
Effects of Inspiratory Muscle Training using Incentive Spirometer
on Aerobic Capacity, Functional Performance, and Quality of Life
of Individuals with Chronic Paraplegia from Spinal Cord Injury:
A Pilot Study
Nita Theresia Reyne
1
, Farida Arisanti
1
, Vitriana Biben
1
, Indriati M. S. Tobing
2
, Rosiana Pradanasari
2
1
Departement of Physical Medicine and Rehabilitation, Dr. Hasan Sadikin General Hospital,
University of Padjadjaran, Bandung, Indonesia
2
Departement of Physical Medicine and Rehabilitation, Fatmawati General Hospital,
University of Indonesia, Jakarta, Indonesia
Keywords: Inspiratory Muscle Training, Maximal Inspiratory Pressure, Functional Capacity, Quality of Life, Paraplegia.
Abstract: In spinal cord injury (SCI), partially or fully denervated inspiratory or expiratory muscles have impaired
contractility and exhibit diminished exercise ventilation and ventilatory reserve. Inspiratory muscle
training (IMT) using an incentive spirometer (IS) improve lung functions in individuals with chronic SCI.
This study aimed to investigate the effects of IMT-using-IS on the aerobic capacity, the functional
performance, and QoL individuals with chronic paraplegia. The quasi-experimental with the pre-post
design conducted at Sasana Bina Daksa Budi Bhakti Pondok Bambu Jakarta in January-February 2019.
The outcomes were the aerobic capacity measured with the 6-Minutes Push Test (6MPT), the functional
activities daily living (ADL) performance with the Spinal Cord Independence Measure III (SCIM III), and
QoL with International SCI Data Sets-Quality of Life Basic Data Set. There were 11 individuals with
chronic paraplegia recruited. After the IMT-using-IS 5 times per weeks for 4 weeks, there were
significant increases in the 6MPT (p=0.002), and the QoL score (p=0.004), however the SCIM scores
were not significantly different (p=0.271). Individuals with chronic paraplegia, the IMT-using-IS
significantly improved aerobic capacity and QoL. There was no effect on functional performance in ADL
as individuals with chronic paraplegia had already reached their highest level in performing ADL.
1 INTRODUCTION
Respiratory dysfunction frequently occurs in
individuals with spinal cord injury (SCI) due to the
loss of autonomic and somatic nerve control
resulting in complete or partial paralysis of the
respiratory muscles. Respiratory dysfunction
resulting from SCI remains a major cause of
morbidity, mortality, and economic burden (Kumar,
2016; Schilero et al, 2009; Sheel et al, 2008; Sisto
and Evan, 2014).
Respiratory muscle dysfunction in SCI leads to
mechanical alterations in inspiration which results in
decreased compliance of the lungs and chest wall.
This is due to the disruption of muscle strength of
the primary inspiratory muscles, the diaphragm, and
external intercostal muscle. The decreased
abdominal muscle function disrupts mechanical
respiration as well. Abdominal muscles play an
important role during inspiration through their tonic
activity, directly facilitating diaphragm muscle
contraction by preventing excessive contraction
during inspiration. In addition, the increased
intraabdominal pressure yielded by the abdominal
muscle contraction during expiration prepares the
respiratory system for the next inspiration by
optimizing the diaphragm muscle length-tension
(Berlowitz and Tamplin, 2013; Galeiras, 2013;
Schilero et al, 2009; Sheel et al, 2018).
Individuals with chronic SCI frequently
experience an alteration in ventilation, becoming
restrictive. The weak abdominal muscles and the
Reyne, N., Arisanti, F., Biben, V., Tobing, I. and Pradanasari, R.
Effects of Inspiratory Muscle Training using Incentive Spirometer on Aerobic Capacity, Functional Performance, and Quality of Life of Individuals with Chronic Paraplegia from Spinal Cord
Injury: A Pilot Study.
