
Anatomy, Kinesiology, Pathomechanics, and Diagnosis
of Shoulder Impingement Symptomp
Tirza Z. Tamin
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo General Hospital,
Faculty of MeAdicine, University of Indonesia, Jakarta, Indonesia
tirzaediva.tamin@gmail.com
Keywords : Shoulder Impingement, Shoulder Problems, Early Diagnosis
Abstract : Musculoskeletal complaints with the highest prevalence of patients coming to the hospital one of which is
shoulder pain. Based on several studies the current prevalence of complaints of shoulder pain ranges from 7-
36% of the population. The most common cause of complaints of shoulder pain coming to the Orthopedic
clinic or Medical Rehabilitation is a patient with Shoulder Impingement Syndrome (SIS). Patients with SIS
will experience functional limitations making it difficult to do work as usual and difficult to lift weights
above the head. SIS that occurs continuously will become a functional disability and decreased quality of
life. Initial treatment in this case is given non-operatively, making rehabilitation the first choice as therapy.
1 INTRODUCTION
Shoulder pain is a common presenting complaint
from patients of all ages in daily clinical practice,
affecting approximately one-third of individuals
during their lifetime (Dong W et al, 2015). Such
pain may lead to the impairment of shoulder joint
function and to severe reduction in quality of life.
Shoulder impingement syndrome, which is defined
as the compression of the rotator cuff and the
subacromial bursa, is considered to be one of the
most common causes of shoulder pain and may be
cited as a contributing factor to shoulder pain in up
to 65% of cases (Garving et al, 2017). Shoulder
impingement is a clinical syndrome in which soft
tissues become painfully entrapped in the area of the
shoulder joint. Shoulder impingement has been
defined as compression and mechanical abrasion of
the rotator cuff structures as they pass beneath the
coracoacromial arch during elevation of the arm
(Dong W et al, 2015). In literature shoulder
impingement syndrome (SIS) is reported to be a
contributing factor between 48% and 65% of all
painful shoulder conditions (Burbank et al, 2008).
Different kinds of SIS are defined in literature
depending on the structures involved: subacromial
impingement syndrome (SAI), internal impingement
(IIM), and Sub-coracoid impingement (SC)
(Garving et al, 2017).
Charles Neer described subacromial
impingement as the compression and abrasion of
the bursal side of the rotator cuff beneath the
anterior acromion, and developed the anterior
acromioplasty as a treatment (Neer, 1983).
External impingement is now understood as a
much broader category than that described by
Neer, and could include compression or abrasion
of the cuff tendons or tendon of the long head of
the biceps brachii beneath any aspect of the
coracoacromial arc (Neer, 1983). The
coracoacromial arch includes not just the acromial
undersurface, but also the coracoacromial
ligament, and the undersurface of the
acromioclavicular (AC) joint (Garving et al,
2017).
2 DISCUSSION
2.1 Joints
The main function of the joints of the shoulder girdle
is to move the arm and hand into almost any position
in relation to the body. As a consequence, the
304
Tamin, T.
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp.
DOI: 10.5220/0009090003040315
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 304-315
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
shoulder joint is highly mobile, where stability takes
second place to mobility, as is evident from the
shape of the osseous structures: a large humeral head
lying on an almost flat scapular surface. Stability is
provided mainly by ligaments, tendons and muscles;
the bones and capsule are of secondary importance.
The function of the shoulder girdle requires an
optimal and integrated motion of several joints. In
fact, five ‘joints’ of importance to ‘shoulder’
function can be distinguished:
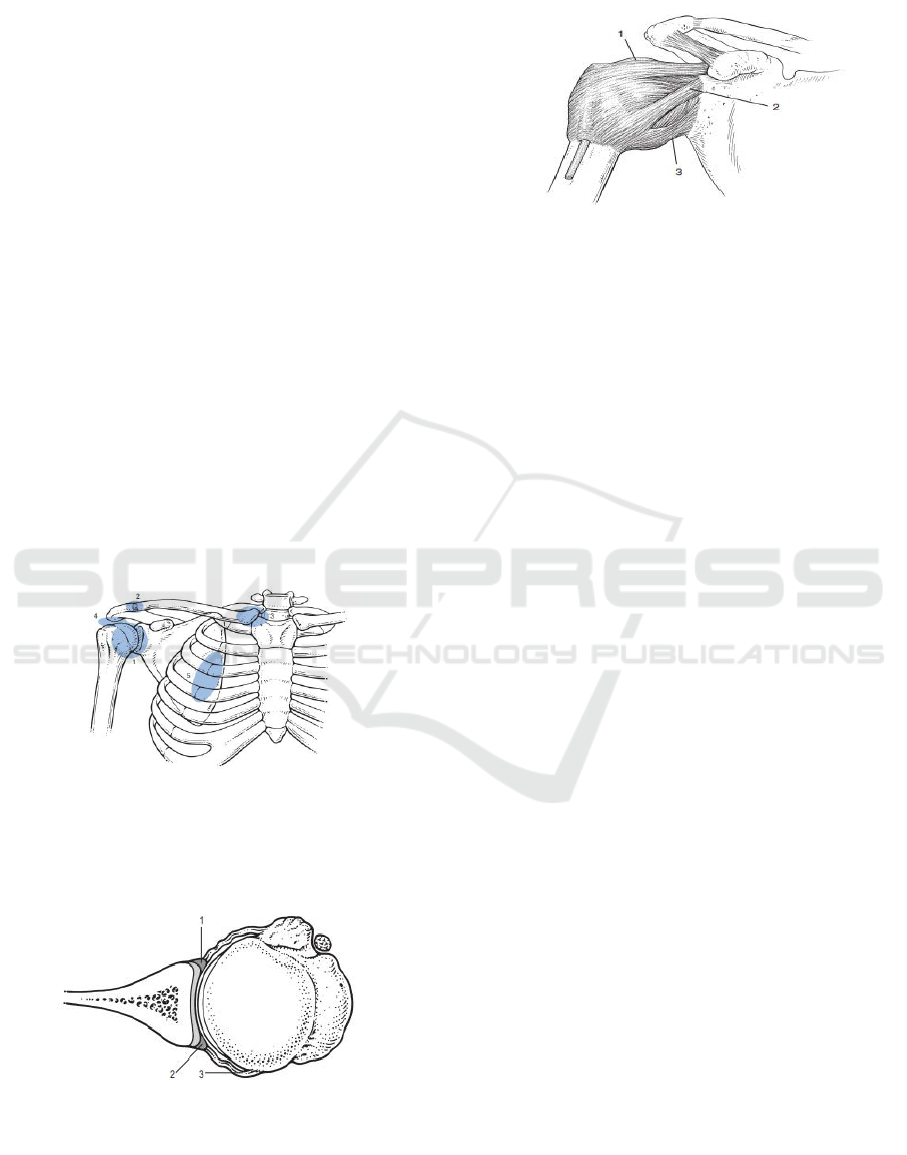
1. The glenohumeral joint
2. The acromioclavicular joint
3. The sternoclavicular joint
4. The subacromial joint or subacromial gliding
mechanism: the space between the
coracoacromial roof and the humeral head,
including both tubercles. This is the location of
the deep portion of the subdeltoid bursa
5. The scapulothoracic gliding mechanism: this
functional joint is formed by the anterior aspect
of the scapula gliding on the posterior thoracic
wall. Optimal mobility also requires an intact
neurological and muscular system.
