
The Effectiveness of Sensory Integration Therapy for Children with
Asperger's Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
Muhammad H. Sahid
1
, Andriani Pratiwi
2
, Ratna Darjanti Haryadi
3
1
Department of Occupational Therapy, University of Indonesia, Jakarta, Indonesia
2
Department of Occupational Therapy, Buahati Mandiri Center, Depok, Indonesia
3
Department of Physical Medicine and Rehabilitation, Dr. Soetomo General Hospital,
University of Airlangga, Surabaya, Indonesia
Keywords: Autism Spectrum Disorders, Asperger's Syndrome, Pervasive Development Disorder NOS, Sensory Integration,
Sensory Profile, BOT-2.
Abstract: Asperger's syndrome (AS) and Pervasive Development Disorder-NOS (PDD-NOS) challenge clinicians to
seek effective interventions. This study aimed to determine if sensory integration (SI) therapy has an effect
on any specific sensory motor deficits. The study used a pretest-posttest design. The intervention was SI
therapy twice weekly for 10 weeks. Subjects were 9 AS and 8 PDD-NOS children. The assessment tools
Sensory Profile and The Bruininks-Oseretsky Test of Motor Proficiency Second Edition (BOT-2) were
performed at start, 5 weeks and after 10 weeks of intervention. Tests results were analyzed in SPSS v22 using
ANOVA. Sensory seeking improved significantly (p<.05). (p<.05) on pretest-posttest and midtest- posttest.
Auditory processing, modulation of movement affecting activity level, modulation of visual input affecting
emotional responses and activity level (p<.05) of the Sensory Profile were significant. Post hoc analysis
revealed significance in auditory processing from pretest to posttest (p<.05). ANOVA analysis approached
significance on fine motor and perceptual skills (p=.08), multisensory processing (p=.08) and modulation
related to body position and movement (p=.08). Significant difference (p<.05) was seen on the balance subtest,
the running speed and agility subtest approached significance (p=.07). This study indicates that SI therapy is
effective in some specific sensory deficits AS and PDD-NOS.
1 INTRODUCTION
Autism Spectrum Disorders (ASD) include
Asperger's Syndrome (AS) and Pervasive-NOS
Development Disorders (PDD-NOS), which are
challenging topics among clinicians (American
Psychiatric Association, 2013). This study relies on
the assumption that the sensory and motor symptoms
in children with AS and PDD-NOS are the results of
abnormalities within the nervous system. It is also
based on the Sensory Integration (SI) theory which
provides a framework for understanding sensory
processing dysfunction and the SI treatment approach
which is described as preparing the body for
purposeful interaction with the environment.
Developmental abnormalities and an altered inferior
olive in the brainstem have been identified in children
with autism (Schaff et al, 2007). Auditory
brainstem response abnormalities, including
Prolonged intervals and abnormal individual waves,
have also been noted, which may result in
characteristics associated with autism and AS
(Davidson and Williams, 2000). A study done by
Minshew (2004) compared dynamic posturography
results from children and adult subjects with autism
to an effect cluster. The subjects with autism were
noted to have delayed postural stability development
and an underdeveloped postural control system. This
suggested that there was basal ganglia involvement
consistent with an increased caudate volume
(Nicholas et al, 2008).
Nicholas and colleagues (2008) reported that 62%
of the cases of ASDs, including children with AS,
PDD-NOS and autism, in South Carolina have
impaired motor skills (Schaff and Nightlinger, 2007).
Within the diagnostic criteria of the DSM-V, motor
delays and clumsiness are listed as associated
270
Sahid, M., Pratiwi, A. and Haryadi, R.
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not Otherwise Specified: A Case Control Study.
DOI: 10.5220/0009089302700280
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 270-280
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

features that are often present in children with AS
(American Psychiatric Association, 2013). Children
with AS have also been noted to have delayed motor
milestones, poor posture, low muscle tone, decreased
awareness and control of the body, decreased arm
swing, stiff gait, poor rhythm and timing, stiff and
clumsy movement patterns, a tendency to break
things, difficulty catching and throwing, and poor
handwriting (Klin, 2003). Khouzam, El-Gabalawi,
Pirwani and Priest (2004) suggest that motor delays
may be one of the first features recognized in young
children, with the more typical AS symptoms
presenting later (Khouzam et al, 2004).
Therefore, in order to contribute to an
understanding about the sensory processing and
motor skills of children with AS and related PDDs,
and to assess the effectiveness of SI treatment, an
intervention program based on the theories of SI was
implemented for children with AS and PDD-NOS.
The aims of this study were to demonstrate the extent
of sensory and motor skills in children with AS and
PDD-NOS and additionally determine if SI therapy
has benefit in improving any specific deficits that
were known in this cluster.
2 METHODS
2.1 Setting
The evaluation and intervention of the participants of
this study took place in an occupational therapy center
setting which contained the equipment necessary to
provide SI therapy.
2.2 Participants
Inclusion criteria: At the time of the study,
participants were required to be 5 to 9 years old, with
a diagnosis of AS or PDD-NOS,. Since SI treatment
relies on the presence of SI deficits, an additional
inclusion criterion was that participants had SI
deficits as determined by initial testing done by the
researcher. Therefore, only children with SI deficits
based on initial testing for the study were eligible to
participate in the intervention phase of the research.
Children receiving other therapy that utilized an SI
approach were excluded.
