
The Relationship between ADMA and Anthropometric Indicators,
Glucose, Lipid, and Inflammatory Parameters in Obese People
M. Aron Pase
1
, Dharma Lindarto
1
*, Brama Ihsan Sazli
1
1
Department of Internal Medicine, Faculty of Medicine, Universitas Sumatera Utara,
H. Adam Malik Hospital, Jalan Bunga Lau No 17, Medan 20136, Indonesia
Keywords: Asymmetrical dimethylarginine, Obesity, Cardiovascular Risk Factor.
Abstract: Asymmetric dimethylarginine (ADMA) is an endogenous inhibitor of nitric oxide production and involved
in various pathological processes, especially processes involving cardiovascular risk. The purpose of this
study was to analyze the correlation between ADMA and anthropometric, glucose, lipid, and inflammatory
parameters. The study was a cross-sectional study of 45 obese subjects at H. Adam Malik Hospital. Blood
tests were carried out after 8-10 hours of aging against cardiovascular risk parameters: anthropometry (body
weight, BMI, and WC), glucose (FPS, PPS, HbA1C, Fasting Insulin, and HOMA-IR), lipid (LDL-C, HDL-
C, TG, and sd-LDL), and inflammation (ApoB and hs-CRP) parameters. Results: Of the 45 subjects, the
average age was 41.69 ± 5.69 years old, and the average BMI was 33.09 ± 5.05 (Obesity I). ADMA was
also found to be correlated significantly with FPG, HBA1c, and TG parameters [r=-0.506, p=0.001; r=-
0.334, p=0.013, dan r = -0.315. p=0.017, respectively]. In obesity, ADMA correlated significantly with
cardiovascular risk parameters: FPG, HbA1C, and TG.
1 INTRODUCTION
Asymmetrical dimethylarginine (ADMA) is an
endogenous inhibitor of nitric oxide synthase (NO)
which appears as a risk marker for various disease
conditions including end-stage kidney failure
(Zoccali et al., 2001), liver failure (Tsikas et al.,
2003), heart failure (Kielsten et al., 2003), diabetes
(Lin et al., 2002), pre-eclampsia (Sayyidou et
al.,2003), and atherosclerotic (Boger et al., 1997). It
has been observed that ADMA is positively
correlated with NO serum concentration and body
mass index (BMI) (Borgeraas et al., 2016).
Inflammation measured by C-reactive protein
(CRP) is another strong risk marker for predicting
cardiovascular death and complications including
inflammatory diseases (Goodson et al., 2005), sepsis
(Lobo et al., 2005), lung disease (Man et al., 2006),
and coronary heart disease (Blake & Ridker, 2002).
The interaction between ADMA and CRP is a
problem of cardiovascular disease because both
ADMA and CRP factors are involved in endothelial
dysfunction in humans (Baylis, 2006).
Obesity increases the risk of morbidity due to
hypertension, dyslipidemia, T2DM, coronary heart
disease (CHD), stroke, gallbladder disease,
osteoarthritis, sleep apnea, respiratory disorders, and
certain types of cancer. Obesity is also associated
with an increased risk of all causes of death due to
cardiovascular disease (CVD) (National Institute of
Health, 1998). Obesity is caused by abnormal or
excessive fat accumulation due to metabolic
disorders (Colak et al., 2010). According to previous
research, the main determinant of obesity is insulin
resistance which is associated with endothelial
dysfunction (El Assar et al., 2016). Obesity can
trigger the activity of tumor necrosis factor in α
proinflammatory cytokine, which then inhibits the
insulin receptor substrate 1 in the insulin signaling
pathway (Peraldi et al., 1996).
Based on several studies, ADMA has a positive
correlation with cardiovascular risk factors in
prediabetes (Eliana et al., 2011), angina pectoris
(Borgeraas et al., 2016), IGT, and obesity (Huang et
al., 2018). Therefore, the aim of this study was to
investigate the correlation between ADMA and
anthropometric, glucose, lipid, and inflammatory
parameters in obesity
.
24
Pase, M., Lindarto, D. and Sazli, B.
The Relationship between ADMA and Anthropometric Indicators, Glucose, Lipid, and Inflammatory Parameters in Obese People.