5
2.1.1 Glenohumeral joint
Figure 3: The glenohumeral joint capsule and ligament:
1. Superior; 2. Medial, 3. Inferior (glenohumeral
ligaments).
The glenohumeral joint is a ball-and-socket between
humeral head and glenoid fossa. There is a
remarkable geometrical relationship between
glenoid and head which is responsible for the
considerable mobility of the joint but is also an
important predisposing factor to glenohumeral
instability. First, the large spherical head of the
humerus articulates against the small shallow
glenoid fossa of the scapula (only 25–30% of the
humeral head is covered by the glenoid surface).
Second, the bony surfaces of the joint are largely
incongruent (flat glenoid and round humerus).
However, the congruence is greatly restored by the
difference in cartilage thickness: glenoid cartilage is
found to be the thickest at the periphery and thinnest
centrally, whereas humeral articular cartilage is
thickest centrally and thinnest peripherally. This
leads to a uniform contact between humeral head
and glenoid surface throughout shoulder motion
(Rockwood et al, 2009).
The labrum is a fibrous structure that forms a
ring around the periphery of the glenoid. It further
contributes to stability of the joint by increasing the
depth of the glenoid socket, enlarging the surface
area and acting as a load-bearing structure for the
humeral head. The synovial membrane of the joint
capsule is mainly attached to the labrum, covering
its inner surface, and at the anatomical neck of the
humerus. The fibrous portion of the capsule is very
lax and has several recesses, depending on the
position of the arm. Very often adhesions form here.
The joint capsule is large, loose and redundant
allowing full and free range of motion of the
shoulder.
The rotator cuff and labrum are the
shoulder structures most vulnerable to
throwing injuries (Lin DJ et al, 2018).
Figure 2: Shoulder (glenohumeral) joint: 1.
Labrum, 2. Glenoid cartilage, 3. Shoulder
capsule.
Figure 1: A global view of five joints of
the shoulder girdle: 1. Glenohumeral
joint; 2. Acromioclavicular joint; 3.
Sternoclavicular joint; 4. Subacromial
joint or subacromial gliding mechanism;
5. Scapulothoracic gliding mechanism.
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
305
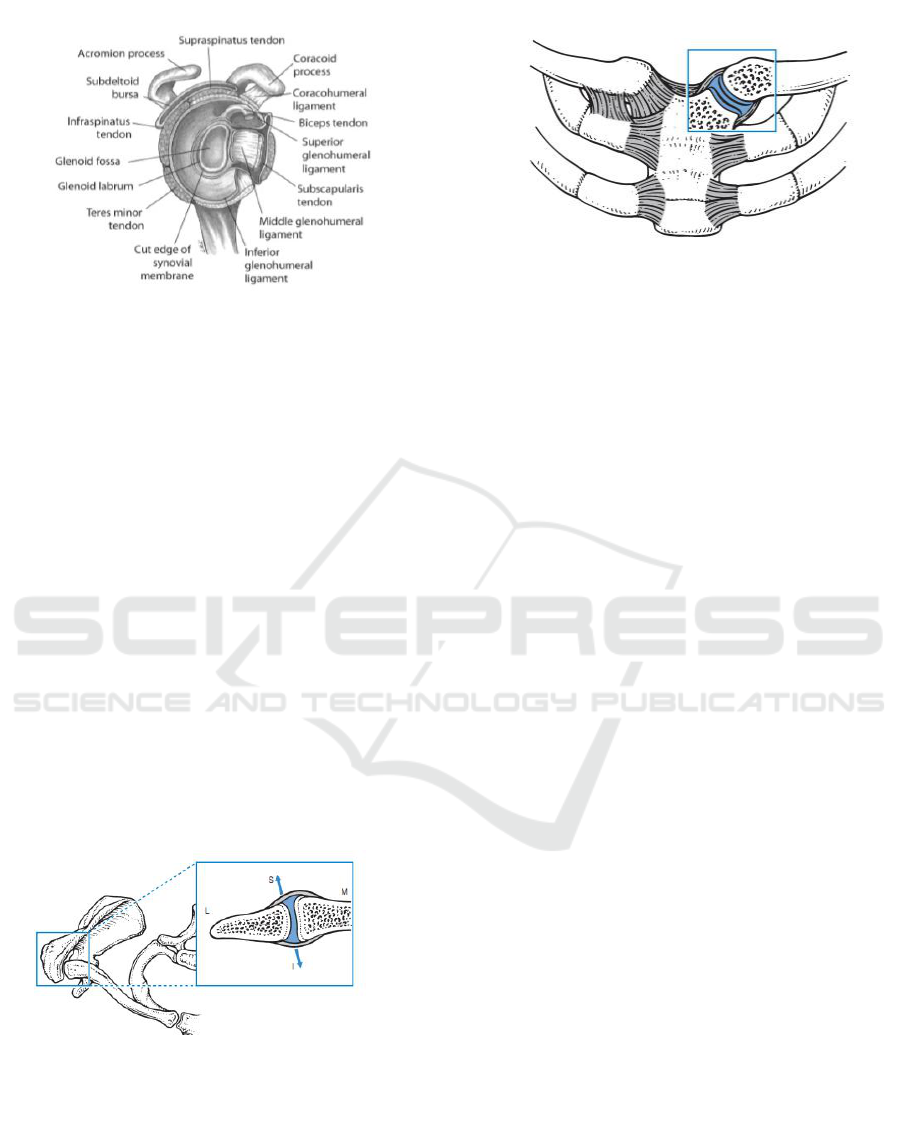
Figure 4: The glenohumeral joint.
