
Dengue Hemorraghic Fever with Massive Gastrointestinal Bleeding
Ayodhia Pitaloka Pasaribu
1
, Irma Sari Nasution
3
,
Munira Ulfah
2
, Syahril Pasaribu
1
1
Departement of Child Heath, Faculty of Medicine, Universitas Sumatera Utara, Adam Malik Tersier Hospital, Medan,
Indonesia
2
Resident Pediatric, Sumatera Utara University, Medan, Sumatera Utara, Indonesia
3
Faculty of Medicine, Sumatera Utara University, Medan, Sumatera Utara, Indonesia
syahrilpasaribu@yahoo.com
Keywords: Expended dengue syndrome, fluid overload, gastrointestinal bleeding
Abstract: Dengue infection is an acute febrile disease that caused by flavivirus, known for its four serotypes. Each of
serotypes may cause varies clinical presentation. The case fatality rate of severe dengue or dengue shock
syndrome could reach 44%, however, with early detection it could reduce to less than 1 %. We reported a
case of severe dengue and expanded dengue syndrome in a 7 year old girl. Patient was referred from other
hospital and had received aggressive fluid. Patient came with breathlessness, bilateral pleural effusion, ascites
and massive gastrointestinal bleeding. From urinalysis we also found high leucocyte and bacteria. The patient
received whole blood transfusion, vitamin K injection, ceftriaxone and other supportive treatment. She was
hospitalized for 5 days and discharge with improvement.
1 INTRODUCTION
Dengue infection has a wide clinical range from
asymptomatic disease, classical dengue fever (DF),
dengue hemorrhagic fever (DHF), dengue shock
syndrome (DSS), and expanded dengue syndrome
(EDS) (WHO). In 2013, worldwide dengue infection
was estimated occurred in 390 million people,
among them 90 million were symptomatic (Bhatt,
2013).
Without proper treatment, case fatality rate
could reach up to 20% and with early detection and
intervention would reduce to <1% (WHO, 2013).
Increasing number of dengue cases with atypical
presentations are being reported as increasing
awareness of the disease (Gulati, 2007).
Herewith we report a case of severe dengue
infection with expanded dengue syndrome in a 7
year old girl.
2 CASE PRESENTATION
AR, a 7 years old girl, was referred to Adam Malik
Hospital on April 2nd 2019 with chief complaint of
shortness of breath that occurred 1 day prior
admission to hospital. History of fever was
experienced for 4 days, typical high fever that was
difficult to treat with antipyretic. There was no fever
found within these 2 days. Headache and athralgia
was found during fever. There was no nauseous or
vomiting found. Abdominal distension and pain was
found. We also found swelling of eyelids, face, and
extremities. Ptechiae was found on the extremities.
Patient was hospitalized in another hospital for 3
days and received aggressive fluid therapy of 4 liter
ringer lactate and 1 liter HES.
On physical examination, her current weight
was 21 kg, while previous body weight was 17 kg.
The patient was still alert but looked ill. Her
temperature on admission was 37.5
