
Effects of Exercise Training on Forced Expiratory Flow in
Individuals with Spinal Cord Injury with Prone Positioning:
A Serial Case Report
Ayu Amalia Utami Putri
1
, S. C. Widjanantie
2
, R. E. Pakasi
3
1
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo Hospital,
University of Indonesia, Jakarta, Indonesia
2
Cardiorespiratory Division, Department of Physical Medicine and Rehabilitation, Persahabatan Hospital,
University of Indonesia, Jakarta, Indonesia
3
Neuromuscular Division, Department of Physical Medicine and Rehabilitation, Fatmawati Hospital,
University of Indonesia, Jakarta, Indonesia
Keywords: Exercise Training, Forced Expiratory Flow, Spinal Cord Injury, Prone Position.
Abstract: Two Spinal Cord Injury (SCI) patients with the diagnosis of thoracic level Asia Impairment Scale (AIS) A
chronic phase were re-hospitalized. A 23-year-old male with accompanying problem of multiple pressure
sores, deep vein thrombosis (DVT), and anemia; and a 13-year-old-female with accompanying problem of
pressure sores and anemia. Debridement and flap surgeries were performed in treating existing pressure
sores. Six weeks of tailored-made rehabilitation program were given including the prone positioning in the
midst of the ongoing program. Each subject completed peak cough flow (PCF), peak flow rate (PFR), and
Spinal Cord independence Measure (SCIM) for respiratory function-interview based. Re-admitted chronic
SCI patients had exercise tolerance which put them at risk of pulmonary complications. A good exercise
tolerance will support the respiratory function by increasing vital capacity (VC), thus enhancing cough
ability as a protection of respiratory system. Prone position also has certain advantages that can still be
conducted by SCI patients in preserving respiratory capacity. Conclusions: Good exercise tolerance along
with good airway cleansing technique is an effective way to prevent complications of the respiratory system
in chronic SCI patients who must be in a prone position for a certain period of time.
1 CASE DIAGNOSIS
Case I, A 13-year-old female patient with chronic
phase of high paraplegia (T3) SCI is being admitted
to hospital due to multiple pressure sores and
anemia. Case II, H, 23-year-old male, suffered from
chronic SCI of lower thoracis (T9) re-admitted to
hospital due to DVT, multiple pressure sores, and
anemia. Both patients needed to be maintained in
prone position due to debridement and flap surgery
performed in treating existing multiple pressure
sores while rehabilitation program remains
continued.
2 CASE DESCRIPTION
Case I, A 13-year-old female patient with chronic
phase of high paraplegia (T3) SCI is being admitted
to hospital due to multiple pressure sores and
anemia, due to limited activity for past 1.5 years.
Patient had no history of pulmonary infection before
admitted to hospital. For the physical examination,
she has inadequate cough ability, and was found to
be low endurance cardiorespiratory due to inability
to maintain active upright position. One week after
admitted to hospital she had worsening anemia
which was thought to be due to worsening pressure
sores. She was then underwent a debridement and
flap surgery procedure. She had been doing active
rehabilitation consist of proper positioning,
breathing exercise with chest splinting, advanced
wheeling to increase cardiorespiratory endurance,
Putri, A., Widjanantie, S. and Pakasi, R.
Effects of Exercise Training on Forced Expiratory Flow in Individuals with Spinal Cord Injury with Prone Positioning: A Serial Case Report.
DOI: 10.5220/0009090503430346
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 343-346
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
343
and transfer techniques prior to surgery, but she was
unable to continue training due to worsening anemia
for the next 2 weeks. Blood cultures and wound
swabs were carried out, and she had been treated
with specific antibiotics. She was then scheduled for
debridement and flap surgery. After procedures, she
was ordered to be in prone position for at least 2
weeks. While in the prone position, she can only do
expiratory muscle training using Positive Expiratory
Pressure (PEP) device. PCF and PFR measurements
were taken prior to the exercise (baseline), before
the prone position (P1), and after the prone position
(P2). (table 1).
Case II, H, 23-year-old male, suffered from
chronic SCI of lower thoracis (T9) re-admitted to
hospital due to DVT, multiple pressure sores, and
anemia. Patient had no previous history of
pulmonary infections. After medically stable, he was
given training to improve cardiorespiratory
endurance. He was also scheduled for debridement
and flap surgery, and was ordered to be in prone
position for at least 2 weeks. Before being in a prone
position, the patient had gone through an upper
extremity strengthening exercise program and was
capable of wheeling advanced. PCF and PFR
measurements were taken prior to the exercise
(baseline), before the prone position (P1), and after
the prone position (P2). (table 1).
3 RESULTS
Exercises provided during the 6 weeks of hospital
treatment include proper positioning, breathing
exercise technique, respiratory muscles training,
upper limb strengthening include body weight lifting
exercise, aerobic exercise to increase
cardiorespiratory endurance, and transfer technique.
All exercises were tailored-made to patient’s needs.