At
the anterior portion of the capsule three local
reinforcements are present: the superior, medial and
inferior glenohumeral ligaments. These contribute,
together with the subscapularis, supraspinatus,
infraspinatus and teres minor muscles, to the
stability of the joint. By virtue of the blending of
their tendons with the glenohumeral capsule and
ligaments, selective contraction of the cuff muscles
can adjust the tension in these structures, producing
‘dynamic’ ligaments (Rockowood et al, 2009).
2.1.2 Acromioclavicular joint
The acromioclavicular joint is the only articulation
between the clavicle and the scapula. The
anteroposterior stability of the acromioclavicular
joint is controlled by the acromioclavicular
ligaments and the vertical stability is controlled by
coracoclavicular ligaments (conoid and trapezoid)
(Rockwood et al, 2009).
2.1.3 Sternoclavicular joint
Its the medial end of clavicle lies in contact with the
superolateral angle of the sternal manubrium and
with the medial part of the cartilage of the first rib to
form the sternoclavicular joint. In both the vertical
and anteroposterior dimensions, the clavicular
portion is larger than the opposing manubrium and
extends superiorly and posteriorly relative to the
sternum. The prominence of the clavicle enables its
palpation. The sternoclavicular joint is mobile along
all axes and almost every movement of the scapula
and the arm is associated with some movement at
this joint (Rockwood et al, 2009).
2.2 Muscles
The primary muscle group that supports the shoulder
joint is the rotator cuff muscles. The four rotator cuff
muscles are supraspinatus, infraspinatus, teres minor,
and subscapularis. Together the rotator cuff muscles
form a musculotendinous cuff as they insert on the
proximal humerus.
The rotator cuff muscles attach to the proximal
humerus anteriorly at the greater tuberosity. The
rotator cuff muscles provide considerable structural
support to the glenohumeral joint and keep the
humeral head in a firm position by articulating with
the scapula within the glenoid cavity. The muscles
of the chest also provide structural support to the
shoulder joint (Eovaldi et al, 2018).
2.2.1 Supraspinatus Muscle
The supraspinatus muscle functions by abduction of
the humerus up to 30 degrees, as well as to stabilize
the glenohumeral joint (Burbank et al, 2008).
Approximately 70% of the muscle fibers attach
to the intramuscular tendon, whereas 30% attach
directly to the extra muscular tendon. This muscle is
categorized as a circumpennate muscle (Eovaldi et al,
2018).
The supraspinatus is part of the force couple to
stabilize the glenohumeral joint by compression and
initializes elevation. Elevation in case of
supraspinatus paralysis requires more deltoid force,
Figure 6: The sternoclavicular joint.
Figure 5: Acromioclavicular joint;
S:Superior, I:Inferior, L:Lateral, M:Middle.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
306
but the other rotator cuff muscles are still able to
stabilize the humeral head sufficiently for full range
of motion. The suprascapular nerve (C4-6) supplies
innervation (Reyes et al, 1978).
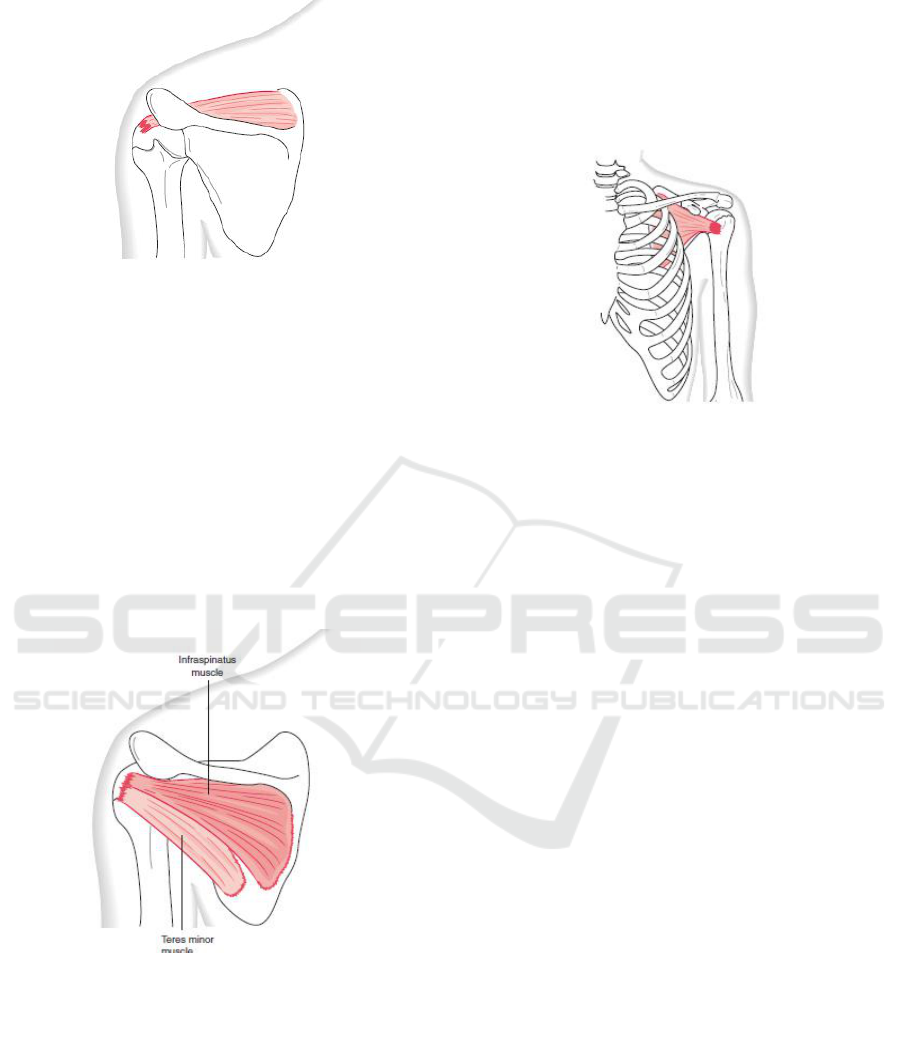
2.2.2 Infraspinatus Muscle
The infraspinatus muscle functions by externally
rotating the humerus and doing horizontal abduction
(Reyes et al, 1978).