DOI: 10.5220/0009848500240029
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 24-29
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

2 MATERIALS AND METHODS
The study design was a cross-sectional study by
recruiting 45 nurses (female and male) at H. Adam
Malik Hospital aged 30-55 years who met the
criteria for obesity (WHO, 2000) and signed an
informed consent form. Subjects were excluded
from the study if they had secondary illness or
obesity that could affect markers of metabolic
disorders, lipid profiles, and inflammations such as
pregnancy or lactation, acute infection, anemia,
menopause, diabetes or hypertension, cardiovascular
disease, chronic kidney disease or liver dysfunction,
smoking, consuming corticosteroids, estrogen, beta-
adrenergic receptor agonists, nitrates, or other
vasodilator agents (Kelm et al., 2002). Venous blood
samples were collected from the subjects in the
morning after 8-10 hours of fasting combined with
ethylenediaminetetraacetate (EDTA) containing
heparin, then centrifuged.
Prior to the commencement of the study, the
study protocol was reviewed and approved by the
Institutional Research Ethics Board.
2.1 Biochemical Analysis
Serum glucose levels, HDL cholesterol (HDL-C),
and triglycerides (TG) were measured by the
enzymatic colorimetric method while Apo-B and hs-
CRP levels were measured by the immunoassay
method with Hitachi Modular analyzer using the
Roche Diagnostic kit. Insulin levels were measured
by the chemiluminescence immunoassay method
using the DPC Immulite-I analyzer (Diagnostic
Products Corp, Los Angeles, CA, USA) kit.
The HbA1c values were measured using the
High-Performance Liquid Chromatography (HPLC)
method which was in accordance with the American
Diabetes Association standard (American Diabetes
Association, 2010). ADMA levels were examined
using ELISA method with a normal range of 0.4-
0.75 μmol/L (80-150 ng/mL) (Miyazaki et al.,
1999). The HOMA-IR formula = [(fasting glucose
serum (mmol / l) x fasting insulin (μU / ml) / 22,5]
was used to determine the index of insulin resistance
(Matthews et al., 1985).
2.2 Statistical Analysis
The mean and standard deviation were summarized
as descriptive statistics. The Shapiro-Wilk test was
used to determine whether a variable was normally
distributed. The parametric test was performed on
variables with normal distribution, whereas the