DOI: 10.5220/0009088001970203
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 197-203
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
197

inability of deep inhalation cause increased
abdominal compliance and chest cavity stiffness
which results in the formation of a restrictive
respiratory pattern. This respiratory pattern will
reduce the ability to produce maximum minute
ventilation, then inhibit maximum oxygen uptake
(VO2 max), and ultimately limit physical activity
performance (Battikha et al, 2014). In addition, SCI
causes a loading shift from lower extremity to
upper extremity during exertion. Muscles in the
upper extremity are not weight-bearing muscles and
can only bear 60% of the workload compared to
lower extremity muscles, thus, causing early fatigue
in SCI patients. Inspiratory muscle dysfunction
decreases aerobic capacity, level of physical
activity, and moreover, leads to physical
deconditioning and decreased the independence and
performance in activities daily living (ADL) among
individuals with SCI (Berlowitz and Tamplin,
2013; Sisto and Evan, 2014). Physical exercise
represents an important therapeutic part of
successful mobility advancement and contributes
greatly to a rehabilitation process aiming at self-
determination and autonomy. Therefore, it also has
a great impact on quality of life (QoL) (Anneken et
al, 2010)
Respiratory muscle training is specific training
inspiratory, expiratory, or both muscles to increase
both muscles strength and endurance. There were
numbers of respiratory muscle training using in SCI
management, one of them was resistive inspiratory
muscle training (IMT). Various systematical reviews
showed improvement in lung function and
respiratory muscle strength in individuals with SCI
after training using resistive IMT technique. The
problem is that determining the intensity of resistive
IMT requires maximum inspiratory pressure (MIP)
measurement using a respiratory pressure meter
(RPM), in which the availability in Indonesia is
scarce and the price is quite expensive. Other
respiratory training methods were using an incentive
spirometer (IS). It is a device used in inspiratory
training which provides feedback when a patient
inhales a predetermined flow or volume and
maintains inhalation for at least five seconds. This
device is inexpensive, easy to apply and superior in
providing a visual feedback during training
compared to the resistive IMT. However, there are
no specific methods, frequency, and duration of
training recommended for pulmonary rehabilitation
in SCI, and thus, further studies are required. Prior
studies investigating IMT-using-IS with a frequency
of 5 times/week and duration of 8 weeks in chronic
paraplegia and tetraplegia SCI phase had shown
improvement in lung functions; however, its effect
to functional performance remains unknown
(Berlowitz and Tamplin, 2013; Kim et al, 2017;
Paiva et al, 2015).
This study was conducted to investigate the
effects of IMT-using-IS on aerobic capacity,
performance in ADL, and QoL of individuals with
chronic paraplegia from SCI.
2 METHODS
The quasi-experimental with the pre-post design was
conducted at Sasana Bina Daksa Budi Bhakti
Pondok Bambu Jakarta in January-February 2019.
Inclusion criteria for the participants were:
individuals with paraplegia from SCI more than six
months, age around 18 to 59 years, a stable spine,
being able to sit for 30 minutes and performing
voluntary ventilation; having the MMSE score more
than 24, the Hamilton Depression score less than 19,
no history of pulmonary disease or respiratory
symptoms, no any recent or active pulmonary
infection, and not receiving medication known to
alter airway tone. They were excluded if they could
not perform deep breathing due to pain or taking an
opiate, having a vital capacity of less than 10 mL/kg.
They will be dropped out from the study if they did
not perform the exercise in 72 hours, wanted to quit
from the study, and had unstable medical conditions
(Kim et al, 2017). All participants gave written
informed consent. The protocol was approved by the
Research Ethics Committee of Universitas
Padjadjaran, Bandung, Indonesia with registration
number 0318050788.
The primary outcomes measured were aerobic
capacity, performance in ADL, and QoL. The
secondary outcomes were lung function and
inspiratory muscle strength. Measurements were
administered before and after the intervention
period.
