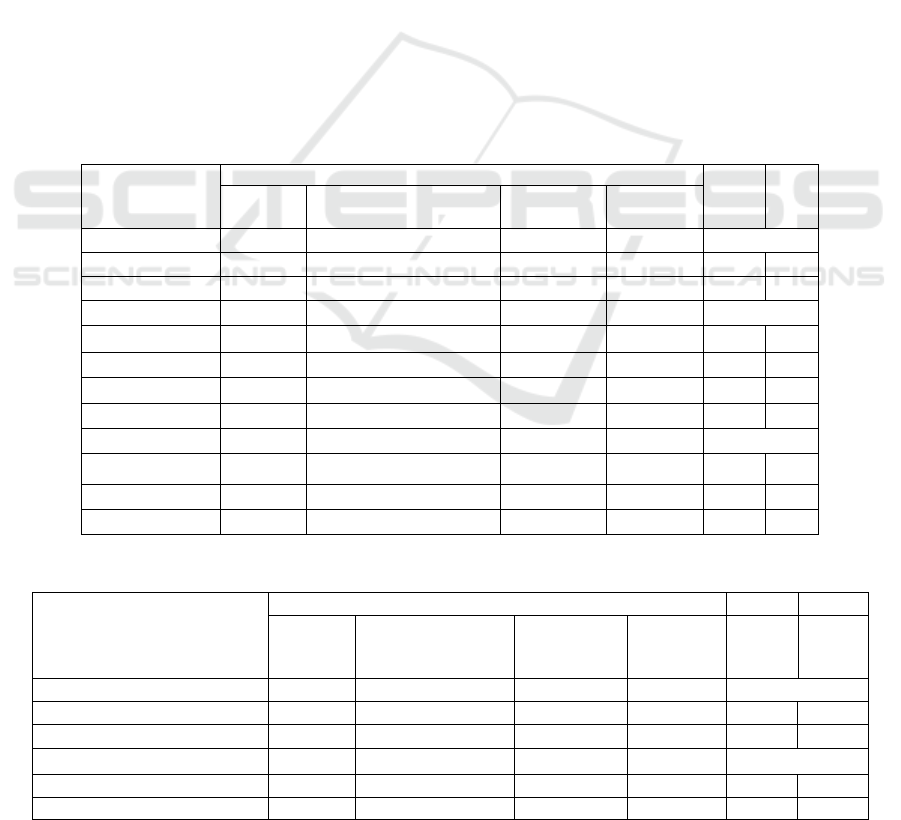
Demographic characteristics are described in
Table 1. Infants aged 0-6 months was the most
prevalent of all age groups (n=24, 60%), and the
male was found to be more common (n=21, 52.5%).
Of those, most were first child (n=25, 62.5%).
Table 2 showed the profile of diaper dermatitis in
infants as follows: born at full-term (n=38, 95.0%),
infants fed with formula milk (n=18, 45.0%), worn
disposable diaper (n=36, 90%), frequency of diaper
change <6 times a day (n=23, 57.5%), frequency of
defecation <3 times a day (n=30, 75.0%), cleansed
using wet wipes (n=17, 42.5%) and did not use a
diaper cream (n=25, 62,5%).
