
Improvement of Knowledge on Iron Deficiency Anemia and Its
Prevention among Bustanul Athfal Teachers in Malang
Diah Hermayanti*, Meddy Setiawan and Hawin Nurdiana
Faculty of Medicine, University of Muhammadiyah Malang
Jalan Bendungan Sutami 188A Malang 65145 East Java, Indonesia
Keywords:
Iron deficiency anemia, knowledge, prevention
Abstract:
Iron deficiency anemia is still one of the national nutritional problems in Indonesia. This anemia mainly
affects women and children. In woman, increased of iron is due to pregnancy, childbirth, and breastfeeding.
In infants and children this due to their needs for growth. Iron deficiency anemia is also influenced by
socio-economic factors, mal absorption, and infection. In this study, a deficiency anemia prevention
training was conducted among Busthanul Athfal Teachers in Malang. This studiy is aimed to compare the
average knowledge about iron deficiency anemia and its prevention before and after training. The research
was conducted with training activities, pretest and posttest. Data was analyzed by comparative analytic
paired t-test. The questionnaire was filled by 46 respondents. The average value of the pretest knowledge
was 47.8, and the test post was 75.2. Result of data analysis on different test was 0,000 (p <0.05). There
was an increase in knowledge about iron deficiency anemia and its prevention. There was an increase in
knowledge about iron-deficiency anemia and its prevention after training among Busthanul Athfal Malang
teachers.
1 INTRODUCTION
The World Health Organization (WHO) reported that
in 2011, there were an estimated 800 million children
and women who developed anemia. The highest
prevalence occurred in children at 42.6% and
pregnant women at 38.2%. In Indonesia, the
prevalence of anemia occurs in 32% of children aged
6-59 months, 22% in non-pregnant women aged 15-
49 years, 30% in pregnant women aged 15-49 years
(WHO et al., 2011; World Health Organization,
2015).
In Indonesia, Riset Kesehatan Dasar (Riskesdas)
in 2013 reported that the prevalence of anemia at age>
1 year was 27.1%. Based on the age group, it was
found that anemia in children under five was quite
high at 28.1%, and pregnant women around 37.1%
(Kementrian Kesehatan Republik Indonesia, 2019).
Efforts should be made to reduce the prevalence
of iron deficiency anemia. The strategic activity is
training on Busthanul Atfal teachers in Malang,
because every day they interact with toddlers and
their parents. After this training, it is expected to be
able to transfer knowledge to parents of students, and
pay more attention to giving iron-rich nutrition to
their students. The obstacle is that the knowledge
about iron deficiency anemia and its prevention is not
good. This activity was carried out by increasing their
knowledge of iron deficiency anemia and its
prevention, and the introduction of a variety of iron-
rich foods.
Anemia occurs when hemoglobin (Hb) levels are
below 13.0 g / dl in adult men, below 12.0 g / dl in
non-pregnant women, and below 11.0 g / dl in
pregnant women (World Health Organization, 2015).
The erythrocytes morphology in iron deficiency
anemia appear microcytic hypo chrome characterized
by a decrease in the mean corpuscular hemoglobin
(MCH) index and mean corpuscular volume (MCV),
there is a decrease in transferrin saturation below 20%
and ferritin below 30 mg / ml (Jimenez, Kulnigg-
Dabsch and Gasche, 2015). On blood smear,
erythrocytes appear hypochromic microcytic,
anisocytosis-poicylocytosis, target cells and pencil
cells. Erythroblasts in the bone marrow show crude
irregular cytoplasm and the absence of iron reserves,
but bone marrow is usually not used for diagnosis
(World Health Organization, 2015; DeLoughery,
2017).
Hermayanti, D., Setiawan, M. and Nurdiana, H.
Improvement of Knowledge on Iron Deficiency Anemia and Its Prevention among Bustanul Athfal Teachers in Malang.