The aerobic capacity was determined with 6MPT
based on the American Thoracic Society guidelines
(Cowan, Callahan and Nash, 2012). The participants
were tested in their wheelchair. The ability to do
ADL and the QoL were assessed with
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
198

Figure 1: Inspiratory muscle training with incentive
spirometer.
questionnaires, the SCIM III and the International
SCI Data Sets-QoL Basic Data Set, respectively.
(Catz et al, 2007; Charlifue et al, 2012). Lung
function was measured with a spirometer MicroLab
ML3500 M5 (Amplivox, Birmingham, USA) by a
skilled nurse. Three repeated flow volume curves
were performed. Outcomes that analyzed was the
score of the trial with the highest value of three close
test readings (Miller et al, 2005). Respiratory muscle
strength was determined with MIP by using a Micro
RPM (CareFusion, Yorba Linda CA, USA). The
highest value of three maneuvers that varied less
than 5% from the next value was recorded and used
for analysis (Postma et al, 2014).
In this study, an incentive spirometer (Voldyne®
5000 volumetric exerciser, Hudson RCI, Temecula
CA, USA), was used for IMT. All measurements
and exercise, except lung function, were conducted
by a physician. The participants were instructed to
hold the spirometer in an upright position, exhaled
normally, and then placed the lips tightly around the
mouthpiece. The next step was a slow inhalation to
raise the piston/plate (volume-oriented) in the
chamber to the set target (Figure 1). At maximum
inhalation, the mouthpiece is removed, followed by
a breath-hold and normal exhalation (Restrepo et al,
2011). All subjects completed 20 supervised training
sessions, 5 times a week for 4 consecutive weeks. A
total of five sets of 10 repetitions made up one
session. After each set, a one-minute rest was
allowed. If participants complained of fatigue or
dizziness during the If participants complained of
fatigue or dizziness during the respiratory exercise,
they took a short rest and then proceeded with the
exercise. If these symptoms became severe, they
were asked to stop the exercise (Kim et al, 2017).
Data were analyzed using SPSS 24.0 for
Windows (SPSS Inc., Chicago, IL, USA). The
paired T-test and the Wilcoxon signed rank test were
used for statistical analysis.
3 RESULTS
Thirteen paraplegics (12 males, 1 female)
participated in the study, however, only 11
completed the study. Two participants were
excluded because they did not want to continue the
study due to personal reason. No complication was
reported. Demographic data and characteristics of
the participans were shown in Table 1.
The demographic characteristics of this study
subjects were dominated by the male (90.9%),
underweight (63.6%), and had the same average and
median age (44 years). Other factors affecting
respiratory function assessment are cigarette
smoking, level of injury, and comorbid respiratory
system diseases, such as post-tuberculosis
obstruction syndrome, pneumonia, chronic
obstructive pulmonary disease, and asthma. About
81.8% of research subjects were smokers with
filtered cigarettes, about 4–8 cigarettes per day, for
20 years on average. Based on the Brinkmann Index,
they were classified into mild active smokers and
they did not show signs and symptoms of respiratory
obstruction at the time of the study. Their clinical
conditions were consistent with the results of
spirometry without bronchodilators: mild-moderate
or normal restrictive, averagely. Based on history
and physical examination, neither the history nor the
presence of active respiratory system diseases were
found, including subjects who had the etiology of
SCI i.e. spondylitis tuberculosis.
From table 2, the distance of 6MPT (p=0.002)
and the QoL score increased (p=0.008) are
improving, however, the SCIM III score did not
show any significant improvement (p=0.271),
although the participants mentioned that performing
ADL and work was easier, lighter and/or faster after
the study ended. There were significant
improvement on lung function, FVC (p=0.005) and
FEV1 (p=0.007), as well as the MIP (p=0.0001). It
proved that respiratory training using IS not only
improves the lung function but also able to increase
the inspiratory muscle strength.