2.2.3 Teres Minor Muscle
The Teres minor acts to externally rotate the
humerus and assists with abduction of the humerus.
Similar to the infraspinatus, this is a circumpennate
muscle with a single intramuscular tendon located in
the center of the muscle belly. The teres minor
muscle acts as stabilizer of the glenohumeral joint
by resisting posterior and superior translation and
generates 45% of the total external rotation force.
2.2.4 Subscapularis Muscle
As the only component of the anterior rotator cuff, it
stabilizes actively the glenohumeral joint by
resisting anterior and inferior translation and acts as
a strong internal rotator. It is considered to be a
passive stabilizer too, because of the dense collagen
structure of its tendon and its fusion with the middle
and inferior glenohumeral ligament (Eovaldi et al,
2018).
2.2.5 Trapezius Muscle
The only muscle which acts to depress the shoulder
is the lower trapezius, which is assisted by gravity in
the upright position. The function of the trapezius
muscle is both elevation and depression of the
shoulder depending on whether the upper or lower
muscle fibers are activated. When the entire
trapezius muscle contracts the fibers are
geometrically opposed, and the forces are balanced
resulting in no movement of the shoulder (Eovaldi et
al, 2017).
Figure 8: The Infraspinatus and Teres
Minor Muscle.
Figure 7. The Supraspinatus Muscle
Figure 9: The Subcapsularis Muscle
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
307
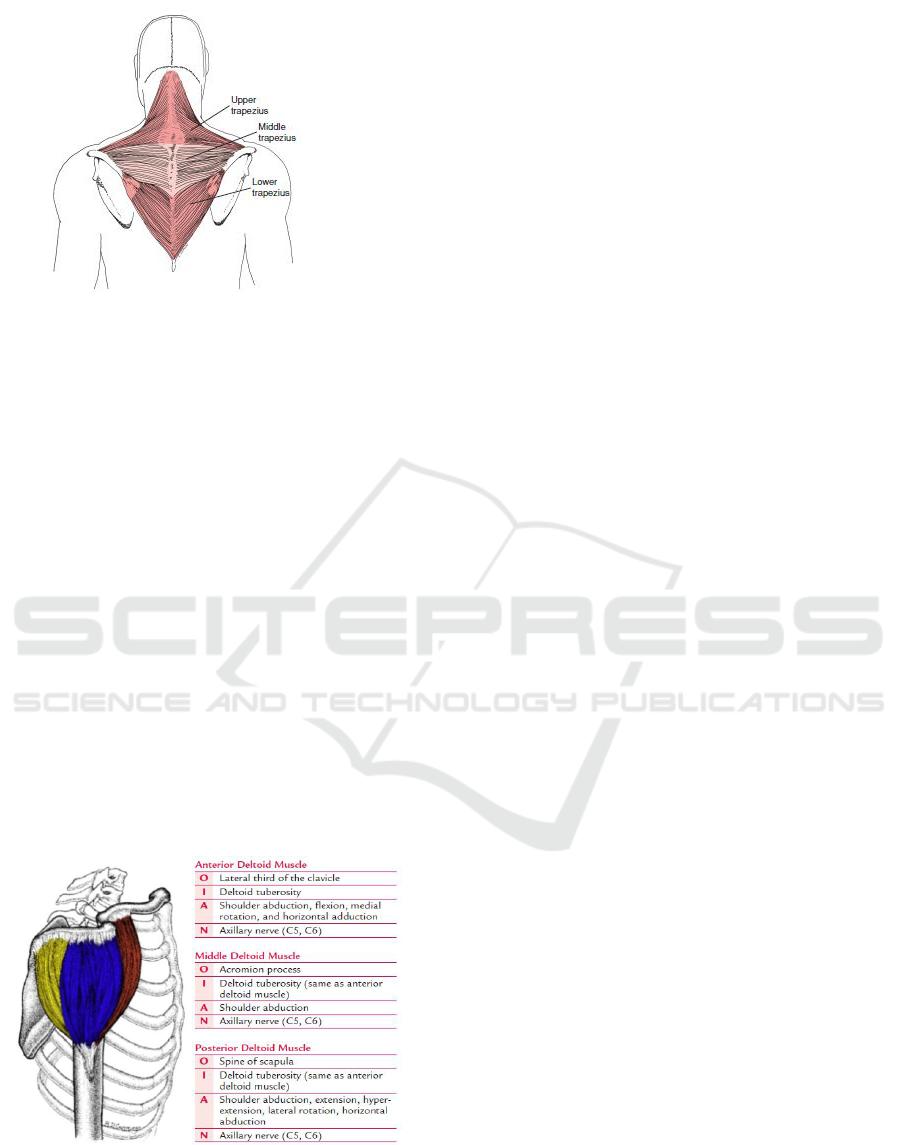
Figure 10: The Trapezius Muscle
2.2.6 Deltoid Muscle
The deltoid muscle overlies the shoulder
superficially and functions to abduct the humerus.
The deltoid muscle has three origins; the body of the
clavicle, the spine of the scapula, and the acromion.
The deltoid muscle has three origins; the body of the
clavicle, the spine of the scapula, and the acromion.
The deltoid muscle has its insertion on the deltoid
tuberosity of the humerus. The short head of the
biceps brachii originates from the coracoid process,
and the long head originates from the supraglenoid
tubercle, passing through the intertubercular groove
of the proximal humerus. The biceps brachii is not a
shoulder muscle but does originate from the
shoulder. Paralysis of the deltoid results mainly in
50% loss of abduction strength. The axillary nerve
(C4-5) innervates the deltoid (Lynn, 2000).
2.3 Etiology of SIS
Internal impingement was first described as a
condition noted in overhead athletes, identified in
part due to poor outcomes of acromioplasty in this
population.
Multiple theories exist as to the primary
etiology of shoulder impingement, including
anatomic abnormalities of the coracoacromial arch
or humeral head“tension overload,” ischemia, or
degeneration of the rotator cuff tendons; and
shoulder kinematic abnormalities. Regardless of the
initial etiology, inflammation in the suprahumeral
space, inhibition of the rotator cuff muscles, damage
to the rotator cuff tendons, and altered kinematics
are believed to exacerbate the condition.