Based on an autism to AS ratio of 5:1, it was
conservatively estimated that approximately 37
children with a diagnosis of AS, were between the
ages of 4 and 11 years (Fombonne, 2003). Since not
all children with AS or PDD-NOS receive services,
and diagnosis may be delayed beyond age 11, it was
recognized that this was likely a low estimate of the
number of children with AS. As we estimated that the
number of potential subjects was relatively small, all
potential participants who met the inclusion criteria,
and agreed to participate by completing consent and
assent forms, were enrolled in the study. During the
recruitment period, we decided to include children
with PDD-NOS, since obtaining study participants
who met all study criteria for AS was difficult. A goal
of at least 10 subjects was set, based on the power
described previously and taking into account the
possibility of attrition.
2.3 Human Subject Protection
Information collected for study purposes including
the child’s test scores and other private information,
was recorded on the score forms in such a way that
both the parents’ and their child’s identities remained
confidential. Since the researcher needed to formulate
a treatment plan for each child based on his or her test
results, the researcher needed to know the child’s
name. Since both the researcher and another therapist
conducted the testing during various phases of the
research, the child’s first name only was used during
test sessions. The other therapist who administered
some of the test procedures was asked to leave
identifying information forms blank, so that code
numbers could be entered by the researcher in order
to maintain confidentiality. Once test forms were
returned to the researcher, a code number was
assigned to that child. With respect to dispersion of
study information, any information regarding this
study is and will be reported so that there is no way
that the child can be identified. All forms have and
will continue to be stored in a locked file cabinet in
the office of the researcher for seven years, after
which time those will be destroyed.
2.4 Study Design
This research was a preliminary study utilized a pre-
test post-test design with a delayed treatment
approach. At the initiation of the study, pretesting was
conducted using the Sensory Profile and the BOT-2.
To allow subjects to act as their own control, a 5-
week baseline phase, in which no intervention was
provided, took place prior to the start of SI therapy.
Sensory integration therapy was provided for 10
weeks. Therapy sessions took place two days per
week, for 45-60 minute sessions. Post-
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
271

testing occurred following the 10 week intervention
period, and all of the testing procedures that were
administered in the mid-testing phase were repeated.
2.5 Instrumentation
The Sensory Profile. The Sensory Profile is a parent
completed questionnaire, which assesses the child’s
sensory processing and sensory modulation. It helps
to determine areas of sensory processing deficits that
may contribute to problems in completing daily life
activities. It was given to the parents to complete at
the start of the study, 5 weeks into the study, and at
the end of treatment (Dunn, 2014).
The test is made up of three sections. The first
section assesses the child’s ability to process sensory
information and is broken down by sensory systems
which include: auditory, visual, vestibular, touch,
multisensory and oral. The second section is used to
assess the child’s ability to modulate more than one
type of sensory input at a time. The final section
assesses behavioral and emotional responses. Results
from the questionnaire provided information on the
child’s sensory seeking behaviors, emotional
reactivity, low endurance or tone, oral sensory
sensitivity and inattention or distractibility, as well as
the presence of poor registration, sensory sensitivity,
sedentary behaviors and fine motor and perceptual
abilities (Dunn et al, 2002).
Internal consistency measures for the Sensory
Profile ranged from .47-.91, and standard errors of
measurement have been reported to be between 1.0
and 2.8, suggesting parental scores are similar to true
scores (Dunn et al, 2002).
2.5.1
The Bruininks-Oseretsky Test of
Motor Proficiency, Second Edition.
The BOT-2 was administered to the children at the
beginning of the study, five weeks into the study, and
at the end of the intervention phase. It measures the
gross and fine motor performance of individuals, ages
4 to 21 years. The test is broken down into four
composites, each with two subtests. The Fine Manual
Control composite examines fine motor precision and
integration. The Manual Coordination composite
assesses manual dexterity and upper-limb
coordination. A 3rd composite: Body coordination,
assesses bilateral coordination and balance. Finally,
running speed and agility and strength are assessed in
the Strength and Agility composite. The scores from
these subtests are added up to determine a Total
Motor Composite Score which can be used to
determine percentile ranks (Bruininks and Brett,
2010).
Internal consistency reliability has been obtained
using Pearson correlations for subtests and a stratified
alpha method for composite scores, and has been
reported to range from moderate to excellent with
subtest and composite correlation coefficients
ranging from .60-.97. Test-retest reliability has been
established based on a time frame of 7 to 42 days, with
Pearson correlation coefficients averaging .78
(subtest) and .83 (composite) for children ages four
to seven years,
.76 (subtest) and .83 (composite) for children ages 8-
12, and .69 (subtest) and .77 (composite) for children
13-21 years of age. Interrater reliability Pearson
correlation coefficients range from .86 to
.99 for all of the BOT-2 subtests and composites. A
BOT-2 test kit is required to administer the test in the
standardized manner, and test completion takes
approximately one hour (Bruininks and Brett, 2005).
2.6 Data Analysis
All information was recorded and analyzed in SPSS
version 22. To analyzed if children with AS and PDD-
NOS demonstrate improvements in sensory
processing or motor skills following SI intervention,
scores for the Sensory Profile and BOT-2 were
analyzed using repeated measures analysis of
variance (ANOVA) in order to compare changes
within individual participant scores across test
sessions. A p value of less than .05 was interpreted to
be significant. Post hoc testing using pairwise
comparisons was performed to determine whether
improvements were related to intervention. If
significant differences were evident from pretest to
posttest, or from midtest to posttest that were not
present from pretest to midtest, the hypotheses that
sensory processing or motor skills can improve
following SI therapy could be accepted.
The researcher conducted all of the testing during
the pretest and midtest phases of the study. In order to
prevent researcher bias, a second examiner conducted
the posttesting for each child who completed the
intervention phase. This second examiner was trained
and certified to administer the tests, and was blind to
the purposes of the study.