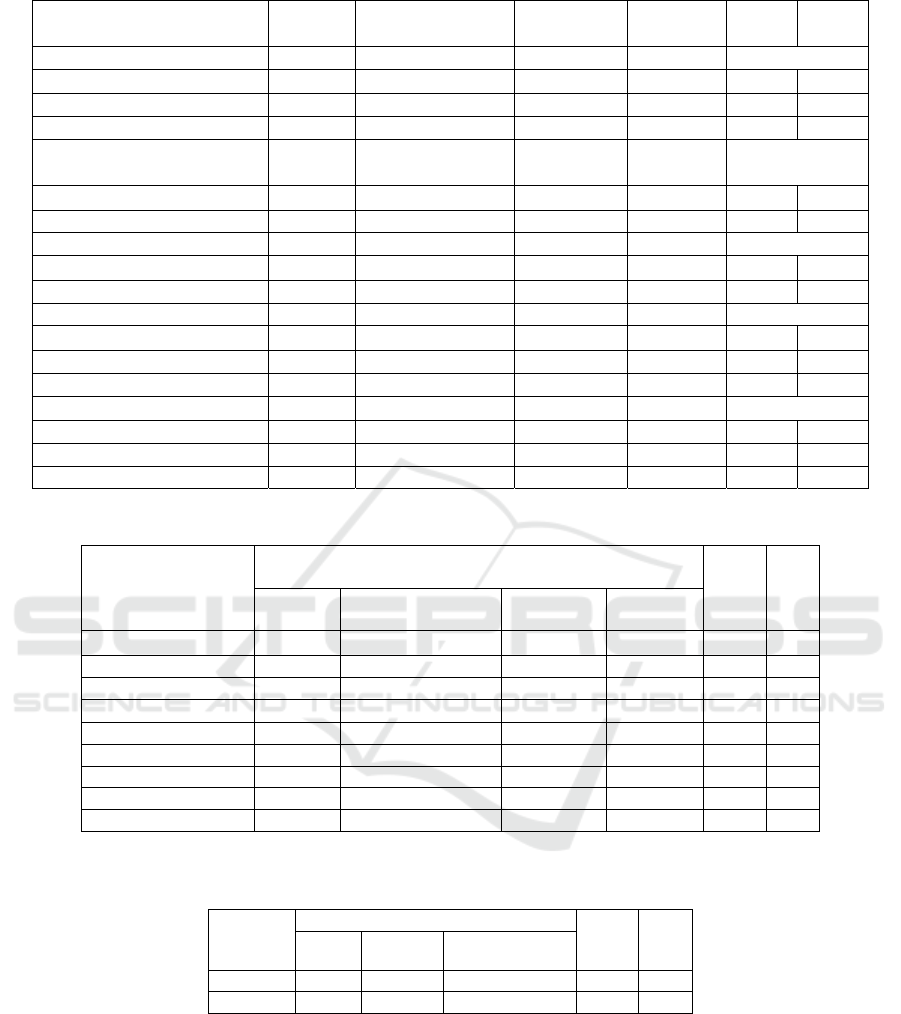
On rash examination, we found that the most
common location of the rash was inguinal area
(n=11, 27.5%), as shown in Table 3.
Skin scraping examination with 10% potassium
hydroxide showed positive result only in 27.5% of
infants (n=11). The assay also found hyphae in 2
samples, pseudohyphae in 9 samples. And there was
no spore identified (Table 4).
Table 1: Demographic Characteristic of Infants
Characteristics
Place of Study
Total %
General
Hospital
Women
and Children Hospital
Puskesmas Posyandu
Gender
Male 8 3 2 8 21 52.5
Female 5 3 0 11 19 47.5
Age (month)
0-6 7 6 1 10 24 60.0
7-13 6 0 1 7 14 35.0
14-20 0 0 0 1 1 2.5
21-24 0 0 0 1 1 2.5
Birth Order
1
st
6 5 0 14 25 62.5
2
n
d
6 1 0 2 9 22.5
≥ 3
r
d
1 0 2 3 6 15.0
Table 2: Profile of Diaper Dermatitis in Infants
Profile
Place of Study Total (%)
General
Hospital
Women
and Children
Hospital
Puskesmas
Posyandu
Delivery history
A term 11 6 2 19 38 95.0
Preterm 2 0 0 0 2 5.0
Feeding history
Breastfeeding 3 2 1 11 17 42.5
Formula milk 7 3 1 7 18 45.0
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
46
Breastfeeding and
formula milk
3 1 0 1 5 12.5
Type of Diaper
Cloth diaper 0 0 0 3 3 8.3
Disposable diaper 13 6 1 16 36 90.0
Modern cloth diaper 0 0 1 0 1 1,7
Frequency of diaper
changing
<6 times/day 5 3 1 14 23 57.5
≥6 times/day 8 3 1 5 17 2.5
Frequency of defecation
<3 times/day 8 4 0 18 30 75.0
≥3 times/day 5 2 2 1 10 25.0
Cleansing agents
Water only 4 2 0 7 13 32.5
Water and soap 2 1 1 6 10
Wet wipes 7 3 1 6 17 42.5
Diaper cream
Never 7 6 0 12 25 62.5
Always 1 0 0 1 2 5.0
Sometimes 5 0 2 6 13 32.5
Table 3: Location of Diaper Dermatitis Rash
Location
of Rash
Place of Study
Total %
General
Hospital
Women and
Children Hospital
Puskesmas Posyandu
Genitalia 0 0 0 4 4 10.0
Pubic 1 0 0 2 3 7.5
Inguinal (R/L) 5 1 1 4 11 27.5
Femoral (R/L) 0 0 0 1 1 2.5
Perineum 1 0 0 0 1 2.5
Perianal 3 2 1 4 10 25.0
Gluteal 2 3 0 2 7 17.5
Genitalia and public 1 0 0 2 3 7.5
Inguinal and femoral 0 0 0 0 0 0
R=right, L=left
Table 4: Skin Scrapping Examination with 10% potassium hydroxide
Result
Microscopic Finding
Total %
Spore Hyphae Pseudohyphae
Positive 0 2 9 11 27.5
Negative 0 0 29 29 72.5
4 DISCUSSION
This study described the diaper dermatitis profile in