Impingement is thought to be due to inadequate
space for clearance of the rotator cuff tendons as the
arm is elevated. Therefore, factors that further
minimize this space are believed to be detrimental to
the condition (Ludewig and Cook, 2000)
There are some structures that could contribute
to its onset, such as the shape of the acromion, the
coracoacromial ligament, the superior aspect of the
glenoid fossa, hypermobility and instability of the
glenohumeral joint, capsular retractions and rotator
cuff tendinopathy (Lewis et al, 2005). Rotator cuff
problems are thought to account for nearly one third
of physician visits for shoulder pain complaints
(Ludewig and Cook, 2000). The vast majority of
people with impingement syndrome who are
younger than 60 years of age relate their symptoms
to occupational or athletic activities that involve
frequent overhead use of the arm. Epidemiologic
investigations have revealed a high prevalence
(16%–40%) of shoulder complaints consistent with
impingement in certain occupations, including
assembly-line workers, welders, steelworkers, and
construction workers. Frequent or sustained shoulder
elevation at or above 60 degrees in any plane during
occupational tasks has been identified as a risk
factor for the development of shoulder tendinitis or
nonspecific shoulder pain. Evidence relating
occupational exposure of frequent or sustained
shoulder elevation to shoulder musculoskeletal
symptoms is strongest for combined exposure to
multiple physical factors, such as holding a tool
while working overhead.
A number of impingement categories have
been identified including subacromial
impingement or “external impingement”; internal
impingement, which can be further divided into
anterior or posterior; and coracoid impingement.
14
Figure 11: The Deltoid Muscle.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
308

All categories of impingement are potential
mechanisms for the development or progression
of rotator cuff disease, or long head biceps
tendinopathy. Physical exam findings consistent
with impingement can also be associated with
labral tears in internal impingement (Budoff, 2003)
or develop secondary to instability or as a delayed
consequence of adhesive capsulitis. There are
multiple mechanisms by which impingement may
occur, including excess or reduced motion and
abnormal patterns of motion at particular portions
of the range of motion (Micahener et al, 2003). In
addition, anatomic abnormalities of the humerus
or acromion have been implicated in impingement.
It should be noted that rotator cuff disease can
develop without impingement, through tensile
overload or intrinsic tissue degeneration.
Regardless of the initial precipitating factor,
however, impingement, abnormal shoulder
motions, and associated rotator cuff disease often
are found in the presence of partial or full
thickness rotator cuff tears. In other words, even if
rotator cuff disease or tearing did not initiate from
impingement or abnormal motion, impingement
and abnormal motion are likely to contribute to
disease progression (Manske et al, 2014).
The subacromial impingement syndrome has
both primary and secondary forms. Primary
impingement is due to structural changes that
mechanically narrow the subacromial space; these
include bony narrowing on the cranial side (outlet
impingement), bony malposition after a fracture
of the greater tubercle, or an increase in the
volume of the subacromial soft tissues – due, e.g.,
to subacromial bursitis or calcific tendinitis – on
the caudal side (non-outlet impingement).
Secondary impingement results from a functional
disturbance of centering of the humeral head,
such as muscular imbalance, leading to an
abnormal displacement of the center of rotation in
elevation and thereby to soft tissue entrapment
(Garving et al, 2017).
2.4 Stages of SIS
Neer graded SIS into 3 different stages. In stage I,
the typical characteristics are reversible lesions with
edema and hemorrhage; most patients younger than
25 years are in this category. In stage II, chronic
inflammation or repeated episodes of impingement
lead to histomorphological changes, such a s
fibrosis and thickening of the supraspinatus, the long
biceps tendon, and subacromial bursae. Patients in
this stage are usually between 25 and 40 years of age.
In stage III, in patients more than 40 years of age,
tears of the rotator cuff, rupture of the biceps tendon,
and bony changes may be observed, accompanied by
significant tendon degeneration following a long
history of refractory tendinitis.
2.5 Normal Motion of Shoulder
During normal motion, the scapula will upwardly
rotate and posteriorly tilt on the thorax during
elevation of the arm in flexion, abduction,
scapular plane abduction, or unrestricted overhead
reaching (Ludewig and Barman, 2011).
Throughout this manuscript, elevation will be
used to refer the raising of the arm overhead in
any of these planes. Scapulothoracic internal or
external rotation is less consistent during arm
elevation, differing in pattern depending on what
plane the arm is elevated in, and depending on
what portion of the elevation range of motion is
considered (Ludewig and Reynolds, 2009). The
scapula must adjust in the transverse plane for the
intended plane of elevation. For flexion, the
scapula will internally rotate somewhat early in
the motion, whereas for coronal plane abduction,
it will externally rotate at the initiation of the
motion. Based on the limited end range data
available, it appears some external rotation of the
scapula will occur near end range for each of
these planes of elevation (Ludewig and Braman,
2011).
Recent investigations have added new
knowledge on how SC and AC joint motions
contribute to overall ST motion. The primary
clavicular motion occurring at the SC joint
during
active arm elevation in any plane
except extension is 30
○
of
posterior long axis
rotation.
17
Secondarily, the clavicle will retract
w15
○
at the SC joint during elevation, even with
flexion. However, the clavicle also “adjusts” in
the transverse plane (less retraction with flexion,
more with abduction) similarly to the changes in
scapular internal rotation with flexion versus
abduction (Ludewig and Reynolds, 2009). Finally,
a small amount of clavicular
elevation will occur
at the
SC joint with humeral elevation in any
plane. Concurrent with clavicular motion relative
to the thorax, measurable motion of the scapula
relative to the clavicle is also occurring at the AC
joint as the humerus is elevated in any plane.
Primary AC joint motions include upward rotation
and posterior tilt of the scapula relative to the
clavicle. Secondarily the scapula will internally
rotate relative to the clavicle at the AC joint, even
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
309

while abducting the arm (Ludewig and Braman,
2011).
Overall ST motion occurs either through
motion of the clavicle relative to the thorax,
motion of the scapula relative to the clavicle, or
some combination of both. During normal arm
elevation in any plane, both clavicular (SC) and
scapular (AC) motions described above are
contributing to the final position of the scapula on
the thorax. However, the non-parallel alignment
of the axes of rotation of the SC and AC joints
makes their contributions to ST motion
challenging to visualize (Teece et al, 2008). The
AC joint axes are aligned consistently with how
the axes are described for the scapula on the
thorax, such that if the scapula upwardly rotates,
posteriorly tilts or internally rotates relative to the
clavicle, there is a
1:1 “coupling” with ST
motion. In other words, 5
○
of scapular
upward
rotation relative to the clavicle would contribute
to 5
○
of ST upward rotation. In order to
understand the coupling of clavicular motion to
ST motion, it is helpful to visualize an axis of
rotation embedded along the long axis of the
clavicle, and another embedded in the scapula
from the root of the scapular spine to the AC joint.
