
Saiful Anwar Hospital Heart Failure Registry (SAHEFAR) : A
Valuable Tool for Improving the Management of Patients with Heart
Failure in Malang, East Java
Anita Surya Santoso
1,2
,
Krishna Ari Nugraha
1,2
, M Rizki Fadlan
1,2
, Dea Arie Kurniawan
1,2
, Liemena
Harold Adrian
1,2
,
Faris Wahyu Nugroho
1,2
, Puspa Lestari
1,2
, Seprian Widasmara
1,2
and Mohammad Saifur Rohman
1,2
1
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Brawijaya University – Dr. Saiful Anwar General
Hospital, Malang, East Java, Indonesia
2
Brawijaya Cardiovascular Research Center, Brawijaya University, Malang, East Java, Indonesia
fariswahyunugroho, pusparyath, seprian.w}@gmail.com, ippoenk@yahoo.com
Keywords: Heart Failure, Malang Registry
Abstract: The incidence of heart failure (HF) in Malang has been increasing. Thus, a registry is required to
accommodate better comprehension of HF patients, particularly in Malang. To examine this demographic,
clinical and biological baseline characteristics and outcomes of hospitalised patients with HF are tracked by
creating the Saiful Anwar Hospital Heart Failure Registry (SAHEFAR) as a manual for continually
improving quality of care. This is a single-centre, retrospective cohort study. We included patients with
diagnosed HF based on 2016 ESC HF criteria. The patients were assessed and their symptoms, physical
examination, laboratory results, electrocardiography, echocardiography, prior medical and in-hospital
treatment were recorded. We followed up with the patient from initial hospital admission until discharge.
The outcome and all-cause mortality were recorded. The total patient data collected from January 2016 to
August 2019 was 1208. Male predominance was seen (58.1%). The most common precipitating factor of
admission for HF was coronary artery disease (60.1%), with the classification NYHA class III–IV (44.5%).
The number of patients receiving optimal medication was 63%. In-hospital for all-cause mortality was
19.5%. SAHEFAR can be a valuable tool for therapeutic approaches undertaken in daily practice and may
improve the outcomes of HF patients in a more specific setting, particularly in Malang.
1. BACKGROUND
Heart failure (HF) is a one of the major public health
problem worldwide. HF has emerged as a major
global health issue, with an estimated worldwide
prevalence of more than 37.7 million.
The burden is
rapidly increasing, and it is projected that by 2030,
the number of HF patients will increase by 25%
(Bacal et al., 2015).
HF is a disease with a high
mortality rate; average survival is five years with
marked impairment in the quality of life, making this
disease the central focus of these patients’ lives.
Approximately 80% require at least one
hospitalisation due to decompensation, which
represents a negative breaking point in patient
evolution (Chioncel et al., 2015).
Epidemiological data on HF is missing in many
countries because of the absence of relevant
observational studies to capture the incidence,
prevalence, prognosis and main causes of HF
(Fairman et al., 2017).
Proper understanding of the
epidemiology and the clinical characteristics of HF
in a specific population is critical for improving
prognosis. Randomised clinical trials bring
important epidemiological information, but
generalisation and applicability are limited by the
strict inclusion and exclusion criteria (Laotavom et
al., 2010). Even though registries do not have such
limitations and likely reflect the global population
with HF in a certain geographical area, there are
significant differences at both the continental and
regional levels in regard to the severity, aetiology
and management for HF (Savarese et al., 2019).
42
Santoso, A., Nugraha, K., Fadlan, M., Kurniawan, D., Adrian, L., Nugroho, F., Lestari, P., Widasmara, S. and Rohman, M.
Saiful Anwar Hospital Heart Failure Registry (SAHEFAR): A Valuable Tool for Improving the Management of Patients with Heart Failure in Malang, East Java.
DOI: 10.5220/0009388400420047
In Proceedings of the 4th Annual International Conference and Exhibition on Indonesian Medical Education and Research Institute (The 4th ICE on IMERI 2019), pages 42-47
ISBN: 978-989-758-433-6
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

The purpose of the Saiful Anwar Hospital Heart
Failure Registry (SAHEFAR) is to improve and
develop the care of patients with a specific diagnosis
in a specific hospital by providing continuous
information about care and therapy. In addition,
information from one hospital can be compared with
the average from the other participating hospital.