infants attending the General Hospital, Women and
Children’s Hospital, Puskesmas and Posyandu in
Medan, Indonesia. In the present study, subjects
with diaper dermatitis were aged between 0-24
months. Infants aged between 0 and 6 months was
the most prevalent among other age groups. The
prevalence of diaper dermatitis was likely to
decrease correspondingly with the increase of
infant's age. This condition is associated with the
incompetent stratum corneum of the neonates. A
recent study has shown that full maturation of
stratum corneum might not be complete until one
The Profile of Diaper Dermatitis in Infants
47

year of age (Nikolovski et al., 2008). It has also been
associated with the skin pH of the neonates. At birth,
the pH has been reported to be around 7.80, which is
higher than 5.7 measured in adults. However, the
level of Ph declines after several weeks of life
(Yosipovitch et al., 2000; Horowitz et al., 2013;
Fluhr et al., 2012). The development of stratum
corneum and the decline of skin pH to be more
acidic are important as the barrier function and as an
antimicrobial defense of the skin. Therefore,
younger infants are more prone to be at risk for
dermatitis. Nevertheless, some other studies have
described that diaper dermatitis was frequently
found among infants aged 6 to 12 months which
might be associated with feeding (Hurdoyal and
Pandamikum, 2015; Yaduwanshi and Kumari,
2012). Li et al., (2012) reported the incidence of
diaper dermatitis tends to increase along with the
increase of age and the peak was infants aged 19-24
months. Adalat et al., (2007) found infants aged 12-
24 months aged to be the most prevalent followed by
aged 6-12 months. Infants aged higher than six
months has given solid foods diet, causing the
adaptation process of the digestive tract and also the
change of digestive enzyme (Hurdoyal and
Pandamikum, 2015; Yaduwanshi and Kumari,
2012).
Diaper dermatitis is a common condition found
in infants and children. The prevalence and
incidence varied among countries around the world.
It is associated with many risk factors such as type
of diaper, duration of diaper use, skin hygiene
practice, and different childcare practices (Andrini,
2016; Merrill, 2012).
In this study, male infants were more common.