In a superior transverse plane view, first imagine a
hypothetical situation where the clavicle and
scapular axes are parallel. In such a hypothetical
alignment, if the clavicle were elevated about its
anteriorly directed axis 9
○
relative to the
thorax,
the scapula would upwardly rotate 9
○
on the
thorax,
assuming no motion of the scapula
relative to the clavicle at the AC joint. If the
clavicle rotated posteriorly about its long axis 30
○
relative to the thorax, the scapula would
posteriorly tilt 30
○
relative to the thorax, and if
the clavicle retracted 9
○
relative to the thorax, the
scapula would externally rotate 9
○
relative to the
thorax (Teece et al, 2008). Now consider an
alternative hypothetical situation where the
scapula is internally rotated 90
○
relative to the
clavicle, such that the described axes in the
transverse plane are at a 90
○
angle (Ludewig
aand Braman, 2011). In such a hypothetical
alignment, if the clavicle were elevated about its
anteriorly directed axis 9
○
relative to the thorax,
the scapula would anteriorly tilt 9
○
on the thorax.
If the clavicle rotated posteriorly about its long
axis 30
○
relative to the thorax, the scapula would
upwardly rotate 30
○
on the thorax, and if the
clavicle retracted 9
○
relative to the thorax, the
scapula would externally rotate 9
○
on the thorax
(Teece et al, 2008).
In addition to the coupling of clavicle
motion to ST motion, during arm elevation in
any plane, the scapula relative to the clavicle is
also moving at the AC joint. These AC joint
motions may increase or decrease the overall
ST joint motion depending on whether they
complement or offset the SC joint coupled
scapular motions. So, in the example above for
scapular plane abduction to
120
○
relative to the
thorax, the 20
○
ST upward rotation coupled with
clavicle posterior rotation on the thorax, and 3
○
ST upward rotation coupled with clavicle
elevation on the thorax would be
complemented by an average of 11
○
of
scapular upward rotation
relative to the clavicle
across the same increment of scapular plane
abduction. The end result would be 34
○
of ST
upward rotation. For ST tilting, the 10
○
posterior
tilting coupled
with clavicle posterior rotation on
the thorax would be reduced by 6
○
anterior
tilting coupled with clavicle elevation on the
thorax as
described above. Subsequently, the
clavicle overall contribution to ST posterior tilting
would only be 4
○
.
However, the scapula relative to the clavicle
is tilting posteriorly during that scapular plane
abduction motion on average 16
○
, to result in
overall ST motion of 20
○
. Finally the 9
○
of ST
external rotation coupled with clavicle
retraction on the thorax is offset by an
average of 6
○
scapula internal rotation relative to
the clavicle, resulting in 3
○
of ST external
rotation. Note that final resulting
scapular
upward rotation motion and position on the
thorax is produced by complementary motion
of the clavicle relative to the thorax and scapula
relative to the clavicle. ST tilting is produced
almost exclusively by scapular motion relative to
the clavicle as the clavicle elevation and
posterior rotation motions at the SC joint are
offsetting. ST external rotation is minimal due to
offsetting motions of clavicle retraction relative
to the thorax and scapular internal rotation
relative to the clavicle (Ludewig and Braman,
2011).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
310

2.6 Abnormal Shoulder Motion in
Impingement
Rrecent review article identified scapular motion
abnormalities in subjects with impingement or
rotator cuff disease. The most frequent findings
have been reduced ST posterior tilting, reduced
ST upward rotation, increased ST internal
rotation, or increased clavicular elevation
relative to the thorax (Ludewig and Reynolds,
2009). These movement alterations are believed
to increase proximity of the rotator cuff tendons
to the coracoacromial arch or glenoid rim
(Ludewig and Braman, 2011).
Additionally, increased humeral head superior
or anterior translation has been found in subjects
with impingement
(Ludewig and Braman, 2011)
.
These directions of humeral head motion are
believed to reduce the subacromial space and
increase impingement risk. Biomechanical
evidence also supports the idea of glenohumeral
internal rotation contributing to sub- acromial
impingement beneath the anterior structures
(Ludewig and Braman, 2011)
.
Figure 12: Anatomical overview of the shoulder (left, above), showing the mechanism of subacromial impingement with
painful entrapment of soft tissues (arrows, right, above) on elevation of the arm, due to pathological contact of the humeral
head with the roof of the shoulder joint, particularly the anterolateral portion of the acromion (below).
Acromial shapes as classified by Bigliani and Morrison: type I (flat), type II (curved), type III (hooked).
Recent work also demonstrates how angles of
humeral elevation which minimize the
subacromial space may differ from angles of
humeral elevation where the rotator cuff soft
tissues are at greatest risk. The subacromial space
is typically described as minimized at 90
○
of
humeral elevation in all planes. However,
the
portion of the humerus in closest contact at that
point in the range of motion of abduction is
actually the lateral aspect of the greater tuberosity,
which has no rotator cuff soft tissue. The rotator
cuff tendons are actually in closest proximity to
the undersurface of the acromion near 45
○
of
humeral abduction relative to the thorax. By
angles past 60
○
humeral abduction, the
attachment sites or footprints of the cuff tendons
on the greater tuberosity have rotated past the
lateral acromial undersurface.
20
Patients may still
have a painful arc of motion near 90
○
of humeral
elevation in any plane, since this is where rotator
cuff muscle forces are highest. However, pain at
or above 90
○
of humeral elevation relative to the
thorax is unlikely a direct result of a compressive
subacromial impingement of the rotator cuff
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
311

tendons. Alternatively, proximity of the
undersurface of the cuff tendons to the superior
glenoid rim increases at higher arc
(Ludewig
and Braman, 2011)
. These same factors can
influence humeral motions. In summary, there is
some evidence of increased upper trapezius
activation and reduced serratus anterior activation
in the same subjects who have demonstrated
reduced ST posterior tilting, increased internal
rotation, and reduced upward rotation. There is
also evidence of increased ST anterior tilting and
internal rotation in subjects with a relatively short
resting length of the pectoralis minor
(Ludewig
and Braman, 2011)
.
