
The Role of Percutaneous Transthoracic Core Needle Biopsy on
Diagnostic of Central and Peripheral Lung Nodule/Mass
using Chest CT Scan and Chest Ultrasound Guidance
Andhika Kesuma Putra
1
, Noni Novisari Soeroso
1*
, Hendra Taufik
1
1
Department of Pulmonology and Respiratory Medicine, Faculty of Medicine, Universitas Sumatera Utara,
Universitas Sumatera Utara Hospital, Jl. Dr. Mansyur No. 5 Medan 20155, Sumatera Utara, Indonesia
Keywords: Core biopsy, Percutaneous, Transthoracic
Abstract: Percutaneous transthoracic core needle biopsy is a technique using a longer sized needle and hooks allowing
tissue for histopathological examination on certain indications (lesion size over 8 mm or transthoracic
needle aspiration (TTNA) is not representative). The aim of this study was to analyze the role of core biopsy
size 14G (the largest size available in Indonesia) with a co-axially needle on diagnostic of central and
peripheral lung nodule/mass with the use of chest CT scan and chest ultrasound guidance. This is a
retrospective study of 58 patients with peripheral lung nodule/mass from the year 2014 to 2019.
1 INTRODUCTION
Core needle biopsy has become the dominant method
in obtaining tissue samples from pulmonary lesions
to make a pathological diagnosis (Zhou et al., 2013).
The development of imaging methods especially
computed tomography (CT) has contributed to more
accurate localization of lung lesions. It has
contributed to making this procedure universally
well-known and performed on a large scale. The
procedure has actually become a viable alternative to
other diagnostic procedures such as sputum cytology,
bronchoscopy, and thoracotomy, with a high quality
of material sampling collected for analysis (Beckh,
Blcskei, and Lessnau, 2002; Junqueira et al., 1990).
The guided biopsy with computed tomography
has been widely accepted as an effective and safe
procedure for a specific diagnosis (Guimarães et al.,
2009; Yu et al., 2002).
Another imaging development for lung lesion is
an ultrasound (US). Sonogram has been described as
a useful tool in characterizing unspecified pleural or
subpleural pulmonary lesions, when there is no lung
aeration in between (Sartori et al., 2007). In addition,
US can be used as a safe and effective method to
guide the biopsy of masses in the chest wall
(Schubert et al., 2005). The main advantage of this
imaging modality is that the US allows real-time
monitoring of procedures and can be done at the
patient's bedside, without using radiation.
Transthoracic core needle biopsy is indicated to
determine nodules or pulmonary masses tissue. Core
biopsy is a technique similar to transthoracic needle
aspiration (TTNA) using a longer and bigger size
needle with a cutting needle so it can obtain tissue for
histopathology examination based on certain
indications (tumor size is more 8 mm or yield TTNA
is not representative).
While core biopsy size 14-18 G was used for the
first time in the early 1980s. It has been shown that
only 40-50% of small peripheral thoracic lesions are
malignant. Using percutaneous biopsy, surgery or
thoracoscopy can be avoided in 64% of patients
(Liao et al., 2000).
Core biopsy was performed with image guidance,
including chest CT and US. Some previously
published articles for CT guided biopsy have
described their role as modalities effective guidelines
for diagnosing intrathoracic lesions (Liang et al.,
2014).
In this study, our aim was to describe the sample
characteristics and the accuracy of transthoracic
biopsy cores using US or CT guidelines to diagnose
lung lesions.
2 METHODS
The researchers collected retrospectively cases of
biopsy procedures that had been conducted by
12
Putra, A., Soeroso, N. and Taufik, H.
The Role of Percutaneous Transthoracic Core Needle Biopsy on Diagnostic of Central and Peripheral Lung Nodule/Mass using Chest CT Scan and Chest Ultrasound Guidance.