Interrater reliability testing was completed for one
child during the post-testing phase. The child was
selected based on convenience with scheduling, and
the posttesting phase was selected for reliability
testing in order to prevent bias by the second
examiner.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
272
3 RESULTS
Initial contact was created with the parents of 25
children. From this cluster, 7 subjects declined
participation. The primary reasons were inability to
comply to the schedule, and the wish to find specific
programs such as day or social programs. One person
participated in a different AS study. The remaining 17
children enrolled in the study, 9 with AS and 8 PDD-
NOS. 10 out of the 17 participants
were male, age range 55 to 109 months, with a mean
age of 80.9 months (6.6 years). Finally 12 participants
completed the study because 5 participants were lost
to follow up.
The result of Sensory Profile showed that most of
17 participants had sensory problems. Table 1
identifies the percentages of children reported as
being definitely different from typically developing
children.
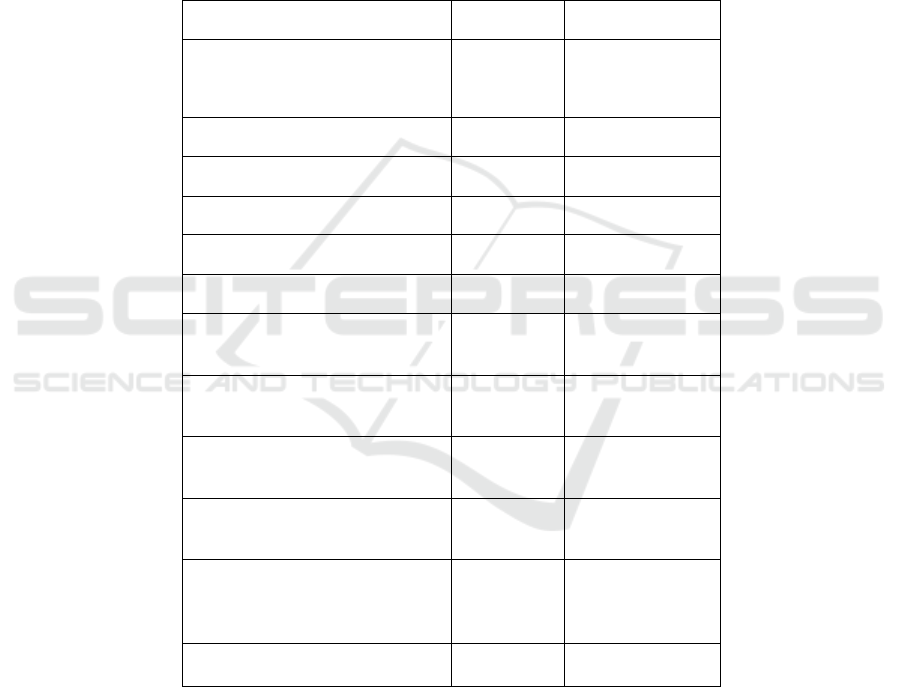
Table 1: Summary of Mean Scores and Repeated Measures ANOVA for Sensory Profile.
Subtest
AS (N9)
PDD NOS (N8)
Auditory Processing
9 = 100%
7 = 88%
Visual Processing
6 = 67%
7 = 88%
Vestibular Processing
9 = 100%
8 = 100%
Touch Processing
9 = 100%
7 = 88%
Multisensory Processing
8 = 89%
7 = 88%
Oral Sensory Processing
7 = 78%
7 = 88%
Sensory Processing Related to
Endurance/Tone
6 = 75%
a
5 = 63%
Modulation Related to Body
Position and Movement
6 = 67%
6 = 75%
Modulation of Movement
Affecting Activity Level
9 = 100%
7 = 88%
Modulation of Sensory Input
Affecting Emotional Responses
9 = 100%
8 = 100%
Modulation of Visual Input
Affecting Emotional Responses
and Activity Level
9 = 100%
8 = 100%
Emotional/Social Responses
9 = 100%
8 = 100%
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
273
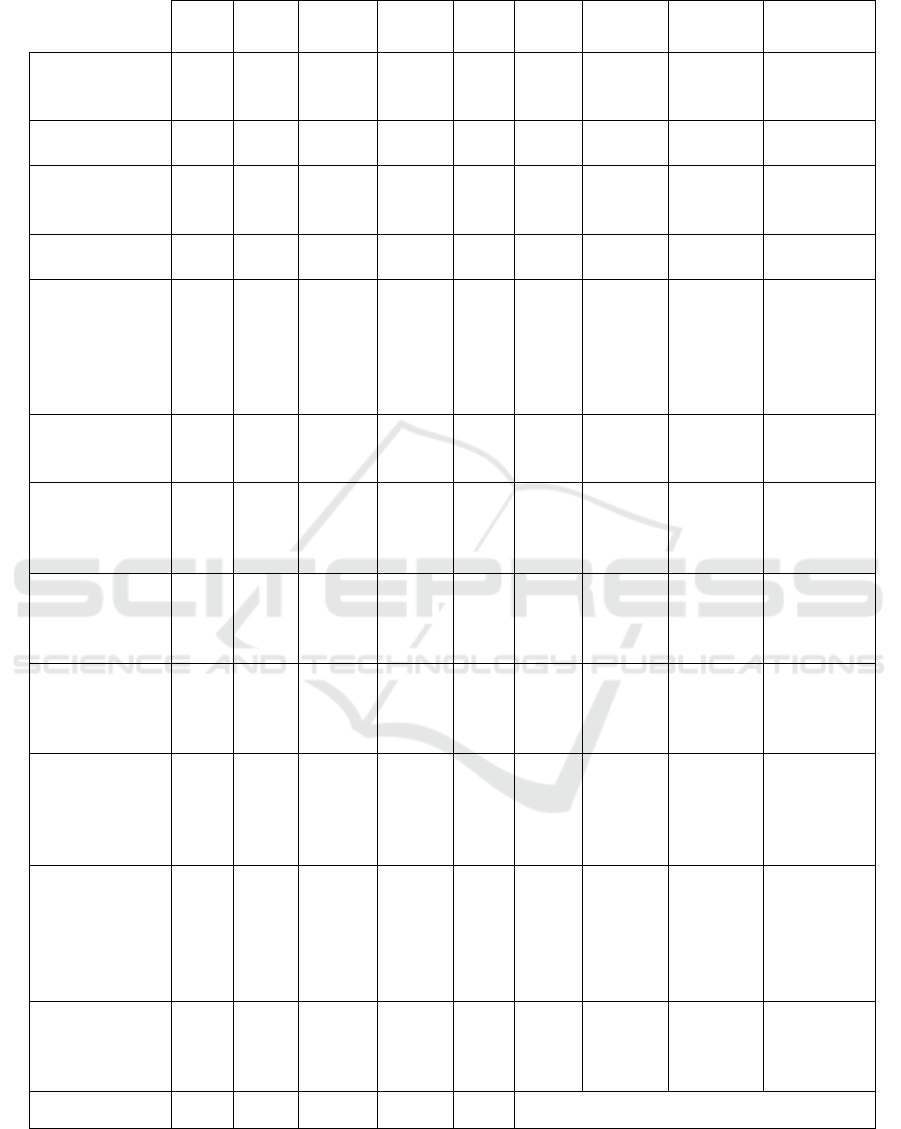
Table 2: Summary of Mean Scores and Repeated Measures ANOVA for Sensory Profile.