nonparametric test was performed on variables with
the abnormal distribution. Furthermore, the Pearson
and Spearman test were used to evaluate the
correlation between variables according to the
variable distribution. P < 0.05 was accepted as an
indication of statistical significance. SPSS for
Windows 22.0 was used for the statistical analysis.
3 RESULTS
From the 45 obese subjects who met the inclusion
criteria, the average age was 41.69 ± 5.69 years, and
the average BMI was 33.09 ± 5.05 (Obesity I).
Table 1. shows the characteristics of the research
subjects in terms of anthropometric, glucose, lipid,
inflammatory parameters in obesity, while Table 2.
shows the correlation analysis between ADMA and
the subject parameters. There was a significant
correlation between the levels of ADMA and fasting
blood glucose (FBG), HbA1c, and TG.
The Relationship between ADMA and Anthropometric Indicators, Glucose, Lipid, and Inflammatory Parameters in Obese People
25
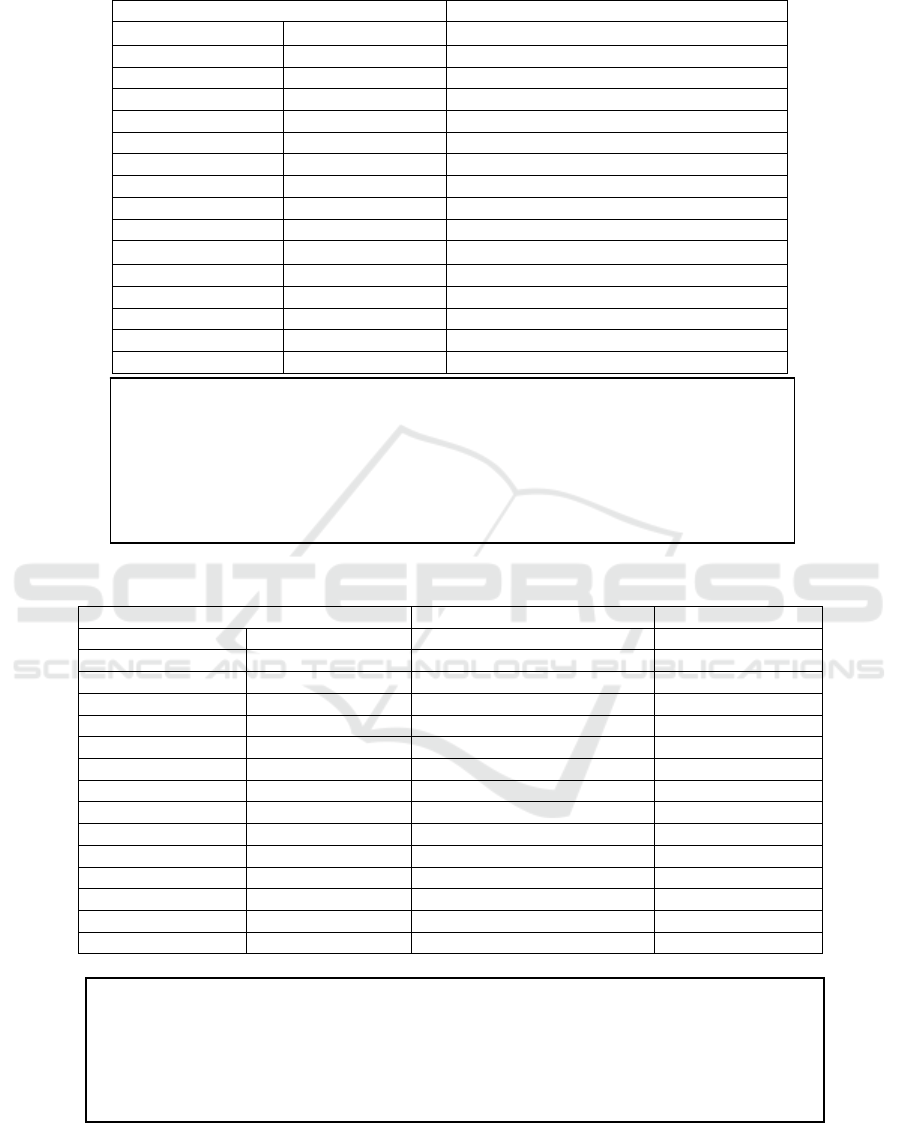
Table 1: Baseline Characteristic of Obese Subjects.
Parameters Total (mean±SD); n=45
Age (years) 41.69±5.69
Body weight (Kg) 78.79±13.26
BMI (kg/m
2
) 33.09±5.05
WC (cm) 96.34±9.33
ADMA (umol/l) 0.82±0.13
FPG (mg/dl) 86.00±10.94
PPG (mg/dl) 109.84±28.56
HbA1C (%) 5.56±0.56
Fasting Insulin (μIU/mL) 9.52±7.32
HOMA-IR 1.24±0.91
LDL-C (mg/dl) 137.51±33.51
HDL-C (mg/dl) 47.06±12.84
TG (mg/dl) 151.22±57.31
sd-LDL (mg/dl) 1.34±0.26
ApoB (g/L) 104.31±18.41
hs-CRP (mg/L) 3.64±2.38
Table 2: Relationship Between ADMA and Anthropometry, Glucose, Lipid, and Inflammation Parameters.
Parameters r P
Age (year) -0.057 0.356
Body weight (Kg) -0.056 0.407
BMI (kg/m
2
) -0.117 0.445
WC (cm) -0.100 0.256
FPS (mg/dl) -0.506 0.001*
PPS (mg/dl) -0.230 0.064
HbA1C (%) -0.334 0.013*
Fasting Insulin (μIU/mL) -0.102 0.255
HOMA-IR -0.225 0.069
LDL-C (mg/dl) -0.149 0.165
HDL-C (mg/dl) 0.154 0.157
TG (mg/dl) -0.315 0.017*
sd-LDL (mg/dl) -0.042 0.392
ApoB (g/L) -0.168 0.135
hs-CRP (mg/L) -0.059 0.351
Abbreviations: BMI, body mass index; WC, waist circumference; ADMA, asymmetric
dimethylarginine; FPG, fasting plasma glucose; PPG, postprandial plasma glucose;
HbA1c, glycosylated hemoglobin; HOMA-IR: homeostasis model assessment of insulin
resistance;; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein
cholesterol; TG, triglycerides; ApoB: apolipoprotein B; sd-LDL: small dense-LDL; CRP,
C-reactive protein;
* p<0.05.
