
An Integrated Framework for Social Contribution of Diabetes Self-care
Management Application
Zul Indra, Liza Trisnawati and Luluk Elvitaria
Departement of Informatics Engineering, Abdurrab University, Pekanbaru, Indonesia
Keywords:
Diabetes Mellitus, Diabetes Self-care Management (DSCM), Web Application.
Abstract:
Diabetes mellitus (DM) has becoming a critical health problem due to number of mortality. This disease will
affect the entire life of diabetic with its biological, psychological and social effects. However, there is no
known cure for this chronic disease. Diabetics can only reduce the complications that arise by taking certain
measures such to keep the blood glucose levels as close to normal as possible. The goal to keep the blood
glucose levels as close to normal requires the involvement of diabetics by diabetes self-care management
(DSCM). However, successful treatment for diabetics is not only depending on patient’s role in the care of
their diabetes but also requires family support. This research proposes an integrated DSCM application which
is enriched of social contribution feature since the DSCM application which accommodates the involvement of
diabetics’ family (social contribution) is still scarce. This proposed DSCM is aimed to allow family member
of diabetics to encourage them to keep their blood glucose levels as close to normal and enabling the doctors
to be actively involved in helping diabetics in managing their lifestyle.
1 INTRODUCTION
Diabetes mellitus (DM) has becoming a critical health
problem due to number of mortality. In 2011, the
International Diabetes Federation (IDF) claimed that
every year 4 million people die of diabetes with an av-
erage of one person dying every 7 seconds (Alrahbi,
2014). It has been estimated that 382 million people
in the world had DM, with more than 90% of them are
type 2 diabetic (Thojampa, 2019). In addition, based
on The World Health Organization report, the number
of people with diabetes has risen from 108 million to
422 million in just 34 years. This number of is ex-
pected to increase to about 439 million in 2030, where
69% of this number is estimated to occur in develop-
ing countries (Shaw et al., 2010). Therefore in 2014,
the World Health Organization (WHO) declared that
diabetes is one of most serious disease and a costly
health condition around the world(Association et al.,
2014).
As a chronic disease, diabetics will experience
various complications in their daily lives. This dis-
ease will affects the entire life of diabetic with its
biological, psychological and social effects (Mankan
et al., 2017). As an example, diabetics have a greater
risk of cardiovascular disease, eye or kidney disease,
and even reduced life expectancy compared to normal
people. In terms of psychological problems, sufferers
will experience a loss of life pleasure because they
lose the confidence to live independently and become
discouraged in living life. Furthermore, they have to
maintain a planned care throughout their lives and re-
ceive professional help from time to time.
Unfortunately, to date, there is no cure for this
chronic disease. Diabetics can only reduce the com-
plications that arise by taking certain measures such
to keep the blood glucose levels as close to normal as
possible (Syaifuddin and Anbananthen, 2013). Effec-
tive control of diabetes depends on self- monitoring
and self-care activities such as blood glucose moni-
toring, appropriate diet and nutrition, exercise regi-
men and medication administration strategies. Also,
individuals have to keep track of their overall health
record a holistic approach instead of only monitoring
their blood glucose reading.
However, the goal to keep the blood glucose lev-
els as close to normal cannot be achieved without in-
volvement of patients in the management plan. This
involvement occurs through diabetes self-care man-
agement (DSCM) with patients assuming an indepen-
dent role in the care of their diabetes. In addition,
successful treatment for diabetics is not only depend
on patients role in the care of their diabetes but also
requires family support a good relationship with the
68
Indra, Z., Trisnawati, L. and Elvitaria, L.
An Integrated Framework for Social Contribution of Diabetes Self-care Management Application.
DOI: 10.5220/0009106100680073
In Proceedings of the Second International Conference on Science, Engineering and Technology (ICoSET 2019), pages 68-73
ISBN: 978-989-758-463-3
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

diabetes care team, including open communication
and easy access to care, is essential for success (Sil-
verstein, 2014). This research proposes an integrated
personal health record which allow family member of
diabetics to contribute in order to keep the blood glu-
cose levels of diabetics as normal as possible.