The long-term goals of the registry are to prevent
worsening symptoms, improve the quality of care,
reduce morbidity and mortality and lower the cost
of managing patients with HF.
2. METHOD
SAHEFAR was established in 2016, and we
collected data from then until now. This is a single-
centre and retrospective cohort study focused on
acquiring information about patients with HF. It was
initially a paper-based registry, and then the data
was transferred onto computerised patient records.
We included a patient with diagnosed HF based on
the 2016 ESC HF criteria.
First, we acquired basic information about the
patients, including sex, age, address, phone number,
level of education, occupation, marital status and
sources of financing. Afterwards, data collection
will include a physical examination and vital signs,
including blood pressure, heart rate, demographic
variables, clinical symptoms, functional status, date
of HF diagnosis and prior cardiovascular
investigations, clinical risk factors, lifestyle factors
and socioeconomic status, and a survey of cultural
beliefs, health practices and attitudes towards device
therapy.
We also collected laboratory samples, which
consisted of haemoglobin, leucocyte, ureum,
creatinine, random blood sugar, uric acid, liver
function test, albumin, haemostatic function,
troponin and CKMB, natrium, kalium, low-density
lipoprotein, high density lipoprotein, triglyceride,
cholesterol and blood gas analysis. Patients were
examined with a 12-lead electrocardiography
standard and transthoracic echocardiography and
followed from their initial hospital admission until
discharge.
2.1 Eligibility Criteria
The inclusion criteria for the database adhere to the
European guidelines for AHF. There must be the
symptoms of HF, which is dyspnoea, increased
fatigue and ankle swelling. Objective signs of HF
consist of elevated jugular venous pressure,
pulmonary crackles and peripheral oedema and
displacement of the apical impulse (Ponikowski et
al., 2016). The decision on inclusion in the registry
and populating the database was made by the doctor
in charge in the emergency room. There was no
exclusion criterion.
Patients were systematically classified according
to the type of AHF (de novo or acute
decompensation of chronic heart failure), aetiology
of AHF (acute coronary syndrome, chronic coronary
artery disease, valvular disease, arrhythmia,
hypertensive crisis and so on) and six basic
syndromes of AHF defined according to ESC
guidelines: 1) acute decompensated heart failure
(ADHF, with signs and symptoms of AHF, which
are mild and do not fulfil criteria for cardiogenic
shock, pulmonary oedema or hypertensive crisis);
2) hypertensive AHF (symptoms of AHF are
accompanied by high blood pressure on admission
and relatively preserved left ventricular function
with a chest radiograph compatible with acute
pulmonary oedema); 3) pulmonary oedema
(accompanied by severe respiratory distress, with
crackles over the lungs and orthopnoea and
O
2
saturation usually <90% prior to treatment); 4)
cardiogenic shock (defined as evidence of tissue
hypoperfusion induced by heart failure after
correction of preload, mostly with systolic BP <90
mmHg ongoing for at least 30 minutes); 5) high
output failure (characterised by high cardiac output,
usually with high heart rate, often caused by
arrhythmias, thyrotoxicosis crisis and anaemia); and
6) right heart failure (characterised by low output
syndrome with increased jugular venous pressure,
increased liver size and hypotension) (Schøedt et al.,
2016; Wang et al., 2016).
The primary endpoint of this registry is to
describe the epidemiological characteristics of
inpatients with heart failure. It can also provide data
related to diagnosis, aetiology, precipitating factor
and treatment.
2.2 Limitation
There are a limited number of participating hospitals
or cardiac centres. Most of the patient recruitment
was in the Saiful Anwar Hospital, rather than from
all parts of Indonesia. Additionally, the registry was
only done in one cardiac centre, and it was a
government or university hospital with limited beds
only available for very sick patients. Finally,
SAHEFAR data came from medical records of
hospitalised patients so it represented an
epidemiologic study of hospital-based heart failure;
Saiful Anwar Hospital Heart Failure Registry (SAHEFAR): A Valuable Tool for Improving the Management of Patients with Heart Failure
in Malang, East Java
43

thus, it does not represent national data on heart
failure.
3. RESULTS
The total number of patients registered in this pilot
study was 1208 patients. The independent factors
were the demographic characteristics that are shown
in Table 1. Overall, our patients had an age of fewer
than 60 years, and 62.3% weremale (see Figures 1
and 2). Compared with patients in the United States,
our patients tended to be younger. Due to our region
within Malang, most our patients were of Javanese
ethnicity and held various occupational statuses.