DOI: 10.5220/0009841100120014
In Proceedings of the 2nd International Conference on Tropical Medicine and Infectious Disease (ICTROMI 2019), pages 12-14
ISBN: 978-989-758-469-5
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
researchers from 2014 to 2019 at Columbia Asia
Hospital Medan and Malahayati Islamic Hospital
Medan, Indonesia. A total of 58 patients consisted of
12 women and 46 men aged 19 to 79 years old was
enrolled.
By using chest radiographs or chest CT scan we
determined if there were nodules or masses in the
lung. All patients were then informed of which
procedures they should receive and all subjects
consented for the procedures to be performed.
Of the 58 core biopsy actions, two guides were
selected, imaging CT scan or US guide. Forty-three
patients were guided using chest CT scan and 15
patients used US guide. If the lesions were located
near the chest wall or peripherally and the size was
more than 2 cm, it will be guided with the US. But if
the lesion was less than 2 cm and located in the
deeper or center, it was done with the CT scan
guidance.
We marked the site of insertion of the core
biopsy needle. We infiltrated the local anesthesia
lidocaine from the skin through the parietal pleura
using a 26G needle syringe. Then we inserted the co-
axially needle as the core biopsy cutting needle
cannula catheter to obtain the tissues. Each specimen
was immediately put into a container containing 10%
formalin and sent to the pathology department for
further examination.
At the end of the procedure, all patients were
monitored for signs and symptoms of complications,
such as hemoptysis and pneumothorax.
3 RESULTS
During this period, a total of 58 core biopsy actions
were carried out. Of those, 43 were guided using CT
scan and 15 patients were guided with the US. Table
1 describes the baseline characteristics of patients.
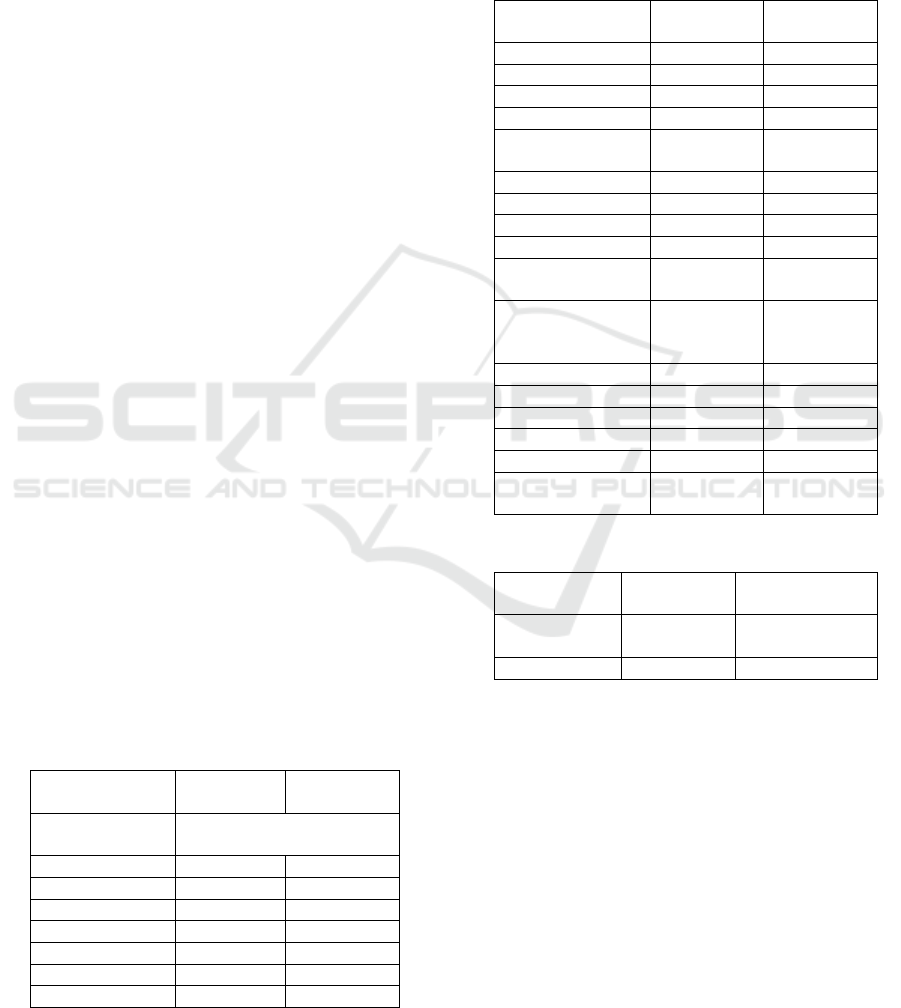
Table 1: Characteristics of patients underwent core biopsy
randomized to US guidance or CT guidance.