o
C. Blood
pressure was 100/60 mmHg, heart rate of 105 bpm,
and respiratory rate of 32 bpm. There was palpebral
and extremities edema. On the chest examination,
she had symmetrical chest expansion. The
respiratory rate was 32 bpm, regular. From
auscultation we found breath sound was decreased
on both of lung. Abdomen was distended and
ascites found. The bowel sound was normal. We
inserted naso gastric tube and blood was found
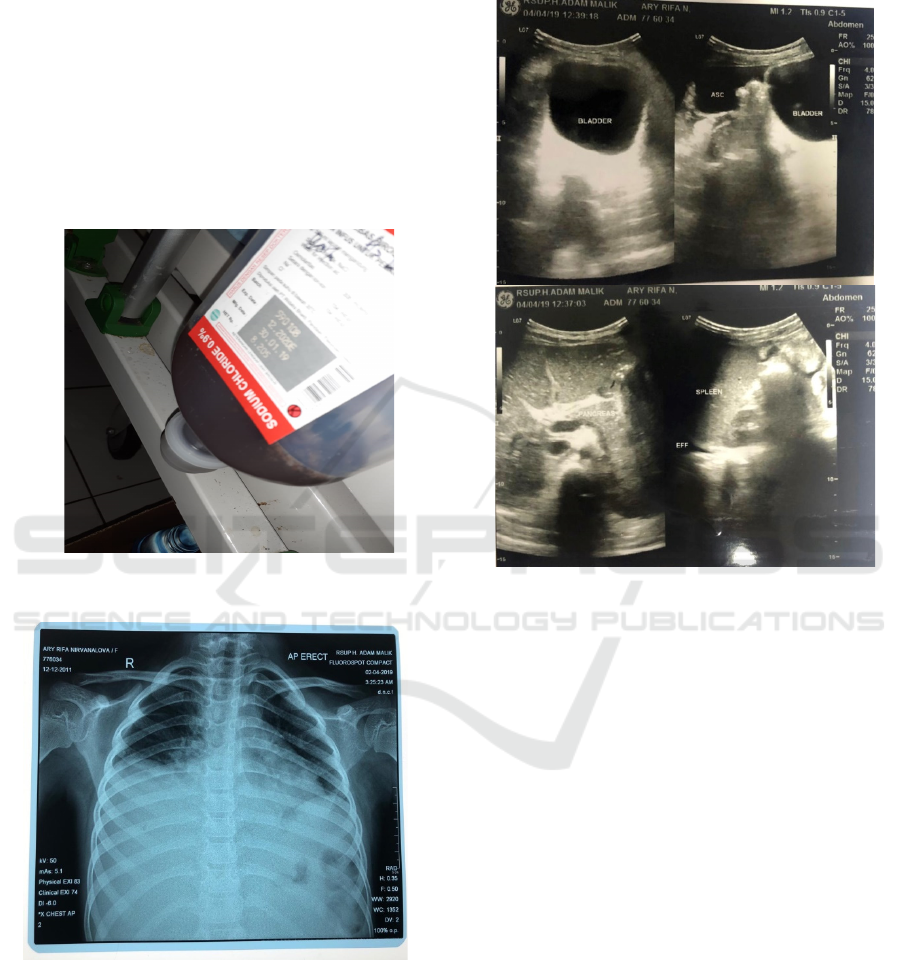
±500ml during follow up (figure 1).
From laboratory result on admission, hemoglobin
level was 13g/dl, hematocrit 38%, leukocyte 5210/
uL, platelet 16.000/uL, lymphocyte was 40.3%, and
blood glucose was 96gr/dL. Anti-dengue IgM and
30
Pasaribu, A., Nasution, I., Ulfah, M. and Pasaribu, S.
Dengue Hemorraghic Fever with Massive Gastrointestinal Bleeding.
DOI: 10.5220/0009855500300032
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 30-32
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
IgG turned out to be positive. During follow up,
hemoglobin level drop to 7.9gr/dL. We also checked
for liver function and found increase AST (102) but
normal renal function. Blood culture result turned
out sterile. We found slightly low sodium level and
increase doubled of APTT level (Table 1). From
urine examination we found leucocyte level 172 and
bacteria was 127.
From chest x-ray, we found bilateral pleural
effusion (figure 2). We did abdominal examination
in this patient and found ascites (figure 3).
We diagnosed the patient severe dengue
infection and expanded dengue syndrome.
Figure 1: Gastrointestinal bleeding
Figure 2: Chest X-ray showed bilateral pleural effusion.
Expanded syndrome that we found in this patient
was fluid overload and co-infection with urinary
tract infection. We treated the patient with
supportive treatment such as oxigenation and
maintained her airway, breathing, and circulation.
We gave ceftriaxone, ranitidine, and furosemide to
remove excessive fluid. We give 200cc whole blood
to replace the blood loss. We treated the patient for 5
days and she was discharged with improved
condition.
Figure 3: Abdominal ultrasound revealed ascites.
3 DISCUSSION
Dengue infection is a major public health problem
concern mostly affected tropical and subtropical
regions (Mandall, 2011). Majority of dengue
infection was dengue fever, but about 13.4% could
lead to severe dengue infection (Mishra, 2016).
Almost all patients that came with dengue infection
had fever or history of fever and headache (Laul,
2016 ). In our case we found similar result, the
patient complained 4 days of fever and headache.
One study found that the prevalence of severe
dengue increase in age > 11 year old (Mishra, 2016),
however in our case report the age of the patient was
younger. Previous study showed that in severe
dengue infection more than 78% of the patient
developed abnormal breath sound and plural
effusion, and more than 82% while other study
found lower number than that (Laul, 2016; Pone,
2016).