Effects of Inspiratory Muscle Training using Incentive Spirometer on Aerobic Capacity, Functional Performance, and Quality of Life of
Individuals with Chronic Paraplegia from Spinal Cord Injury: A Pilot Study
199
Table 1: Characteristics of subjects.
Variables n=11
Age (year-old) 44.27±7.69
Gender (male/female) 10(90.9%)/1(9.1%)
Bodyweight (kilogram) 51.09±6.64
Body height (centimeter) 165.09±5.90
BMI 18.72±2.17
Underweight 7(63.6%)
Normal 3(27.3%)
Overweight 1(9.1%)
Vocational
Craftsman 10(90.9%)
Mechanic 1(9.1%)
Smoking status 9(81.8%)
Duration of SCI (months) 259.63±104.37
AIS classification (Com/Inc) 10(90.9%)/1(9.1%)
Lesion Level
T2-T11 8(72.7%)
T12-L3 3(27.3%)
Respiratory Comorbid 0(0.0%)
MMSE>24 11(100%)
Severe depression 0(0%)
Categoric data are expressed as number/frequency and percentage, numerical data as mean ± standard deviation. BMI, body
mass index; AIS, American Spinal Injury Association Impairment Scale; T, thoracic; L, lumbar.
4 DISCUSSIONS
The demographic data is consistent with the existing
epidemiology data in Indonesia that reported the
majority of SCI patients were young adult males of
productive age (Departemen Rehabilitasi Medik
RSUP Fatmawati, 2015). The National Spinal Cord
Injury Statistical Center Data in Birmingham
reported that men and women ratio was 4:1, with
average age of 27 years and highest occurrence at
the age of 19 years (National Spinal Cord Injury
Statistical Center, 2016). The results of respiratory
function are influenced by several variables such as
age, height, and sex, thus, they could become the
confounding factors in this study (Kim et al, 2017).
However, these confounding factors had been
minimized in this study. SCI lesions in this study
were dominantly complete lesions (according to the
American Spinal Injury Association Impairment
Scale criteria), most injuries were in the level of T2-
T11, and the highest is T5; or they could be
classified as high paraplegia where the nervous
system disorders affected the respiratory muscles,
both inspiratory (especially the muscles of chest
wall), and expiratory muscles (McConell, 2013).
The most frequently used method for assessing
physical activity is self-report by questionnaire.
However, the existing questionnaire is not sensitive
to the SCI population because it does not calculate
ambulation using a wheelchair as in most individuals
with SCI. The existing self-reports in the disabled
population do not assess an important part of
physical activity as well, i.e. intensity. The PARA-
SCI, a specific self-report of the SCI population, is
still developed (Ginis et al, 2005).
The level of
activity of all research subjects tended to be similar,
i.e. ADL and working. Most of the study subjects
were craftsmen and spent their leisure time by
browsing online and singing. MMSE results showed
all the subjects could follow the instruction of the
exercise. Hamilton Depression results showed no
depression that could interfere the exercise
compliance.
Respiratory muscle dysfunction in SCI,
especially in those with tetraplegic, leads to
mechanical alteration in the inspiratory process
which results in decreased breathing efficiency,
reduced maximum static respiratory pressure, the
inability of inhalation and reduced lung volume.
These can be measured by FVC, FEV
1
, and MIP.