There were 81.6% of patients living in and around
Malang, which is <50 km from Saiful Anwar
General Hospital.
Table 1: Sociodemographic characteristics.
Sociodemographic characteristics
Percentage (%)
Male
62.3
Female
37.7
< 60
57.4
60–69
28.7
70–79
10.7
> 80
3.3
Javanese
98.4
Chinese
0.8
Arabian
0.8
Less than elementary school
8.2
Elementary school (finished)
24.8
Junior high school (finished)
21.5
Senior high school (finished)
37.2
University
8.2
Jobless
18
Student
1.6
Housewife
13.1
Employee
4.9
Pensionary
10.7
Entrepreneur
35.2
Farmer/Fisherman
11.5
Labour
4.9
Not married
1.6
Married
93.4
Divorced
4.9
Private/Independent
4.9
Government
95.1
Figure 1: Characteristics of gender.
Figure 2: Characteristics of age.
The 4th ICE on IMERI 2019 - The annual International Conference and Exhibition on Indonesian Medical Education and Research Institute
44

Figure 3: Aetiologies of heart failure.
Table 2: Clinical characteristics.
Clinical characteristics
Percentage (%)
History of HF
Yes
69.7
No
30.3
IHD documented by coronary
angiography
12.3
IHD not documented by coronary
angiography
54.1
Dilated cardiomyopathy
9.8
Valve disease
5.7
Tachycardia related
cardiomyopathy
0.8
HFpEF syndrome
3.3
Hypertension
9
Pulmonary hypertension
1.6
Others
3.3
No
82.8
Permanent
4.9
Persistent
4.9
Paroxysmal
7.4
I
2.5
II
27.9
III
44.3
IV
25.4
Infection
11.8
Poor compliance
15.7
Inadequate treatment
7.8
Acute coronary syndrome
33.3
Arrhythmia
10.8
Volume overload
2.9
Hypertension crisis
6.9
Valve regurgitation
2
Post-partum cardiomyopathy
1
Decreased renal function
1
Overactivity
1
Pulmonary hypertension
1
Coronary arterial disease
2.9
Hypertensive heart disease
1
Others
1
Sinus rhythm
82
Junctional
0.8
Atrial fibrillation
15.6
Total AV block
0.8
Ventricular pacing rhythm
0.8
Mean EF
46.7
EF 40%
65.6
EF < 40%
34.4
Resolved
86.9
Death
13.1
Cardiogenic shock
25
Septic shock
37.5
Respiratory distress
18.75
Ventricular fibrillation
6.25
Ventricular tachycardia
6.25
Critical pulmonary hypertension
6.25
Saiful Anwar Hospital Heart Failure Registry (SAHEFAR): A Valuable Tool for Improving the Management of Patients with Heart Failure
in Malang, East Java
45
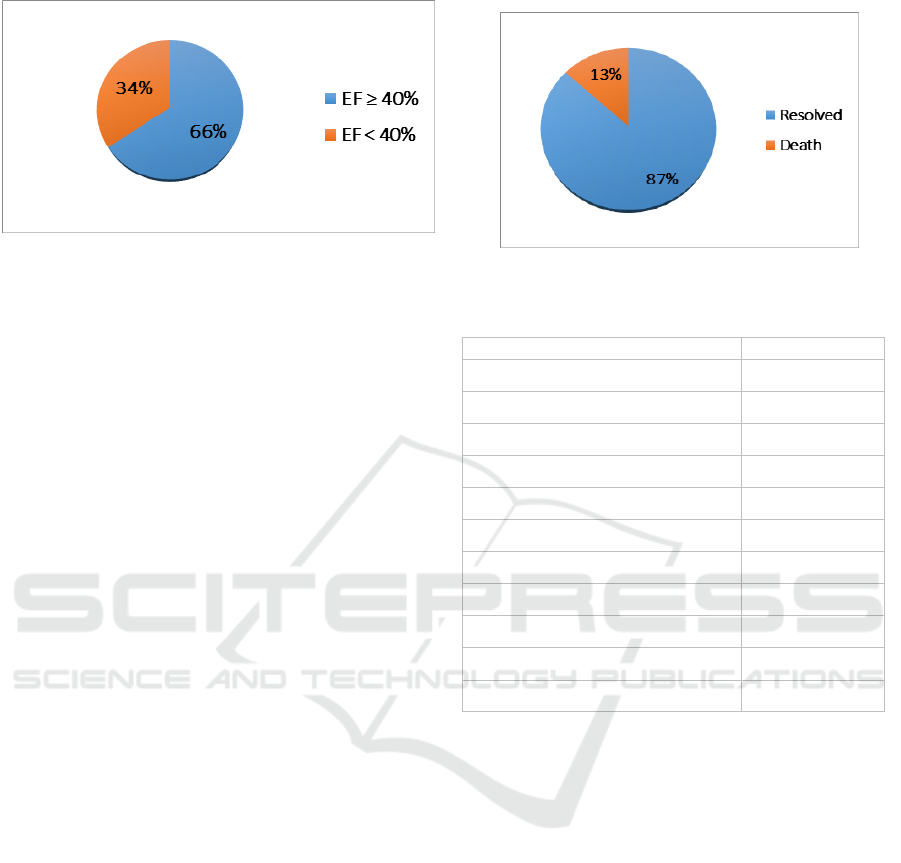
Figure 4: Variation of ejection fraction.