Characteristics US-guided
(n=15)
CT-guided
(n=43)
Mean age
(years)
53,28 ± 14,63 years
Age (years)
16-35 3 (19.8.%) 9 (20.8%)
36-55 6 (39.9%) 17 (39.4%)
56-75 6 (40.0%) 17 (39.4%)
Sex
Male 12 (80.0%) 34 (79.0%)
Female 2 (13.3%) 10 (23.0%)
Histopathology diagnosis is described in table 2, and
the complications of the procedures are stated in
table 3. There were 3 pneumothorax complications
(6.9%) that occurred with an area of pneumothorax
<20% but there was no requirement to place
intercostal chest tube placement, and 1 (1.7%)
hemoptysis complication was reported.
Table 2: Final histopathology diagnosis.
Histopathology
Classification
US-guided
(n=15)
CT-guided
(n=43)
Adenocarcinoma 8 (53.0%) 10 (23.0%)
Squamous cell ca 4 (26.0%) 11 (25.0%)
Large cell ca 1 (6.6%) 2 (4.6%)
Adenosquamous 1 (6.6%) 0
Small cell lung
carcinoma
0 3 (6.9%)
Oat Cell 0 1 (2.3%)
Yolk sac 0 2 (4.6%)
Mature teratoma 0 1 (2.3%)
NHL 1 (6.6%) 0
Lung
fibrosarcoma
0 1 (2.3%)
Non specific
inflamatory
process
0 2 (4.6%)
Pulmonary TB 1 (6.6 %) 4 (9.3 %)
Pneumonia 0 1 (2.3%)
Fibrotic Mass 0 2 (4.6%)
Plasmacytoma 0 1 (2.3%)
Cryptococcus 0 1 (2.3%)
Loss Connective
Tissue
0 1 (2.3%)
Table 3: Complication core biopsy
Complication US-guided
(n=15)
CT-guided
(n=43)
Pneumothorax
<20%
0 3 (9.3%)
Hemoptysis 0 1 (2.3%)
4 DISCUSSION
Transthoracic core needle biopsy is an alternative
intervention when bronchoscopy is not available. A
percutaneous pulmonary biopsy is a safe and
accurate procedure for the diagnosis of focal
thoracic lesions. A study conducted by Liang et al.
(2014) showed that CT-guided biopsy cores with
cytology evaluation had a low and adequate atypical
level. Pulmonary core biopsy can provide a more
accurate tumor classification and specific diagnosis
for non-neoplastic lesions. Adequate networks are
often available for molecular studies.
The Role of Percutaneous Transthoracic Core Needle Biopsy on Diagnostic of Central and Peripheral Lung Nodule/Mass using Chest CT
Scan and Chest Ultrasound Guidance
13

The rate of complication of biopsy of
pneumothylactic core needles is compatible with
fine needle aspiration. Pneumothorax and mild
bleeding are the common complications of core
biopsy. Liang et al. (2014) reported pneumothorax
incidence at 31.4%. Beslic et al. (2012) compared
the rates of complications in percutaneous fine
needle aspiration biopsy guided by CT and core
needle biopsy and discovered that pneumothorax
was detected in 9.7% of patients with a fine needle
biopsy and 31.5% in patients with core biopsy.
However, other authors reported varying rates of
pneumothorax ranging from less than 10% to more
than 60% in fine needle aspiration and core biopsy
(Minot et al., 2012). In our institution, CT-scan and
US were immediately performed post-procedure in
all patients and broad criteria for the pneumothorax
was used from the Light study (Light, 1990).