DOI: 10.5220/0009127302010204
In Proceedings of the 2nd Health Science International Conference (HSIC 2019), pages 201-204
ISBN: 978-989-758-462-6
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
201

Iron deficiency anemia will only occur when the
body's iron reserves are very low and not enough to
produce erythrocyte cells. The etiology of iron
deficiency anemia can occur due to low iron in diet,
blood loss (excessive menstrual blood, blood loss
after childbirth, diseases that cause chronic blood
loss) and low absorption of iron in the intestine
(Chron's disease, gastric bypass, worms, or the
presence of substances that inhibit iron absorption in
food (Harper et al., 2007; Jimenez, Kulnigg-Dabsch
and Gasche, 2015).
The initial symptoms of iron deficiency, often in
the form of weakness and restless leg syndrome. The
anemia will occur if the iron deficiency continues and
a negative balance arises between iron input and its
use. (Jimenez, 2015). The symptoms of anemia may
not be specified in the form of paleness, fatigue,
dizziness, sensitivity to light, shortness of breath,
anorexia, and headache (DeLoughery, 2017; Wong,
2017). There are also symptoms such as brittle and
jagged nails (koilonikia), mouth sores (angular
ciliosis), red and swollen tongue (glossitis), abnormal
appetite (pica), thinning hair, pharyngeal looking like
a nest (Patrson-Kelly syndrome) (Reynolds et al.,
1968; Korman, 1990; Borgna-Pignatti and Zanella,
2016)
The management of iron deficiency anemia
depends on their etiology (Goddard et al., 2011;
Pavord et al., 2012). It is necessary to manage the
underlying primary disease, provide iron
supplements, a diet of rich iron-containing foods, and
avoid consuming food along with other foods that
contain other ingredients that inhibit iron absorption
(Harper et al., 2007; Jimenez, Kulnigg-Dabsch and
Gasche, 2015)
Iron is a mineral that is very important in the
synthesis of hemoglobin in erythrocytes. Iron in food
from animal sources (home iron) is two to three times
higher absorbed by the intestine than non-home iron
(Verena T, 2017; Kaufman C, 2016). Some of the best
sources of iron are lean beef, oysters, chicken, and
turkey. Although iron absorption from plant sources
is lower, consumption of iron-rich plants can be
combined with vitamin C to increase iron absorption.
Some plants that are rich in iron are: nuts, tofu, baked
potatoes, cashews, dark green vegetables like
spinach, fortified cereals, fortified wheat bread
(Zimmermann and Hurrell, 2007)
Some foods can inhibit iron absorption, so it is
recommended to eat it not at the same time or not
close to the time with food sources of iron. These
foods include: foods that contain phytate or phytic
acid are found in grains, cereals, soybeans, and nuts,
foods that are high in calcium, such as in dairy
products and calcium supplements, and foods that
contain polyphenols, such as tea and coffee (Hurrell,
2009).
The iron deficiency anemia caused by dietary
factors can be prevented by consuming food in a
balanced composition and consuming iron-based
foods. The combination of vegetable food sources of
iron with vitamin C also prevents iron deficiency by
increasing its absorption capacity. An example is a
combination of spinach with lemon juice, fortified
cereals with berries, etc. (Zimmermann and Hurrell,
2007; Hurrell, 2009). Another prevention is to avoid
consumption together or in the close time meal
between food sources of iron and those that inhibit
absorption such as food from dairy products, or coffee
(Zimmermann and Hurrell, 2007; Hurrell, 2009).
2 METHODS
The study was conducted at the Busthanul Athfal
Aisyiyah Malang Teachers Association, after being
given training in knowledge and prevention of iron
deficiency, followed by pretest and posttest. Data
were analyzed using a comparative pairing t-test.
3 RESULTS AND DISCUSSION
The training was held on February 26, 2019, at TK
Aisyiyah Busthanul Athfal X, Jl. Manyar 29 Malang.