Glenohumeral internal rotation deficit and
experimentally induced posterior capsule
tightness have also been shown to increase ST
anterior tilting and humeral anterior translations
relative to the glenoid, respectively. Slouched
sitting, thoracic kyphosis, and increased age have
also been related to increased ST anterior tilting
and internal rotation and reduced ST upward
rotation
(Ludewig and Braman, 2011)
.
Although not experimentally demonstrated,
other factors including reduced rotator cuff
activation and pectoralis major tightness can be
biomechanically theorized to impact ST or
glenohumeral kinematics in ways that are
believed to increase impingement risk. Each of
these factors provides additional insight in
planning treatment intervention approaches
targeted to specific movement deviations.
2.7 Clinical Presentation
The patient should be asked about the nature,
duration, and dynamics of the pain and about any
precipitating trauma (perhaps trivial trauma) or
stress, as well as about analgesic use. Patients
often report painful elevation and depression of
the arm between 70 ° und 120 °, pain on forced
movement above the head, and pain when lying
on the affected shoulder. The physical
examination consists of inspection, palpation,
and passive and active range-of-motion testing of
the shoulder, with attention to scapular
dyskinesia and hyperlaxity or instability of the
glenohumeral joint. Strength is tested in
comparison to the opposite side. In sub- acromial
impingement syndrome, weakness mainly affects
abduction or external rotation. Testing includes
the active and passive range of motion, iso-
metric contraction testing for the selective
determination of strength in internal and external
rotation and in abduction, and additional
impingement tests. The sensitivity and
specificity of such tests is low individually, but,
taken together, they are indispensable for the
differential diagnosis. Examining techniques are
summarized in Table 1.
Although impingement symptoms may arise
following trauma, the pain more typically develops
insidiously over a period of weeks to months. The
pain is typically localized to the anterolateral
acromion and frequently radiates to the lateral mid-
humerus. Patients usually complain of pain at night,
exacerbated by lying on the involved shoulder, or
sleeping with the arm overhead. Normal daily
activities such as combing one’s hair or reaching up
into a cupboard become painful, and a general loss
of strength may be noted. Onset of shoulder pain and
weakness following a fall in an individual over 40
years of age should raise concern for a complete tear
of the rotator cuff (Garving et al, 2017).
2.7.1 The tests
A thorough examination of the neck and shoulder is
critical to properly diagnosing SIS. Strength testing
of the upper extremities as well as neck and shoulder
ranges of motion should be carefully assessed. In
SIS, active and passive shoulder range of motion is
typically normal. The muscles of the rotator cuff are
Table 1: Examination for Shoulder Impingement
Syndrome.
Hawkins
test
Positive when pain arises on maximal
internal rotation of the arm in 90° of
anteversion with the elbow flexed. This
narrows the subacromial space
between the greater tubercle and the
coracoacromial ligament, causing
pain.
Neersign
One hand fixes the scapula while the
other elevates and internally rotates the
arm. This causes painful contact of the
greater tubercle with the roof of the
shoulder joint.
Jobe test
Both of the patient’s arms are held in
90° of abduction, 45° of flexion, and
internal rotation. The patient tries to
elevate the arms further against the
examiner’s marked resistance.
Painful
arch
Pain on abduction, with extended
elbow, in the scapular plane between
60° and 120° indicates pathology in the
subacromial space.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
312

best isolated with 3 separate maneuvers. To isolate
the subscapularis, the patient places their hand
behind the back and attempts to push away the
examiner’s hand, a maneuver called the lift-off test.
Next, with the arms at the sides and the elbows
flexed, the examiner resists the patient in external
rotation of the shoulder. Next, to isolate the
supraspinatus, which may be painful with SIS, the
patient abducts the arms to 90°, forward flexes to 30°,
and internally rotates each humerus so that the
thumbs are pointed to the floor. A downward force
is then applied to the forearms as the patient resists
(Garving et al, 2017).
Two provocative examination techniques are
highly sensitive but not very specific for diagnosing
SIS. Neer’s sign elicits pain with maximum passive
shoulder elevation and internal rotation while the
scapula is stabilized (Dong W et al, 2015). Hawkins
sign is pain with passive forward elevation to 90°
and maximum internal rotation (Garving et al, 2017).
These 2 tests have a negative predictive value of
greater than 90% when combined (Burbank et al,
2008). Marked rotator cuff weakness with positive
impingement signs may indicate a complete cuff
rupture. The Neer impingement test involves
injecting the subacromial space with 10 mL of local
anesthetic and observing an amelioration of pain
with these provocative tests (Garving et al, 2017).
2.8 Diagnostic And Evaluation
Clinical history-taking and a thorough physical
examination are the basis of the diagnostic
assessment. The diagnostic sensitivity of
physical examination is 90%. Imaging studies
(initially, plain x-rays) are indispensable for
differential diagnosis and for the exclusion of
calcific tendinitis or arthritic changes. If the
patient has had a circumscribed functional
limitation or persistent pain for 6 weeks or more
despite the usually adequate analgesia and
physical therapy, further imaging studies and
referral to a specialist are recommended
(Garving
et al, 2017).
2.8.1 Differential Diagnosis
Narrowing the etiology of shoulder pain can be
difficult as a number of conditions often coexist in
older individuals. The etiology of adhesive capsulitis
is unknown, although thought to be inflammatory in
nature. The disease is more commonly encountered
among women in their 50s and 60s. It is 5 times
more likely to occur in patients with diabetes
mellitus
2
and has been associated with
hypothyroidism. Adhesive capsulitis often presents
with unremitting shoulder pain at rest, and early
stages of adhesive capsulitis may present much like
impingement syndrome. Later, patients will develop
progressive loss of motion, with loss of internal
rotation an early sign of the motion loss. Patients
with adhesive capsulitis will be limited in both
active and passive ranges of motion, particularly in
contrast to SIS, where passive motion is unrestricted
(Garving et al, 2017).
Cervical radiculopathy may present with unilateral
shoulder pain. This can be particularly difficult to sort
out in older patients who may have both rotator cuff
pathology and cervical spine osteoarthritis. The patient
with shoulder pain of a cervical origin may have pain
and spasm in the trapezius muscles and a limited neck
range of motion. They may also experience pain,
numbness, or paresthesia radiating to the arm and hand.