M
(SD)
M
(SD)
M (SD)
Effect
Size
Pretest-
Midtest
Pretest-
Posttest
Midtest-
Postest
Auditory
Processing
(sound)
21,67
(5,47)
22, 18
(5,08)
25,80
(6,40)
7,41*
0,01
0,47
0,08
0,00
0,21
Visual Processing
(vision)
27,07
(6,55)
27,82
(5,00)
29,65
(7,38)
0,98
0,44
0,27
0,58
0,26
0,49
Vestibular
Processing
(movement)
38,66
(6,96)
41,33
(5,36)
42,81
(6,11)
3,43
0,05
0,28
0,03
0,10
0,42
Touch Processing
57,30
(9,61)
60,30
(9,54)
66,66
(9,87)
10,40*
0,00
0,65
0,02
0,01
0,05
Multisensory
Processing
(multiple,
simultaneous
sensory
experiences)
20,30
(1,21)
22,52
(2,59)
25,31
(4,52)
3,20
0,09
0,75
0,86
0,17
0,06
Oral Sensory
Processing
(mouth)
38,17
(11,86)
36,68
(15,28)
40,18
(11,03)
0,92
0,41
0,18
0,77
0,20
0,36
Sensory
Processing
Related to
Endurance/Tone
26,66
(9,40)
27,50
(9,90)
32,00
(7,87)
0,61
0,58
0,27
0,66
0,43
0,47
Modulation
Related to Body
Position and
Movement
34,65
(4,03)
35,31
(5,82)
38,50
(8,06)
3,23
0,07
0,46
0,11
0,08
0,22
Modulation of
Movement
Affecting
Activity Level
20,00
(2,43)
19,50
(3,15)
23,01
(2,19)
4,31*
0,04
1,28
0,61
0,08
0,05
Modulation of
Sensory Input
Affecting
Emotional
Responses
11, 01
(2,53)
12,02
(2,10)
12,65
(2,34)
0,61
0,57
0,33
0,32
0,37
0,73
Modulation of
Visual Input
Affecting
Emotional
Responses and
Activity Level
11,00
(0,63)
11,15
(1,73)
12,52
(1,86)
4,74*
0,40
0,73
0,72
0,06
0,06
Emotional/Social
Responses
(inappropriate
behaviors)
48,10
(8,09)
50,52
(3,94)
55,52
(5,21)
1,80
0,22
1,06
0,60
0,21
0,21
Subtest
Pretest
Midtest
Post test
F
P
Post-Hoc Test
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
274
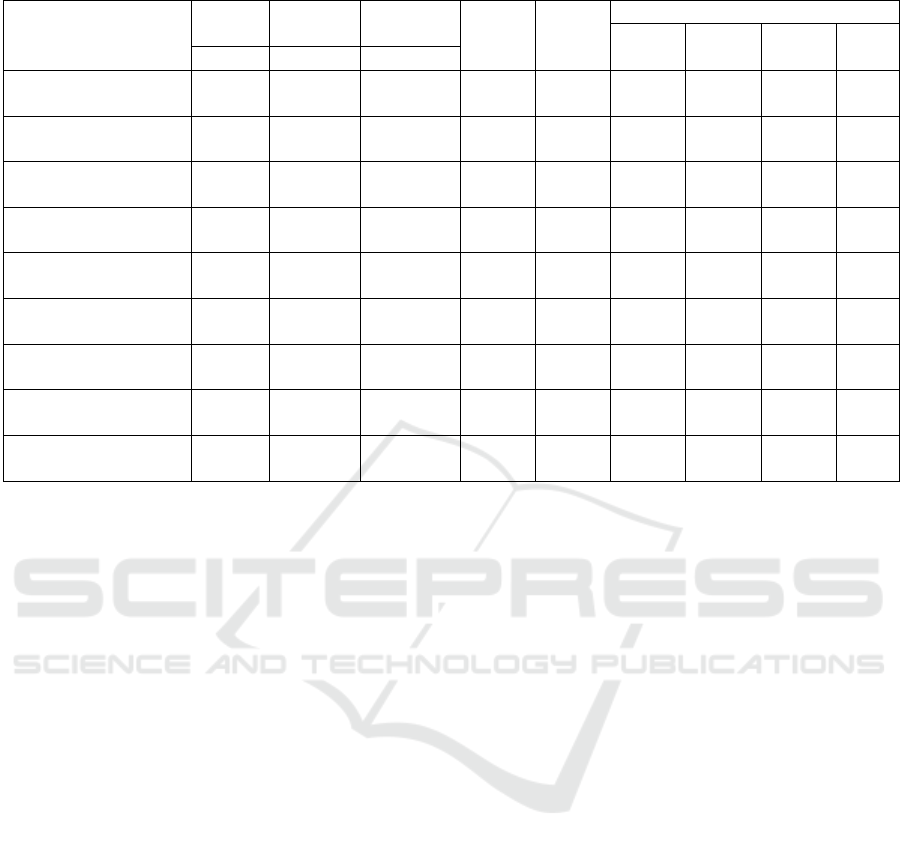
Table 3: Summary of Mean Scores and Repeated Measures ANOVA for Sensory Profile.