The FVC, FEV
1
and MIP values in tetraplegia and
paraplegia (both high and low paraplegia) were
proven to be lower than the predicted value of able-
bodied population (Berlowitz and Tamplin, 2013;
Schilero et al, 2009; Sheel et al, 2008).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
200
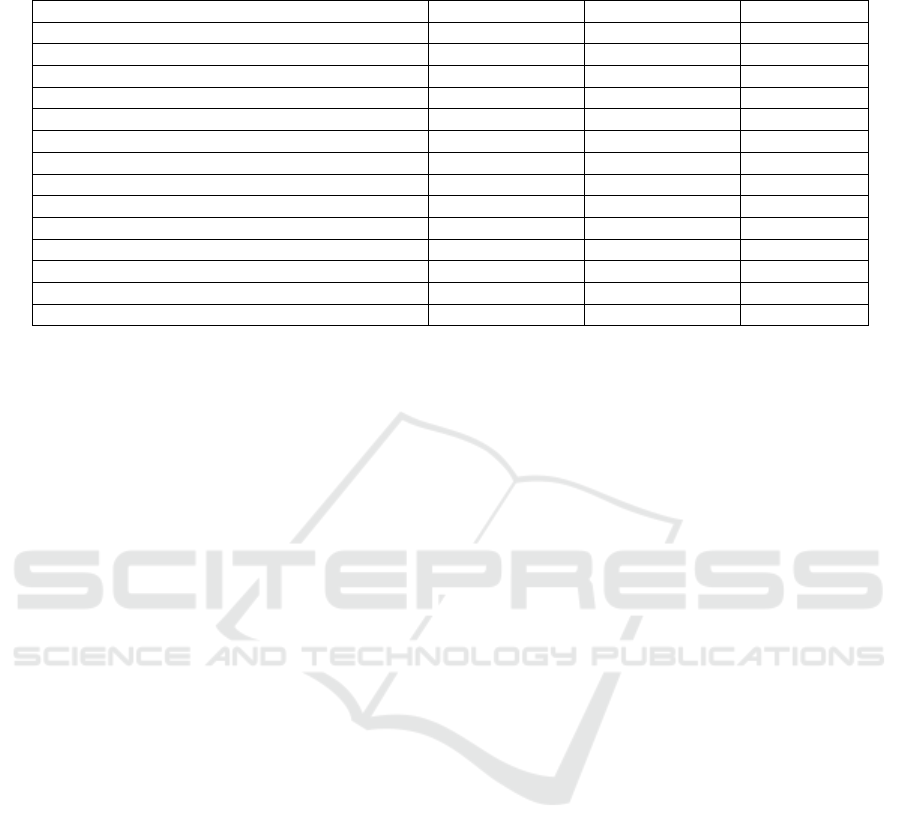
Table 2: Comparison of lung function, inspiratory muscle strength, aerobic capacity, independence in ADL, and QoL pre-
and post-intervention
.
Variables Pre- (n=11) Post- (n=11) p value
Lung function
FVC (liter) 2.32±0.55 2.59±0.62 0.005**
FEV
1
(liter) 2.16±0.59 2.40±0.65 0.007**
MIP (cm H
2
0) 43.81±2.48 52.72±5.78 0.0001**
6MPT (meter) 390.63±57.59 477.72±76.60 0.002**
SCIM III scores
Self-care 20.00 20.00 1.000
Respiration and sphincter management 33.54±4.52 34.00±4.44 0.138
Mobility 17.72±1.55 17.72±1.61 1.000
Total 71.27±4.00 71.72±3.90 0.271
QoL
General QoL (overall well-being) 5.54±1.507 6.54±1.368 0.008**
Rating of physical health 5.27±0.786 6.63±1.026 0.004**
Satisfaction with psychological health 5.36±0.924 6.81±0.981 0.004**
Mean ± SD **p value<0,05: statistically significant different. SD: Standard Deviation; FVC: Forced Vital Capacity; FEV
1
:
Forced Expiratory Volume in 1 minute; MIP: Maximal Inspiratory Pressure; 6MPT: 6-Minutes Push Test; SCIM III:
Spinal Cord Independence Measure III; QoL: Quality of life
2013;
Similar results appeared in this study with an
average predictive value of 67% when compared to
able-bodied population. These lung function results
were following the average pre-intervention MIP.