Symptoms may be provoked by hyperextension and
lateral rotation of the neck (Spurling’s maneuver). A
key historical detail may be that pain is alleviated
when the forearm is rested above the head (Garving et
al, 2017).
Degenerative changes within the acromioclavicular
(AC) joint and osteolysis of the distal clavicle are often
found in individuals with a history of heavy labor or
weightlifting but may occur in anyone. The pain may
be present over the AC joint itself or be referred to the
upper shoulder and neck. Sleeping on the affected side
and overhead movements exacerbate the symptoms.
Physical examination typically confirms the diagnosis
with marked tenderness over the AC joint and pain
with compression of the joint through adduction of the
elevated arm. Osteoarthritis of the glenohumeral joint
presents with a painful diminished range of motion.
Arthritic changes in either joint are apparent on
radiographs (Garving et al, 2017).
3 CONCLUSION
The natural course of SIS is poorly described, but
evidence suggests that the condition is not self-
limiting (Garving et al, 2017). The initial
management of shoulder impingement has
traditionally included medical rehabilitation program
(therapeutic exercise and modalities), nonsteroidal
anti-inflammatory drugs (NSAIDs), and
corticosteroid injection. Medical rehabilitation
program (therapeutic exercise and modalities) is
frequently implemented to lessen pain and improve
function in SIS. In addition to medical rehabilitation
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
313
programs (therapeutic exercise and modalities) and
medications, activity and workplace modifications
must be discussed. Patients should attempt to
discontinue overhead activities until symptoms
diminish. It may be helpful to discuss “living within
a window” in which they consciously attempt to keep
their hands within an area in front of their body
during activity. The “window” should be from chest
to waist and 2 to 3 feet wide, allowing the patient to
avoid reaching over- head, away from the body, or
behind the back, all of which will exacerbate their
symptoms (Garving et al, 2017).
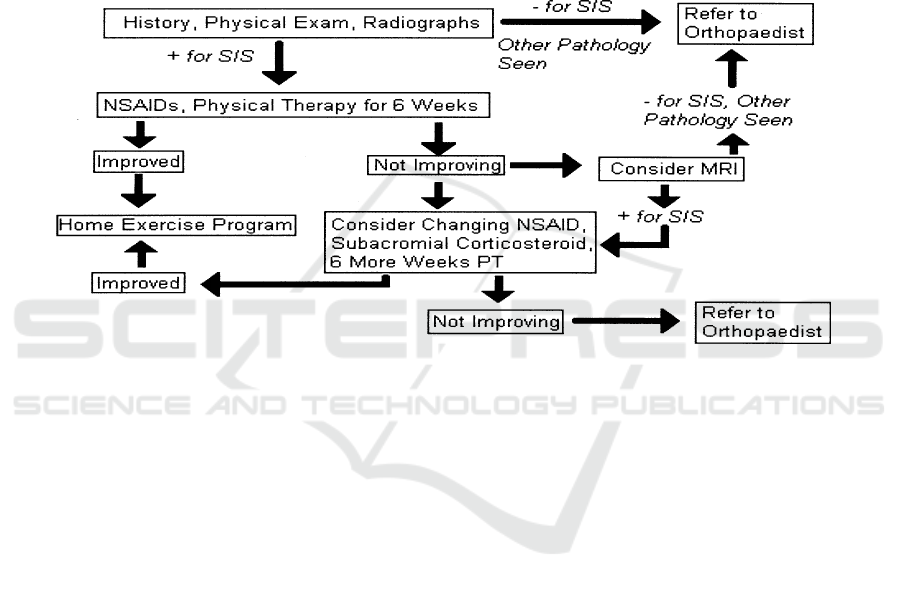
Bearing in mind that the literature offers few
truly well-conducted trials regarding the
management of SIS, we present an algorithm of our
recommended management of SIS based upon a
synthesis of the best available literature. Note that an
MRI is not recommended until at least a 6-week
therapeutic trial has been implemented unless a
complete rupture is suspected (Garving et al, 2017).
Figure 13: Treatment algorithm for subacromial impingement syndrome. SIS = subacromial
impingement syndrome; NSAID = nonsteroidal anti-inflammatory drug; PT = physical therapy.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
314

REFERENCES
Dong W, et al. 2015. Treatments for Shoulder
Impingement Syndrome. Medicine. 94(10):1-7.
Garving C, Jakob S, Bauer I, Nadjar R, Brunner UH.2017.
Impingement syndrome of the shoulder. Dtsch Arztebl.
114: 765–76
Burbank KM, Stevenson JH, Czarnecki GR, Dorfman
J.2008. Chronic shoulder pain: part I Evaluation and
Diagnosis. Am Fam Physician. 77(4):453-60.
Rockwood CA, Matsen FA, Wirth MA, Lippitt SB. 2009.
The Shoulder. Fourth Edition. Volume One. Saunders
Elsevier: Philadelpia
Lin DJ, Wong TT, Kazam JK. 2018. Shoulder Injuries in
the Throwing Athlete. Radiology. 286(2): 370-87
Eovaldi BJ. Varacallo M. 2018. Anatomy, shoulder and
upper limb, shoulder muscle. NCBI Bookshelf.
[accessed online at:
https://www.ncbi.nlm.nih.gov/books/NBK534836/]
Manske R, Nierman MG, Lucas B. 2013. Shoulder
posterior internal impingement in the overhead athlete.
International Journal of Sports Physical Therapy.
8(2):194-204
Ludewig PM, Braman JP. 2011. Shoulder impingement:
biomechanical considerations in rehabilitation. Man
Ther. 16(1):33-9.
Ludewig PM, Reynolds JF. 2009. The association of
scapular kinematics and glenohumeral joint
pathologies. J Orthop Sports Phys Ther. 39(2):90-104
Teece RM, Lunden JB, Lloyd AS, Kaiser AP, Cieminski
CJ, Ludewig PM. 2008. Three-dimensional
acromioclavicular joint motion during elevation of the
arm. Journal of Orthopaedic and Sports Physical
Therapy. 38(4):181–190.
Bey MJ, Brock SK, Beierwaltes WN, Zauel R, Kolowich
PA, Lock TR. 2007. In vivo measurement of
subacromial space width during shoulder elevation:
technique and preliminary results in patients following
unilateral rotator cuff repair. Clin Biomech. 22(7):767-
73.
Anatomy, Kinesiology, Pathomechanics, and Diagnosis of Shoulder Impingement Symptomp
315