Abbreviations: BMI, body mass index; WC, waist circumference; FPG, fasting plasma glucose;
PPG, postprandial plasma glucose; HbA1c, glycosylated hemoglobin; HOMA-IR: homeostasis
model assessment of insulin resistance; LDL-C, low density lipoprotein cholesterol; HDL-C, high
density lipoprotein cholesterol; TG, triglycerides; ApoB: apolipoprotein B; sd-LDL: small dense-
LDL; CRP, C-reactive protein;
* p<0.05.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
26

4 DISCUSSION
ADMA is believed to be a mediator that affects the
risk of atherosclerosis. Several clinical studies have
shown that increased ADMA is present in the
conditions of chronic kidney insufficiency,
dyslipidemia, hypertension, diabetes mellitus, and
hyperhomocysteinemia, and other conditions
(Landim, Casella & Chagas, 2009). The presence of
cardiovascular disease risk factors, especially
atherosclerotic disease will induce functional and
morphological changes in endothelium, become
easily inflamed, thrombosis, and vasoconstriction
(Vita & Keaney, 2002). The dysfunctional
endothelium can be detected by an imbalance
between widening and constricting factors,
procoagulant factors, and anticoagulant factors
which stimulate and inhibit the development and
proliferation of cells (Rubanyi, 1993).
Other clinical evidence also supported that
increased plasma ADMA was associated with
decreased NO synthesis (Boger et al.,1998). Plasma
ADMA levels can change rapidly in response to
changes in the risk factors. In diabetic patients, a few
hours after high-fat eating, plasma ADMA level
increases, and vasodilation is reduced (Fard et al.,
2000). In low body mass index (BMI) condition,
each 0.1 μmol/L increase in the plasma ADMA level
was associated with an increased risk of acute
myocardial infarct (AMI) with HR (95% CI) 1.21
(1.08-1.35) and cardiovascular death 1.30 (1.13-
1.49) (Hoy et al., 2007). ADMA level was 0.40-0.77
mol/L for the entire population, 0.41-0.79 mol/L
for men, 0.38-0.73 mol/L for women under 45
years old, and 0.41-0.84 mol/L for women above
45 years old (Hoy et al., 2007). Past studies showed
that plasma ADMA levels were higher in obesity
(McLaughlin et al., 2006). In this study, ADMA
levels were 0.82 ± 0.13 mol/L.
Based on several previous studies, plasma
ADMA levels were associated with the risk of AMI
and cardiovascular death (Borgeraas et al.,2016),
unchanged with weight loss in obesity (Rudofsky et
al.,2011), hypertension and insulin resistance
(Perticone et al., 2010), resistance insulin at the
beginning of diabetes (Nakhjayani et al., 2010),
HOMA-IR in prehypertension (Novianti et al.,
20013), BMI in overweight (Eid et al, 2004), and
HOMA-IR in obesity (Hidayat et al., 2011). In this
study, ADMA had a significant correlation with
FPG, HbA1c, and TG parameters [r = -0.506, p =
0.001; r = -0.334, p = 0.013, and r = -0.315. p =
0.017, respectively] in obesity.
5 CONCLUSION
The association between ADMA and increased
cardiovascular risks was related to glucose
metabolism, lipid, and insulin resistance with
various unknown mechanisms. Thus, further and
extensive research should be done to determine the
role of ADMA in the risk of cardiovascular disease.
CONFLICT OF INTERESTS
The authors declare that there is no conflict of
interests regarding the publication of this paper.
REFERENCES
Baylis C. 2006. Arginine, arginine analogs and nitric
oxide production in chronic kidney disease. Nat Clin
Pract Nephrol, 4, pp. 209-20.
Blake GJ, Ridker PM. 2002. Inflammatory Bio-Markers
And Cardiovascular Risk Prediction. J Intern Med,
252, pp. 283-94.
Boger RH, Bode-Boger SM, Thiele W, Junker W,
Alexander K, Frolich JC. 1997. Biochemical Evidence
For Impaired Nitric Oxide Synthesis In Patients With
Peripheral Arterial Occlusive Disease. Circulation, 95,
pp. 2068-74.
Böger RH1, Bode-Böger SM, Szuba A, Tsao PS, Chan JR,
Tangphao O, et al. 1998. Asymmetric
dimethylarginine (ADMA): a novel risk factor for
endothelial dysfunction: its role in
hypercholesterolemia. Circulation, 98(18), pp. 1842-7.
Borgeraas H, Hertel JK, Svingen GVT, Pedersen ER,
Seifert R, Nygård O, et al. 2016. Association between
Body Mass Index, Asymmetric Dimethylarginine and
Risk of Cardiovascular Events and Mortality in
Norwegian Patients with Suspected Stable Angina
Pectoris. PLoS ONE, 11(3), pp. 1-13.