Sixty-three respondents attended it, but 46
respondents only filled the questionnaire. The pre-test
average value was 47.8, and the test post was 75.2. T-
test results 0,000 (p <0.05). The pre-test value appears
low and increases after training. The results show a
significant increase in respondents’ knowledge.
From the study, respondents were mostly aware of
the causes of iron deficiency anemia. After training,
the respondents who answered incorrectly declined
from 6.5% to 2.2%. The respondents were not aware
of the most frequent age group affected by iron
deficiency anemia, but after training those who
answered incorrectly appeared to decline from 95.7%
to 87%. The respondents were less aware of
symptoms of iron-deficiency anemia. After training,
there was an increase from 69.6% to 91.3%. Most
respondents did not know about foods that contain a
lot of iron (91.3%). After training, those who did not
know were reduced (21.7%). Respondents who knew
the cause of iron deficiency anemia after training
78.3%.
HSIC 2019 - The Health Science International Conference
202
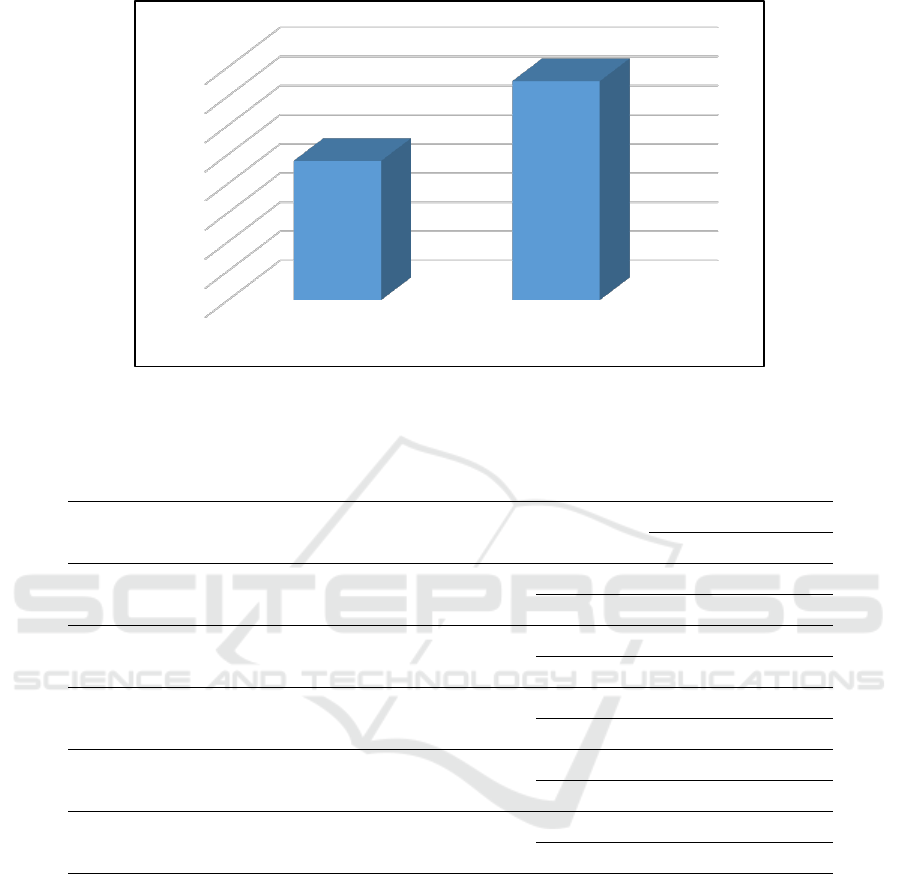
Figure 1: Chart of average pretest and post-test value
Table 1: Pretest and posttest questionnaire answer.
Question
Answer (%)
Wrong
Right
What cause of iron deficiency anemia?
Pretest
6,5
93,5
Posttest
2,2
97,8
What is the common age group with iron deficiency anemia
Pretest
95,7
4,3
Posttest
87
13
What is the symptom of iron deficiency anemia?