Based on the calculation of the predictive respiratory
muscle strength in able-bodied population by Evans
and Whitelaw (2009), the predicted MIP in
individuals with SCI was shown below normal
(68.6–101.96 cmH
2
O). These could be influenced by
the severity (complete/incomplete) and lesion level,
duration of injury, and relatively lower (than able-
bodied individuals) physical activities. The value of
lung function and muscle strength are related to one
another. The pressure yielded during inspiration and
expiration is resulted from the activities of
respiratory, diaphragm, intercostal and abdominal
muscles. An increase in transpulmonary pressure of
1 cm H
2
O will increase lung volume by 200 ml
(Guyton and Hall, 2006). The increased lung volume
results from the increase in respiratory muscle
strength. This principle applies to the IMT-using-IS.
This was evidenced by the statistically significant
increase in post-intervention FVC, FEV
1
and MIP.
Although the current study had a shorter duration,
the results were consistent with the study conducted
by Kim et al. (2017), which reported an increase in
FVC and FEV
1
after administration of IMT-using-IS
and abdominal drawing-in for 8 weeks. May be the
difference is the gain of improvement of lung
function. The increased skeletal muscle strength due
to physical exercise occurs, especially, within the
first 2 weeks of exercise, precedes an increase in
muscle mass (Johnson, Sharpe and Brown, 2007).
Previous study has shown that paraplegic and
tetraplegic subjects have more restricted pulmonary
and cardiovascular responses to exercise and
significantly lower peak oxygen consumption and
minute ventilation than uninjured controls. It has
also been suggested that the loss of function of the
abdominal muscles, especially in individuals with an
injury level above T7, can limit the ability to meet
increasing expiratory requirements that occur in
moderate to intense activities. It might be the reason
that inspiratory and expiratory pulmonary deficits
consequent to SCI impair ventilation during exercise
and contribute to the lower peak oxygen
consumption
; however, it could be improved by
training (Battikha et al, 2014). Assessing the
wheeling distance for 6MPT is an easy, validated
way to measure aerobic capacity in individuals with
SCI (Cowan, Callahan and Nash, 2012). This study
showed a statistically significant increase in 6MPT
before the intervention (390.63±57.59 meters) and
after the intervention (477.72 ±76.60 meters).
The effect of IMT on exercise tolerance and/or
performance in SCI is less clear.
In able-bodied
individuals, IMT may reduce the severity of
respiratory and/or locomotor muscle fatigue by
attenuating or delaying the respiratory muscle
metaboreflex. In SCI, it is unclear if exercise
imposes sufficient stress to induce a respiratory
muscle metaboreflex. Although the mechanisms
underlying the increase in VO
2
peak remain elusive,
some researchers speculate that increased aerobic
capacity may be caused by an increase in diaphragm
strength and/or a change in rib-cage configuration.
Effects of Inspiratory Muscle Training using Incentive Spirometer on Aerobic Capacity, Functional Performance, and Quality of Life of
Individuals with Chronic Paraplegia from Spinal Cord Injury: A Pilot Study
201

Conceivably, both changes may result in a greater
circulatory pump action of the diaphragm and/or
prevention of the transition to a predominant rib-
cage contribution to inspiration during the latter
stages of exercise, which may have the net effect of
increasing venous return, stroke volume, and O
2
delivery. It is equally possible, however, that any
improvements in aerobic performance may occur by
way of relieving the sensation of respiratory
discomfort (Taylor, 2016).
The functional ability and performance in SCI
depends on several factors, such as level of injury,
muscle strength, aerobic capacity, and motivation.
The administration of IMT is expected to increase
aerobic capacity, and ultimately improve functional
performance in individuals with SCI. The SCIM III
questionnaire is a tool for evaluating the level of
independence in ADL comprehensively in
individuals with SCI. The pre-intervention self-care
subscale of SCIM III in this study had reached the
maximum score (100%), indicating that all study
subjects had fully rehabilitated, and were able to
perform self-care independently. Respiration and
sphincter management subscale scored had reached
its maximum value, indicating that the study
subjects were breathing independently and had fully
rehabilitated for bowel bladder management.