Subtest
Pretest
Midtest
Post test
F
P
Post-Hoc Test
Effect
Size
Pretest-
Midtest
Pretest-
Posttest
Midtest-
Postest
M (SD)
M (SD)
M (SD)
Sensory Seeking
49,69
(3,63)
51, 03
(5,81)
60,50
(12,82)
6,61*
0,02
0,95
0,50
0,05
0,03
Emotionally Reactive
40,07
(6,52)
41,82 (4,56)
46,83 (5,38)
2,23
0,17
0,87
0,33
0,16
0,29
Low Endurance/Tone
28,66
(9,41)
29,53 (9,92)
32,00 (7,81)
0,63
0,58
0,28
0,68
0,40
0,46
Oral Sensory Sensitivity
28,30
(9,31)
26,03
(12,54)
28,66 (9,37)
1,08
0,30
0,25
0,42
0,78
0,23
Inattention/Distractibility
15,78
(3,06)
19,02
(3,09)
20,81
(5,82)
7,40
0,04
0,40
0,02
0,01
0,33
Poor Registration
28,07
(3,53)
28,01 (2,98)
29,68 (5,25)
0,88
0,46
0,38
1,01
0,42
0,23
Sensory Sensitivity
15,16
(4,54)
15,01 (4,23)
15,80 (3,73)
0,71
0,53
0,27
0,76
0,39
0,47
Sedentary
13,07
(4,40)
12, 51
(4,04)
14,30
(2,87)
1,60
0,27
0,54
0,59
0,23
0,24
Fine Motor/Perceptual
7,65
(2,73)
8,81 (2,16)
9,20 (1,96)
3,53
0,07
0,17
0,21
0,05
0,32
Sensory Profile subtest were analyzed to
determine if significant differences were evident
following Sensory Integration therapy. The Sensory
Seeking factor improved significantly (p<.05). Post
hoc analysis identified significant (p<.05) changes
between pretest and posttest, and also between
midtest and posttest. This means that parents
reported less frequent attempts by their child to
seek out and provide himself or herself with
additional sensory input. Three sections of the
Sensory Profile, also showed significant
improvement following intervention (table 3).
These include Auditory Processing, Modulation of
Movement Affecting Activity Level and
Modulation of Visual Input Affecting Emotional
Responses and Activity Level (p<.05). Post hoc
analysis revealed significant improvements in
Auditory Processing from pretest to posttest
(p<.05). Modulation of Visual Input Affecting
Emotional Responses and Activity Level assesses a
child’s ability to use visual input appropriately
during personal interactions including the ability to
make eye contact, and the ability to recognize but
not visually obsess about the actions of others. In
this subtest, children demonstrated significant
improvement from pretest to posttest (p<.05).
Significant differences were also identified for
Modulation of Movement Affecting Activity
Level. For this subtest however, when post hoc
analyses were completed, the results did not
indicate significant differences. Repeated measures
ANOVA approached significance on four other
subtests of the Sensory Profile (table 2). These tests
included Fine Motor and Perceptual Skills (p=.08),
Multisensory Processing (p=.08) and Modulation
Related to Body Position and Movement (p=.08).
An improvement in Fine Motor and Perceptual
skills reflects improvements in a child’s ability to
perform fine motor skills such as writing and
drawing. An improvement in Multisensory
Processing points to improvements in a child’s
ability to process information that is entering the
body from more than one sensory system. Finally,
the results on the Modulation Related to Body
Position and Movement subtest suggest that
following the 10-week intervention phase, the
children were better able to control the amount of
movement in which they engaged. A 10 week
intervention phase was effective in improving some
areas of sensory processing, some motor skills and
some behaviors.
Table 4 showed that most of 17 participants
had impaired motor skills. Percentages of 4
aspect in motor skills problems. A 10 weeks
intervention phase was effective in improving
certain areas of sensory processing, motor skills
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
275
and behaviors. The results from this study
provide preliminary evidence to support the use
of SI therapy in children with AS and PDD- NOS
(table 5). The results indicated that the
participants demonstrated significant
improvements (p<.05) on the Balance subtest,
with significant changes occurring from pretest
to posttest. Additionally, significance was
approached on the Running Speed and Agility
subtest (p=.07) (table 5). This means that
children demonstrated more success to perform
complex motor skills following the intervention.
Composite scores were not significantly
impacted following intervention.