The limitation of our study is that the authors
did not report the size of radiological lesions, TNM
grading, and pain score.
5 CONCLUSION
The percutaneous core needle biopsy procedure
guided by CT and US showed high accuracy of
results, 79.3% of the lesions obtained
histopathologically were malignant lesions.
In all cases studied, there was no report from the
pathologists of an inadequate sample or
unavailability of tissue. Although the needle used is
a large type of needle (size 14G) and it is the largest
needle available in Indonesia but the complications
of pneumothorax turned out to be low (6,9 %).
Pneumothorax is a common complication and has
been reported to occur in 50% of events. In our
report, there were no additional intervention
procedures like simple aspiration or chest tube
insertion needed.
Our study shows that CT biopsy with CT or US
guidelines is a safe procedure and is generally well
tolerated. Some patients may experience significant
and lasting pain and therefore must receive detailed
information regarding this procedure.
FUNDING
No grant support or funding from public institutions
or private enterprises was received for this research.
ACKNOWLEDGMENTS
The researcher would like to thank Columbia Asia
Hospital and Universitas Sumatera Utara Hospital
which have allowed the retrieval of medical history
data.
REFERENCES
Beckh, S., Blcskei, P. L. and Lessnau, K. D., 2002. Real-
time chest ultrasonography: A comprehensive review
for the pulmonologist. Chest. 122: 1759-1773. doi:
10.1378/chest.122.5.1759.
Beslic, S., Zukic, F. and Milisic, S., 2012. Percutaneous
transthoracic CT guided biopsies of lung lesions; Fine
needle aspiration biopsy versus core biopsy. Radiology
and Oncology. 46: 19-22. doi: 10.2478/v10019-012-
0004-4.
Guimarães, MD. et al., 2009. Predictive success factors
for CT-guided fine needle aspiration biopsy of
pulmonary lesions. Clinics. 64:1139–44.
Junqueira, MAF. et al., 1990. Biópsia pulmonar
transtorácica orientada por tomografia
computadorizada. J Pneumol. 16:1–5.
Liang, L. et al., 2014. CT-Guided Core Needle Biopsy of
Peripheral Lung Lesions with Onsite Adequate
Evaluation: Review of 215 Cases. Journal of Cytology
& Histology. doi: 10.4172/2157-7099.s4-018.
Liao WY. et al., 2000. US-guided transthoracic cutting
biopsy for peripheral thoracic lesions less than 3 cm in
diameter. Radiology. 217: 685-91.
Light RW. Pneumothorax. In Light RW (ed): Pleural
Diseases, 3
rd
ed. Baltimore: Williams & Wilkins,
1990.
Minot, D. M. et al., 2012. Evolution of transthoracic fine
needle aspiration and core needle biopsy practice: A
comparison of two time periods, 1996-1998 and 2003-
2005. Diagnostic Cytopathology. 40: 876-881. doi:
10.1002/dc.21666.
Sartori, S. et al., 2007. Accuracy of transthoracic
sonography in the detection of pneumothorax after
sonographically guided lung biopsy: Prospective
comparison with chest radiography. American Journal
of Roentgenology. 188(1): 37-41. doi:
10.2214/AJR.05.1716.
Schubert, P. et al., 2005. Ultrasound-assisted transthoracic
biopsy: Cells or sections?. Diagnostic Cytopathology.
33(4): 233-237. doi: 10.1002/dc.20342.
Yu, LS. et al., 2002. Computed tomography-guided
cutting needle biopsy of pulmonary lesions. Rev Hosp
Clin Fac Med Sao Paulo. 57:15–8.
Zhou, Y. et al., 2013. CT-guided robotic needle biopsy of
lung nodules with respiratory motion - Experimental
system and preliminary test. International Journal of
Medical Robotics and Computer Assisted Surgery. 9:
317-330. doi: 10.1002/rcs.1441.
ICTROMI 2019 - The 2nd International Conference on Tropical Medicine and Infectious Disease
14