2 LITERATURE REVIEW
DSCM can be defined as implementing actual per-
formance for self-care activities for those who suffer
from diabetes to manage their condition (Gharaibeh
et al., 2017). The main purposes of DSCM manage-
ment is to the glucose levels as close to normal as
possible by doing diet, performing physical activities,
monitoring blood glucose level, using of medications,
another self-care actions. The workings of DSCM is
to modify health behaviour by making changes to the
daily plan, if necessary, in accordance with the treat-
ment regimen and completion of self-care activities
such as following a regular diet and exercise plan,
independent monitoring of blood glucose levels, and
taking medication according to prescription (Khairnar
et al., 2019).
Nowadays, DSCM is considered a critical part of
diabetes management and has an important role in
helping diabetics to control the glycaemic and prevent
complications (Funnell, 2009). Furthermore, several
research has shown that DSCM can improve the qual-
ity of life of diabetics and contributed in prevent-
ing and lessening the severity of complications (Lorig
et al., 2009).
During the last five years, there are several re-
searches that have been done to develop DSCM ap-
plication. In 2014, an integrated model for cognitive
behavioural therapy for DSCM was proposed (Alanzi
et al., 2014). This proposed DSCM was intended
to implemented cognitive behavioural therapy for di-
abetics by using smartphone technology. In 2016,
another work for DSCM was performed by utilizing
the digital engagement concept (Burford et al., 2016).
This research attempted to empower the diabetics by
inviting them to participate in various digital activi-
ties for the management of their health condition. The
second work for DSCM research in 2016 was carried
out by developing an application which is called by
DiaHealth (Islam et al., 2016).
Based on the review of these several related
works, it can be inferred that there are many e-health
applications for diabetes management systems avail-
able, but most of these systems only focus on glucose
measurement levels and have not accommodated the
involvement of diabetics’ family (social contribution).
Therefore, this research proposes an integrated per-
sonal health record which is enriched of social contri-
bution feature. This feature is aimed to allow family
member of diabetics to encourage them to keep their
blood glucose levels as close to normal. Furthermore,
this proposed DSCM is enabling the doctors to be ac-
tively involved in helping diabetics in managing their
lifestyle.
3 SYSTEM REQUIREMENT
The DSCM application that is created is a web-based
application because it tends to be more flexible. Web-
based applications can be accessed through various
devices and various operating systems such as via
smartphones or tablets and others including smart
watches. It doesn’t matter whether users use Win-
dows, Linux, iOS, Mac OS, Blackberry, Android or
other devices; users can still use it only with a web
browser. Users simply open a web browser (for ex-
ample Firefox or Google Chrome) which then points
that web browser to the DSCM application URL to
use this DSCM application.
In addition, users can also access this applica-
tion through all the devices they have without hav-
ing to install it first on each of these devices. This
of course will make it easier for users who tend to
have multiple devices at once or change devices fre-
quently. As for the website interface, DSCM appli-
cation uses a bootstrap framework which is known as
one of the best website front-end framework. By us-
ing this bootstrap framework, the DSCM application
becomes more responsive and can adjust its appear-
ance according to the devices that access it. How-
ever, to use this website-based application, users do
not need hardware with strong specifications because
all applications are placed on the server side rather
than on the client side.
4 FEATURE OF PROPOSED
DSCM APPLICATION
Based on literature study that has been conducted, this
DSCM application is designed to have 5 main mod-
ules namely personal health record, knowledge base
and extraction, intelligent suggestion, notification and
reminder and social contribution.
As seen in the figure 2, the DSCM application is
divided into two levels of users, namely the level of
diabetics and social (family members and internists)
who have different access rights. Diabetic Users will
An Integrated Framework for Social Contribution of Diabetes Self-care Management Application
69

Figure 1: Module of Proposed DSCM
Figure 2: Context Diagram of Proposed DSCM
be given the right to access the blood sugar level data
input features, input insulin data, input exercise data
and obtain a profile of their health records. In addition
they will also be given a notification to remind them
to routinely check (input) blood sugar level data, diet
advice and also advice on physical activity. For social
level user, they will be given access to the health pro-
file of diabetics, get notifications from the system and
provide encouragement so that diabetics can manage
their lifestyle. Moreover by using this DSCM, it is
expected the internist can get a health picture of the
patient real time and provide better treatment.