Table 4: Percentage of part
normative data indicating imp
Therefore, since significant or nearly significant
improvements were noted for two subtests of the
BOT-2 during posttest that were not present for
pretest or midtest, it appears that certain areas of
motor function were improved following SI
therapy. It should also be note that the
participants did not demonstrate significant
improvements in Fine Motor Precision, Fine
Motor Integration, Manual Dexterity, Upper-
Limb Coordination, Bilateral Coordination or
Strength, which may suggest that some types of
motor skills, such as balance, running and agility
may respond better to ten weeks of SI therapy
than other types of motor skills.
percentile compared to
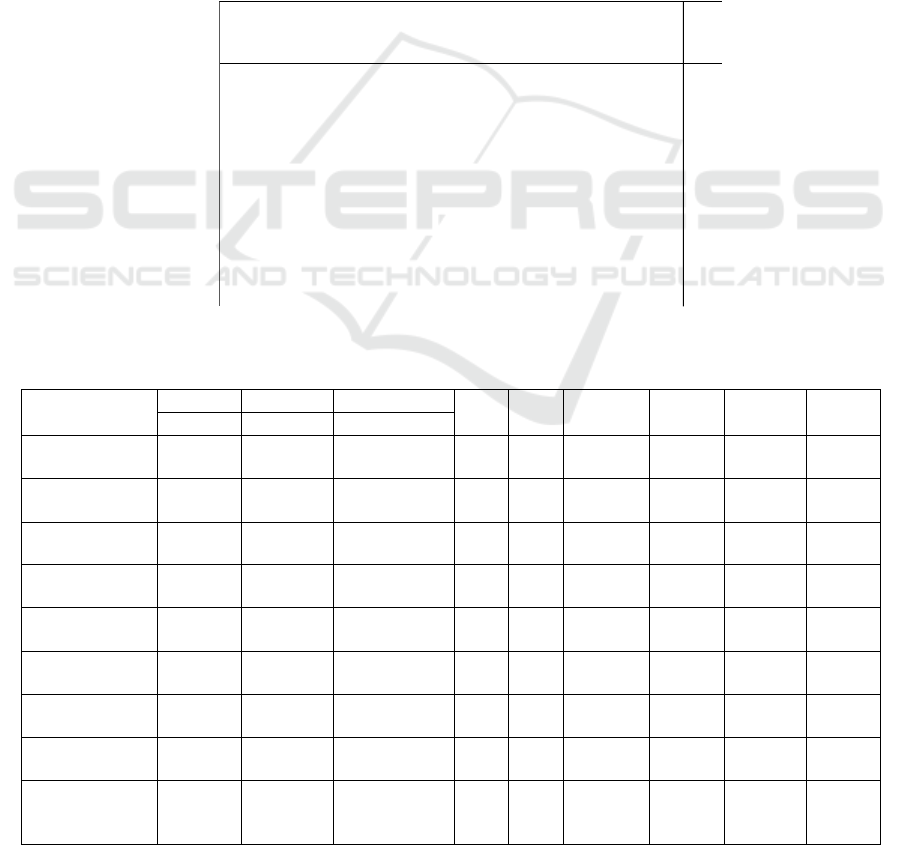
Table 5: Summary of Mean Scores and Repeated Measures ANOVA for BOT-2.
Subtest
Pre test
Mid test
Post test
F
P
Effect Size
Pre test-
Mid test
Pre test-
Post test
Midtest-
Post test
M (SD)
M (SD)
M (SD)
Fine Motor
Precision
11,67
(5,79)
13, 18
(6,23)
9,16
(5,98)
2,50
0,10
-0,63
0,16
0,24
0,15
Fine Motor
Integration
13,93
(6,13)
14,35
(6,59)
13,02 (5,57)
0,98
0,44
-0,25
0,58
0,29
0,41
Manual Dexterity
11,66
(5,96)
11,73
(6,09)
12,66 (6,06)
0,80
0,45
0,16
0,63
0,20
0,49
Upper-Limb
Coordination
8,68
(3,12)
8,50
(2,86)
9,32 (3,87)
0,36
0,74
0,25
0,82
0,49
0,58
Bilateral
Coordination
11,15
(3,14)
10,52
(2,34)
10,31 (4,02)
0,09
0,90
0,05
0,66
0,81
0,90
Balance
7,52
(2,43)
8,68
(1,52)
9,54 (2,59)
5,40
*
0,04
0,37
0,11
0,01
0,29
Running Speed
and Agility
13,66
(3,91)
13,00
(3,74)
15,02 (4,07)
3,51
0,06
0,52
0,38
0,16
0,03
Strength
9,67
(3,75)
10, 02
(4,48)
10,33 (3,48)
0,18
0,83
0,08
0,78
0,63
0,57
Fine Manual
Control
Composite
45,33
(12,63)
38,76
(7,19)
41,55 (12,06)
1,73
0,23
0,28
0,09
0,28
0,52
icipants whose BOT-2 composite scores fell at or below the 18
th
aired motor skills.
BOT-2 Composite Scores
AS
PDD NOS
(N=9)
(N=8)
Fine Manual Control (Fine Motor
Precision and Fine Motor 6 = 67% 6 = 75%
Integration)
Manual Coordination (Manual
Dexterity and Upper-Limb 6 = 67% 4 = 50%
Coordination)
Body Coordination (Bilateral
9 = 100% 7 = 88%
Coordination and Balance)
Strength and Agility (Running
5 = 56% 4 = 50%
Speed and Agility and Strength)
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
276

4 DISCUSSIONS
This study hypothesized that children with AS
and PDD-NOS would demonstrate sensory and
motor impairments when compared to normative
samples, as identified on the Sensory Profile and
the BOT-2. The participants in this study were
identified as being typically different or
definitely different from the normative sample
on all 23 subtests of the Sensory Profile. More
than half of the parents reported impairments
that were greater than typically developing
children in 21 of those areas. Subjectively, this
supports the hypothesis that children with AS or
PDD-NOS have sensory impairments as
compared to normative samples on the Sensory
Profile. On both pretest and midtest, which
occurred prior to the start of the intervention
phase, 100% of the participants were rated by
their parents to have difficulty in several areas of
sensory processing. Among the most common
sensory impairments in this data were Emotional
Reactivity, Inattention or Distractibility,
Modulation of Sensory Input Affecting
Emotional Responses, Emotional or Social
Responses and Behavioral Outcomes of Sensory
Processing. Emotional reactivity can be
described as having an emotional reaction to
sensory input that is more than would typically
be expected. A child who is considered
emotionally reactive may be overly sensitive to
criticism, may cry easily or may offer more than
typical affection towards others. A poor score on
Inattention and Distractibility would be
identified in children who tend to be easily
distracted or inattentive. Emotional and Social
responses describe inappropriate or immature
behaviors, such as throwing temper tantrums,
having signs of low self esteem or having
excessive fears that interfere with daily routines.