Case I, patient had done very well for the first
two weeks, but entering the third week, patient had
fever and anemia, her pressure sore started to build a
tunnel around the first wound and actively bleed,
thus she had to stop exercising for a while. On the
fourth week, she had to do the debridement and flap
surgery that required prone position for at least 2
weeks after the operation was performed. At that
time, she still hadn’t been able to lift the body using
the upper limbs strength, thus she only did exercises
using positive expiratory pressure (PEP) device
started with 30% dose of maximal expiratory
pressure (MEP) with a gradual increase. The results
obtained were increase in PCF and PFR at week 4
(P1) and at week 6 (P2) . No increase in SCIM score
for management sphincter and respiratory (table 2).
In case II, patient had already had a good
exercise capacity before starting the regiments. the
patient was able to do exercise regimen in the first 4
weeks of treatment in the form of strengthening the
muscles of the upper limbs and cardiorespiratory
endurance, so that after debridement and flap
surgery on the fifth week and the patient is required
to be in a prone position, he was able to continue the
strengthening exercise regimen that has been done
before, although he has not been able to continue
aerobic exercise due to limited space. The results
showed, the patient had an increase in PCF and PFR
in the fourth week before the prone position (P1),
and at the end of the sixth week after the prone
position lasted for 2 weeks (table 1). No increase in
SCIM score for management sphincter and
respiratory (table 2).
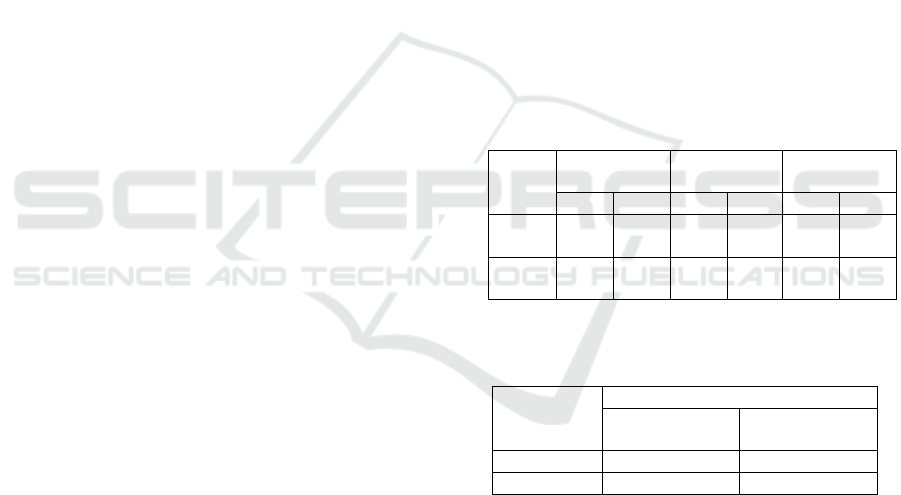
Table 1: Results of Peak Flow Meter (PFM) at baseline,
before prone positioning (P1), after prone positioning
(P2).
Table 2: Results of Spinal Cord Independence Measure for
sphincter management – bowel at baseline, and post
treatment (S1 (S0)).
Subject
SCIM
Baseline
(S0)
Post
(S1)
Case I 10 10
Case II 8 8
4 DISCUSSION
Pulmonary complications remain a major cause of
morbidity and mortality in SCI population. Injury to
the upper and lower thoracic cord may disrupts
function of the intercostal muscles, accessory
respiratory muscles, and abdominal muscles.
Patients may have ineffective cough and difficulty
clearing secretions which in turn predispose to
mucus retention, atelectasis and pulmonary
infections, and ultimately to significant morbidity
and mortality.
Baseline
(l/m)
P1
(l/m)
P2
(l/m)
PCF PFR PCF PFR PCF PFR
Case
I
110 130 140 160 150 170
Case
II
350 360 420 400 480 460
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
344

Ability to generate adequate cough is important
to protect respiratory functions in SCI patients. Peak
Cough Flow is the maximum flow recorded
immediately following opening of the glottis. This
leads to the rapid expulsive phase of a cough,
resulting from the sudden release of high intrapleural
and thoraco-abdominal pressures. To achieve a
functional PCF (to expectorate secretions) requires
at least 50% of vital capacity and sufficient thoraco-
abdominal pressure (in excess of 100 cmH
2
O) to
produce at least a flow of 270 l/m. In order to move
any mucus within the airways, PCF must exceed at
least 160l/m. Combination with sufficient expiratory
muscle strength is required to generate the required
thoraco-abdominal pressures (Anderson, 2005).
Both patients had been through rehabilitation
program for six weeks. The results corresponding to
the PCF and PFR before and after rehabilitation
program are described in Table 1. In case I, patient
experienced an increase in PCF and PFR during
active rehabilitation following training to improve
cardiorespiratory endurance, this is in line with
research by Houtte et al and Moro et al which
confirmed that respiratory muscle training tended to
improve expiratory muscle strength, vital capacity,
residual volume, and also increasing ventilation
efficiency in subjects with SCI (Moro et al, 2005).