4.1 Personal Health Record
In this proposed DSCM application, the Personal
Health Record Module consists of two main parts,
namely data input section and the health profile of
diabetics section. There are several data which is
inputted by users into personal health records such
as blood sugar levels, insulin intake, exercise activi-
ties and diet activities. All these records of data will
be processed by the Knowledge Base and Extraction
module and then delivered to diabetics in the form of
suggestions.
Figure 3: Homescreen of Proposed DSCM
DSCM application will give suggestion to diabet-
ics regarding physical activity and a better and appro-
priate diet in order to maintain their blood sugar levels
as close to normal. All data that has been inputted by
the diabetic user will be displayed by this DSCM ap-
plication on the health profile display page so that the
related users, diabetics and family members of the in-
ternist, can monitor the patient’s health condition real
time.
Figure 4: Profile of Diabetic
Figure 5: Graph Representation for Glucose and Blood
Pressure Level
4.2 Knowledge Base and Extraction
This module has a task to process raw data which
are inputted by users where concepts of data min-
ing and machine learning are utilized in this mod-
ule. So that the presence of the Knowledge Base and
ICoSET 2019 - The Second International Conference on Science, Engineering and Technology
70
Extraction module makes this DSCM application be-
come smarter as this DSCM will adjust itself, in terms
of giving advice and notifications, according to the
health profile of each user. For example, based on the
results of the blood sugar level record the DSCM ap-
plication will look at the blood sugar level trend of
diabetics then analyse the causes of elevated or de-
creased blood sugar levels.
The results of this analysis will be displayed and
can be accessed by the user in personal health record
module. In addition, the results of this analysis will be
further processed in the intelligent suggestion module
to be able to provide more suitable treatments related
to diet, physical activity and so on.
4.3 Intelligent Suggestion
As explained in the knowledge base and extraction
module, this developed DSCM application will intel-
ligently provide advice according to the health profile
of each diabetic. Thus the advice which is delivered
will be more in accordance. For example, based on
the results of the analysis that has been carried out
in the knowledge base and extraction, users will get
advice about physical activity and diet control that is
more in line with their habits in order to make it easier
for them to keep their blood sugar levels normal.
Figure 6: Sample of Intelligent Suggestion
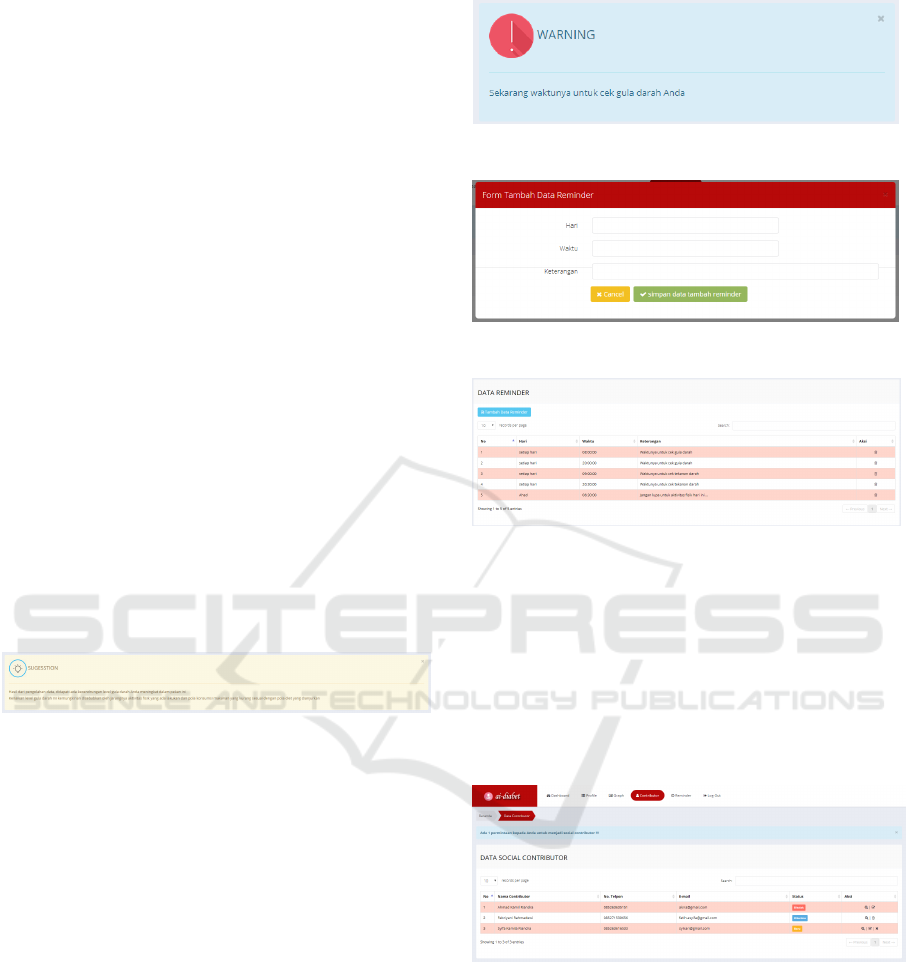
4.4 Notification and Reminder
This module is an important module in the DSCM
application that has the task of giving reminders to
users. Patients will be reminded to record their health
data such as their blood sugar level and regular phys-
ical activity. Due to diabetics are tend to forget or
lazy to record their health data because they consider
this troublesome. This module will routinely check
whether the patient has recorded their health data. If
diabetics have not yet recorded the data, the DSCM
application through this module will send notifica-
tions to users in order to remind diabetics to imme-
diately record their health data.