We found bilateral effusion in our case that
also showed from chest x-ray. One study also
showed that gastrointestinal bleeding was common
Dengue Hemorraghic Fever with Massive Gastrointestinal Bleeding
31

in dengue infection (Bhaskar, 2015).
In our case, the
patient has massive gastrointestinal bleeding. A
study showed ascites could be found in 34% dengue
infection patients with gastrointestinal bleeding
(Huang, 2018). This was similar to our finding, our
severe dengue patient developed ascites and proved
by ultrasound result. In another study showed
increase level of AST more than 200 in severe
dengue while other only 80 (Pone, 2016; Bhaskar,
2015). In our case, the AST level increase slightly
above 100.
More than 78% children with spontaneous
bleeding had decrease platelet count and 75%
bleeding manifestation occurred in patients with
platelet <20,000/mm
3
as reported in a study
(Chairulfatah, 2003). This was confirmed in our
case, where the platelet level was 16,000/mm
3
on
admission and patient had gastrointestinal bleeding.
Platelet transfusion could be given in dengue
infection with active bleeding and platelet count
<50,000/mm
3
(Photapregadha, 2015). In our case,
we gave transfusion with whole blood because
hemoglobin level also decreased due to active
bleeding. The mechanism of bleeding manifestation
in dengue infection is multifactorial, including
coagulation defects (Photapregadha, 2015).
This was
proved in our case which APTT level also disturbed.
Among all dengue infection, about 4.3% cases will
develop to expanded dengue syndrome with
different manifestations (Laul, 2016).
Our report
found fluid overload and urinary tract infection as
co-infection as manifestation of expanded dengue
syndrome.
4 CONCLUSION
We have treated a 7 year old girl who came with
history of fever for 4 days, bilateral pleural effusion,
ascites, massive gastrointestinal bleeding, severe
thrombocytopenia, and co-infection with urinary
tract infection. She was diagnosed with severe
dengue infection with expanded dengue syndrome.
The patient was hospitalized for 5 days and was
discharged with great improvement.
REFERENCES
WHO, “Comprehensive guidelines for prevention and
control of dengue and dengue hemorrhagic fever”,
World Health Organization, Regional Office for
South-East Asia,
http://apps.searo.who.int/pds_docs/B4751.pdf?ua=1
Bhatt S., Gething P.W., Brady O.J., et al. The global
distribution and burden of dengue.
Nature.2013;496:504-7.
Dengue hemorrhagic fever: Diagnosis, treatment,
prevention and control. II ed. Geneva: World Health
Organization 2011.
Gulati S., Maheshwari A., 2007. “ Atypical manifestations
of dengue,” Tropical Medicine and International
Health, vol 12,no.9,pp.1087-1095.
Mandal S.K., Ganguly J., Sil K., et al., 2013. Clinical
profiles of dengue fever in a teaching hospital of
eastern Indian, ”National Journal of Medical
Research,vol.3, no.2,pp.173-176.
Mishra S., Ramanathan R., Agarwalla S., 2016. Scientica.
http://dx.doi.org/10.1155/2016/6391594
Laul A., Laul P., Merugumala V., et al. Clinical profile of
dengue infection during outbreak in Northern India. J
Trop Med 2016.
http://dx.doi.org/10.1155/2016/5917934
Pone S., Hokerberg Y., Oliveira R., et al. Clinical and
laboratory signs associated to serious dengue disease
in hospitalized children. J Pediatr (Rio J)
2016;92(5):464-471
Bhaskar E., Sowmya G., Moorthy S., Sundar V.,
Prevalence, patterns, and factors associated with
bleeding tendencies in dengue. J Infect Dev Ctries
2015;9(1):105-110.
Huang W., Lee I., Chen Y., Tsai C., Liu J., Characteristics
and predictors for gastrointestinal hemorrhage among
adult patients with dengue virus infection:
emphasizing the impact of existing comorbid
disease(s). PLos One 2018;13(2):e0192919
Chairulfatah A., Setiabudi D., Agoes R., Colebunders R.,
Trombocytopenia and platelet transfusion in dengue
hemorrhagic fever and dengue shock syndrome. WHO
Dengue Bull 2003;27:141-3
Pothapregada S., Kamalakannan B., Thulasingam M.,
Role of platelet transfusion in children with bleeding
in dengue fever. J vector Borne Dis 2015;52:304-8
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
32