She continues to train her expiratory muscles using
PEP. In case II, after the prone position is applied,
the patient is still able to do strengthening exercises
on the upper limb in the form of push up and weight
training for as long as 30 minutes/day, 5 days a
week. Patient wasn’t given training using PEP
because he have good PCF and PFR baselines (more
than 270 l/m).
Pulmonary function in SCI is mainly limited by
the weakness of respiratory muscles, therefore,
training of the remaining respiratory muscles in SCI
and the use of compensatory respiratory mechanism,
such as m. pectorals function for expiration may
improve pulmonary function (Houtte et al, 2006).
Prone position can also give benefit to respiratory
function by improving lung parenchyma mechanics
and arterial oxygenation, attenuating lung inflation
gradient, eliminating lung compression by the heart,
and make regional alveolar ventilation become more
homogenous resulting in reduction of alveolar
atelectasis and hyperinflation. Decreased atelectasis
and more uniform inflation may result in more
homogenous and increased average alveolar septal
tension (Metzelopoulos et al, 2005). The
gravitational gradient of intrapleural pressure is
suggested to be less in prone posture than supine.
Thus the gravitational distribution of ventilation is
expected to be more uniform prone, potentially
affecting regional ventilation-perfusion ratio
(Henderson et al, 2014).
In the supine position, there is predominance of
ventilation in the ventral area of the lung and
perfusion in the dorsal area of the lung, resulting in a
heterogeneous ventilation-perfusion ratio in various
lung areas. This is due to the influence of gravity on
the solid mass of the lung, pulmonary
vascularization and the transpulmonary gradient
associated with alveolar size. In contrast to the
pronation position, the solid lung mass and blood
flow are distributed to the ventral by the influence of
gravity, resulting in a more homogeneous
ventilation-perfusion ratio in the ventral and dorsal
areas so as to improve gas exchange and increase
oxygenation (Glenny et al, 2011).
Patients with prone positioning experience a
more even distribution of tidal volume because the
vertical gradient of pleural pressure becomes more
negative in the dorsal portion of the lung. In the
pronation position, the pressure from the heart and
the abdominal cavity also decreases so that the lung
volume in the dorso-caudal region increases (Glenny
et al, 2011).
In the supine position, the size of the alveolar
will become more heterogeneous, where the size of
the alveolar from the non-dependent (ventral) to the
dependent (dorsal) area of the lung will become
smaller, thereby increasing the risk of atelectasis in
the lung-dependent area. In contrast to the pronation
position, alveolar size in the lung dependent area
will be greater due to the Slingky effect on lung
tissue, thus, alveolar size will become more
homogeneous while reducing the risk of atelectasis
(figure 1) (Hopkins et al, 2015).
Figure 1: Slinky effect.
5 CONCLUSIONS
Good exercise tolerance is required to maintain
activities level needed by SCI patients along with
good airway cleansing technique to prevent
Effects of Exercise Training on Forced Expiratory Flow in Individuals with Spinal Cord Injury with Prone Positioning: A Serial Case Report
345

complications of the respiratory system in chronic
SCI patients.
Prone position turns out to have benefits for both
SCI patients in Case I and Case II. In Case I, there is
no episodes respiratory tract infections during
treatment in the hospital despite having a minimum
PCF and PFR limits to be able to do good airway
clearance. In Case II, patient was still able to carry
out exercise activities while in the prone position,
and showed increasing PCF and PFR which are the
reflection of improving airway clearance ability.
REFERENCES
Anderson JL, Hasney KM, Beaumont NE. 2005.
Systematic review of techniques to enhance peak
cough flow and maintain vital capacity in
neuromuscular disease: the case for mechanical
insufflation–exsufflation. Phys Ther Rev. 10(1):25–33.
Houtte S Van, Vanlandewijck Y, Gosselink R. 2006.
Respiratory muscle training in persons with spinal
cord injury : A systematic review. 1886–95.
Moro DLF, Tordi N, Lonsdorfer E. 2005. Ventilation
Efficiency and Pulmonary Function After a
Wheelchair Interval-Training Program in Subjects
With. 86(August):1582–6.
Mentzelopoulos SD, Roussos C, Zakynthinos SG. 2005.
Prone position improves expiratory airway mechanics
in severe chronic bronchitis. 59–68.
Henderson AC, Sá RC, Theilmann RJ, Buxton RB, Prisk
GK, Hopkins SR, et al. 2014. The gravitational
distribution of ventilation-perfusion ratio is more
uniform in prone than supine posture in the normal
human lung The gravitational distribution of
ventilation-perfusion ratio is more uniform in prone
than supine posture in the normal human lung.
Glenny RW, Robertson HT. 2011. Spatial Distribution of
Ventilation and Perfusion : Mechanisms and
Regulation.1(January):373–95.
Hopkins SR, Henderson AC, Levin DL, Yamada K,
Buxton RB, Prisk GK, et al. 2015. Vertical gradients
in regional lung density and perfusion in the supine
human lung : the Slinky effect Vertical gradients in
regional lung density and perfusion in the supine
human lung : the Slinky effect. March 2007:240–8.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
346