4.5 Social Contribution
As explained earlier, another factor in the success of
treating diabetics is the contribution of family mem-
bers. This module is intended to be a medium for
Figure 7: Sample of Intelligent Suggestion
Figure 8: Adding of Reminder Notification
Figure 9: Reminder Data
family members and doctors to be actively involved in
helping diabetics in managing their lifestyle. Through
this module, they can easily monitor the health condi-
tions of diabetic real time and encourage them to be
able to regulate their lifestyle such as reminding them
to check their blood sugar levels, follow a healthy
diet, and do physical activities and so on.
Figure 10: List of Social Contributor
5 CONCLUSIONS
Successful treatment for diabetics is not only depend
on patients role in the care of their diabetes but also
requires family support to encourage them to keep the
blood glucose levels of diabetics as normal as possi-
ble. This research proposes an integrated DSCM ap-
plication which allow family member of diabetics to
An Integrated Framework for Social Contribution of Diabetes Self-care Management Application
71
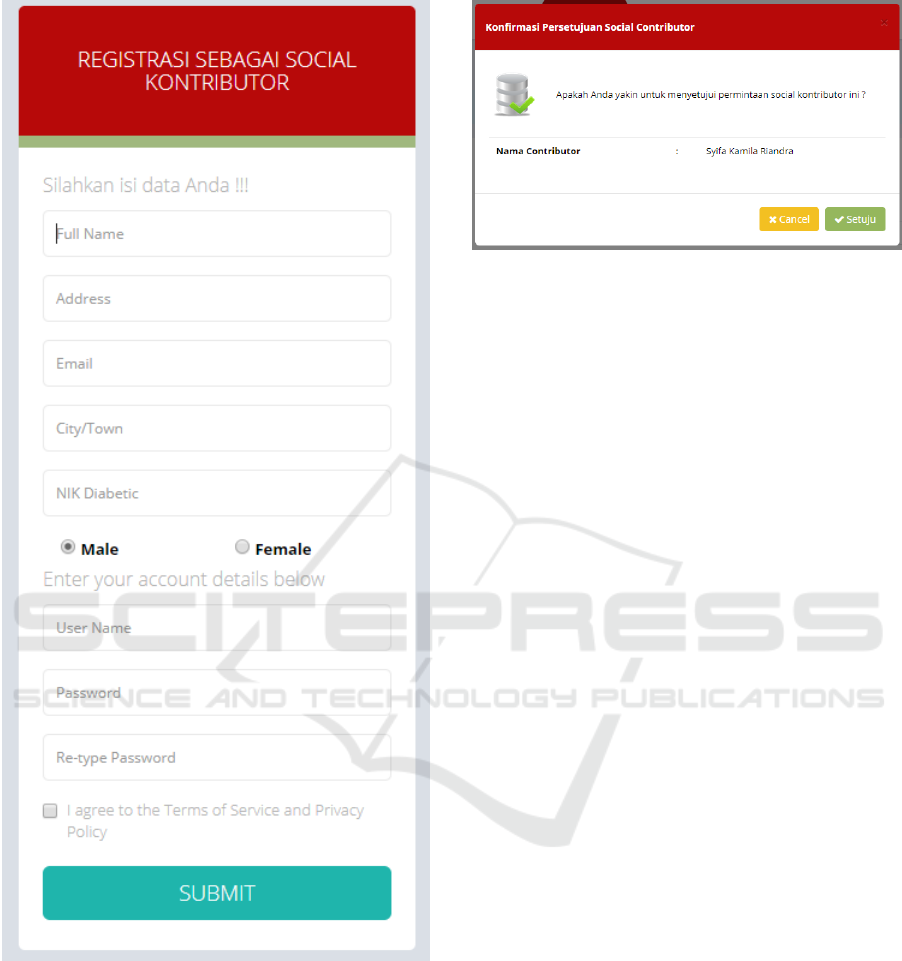
Figure 11: Form of Social Contributor Registration
encourage them to manage their lifestyle and enabling
the doctors to be actively involved in helping diabet-
ics real time. This research is still in the initial stages
in terms of identifying what modules are needed in
the development of DSCM applications. Further re-
search needs to be carried out to find out how much
the influence of proposed DSCM application in order
to ease the treatment of diabetics.