In our cases, we found that most patients came
with worsening heart failure due to acute coronary
syndrome (33.3%) and paralleled with ischemic
heart condition (66.4%), documented or
undocumented by coronary angiography, to be the
leading precipitating factor. Other aetiologies were
dilated cardiomyopathy (9.8%) and valve disease
(5.7%) (Figure 3). We found poor compliance
(15.7%) and infection (11.8%) to be the leading
precipitating factors after myocardial infarction. The
incidence of coronary arterial disease is relatively
high at our hospital, and in Western countries. It is
contradictive with South Asian countries, suggesting
that the incidence was relatively low. The ethnic
predisposition can be exaggerated by nutritional,
environmental and behavioural factors. However,
our data in Indonesia demonstrated the finding that
coronary artery disease tends to be higher and has an
important role in the development of heart failure.
Another challenging condition showed that our
patients had dilated cardiomyopathy and valve
disease because further aggressive treatment was
needed.
The median hospital length of stay was 7.5 days,
a shorter period than in Europe and Latin America
(9.0 and 9.9 days, respectively). We found a hospital
mortality of 13.1% (see Figure 5), which was higher
than the mortality rate in the Asia Pacific Region
(4.8%) vs. the United States (3.0%), similar to
Europe (6.7%) and lower than Latin America
(8.0%). The most common of aetiologies were septic
shock (37.5%) and cardiogenic shock (25%). Our
patients were commonly found with preserved
ejection fraction (65.6%), but the mean of ejection
fraction was 46.7% (Figure 4). Such facts indicated
that most of our patients came in better condition,
but had a poorer outcome. Such conditions may be
indicated for treatment strategy at our hospital.
Figure 5: Clinical outcome.
Table 3: Risk factors.
Risk factors
Percentage (%)
Never
50
Current
21.3
Former
28.7
Yes
30.3
No
68.9
Newly diagnosed
0.8
Never
95.1
Former
4.9
Minimal
27.9
Moderate
68.0
Heavy
4.1
Based on clinical presentation, we also noted that
newer patient (de novo acute HF) as represented by a
lower incidence of a prior heart failure history
compared to the U.S. data (69.7% vs 76%). Half of
our total patients had a smoking habit (50%), and
68% participated in moderate physical activity.
Based on the above data, we conclude that heart
failure is one of the leading causes of readmission
and mortality at Saiful Anwar General Hospital in
Malang. In summary, our data show that males are
twice as common as females, younger, of Javanese
ethnicity with EF 40%; and the leading aetiologies
of heart failure are coronary artery disease, dilated
cardiomyopathy and hypertension. The mortality
rate is 13.1%, and the leading death aetiologies are
septic shock and cardiogenic shock. Due to our
limitations and poor compliance of patients,
however, we were unable to completely perform
comprehensive examinations such as biomarkers,
exercise tests and Holter monitoring.
The 4th ICE on IMERI 2019 - The annual International Conference and Exhibition on Indonesian Medical Education and Research Institute
46

From these initial data, we are now building a
local registry of incidences of heart failure with
more subjects and greater examination. We feel it is
essential that we convince the doctors and the
government that heart failure has become an
epidemic cardiovascular disease with high mortality
and morbidity rates and a significant cost that could
be prevented by a national health program that
addresses coronary artery disease and hypertension.