Behavioral Outcomes of Sensory Processing
are those daily activities that require the ability
to process sensory information, such as writing,
performing tasks efficiently and tolerating
changes in routine. It appears from the results
that the sensory processing impairments
identified in the children in this study frequently
affect their behavior and their ability
to control their emotions. Less common parental
concerns, where fewer than 50% of the children
were rated as being probably different or
definitely different include Sensory Sensitivity,
which describes a child who, for example, is
overly fearful of movements and heights, and
Sedentary behaviors which describe preferences
toward quiet activities or activities that do not
require much movement.
In order to identify if motor skill impairments
existed in this group of children, the BOT-2 was
administered during the pretest and midtest
phases of the study, prior to the intervention
phase. The BOT-2 is a performance-based test
which provides objective information regarding
a child’s ability to perform gross and fine motor
skills. The scores achieved by the subjects on the
BOT-2 were compared to established age and
gender referenced norms. If subjects fell at or
below the 18th percentile they were considered
to have greater impairments than children who
are typically developing. Subtest scores are
combined to form composite scores in four key
areas of motor skill performance: Fine Manual
Control, Manual Coordination, Body
Coordination and Strength and Agility. On all of
the composite scores obtained during pretest and
midtest, more than half of the participants were
found to score below the 18th percentile for their
age and gender. As a group, the children had the
most difficulty with the Manual Coordination
and Body Coordination composites. The Manual
Coordination composite examines a child’s
manual dexterity in tasks such as sorting cards,
stringing blocks and placing pegs in a pegboard.
It also assesses upper-limb coordination through
a series of ball skills using a tennis ball. The
Body Coordination composite assesses bilateral
coordination including hand tasks, hand and feet
tasks, and whole body skills, as well as standing
balance skills on the floor and on a narrow
balance beam. These findings suggest that
perhaps the children’s greatest difficulties with
respect to their motor skills is in their inability to
coordinate their bodies to perform fine motor and
gross motor movements. The data obtained
provides quantifiable evidence to
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
277

support the hypothesis that the children with AS
and PDD-NOS in this study had motor
impairments as compared to children in the
normative sample of the BOT-2 who were
typically developing. Therefore, the hypothesis
is accepted for impairments in Manual
Coordination and Body Coordination. The
children were also impaired in other areas of
motor skill performance, including Fine Manual
Control and Strength and Agility, although these
impairments were less frequent.
In order to address the hypothesis that
children would demonstrate improved motor
performance following SI therapy, posttest
scores from the BOT-2 were compared to pretest
and midtest scores using repeated measures
ANOVA. The results indicated that the
participants demonstrated significant
improvements (p<.05) on the Balance subtest,
with significant changes occurring from pretest
to posttest. Additionally, significance was
approached on the Running Speed and Agility
subtest (p=.07), which assessed a child’s running
speed and ability to perform repetitive stepping
and hopping skills. This means that children
demonstrated more success in balancing and
coordinating their bodies to perform complex
motor skills following the intervention.
Composite scores were not significantly
impacted following intervention. Therefore,
since significant or nearly significant
improvements were noted for two subtests of the
BOT-2 during posttest that were not present for
pretest or midtest, the third hypothesis is
accepted for the specific areas of balance and
running speed and agility. Therefore, it appears
that certain areas of motor function can be
improved following SI therapy. It should also be
noted that the participants did not demonstrate
significant improvements in Fine Motor
Precision, Fine Motor Integration, Manual
Dexterity, Upper-Limb Coordination, Bilateral
Coordination or Strength, which may suggest
that some types of motor skills, such as balance,
running and agility may response better to ten
weeks of SI therapy than other types of motor
skills.
The current study that assess children with
AS using the Sensory Profile are Dunn and
colleagues (2002) and Klyczek and colleagues
(2005) both identified difficulty with modulating
sensory input in their samples of children with
AS. The participant’s scores on the Sensory
Profile suggest that the children in the current
study had impairments in both sensory
processing and sensory modulation. This
supports the previous research which has
provided evidence that there is a connection
between sensory processing and sensory
modulation, and that these impairments are
present in children with ASDs.
Those studies identified similar
improvements in sensory-based functional
behaviors. These improvements indicated fewer
disruptive behaviors, improved attention and
improved responses to sensory input. Findings
from both studies therefore appear to offer
support for the use of SI therapy as an
intervention for these children. A more recent
case study of a four year old boy with poor
sensory processing was reported by Schaaf and
McKeon Nightlinger (2007). The results of ten
months of individualized SI therapy, provided
once a week, resulted in improvements in Sensory
Profile scores and the achievement of several
established occupational performance goals
[22]. The authors suggested that the results
obtained indicated that an improvement was
made in the child’s sensory processing as a result
of the intervention. The current study is the
second known study to utilize Sensory Profile
scores in a pretest-posttest scenario. In both
cases, parents reported via the Sensory Profile
that improvements were seen in their children’s
ability to receive, process and integrate sensory
information in a manner that allowed for more
appropriate and more efficient performance in
daily activities (Wahyuni and Wardhani, 2019).