Several previous studies reported the same results
(Hurdoyal and Pandamikum, 2015; Frilasari, 2016;
Mohamadi et al., 2014). Other studies stated that
gender is not significantly different compared to the
control subjects (Li et al., 2012; Elfaituri et al.,
2016). But in contrast to those studies,
Yaduwanshi and Kumari (2012) and Blanco and van
Rossem (2013) reported female subjects are greater
in infant's diaper dermatitis.
In the present study, we found that most infants
are the first child in the family. This might be due to
the lack of experience and knowledge of baby care.
New parents often follow the method of babysitting
by the grandparents, but some of them do not look
for information online or ask experienced friends.
This often happens because most working parents
entrust the baby to the grandparents when they are at
work. However, this theory still needs to be studied
to prove the relationship.
We also found that infants born at a term
gestational pregnancy age to be more common. This
is in accordance with a previous study stating that
healthy, a term neonate's skin does not completely
mature to function as a barrier toward irritants and
infections (Adam, 2008; Merill, 2015; Agustinus et
al., 2017). Infants who were fed with formula milk
also had more diaper dermatitis in this study. It has
been reported that breastfed children have a lower
prevalence of diaper dermatitis because their feces
have a higher pH, lower digestive enzyme activity
and less urease-producing bacteria than formula
milk-fed children (Yoshioka et al., 1983).
Further, infants with a disposable diaper with
diaper changes <6 times a day had more diaper
dermatitis in this study. Li et al., (2012) reported the
same findings. This is due to the skin covered by
diaper get more moisture and humidity which can
lead to maceration. Thus, frequent diaper changes
are good to maintain skin dryness.
In the present study, most infants did not have
diarrhea at the time of the study. Diarrhea may be an
important risk factor to develop diaper dermatitis.
Frequent exposure to liquid feces is associated with
greater amounts of an enzyme which pass with the
feces (Atherton, 2001).
Wet wipes have been used widely as an
alternative to cleansing the skin. In this study,
parents or guardians had already worn wet wipes as
an alternative to water and soap. The use of wet
wipes consider to be better in reducing the
occurrence of diaper dermatitis is infants
(Ehretsmann et al., 2001). Diaper creams may also
provide a protective lipid film that prevents exposure
to irritants (Stamatas and Tierney, 2014). Diaper
cream should be applied at every diaper change for
infants at risk of developing diaper dermatitis and
whenever diaper dermatitis is present (Atherton,
2016; Noonan et al., 2006). In this study, parents did
not yet use any diaper cream because of the lack of
information on the function of diaper cream as a
protector for infant skin.
The location of diaper dermatitis rash was found
greater in the inguinal area, followed by the perianal
area. Andrini (2016) also reported that inguinal to be
the most affected area in diaper dermatitis subjects.
The rash in covered diaper skin often appears in the
area which contacts with diaper and gets more
friction. The skin folds and convex area of gluteal
are also frequently affected because of the high
humidity (Adam, 2008; Alonso et al., 2013).
Most infants with diaper dermatitis were found at
the Posyandu in this present study. Posyandu is a
place which health activities organized from, by and
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
48

for communities assisted by health workers from
Puskesmas. It primarily starts to serve not only
babies and toddlers but also the elderly. Baby health
services specifically in weighing and immunization
is common, but baby caring is not done routinely.
Skin scraping examination is easy, cheap and can
be done immediately. The examination is important
to identify fungal infection, thus clinicians can
choose the appropriate treatment for diaper
dermatitis. The sensitivity of this test is about 60%,
thus the possibility to detect fungal infection is still
high (Mutiawati, 2016; Sari et al., 2013). The
percentage of skin scrapping examination with 10%
potassium hydroxide preparation in this study is
different from the previous study. Blanco and van
Rossem (2013) has shown that the positivity of
diaper dermatitis in infants was 59%. The role of
fungal infection in diaper dermatitis has been studied
in other studies. The most common fungal infection
associated with diaper dermatitis is Candida,
especially Candida albicans, which has been
reported in more than 80% of cases (Klunk et al.,
2014; Ferrazini et al., 2003). Normally the number
of Candida in the diaper area without dermatitis is
low and yeasts are isolated in <4% of cases, while
they are present between 70 and 92% of children
with diaper dermatitis (Adalat et al., 2007; Adam,
2008).