To improve heart failure treatment, every large
hospital should have a heart failure clinic with a
prevention program that will work to decrease the
cost, morbidity and mortality of heart failure.
4. CONCLUSIONS
Heart failure has a high prevalence in Malang,
resulting in hospital admission. SAHEFAR can be
an effective and useful media to collect data and
reveal characteristics of patients with HF,
hospitalisation length-of-stay, mortality and
suboptimal guideline-directed medical treatment.
This registry can be a valuable tool for guiding
therapeutic approaches undertaken in daily practice.
It may also improve the outcomes of HF patients in
a more specific setting, particularly in Malang.
ACKNOWLEDGEMENTS
The Saiful Anwar Hospital Heart Failure Registry
(SAHEFAR) was endorsed by the heart team of the
cardiovascular division at Brawijaya University, and
collaboration was provided through the Saiful
Anwar Hospital.
REFERENCES
Albuquerque, D. C., Neto, J. D., Bacal, F., Rohde, L. E.,
Bernardez-Pereira, S., Berwanger, O., and Almeida,
D. R. (2015). I Brazilian Registry of Heart Failure –
Clinical Aspects, Care Quality and Hospitalization
Outcomes. Arquivos Brasileiros De
Cardiologia, 104(6), 433–442.
http://doi.org/10.5935/abc.20150031
Arcopinto, M., Salzano, A., Ferrara, F., Bobbio, E., Marra,
A. M., Abete, R., … Cittadini, A. (2015). The TOSCA
Registry: An Ongoing, Observatuional, Multicenter
Registry for Chronic Heart Failure. Translational
Medicine @ UniSa, 14(5), 21–27.
Chioncel, O., Tatu-Chitoiu, G., Christodorescu, R.,
Coman, I. M., Deleanu, D., Vinereanu, D., …
Filippatos, G. (2015). Characteristics of patients with
heart failure from Romania enrolled in – ESC-HF
Long-Term (ESC-HF-LT) Registry. Romanian
Journal of Cardiology, 25(4), 413–420.
Fairman, E. B., Diez, M., Fernández, A. A., Tala Vera, M.
L., Perna, E. R., Pereiro, S. M., … Belziti, C. A.
(2017). Participation of Argentina in the European
Registry of Heart Failure. Argentine Journal of
Cardiology, 85(4), 332–339.
http://doi.org/10.7775/rac.v85.i4.10972
Laothavorn, P., Hengrussamee, K., Kanjanavanit, R.,
Moleerergpoom, W., Laorakpongse, D., Pachirat, O.,
… Sritara, P. (2010). Thai Acute Decompensated
Heart Failure Registry (Thai ADHERE). CVD
Prevention and Control, 5(3), 89–95.
http://doi.org/10.1016/j.cvdpc.2010.06.001
Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H.,
Cleland, J. G. F., Coats, A. J. S., … van der Meer, P.
(2016). 2016 ESC Guidelines for the diagnosis and
treatment of acute and chronic heart failure: The Task
Force for the diagnosis and treatment of acute and
chronic heart failure of the European Society of
Cardiology (ESC). European Heart Journal, 37(27),
2129–2200. http://doi.org/10.1093/eurheartj/ehw128
Savarese, G., Vasko, P., Jonsson, Å., Edner, M.,
Dahlström, U., and Lund, L. H. (2019). The Swedish
Heart Failure Registry: A living, ongoing quality
assurance and research in heart failure. Upsala
Journal of Medical Sciences, 124(1), 65–69.
http://doi.org/10.1080/03009734.2018.1490831
Schjødt, I., Nakano, A., Egstrup, K., and Cerqueira, C.
(2016). The Danish Heart Failure Registry. Clinical
Epidemiology, 8, 497–502.
http://doi.org/10.2147/CLEP.S99504
Wang, C. C., Chang, H. Y., Yin, w H., Wu, Y. W., Chu, P.
H., Wu, C. C., … Cherng, W. J. (2016). TSOC-HFrEF
Registry: A Registry of Hospitalized Patients with
Decompensated Systolic Heart Failure: Description of
Population and Management. Acta Cardiologica
Sinica, 32(4), 400–411.
http://doi.org/10.6515/acs20160704a
Saiful Anwar Hospital Heart Failure Registry (SAHEFAR): A Valuable Tool for Improving the Management of Patients with Heart Failure
in Malang, East Java
47