Pretest
30,4
69,6
Posttest
8,7
91,3
What food is the most contain a lot of iron?
Pretest
91,3
8,7
Posttest
21,7
78,3
What food can inhibit iron absorption
Pretest
34,8
65,2
Posttest
2,2
97,8
Respondents who knew the food that could inhibit
iron absorption, only 65.2% increased to 97.8% after
training. After the training, it appeared that
respondents became more aware of the symptoms of
iron deficiency anemia, the types of foods that contain
a lot of iron, and foods that inhibit iron absorption.
However, respondents were still not aware of the
most frequent group affected by anemia, and possibly
the respondents were not in a state of full
concentration (Goddard et al., 2011; Jimenez,
Kulnigg-Dabsch and Gasche, 2015).
4 CONCLUSIONS
The early knowledge of Malang Aisyiyah Busthanul
Athfal Teacher about iron deficiency anemia and its
prevention is still low. After the training activities,
there was an increase in knowledge about iron
deficiency anemia and its prevention. It is necessary
to feedback to the respondents regarding the results
of the questionnaire about the most frequent groups
that have this disease, so that they know and are more
aware to prevent iron deficiency anemia in their
students.
0
10
20
30
40
50
60
70
80
Pre-test Post-test
Improvement of Knowledge on Iron Deficiency Anemia and Its Prevention among Bustanul Athfal Teachers in Malang
203

REFERENCES
Borgna-Pignatti, C. and Zanella, S. (2016) ‘Pica as a
manifestation of iron deficiency,’ Expert
Review of Hematology. doi:
10.1080/17474086.2016.1245136.
DeLoughery, T. G. (2017) ‘Iron Deficiency Anemia,’
Medical Clinics of North America. doi:
10.1016/j.mcna.2016.09.004.
Goddard, A. F. et al. (2011) ‘Guidelines for the
management of iron deficiency anaemia’, Gut.
doi: 10.1136/gut.2010.228874.
Harper, J. W. et al. (2007) ‘Anemia in celiac disease
is multifactorial in etiology’, American
Journal of Hematology. doi:
10.1002/ajh.20996.
Hurrell, R. F. (2009) ‘Preventing Iron Deficiency
Through Food Fortification’, Nutrition
Reviews. doi: 10.1111/j.1753-
4887.1997.tb01608.x.
Jimenez, K., Kulnigg-Dabsch, S. and Gasche, C.
(2015) ‘Management of iron deficiency
Anemia’, Gastroenterology and Hepatology.
doi: 10.1016/S1769-7344(11)70351-1.
Kementrian Kesehatan Republik Indonesia (2019)
Laporan Nasional Riskesdas 2018, Riskesdas
2018.
Korman, S. H. (1990) ‘Pica as a presenting symptom
in childhood celiac disease’, American
Journal of Clinical Nutrition. doi:
10.1093/ajcn/51.2.139.
Pavord, S. et al. (2012) ‘UK guidelines on the
management of iron deficiency in pregnancy’,
British Journal of Haematology. doi:
10.1111/j.1365-2141.2011.09012.x.
Reynolds, R. D. et al. (1968) ‘Pagophagia and iron
deficiency anemia.’, Annals of internal
medicine. doi: 10.7326/0003-4819-69-3-435.
WHO et al. (2011) ‘Prevalence of iron deficiency and
iron deficiency anemia among females at
university stage’, Journal of the Pakistan
Medical Association. doi: 10.5005/jp-
journals-10006-1177.
Wong, C. (2017) ‘Iron deficiency anaemia’,
Paediatrics, and Child Health (United
Kingdom). doi: 10.1016/j.paed.2017.08.004.
World Health Organization (2015) The global
prevalence of anaemia in 2011, WHO.
Zimmermann, M. B. and Hurrell, R. F. (2007)
‘Nutritional iron deficiency’, Lancet. doi:
10.1016/S0140-6736(07)61235-5.
HSIC 2019 - The Health Science International Conference
204