There are a few limitations in this study. First,
the numbers of samples enrolled in this study was
relatively small. Second, there is no control subjects
participated in this study. However, this study
showed that diaper dermatitis is a common problem
during infancy and fungal infection is still common
to present as a secondary infection. The further
comprehensive study is needed to be done.
5 CONCLUSION
1. The proportion of diaper dermatitis in this study
was greater among infants aged 0-6 months, the
male was found to be the most common
compared to female, and the first child was also
commonly found.
2. The present study showed that most infants with
diaper dermatitis were born a term, fed with
formula milk, wore a disposable diaper, had a
diaper changed <6 times a day, defecated <3
times a day, cleansed with wet wipes and did
not use any diaper cream.
3. The location of rash in the diaper dermatitis
varied in this study. Inguinal was the most
affected area, followed by the perianal area.
4. The percentage of fungal infection in the diaper
dermatitis in this study was 27.5% as confirmed
by a skin scraping examination with 10%
potassium hydroxide preparation.
6 SUGGESTION
1. Special care for infants with diaper dermatitis in
the hospital needs to be done carefully by
doctors and nurses in the pediatric room.
2. Joint care of pediatrician and dermatologist for
the prevention and treatment of infants with
diaper dermatitis in hospital needs to be done
continuously (integrated care).
3. Health workers in Puskesmas and Posyandu
need to be trained about the good skin care
practice for infants so that they can educate the
parents.
4. Fungal culture examination as the gold standard
can be done in further study to explain the role
of fungal as the cause of diaper dermatitis.
REFERENCES
Adalat, S., Wall, D. and Goodyear, H. 2007. Diaper
dermatitis-frequency and contributory factors in
hospital attending children. Pediatric Dermatology;
24: 483–8.
Adam, R. 2008. Skin Care of the Diaper Area. Pediatric
Dermatology; 25: 427-433. DOI: 10.1111/j.1525-
1470.2008.00725.x.
Agustinus, O. P., Wignjosoesastro, C. and Angeline, D.
2017. Formulasi Topikal untuk Manajemen Dermatitis
Popok pada Bayi. Continuing Professional
Development; 44: 184-187.
Alonso, C., Larburu, I., Bon, E., González, M. M.,
Iglesias, M. T. and Urreta, I. 2013. Efficacy of
petrolatum jelly for the prevention of diaper rash: A
randomized clinical trial. Journal for Specialists in
Pediatric Nursing; 18: 123-132. DOI:
10.1111/jspn.12022.
Andrini, N. 2016. Karakteristik Dermatitis Popok pada
bayi di RSUP Haji Adam Malik Medan pada tahun
2014. Repositori Institusi Universitas Sumatera Utara.
http://repository.usu.ac.id/handle/123456789/57870
Atherton, D. J. 2001. The Etiology and Management of
Irritant Diaper Dermatitis. J Eur Acad Dermatol
Venereol; 15(suppl. 1): 1-4.
Atherton, D. J. 2004. A Review of The Pathophysiology,
Prevention And Treatment of Irritant Diaper
Dermatitis. Current Medical Research and Opinion;
20: 645-649. DOI:10.1185/030079904125003575.
The Profile of Diaper Dermatitis in Infants
49

Atherton, D. J. 2016. Understanding irritant napkin
ermatitis. International Journal of Dermatology; 55:
7-9.
Association of Women’s Health, Obstetric and Neonatal
Nurses (AWHONN). 2013. Neonatal skin care
evidence-based clinical practice guideline (3rd Ed).
Washington, DC: Author.
Blume-Peytavi, U., Hauser, M., Lunnemann, L.,
Stamatas, G. N., Kottner, J. and Bartels, N. G. 2014.