Figure 12: Approval for Social Contributor
REFERENCES
Alanzi, T., Istepanian, R. S., and Philip, N. (2014). An in-
tegrated model for cognitive behavioural therapy for
mobile diabetes self-management system. In 2014
36th Annual International Conference of the IEEE
Engineering in Medicine and Biology Society, pages
5393–5396. IEEE.
Alrahbi, H. (2014). Diabetes self-management (dsm) in
omani with type-2 diabetes. International Journal of
Nursing Sciences, 1(4):352–359.
Association, A. D. et al. (2014). Standards of medical
care in diabetes—2014. Diabetes care, 37(Supple-
ment 1):S14–S80.
Burford, S., Park, S., Carpenter, M., Dawda, P., and Burns,
J. (2016). Digital engagement, self-management, and
shifting the locus of control: A mhealth program for
people with type 2 diabetes. In 2016 49th Hawaii In-
ternational Conference on System Sciences (HICSS),
pages 3369–3378. IEEE.
Funnell, M. (2009). Bro n tl, childs bp, haas lb, hose gm,
jensen b, et al. National standards for dia etes self-
management education. Dia etes Care.
Gharaibeh, B., Al-Smadi, A. M., and Boyle, D. (2017).
Psychometric properties and characteristics of the di-
abetes self management scale. International journal
of nursing sciences, 4(3):252–259.
Islam, M. A., Alvi, H. N., and Al Mamun, K. A. (2016). Di-
ahealth: A smart app for complete diabetes lifestyle
management. In 2016 International Conference on
Medical Engineering, Health Informatics and Tech-
nology (MediTec), pages 1–6. IEEE.
Khairnar, R., Kamal, K. M., Giannetti, V., Dwibedi, N.,
and McConaha, J. (2019). Barriers and facilitators to
diabetes self-management in a primary care setting–
patient perspectives. Research in Social and Adminis-
trative Pharmacy, 15(3):279–286.
Lorig, K., Ritter, P. L., Villa, F. J., and Armas, J.
(2009). Community-based peer-led diabetes self-
management. The Diabetes Educator, 35(4):641–651.
Mankan, T., Erci, B., Turan, G. B., and Akt
¨
urk,
¨
U. (2017).
Turkish validity and reliability of the diabetes self-
efficacy scale. International journal of nursing sci-
ences, 4(3):239–243.
ICoSET 2019 - The Second International Conference on Science, Engineering and Technology
72

Shaw, J. E., Sicree, R. A., and Zimmet, P. Z. (2010).
Global estimates of the prevalence of diabetes for
2010 and 2030. Diabetes research and clinical prac-
tice, 87(1):4–14.
Silverstein, J. H. (2014). Can we reduce barriers to diabetes
care? The Journal of pediatrics, 164(6):1245–1247.
Syaifuddin, M. and Anbananthen, K. S. M. (2013). Frame-
work: Diabetes management system. In IMPACT-
2013, pages 112–116. IEEE.
Thojampa, S. (2019). Knowledge and self-care manage-
ment of the uncontrolled diabetes patients. Interna-
tional Journal of Africa Nursing Sciences, 10:1–5.
An Integrated Framework for Social Contribution of Diabetes Self-care Management Application
73