Other researchers have used modified
versions of traditional SI therapy in an effort to
measure its effectiveness. In an attempt to
measure the outcomes of intervention using a 10-
week Sensory Integration and Perceptual- Motor
protocol, Davidson and Williams (2000) studied
the impact of treatment for children with
Developmental Coordination Disorders. Unlike
the current study which identified
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
278

significant improvements in the Balance subtest
and nearly significant improvements in the
Running Speed and Agility composite of the
BOT-2, the Davidson and Williams study did not
find significant improvements on tests of motor
skills using the Movement Assessment Battery
for Children, and the Beery-Buktenica
Developmental Test of Visual-Motor Integration
(Davidson and Williams, 2000).
5 CONCLUSIONS
After following 10-weeks of SI therapy,
respondens demonstrated improvements in
behavior, sensory processing and modulation,
balance and praxis. This is mean that SI therapy
may be an appropriate treatment technique for
children with AS and PDD-NOS. As more
children are being diagnosed with ASD, it is
critical that researchers and clinicians address all
their needs, including those that involve sensory
processing and motor skill performance. This
research study provides one of preliminary
evidence on the efficacy of SI therapy for
children with AS and PDD-NOS.
ETHICAL CLEARANCE
Ethical clearance has been approved by
University of Indonesia Public Health Ethics
Commite with 436/UN2.F10/PPM.00.02/2018
as ethical number registered.
REFERENCES
American Psychiatric Association. 2000. Diagnostic and
Statistical Manual of Mental Disorders, 4th Edition -
Text Revision (DSM-IV-TR). Washington, DC:
American Psychiatric Association.
American Psychiatric Association. 2013. Diagnostic and
Statistical Manual of Mental Disorders, 5th Edition
(DSM-V). Washington, DC: American Psychiatric
Association.
Bruininks, H.R., & Brett, D. 2010. Bruininks-Oseretsky
Test of Motor Proficiency Second Edition Brief Form.
United States of America. NCS Pearson, Inc.
Bruininks, H.R., & Brett, D. 2005. Bruininks-Oseretsky
Test of Motor Proficiency Second Edition Full Form.
United States of America. NCS Pearson, Inc.
Cederlund, M. 2004. One hundred males with Asperger
syndrome: a clinical study of background and
associated factors. Developmental Medicine and Child
Neurology, 46, 652-660.
Davidson, T., & Williams, B. 2000. Occupational therapy
for children with Developmental Coordination
Disorder: a study of the effectiveness of a combined
sensory integration and perceptual-motor intervention.
British Journal of Occupational Therapy, 63(10), 495-
499.
Dunn, W. 2014. Sensory Profile 2. United States of
America. Pearson Education, Inc.
Dunn, W., Saiter, J., & Rinner, L. 2002. Asperger
Syndrome and Sensory Processing: A Conceptual
Model and Guidance for Intervention Planning. Focus
on Autism and Other Developmental Disabilities,
17(3), 172-185.
Dunn, W., Smith Myles, B., & Orr, S. 2002. Sensory
Processing Issues Associated with Asperger Syndrome:
A Preliminary Investigation. The American Journal of
Occupational Therapy, 56(1), 97- 102.
Fombonne, E. 2003. Epidemiological Surveys of Autism
and Other Pervasive Developmental Disorders: An
Update. Journal of Autism and Developmental
Disorders, 33(4), 365-382.
Fombonne, E., & Tidmarsh, L. 2003. Epidemiologic data
on Asperger disorder. Child and Adolescent Psychiatric
Clinics of North America, 12, 15-21.
Khouzam, H. R., El-Gabalawi, F., Pirwani, N., & Priest, F.
2004. Asperger's Disorder: A Review of Its Diagnosis
and Treatment. Comprehensive Psychiatry, 45(3), 184-
191.
Klin, A. 2003. Asperger syndrome: an update. Revista
Brasileira de Psiquiatria, 25(2), 103-109.
Klin, A., & Volkmar, F. 2003. Asperger syndrome:
diagnosis and external validity. Child and Adolescent
Psychiatric Clinics of North America, 12, 1-13.
Klyczek, K., Shriber, L., Timler, G., & Ohtake, P.2005. A
Preliminary Examination of the Sensory and Motor
Performances of Children with Asperger’s Syndrome.
Empire State Physical Therapy, 39, 6A.
Minshew, N., Sung, K., Jones, B., & Furman, J. 2004.
Underdevelopment of the postural control system in
autism. Neurology, 63, 2056-2061.
Nicholas, J., Charles, J., Carpenter, L., King, L., Walter, J.,
& Spratt, E. 2008. Prevalence and Characteristics of
Children with Autism-Spectrum Disorders. Annals of
Epidemiology, 18, 130-136.
The Effectiveness of Sensory Integration Therapy for Children with Asperger’s Syndrome and Pervasive Developmental Disorder-Not
Otherwise Specified: A Case Control Study
279

Palmen, S. J. M., van Engeland, H., Hof, P. R., & Schmitz,
C. 2004. Neuropathological findings in autism. Brain,
127, 2572-2583.
Schaff, R. C., & Nightlinger McKeon, K. 2007.
Occupational Therapy Using a Sensory Integrative
Approach: A Case Study of Effectiveness. The
American Journal of Occupational Therapy, 61(2), 239-
246.
Wahyuni, K.L., & Wardhani, K.R. 2019. Pemeriksaan
Profil Sensori Anak. Jakarta. CV Red Octopus.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
280