Prevention of Diaper Dermatitis in Infants—a
Literatur Review. Pediatric Dermatology; 31: 413-
429. DOI: 10.1111/pde.12348.
Bonifaz, A., Rojas, R., Tirado-Sa´nchez, A., Cha´vez-
Lo´pez, D., Mena, C., Caldero´n, L., et al. 2016.
Superficial Mycoses Associated with Diaper
Dermatitis. Mycophatologia, 671-679.
Coughlin, C. C., Eichenfield, L. F. and Frieden, I. J. 2014.
Diaper Dermatitis: Clinical Characteristics and
Differential Diagnosis. Pediatric Dermatology; 31:
19-24. DOI: 10.1111/pde.12500.
Blanco, D. and van Rossem, K. 2013. A Prospective Two-
Year Assessment of Miconazole Resistance in
Candida Spp. with Repeated Treatment with 0,25 %
Miconazole Nitrate Ointment in Neonates and Infants
with Moderate to Severe Diaper Dermatitis
Complicated by Cutaneous Candidiasis. Pediatric
Dermatology; 30: 717–724. DOI: 10.1111/pde.12107.
Ehretsmann, C., Schaefer, P. and Adam, R. 2001.
Cutaneous tolerance of baby wipes by infants with
atopic dermatitis, and comparison of the mildness of
baby wipe and water in infant skin. J Eur Acad
Dermatol Venereol; 15(suppl. 1): 16-21.
Ferrazzini, G., Kaiser, R.R., Hirsig-Cheng, S.K., Wehrli,
M., Della Casa, V., Pohlig, G., Gonser, S., Graf, F.
and Jorg, W. 2003. Microbiological Aspects of Diaper
Dermatitis. Dermatology; 206: 136–41.
Frilasari, H. 2016. Derajat Diaper Rash Pada Bayi Usia 0-
12 Bulan Di RSUD Wahidin Sudiro
Husodo Kota Mojokerto. Surya, 16-20
Fluhr, J. W., Darlenski, R., Lachmann, N., Baudouin, C.,
Msika, P., De Belilovsky, C. and Hachem, J. P. 2012.
Infant epidermal skin physiology: Adaptation at birth.
British Journal of Dermatology;166 (3), 483-490.
DOI:10.1111/j.1365-2133.2011.10659.x
Hurdoyal, B. and Pandamikum, L. 2015.A Study to
Investigate the Prevalence of Nappy Rash Among
Babies aged 0-36 Months Old in A tropical Country.
Austin Journal of Dermatology; 2(2), 1-3.
Horowitz, P., McLeod, R. P., Eichenield, L. F., Fowler, J.
F., Jr. and Elias, P. M. 2013. Skin-cleansing and care
principles for special pediatric populations. Seminars
in Cutaneous, Medicine, and Surgery; 32(2 Suppl. 2):
30-32.
Jahidin, A. 2015. Hubungan Pengetahuan Dengan Sikap
Ibu Balita Terhadap Kejadian Dermatitis di Wilayah
Kerja Puskesmas Campalagian Kabupaten Polewali
Mandar. Jurnal Kesehatan Bina Generasi. http://
ejurnal.biges.ac.id/index.php/kesehatan/article/view/13
Klunk, C., Domingues, E. and Wiss, K. 2014. An Update
on Diaper Dermatitis.
Clin Dermatol; 32: 477-87.
Kusumastuti, M. J. and Alfiyanti, D. 2017. Peningkatan
Pengetahuan Ibu Tentang Diaper Dermatitis Dengan
Program Penyuluhan Kesehatan di Posyandu Melati
Desa Brumbung. Sekolah Tinggi Ilmu Kesehatan
Telogorejo. http://ejournal.stikestelogorejo.ac.id/
index.php/ilmukeperawatan/article/view/603
Lawton, S. 2014. Nappy rash: Diagnosis and treatment.
Journal of Family Health Care, 36-40.