Colak A, Coker I, Diniz G, Karademirci İ, Hanci T &
Bozkurt U. 2010. Interleukin 6 and tumor necrosis
factor alpha levels in women with and without glucose
metabolism disorders. Turkish Journal of
Biochemistry, 3(35), pp. 190-4.
Eid HMA, Arnesen H, Hjerkinn EM, Lyberg T, Seljeflot I.
2004. Relationship Between Obesity, Smoking, and
the Endogenous Nitric Oxide Synthase Inhibitor,
Asymmetric Dimethylarginine Metabolism, 53(12),
pp. 1574-9.
El Assar M, Angulo J, Santos Ruiz M, Adana RD,
Pindado JC, Sánchez Ferrer ML, et al. 2016.
Asymmetric dimethylarginine (ADMA) Elevation
And Arginase Up-Regulation Contribute To
Endothelial Dysfunction Related To Insulin Resistance
In Rats And Morbidly Obese Humans. Journal of
Physiology, 594(11), pp. 3045-60.
The Relationship between ADMA and Anthropometric Indicators, Glucose, Lipid, and Inflammatory Parameters in Obese People
27

Eliana F, Suwondo P, Makmun LH, Harbuwono DS.
2011. ADMA as a Marker of Endothelial Dysfunction
in Prediabetic Women. Acta Med Indones-Indones J
Intern Med, 43(2), pp. 92-8.
Fard A1, Tuck CH, Donis JA, Sciacca R, Di Tullio MR,
Wu HD, et al. 2000. Acute elevations of plasma
asymmetric dimethylarginine and impaired endothelial
function in response to a high-fat meal in patients with
type 2 diabetes. Arterioscler Thromb Vasc Biol, 20(9),
pp. 2039-44.
Goodson NJ, Symmons DP, Scott DG, Bunn D, Lunt M,
Silman AJ. 2005. Baseline levels of C-reactive Protein
And Prediction Of Death From Cardiovascular
Disease In Patients With Inflammatory Polyarthritis: a
ten-year follow-up study of a primary care-based
inception cohort. Arthritis Rheum, 52, pp. 2293-99.
Hidayat A, Wijaya A, Alrasyid H. 2011. Correlation
between IL-6, hsCRP, ET-1, ADMA and HOMA-IR in
Central Obese Men. Indones Biomed J, 3(1), pp. 43-50.
Hov G, Sagen E, A. Bigonah & Sberg AA. 2007. Health-
associated reference values for arginine, asymmetric
dimethylarginine (ADMA) and symmetric
dimethylarginine (SDMA) measured with high-
performance liquid chromatography G. Scand J Clin
Lab Invest, 67, pp. 868-76.
Huang S, Xu Y, Peng WF, Cheng J, Li HH, Shen LS, Xia
LL. 2018. A Correlational Study Between Serum
Asymmetric Dimethylarginine Level And Impaired
Glucose Tolerance Patients Associated With Obesity.
J Cell Physiol, pp. 1-6.
Kelm M. 2002. Flow-mediated dilatation in human
circulation: Diagnostic and Therapeutic Aspects. Am J
Physiol Heart Circ Physiol, 282, pp. 1-5.
Kielstein JT, Bode-Boger SM, Klein G, Graf S, Haller H,
Fliser D. 2003. Endogenous Nitric Oxide Synthase
Inhibitors And Renal Perfusion In Patients With Heart
Failure. Eur J Clin Invest, 33, pp. 370-5.
Landim MBP, Casella Filho A, Chagas ACP. 2009.
Asymmetric dimethylarginine (ADMA) and
Endothelial Dysfunction: Implications for
Atherogenesis. Clinics, 64(5), pp. 471-8.
Lin KY, Ito A, Asagami T, Tsao PS, Adimoolam
S, Kimoto M, et al. 2002. Impaired Nitric Oxide
Synthase Pathway In Diabetes Mellitus: Role of
Asymmetric Dimethylarginine and Dimethylarginine
Dimethylaminohydrolase. Circulation, 106, pp. 987-
92.
Lobo SM, Lobo FR, Bota DP, Lopes-Ferreira F, Soliman
HM, Mélot C et al. 2003. C-reactive Protein Levels
Correlate With Mortality And Organ Failure In
Critically Ill Patients. Chest, 123, pp. 2043–9.