Li, C., Zhu, Z. and Dai, Y. 2012.Diaper Dermatitis: A
Risk Factor for children aged 1-24 Months in China.
The Journal of International Medical Research; 40:
1752-1760.
Merrill, L. 2015. Prevention, Treatment, and Parent
Education for Diaper Dermatitis.Continuing Nursing
Education, 325-337. DOI: 10.1111/1751-486X.12218.
Mohamadi, J., Motaghi, M., Panahi, J., Havasian, M.R.,
Delpisheh, A., Azizian, M., et al. 2014. Anti-fungal
resistance in candida isolated from oral and diaper rash
candidiasis in neonates. Bioinformation; 10:667-670.
Mutiawati, V. K. 2016. Pemeriksaan Mikrobiologi Pada
Candida Albicans. Jurnal KedokteranSyiah Kuala, 53-
63.
Nikolovski, J., Stamatas, G. N., Kollias, N. and Wiegand,
B. C. 2008. Barrier function and water-holding and
transport properties of infant stratum corneum are
different from adult and continue to develop through
the first year of life. Journal of Investigative
Dermatology; 128(7): 1728-1736.
DOI:10.1038/sj.jid.5701239.
Noonan, C., Quigley, S. and Curley, M. A. 2006. Skin
integrity in hospitalized infants and children: A
prevalence survey. Journal of Pediatric Nursing;
21(6): 445-453. DOI:10.1016/j.pedn.2006.07.002.
Odio, M. and Thaman, L. 2014. Diapering, Diaper
Technology and Diaper Area Skin Health. Pediatric
Dermatology, 9-14.
Pogacar, M. S., Maver, U., Varda, N. M. and Micetic-
Turk, D. 2018. Diagnosis and Management of diaper
dermatitis in infants with emphasis on skin microbiota
in the diaper area. International Journal of
Dermatology; 55: 265-275.
Sari, K., Thaha, A., Soenarto and Tjekyan, R. M. 2013.
Nilai Diagnostik Rapid yeast Test Untuk Diagnosis
Kandidiasis Vulvovaginal Pada Wanita Pekerja Seks
Komersial di Klinik Graha Sriwijaya Palembang.
Majalah Kedokteran Sriwijaya, 1-4.
Serdaroğlu, S. and Üstünbaş, T. K. 2010. Diaper
Dermatitis(Napkin Dermatitis, Nappy Rash). Journal
of the Turkish Academy of Dermatology; 4: 1-4.
Shin, H. T. 2014. Diagnosis and Management of Diaper
Pediatr Clin N Am; 61: 367-382.
http://dx.doi.org/10.1016/j.pcl.2013.11.009.
Stamatas, G. N. and Tierney, N. K. 2014. Diaper
Dermatitis: Etiology, Manifestations, Prevention, and
Management.
Pediatric Dermatology; 31:1-7. DOI:
10.1111/pde.12245.
Ullya, U., Widyawati, W. and Armalina, D. 2018.
Hubungan Antara Pengetahuan dan Perilaku Ibu dalam
Pemakaian Disposable Diapers Pada Bayi dan Batita
dengan Kejadian Ruam Popok. Diponegoro University
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
50

Institutional Repository. http://eprints.undip.ac.id/
61945/
Yaduwanshi, D. and Kumari, C. 2012. Frequency and
Prevalence of Nappy Rash in Indian Infant’s
Population. International Journal of
Pharmaceutical Erudition, 25-32.
Yoshioka, H; Iseki, K. and Fujita K. 1983. Development
and Differences of Intestinal Flora in the Neonatal The
period in Breast-Fed and Bottle-Fed Infants.
Pediatrics; 72: 317-321.
Yosipovitch, G., Maayan-Metzger, A., Merlob, P. and
Sirota, L. 2000. Skin barrier properties in different
body areas in neonates. Pediatrics; 106(1 Pt 1): 105-
108.
The Profile of Diaper Dermatitis in Infants
51