Man P, Connett JE, Anthonisen NR, Wise RA, Tashkin
DP, Sin DD. 2006. C-reactive protein and mortality in
mild to moderate chronic obstructive pulmonary
disease. Thorax, 61(10), pp. 849-53.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA,
Treacher DF, et al. 1985. Homeostasis model
assessment: insulin resistance and β-cell function from
fasting plasma glucose and insulin concentrations in
man. Diabetologia, 28, pp. 412–9.
McLaughlin T, Stuhlinger M, Lamendola C, Abbasi F,
Bialek J, Reaven GM, et al. 2006. Plasma asymmetric
dimethylarginine concentrations are elevated in obese
insulin-resistant women and fall with weight loss. J
Clin Endocrinol Metab, 91, pp. 1896–900.
Miyazaki H, Matsuoka H, Cooke JP, Usui M, Ueda S,
Okuda S, et al. 1999. Endogenous Nitric Oxide
Synthase Inhibitor: A Novel Marker Of
Atherosclerosis. Circulation, 99, pp. 1141-6.
Nakhjavani M, Karimi-Jafari H, Esteghamati A,
Khalilzadeh O, Asgarani F, Ghadiri-Anari A. 2010.
ADMA is a correlate of insulin resistance in early-
stage diabetes independent of hs-CRP and body
adiposity. Annales d’Endocrinologie, 71, pp. 303-8.
National Institutes of Health. 1998. Clinical Guidelines on
the Identification, Evaluation, and Treatment of
Overweight and Obesity in Adults; The Evidence
Report. Obes Res, 6(2), pp. 51S–209S.
Novianti ME, Bakri S, Arief M, Sandra F. 2013.
Correlation between HOMA-IR with ADMA in
Prehypertension. Indones Biomed J, 5(3), pp. 169-72.
Peraldi P, Hotamisligil GS, Buurman WA, White MF &
Spiegelman BM. 1996. Tumor necrosis factor (TNF)
alpha inhibits insulin signaling through stimulation of
the p55 TNF receptor and activation of
sphingomyelinase. Journal of Biological Chemistry,
271(22), pp. 13018-22.
Perticone F, Sciacqua A, Maio R, Perticone M, Galiano
Leone G, Bruni R, et al. 2010. Endothelial
dysfunction, ADMA and insulin resistance in essential
hypertension. Int J Cardiol, 142(3), pp. 236-41.
Rubanyi GM. 1993. The role of the endothelium in
cardiovascular homeostasis and diseases. J Cardiovasc
Pharmacol, 22(4), pp. S1-S4.
Rudofsky G, Roeder E, Merle T, Hildebrand M, Nawroth
PP, Wolfrum C. 2011. Weight Loss Improves
Endothelial Function Independently of ADMA
Reduction in Severe Obesity. Horm Metab Res, 43,
pp. 343-8.
Savvidou MD, Hingorani AD, Tsikas D, Frolich JC,
Vallance P, Nicolaides KH. 2003. Endothelial
Dysfunction And Raised Plasma Concentrations Of
Asymmetric Dimethylarginine In Pregnant Women
Who Subsequently Develop Pre-Eclampsia. Lancet,
36, pp. 1511-7.
American Diabetes Association. 2010. Standards of
Medical Care in Diabetes. Diabetes Care, 33, pp. S11-
61.
Tsikas D, Rode I, Becker T, Nashan B, Klempnauer J,
Frolich JC. 2003. Elevated plasma and urine levels of
ADMA and 15(S)-8-iso-PGF2alpha in end-stage liver
disease. Hepatology, 38, pp. 1063-4.
Vita JA, Keaney Jr JF. 2002. Endothelial function: a
barometer for cardiovascular risk? Circulation, 106,
pp. 640-2.
WHO. Obesity: Preventing and managing the global
epidemic. Report of a WHO Consultation. WHO
Technical Report Series 894. Geneva: WHO,2000.
Zoccali C, Bode-Boger S, Mallamaci F, Benedetto
F, Tripepi G, Malatino L, et al. 2001. Plasma
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
28

Concentration of Asymmetrical Dimethylarginine And
Mortality In Patients With End-Stage Renal Disease: a
Prospective Study. Lancet, 358, pp. 2113-7.
The Relationship between ADMA and Anthropometric Indicators, Glucose, Lipid, and Inflammatory Parameters in Obese People
29