However, the extent to which lung function, will
affect aerobic capacity in individuals with SCI is
below the normal range of able-bodied individuals.
This is primarily influenced by the severity and level
of SCI lesion, as well as relatively lower (than able-
bodied individuals) physical activities which
worsens respiratory capacity and ultimately affects
the aerobic capacity in individuals with SCI
(Anneken et al, 2010; Taylor, 2016). The mobility
subscale had reached the maximum score, while
others could still be improved by IMT intervention,
as seen in this study, although the improvements
were not statistically significant. The statistically not
significant difference in the results of SCIM III was
due to the high score of pre-intervention results,
called the ceiling effect. We propose International
Spinal Cord Injury Data Sets-Activities and
Participation Basic Data Set, which has a
performance ratings provide insight in the actual
functioning of persons with SCI in the rehabilitation
setting or in the community and
the point of view of
perceived difficulty or satisfaction with
performance; or, Comprehensive ICF Core Set for
Spinal Cord Injury-chronic situation, which has a
qualifier.
Although the results of SCIM III in this study
were statistically not significant, some subjects
reported improvement after the intervention. Most of
them found it easier, lighter and/or faster when
doing ADL, thus, they were more motivated to do
ADL. Two subjects who previously complained
neuropathic pain associated with SCI reported that
the pain was reduced by the third week of training.
A study conducted by Hicks et al. (2003) reported
that training could improve the psychological well-
being of populations with SCI, such as reducing pain
and depression. This was evidenced by the
statistically significant increase in the value of The
International SCI data sets for QoL, which consisted
of general QoL (overall well-being), rating of
physical health, and satisfaction with psychological
health. QoL is an important aspect of a complete
outcome evaluation to document the effects of
rehabilitation for persons with disabilities, including
those with SCI. SCI event is unexpected and
dramatically alters the course of an individual’s life.
It causes sudden, often devastating damage to the
central nervous system, with potential adverse
effects in multiple body systems. Individuals with
SCI must relearn basic skills such as eating, bathing,
dressing, and driving. Living with SCI may also
require the use of adaptive technologies such as
manual or power wheelchairs, all of which greatly
affect QoL. Individuals with SCI also often have to
cope with altered social roles and psychiatric
comorbidities including reactive depression and
anxiety disorders. These issues represent major
challenges to living with SCI. Therefore, anything
we can do for the QoL of an individual with SCI is
worth it (Tulsky et al, 2015). As well as the
experience in this study, although they were chronic
cases that could cope with SCI, they should be
persuaded for the exercise.
The limitation of this study was that the detailed
physical activity of subjects, as a potential
confounding factor, was not recorded and assessed
due to the lack of a questionnaire that could
accommodate the activities of individuals with SCI.
We suggest future studies with a large sample and/or
different research designs (randomized controlled
clinical trials). We also suggest future studies
focusing on subacute phase SCI to assess the effect
of IMT on improving the functional training
performance, shortening the length of stay, and
reducing treatment cost.
5 CONCLUSIONS
Individuals with chronic paraplegia from SCI often
survived with a lot of functional disabilities
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
202

including respiratory that can lead to physical
inactivity and deconditioning that affect the QoL.
Our study shows that the inspiratory muscle training
with an incentive spirometer 5 sets of 10 repetitions
per day, 5 days per week for 4 consecutive weeks,
could improve lung function, inspiratory muscle
strength, increase aerobic capacity and quality of
life, but not functional of individuals with chronic
paraplegia from SCI that had fully rehabilitated.
Therefore, it is encouraged to add IMT-using-IS in
the management of chronic SCI to improve aerobic
capacity and QoL.
REFERENCES
Anneken V, Hanssen-Doose A, Hirschfeld S, Scheuer T,
Thietje R. 2010. Influence of physical exercise on
quality of life in individuals with spinal cord injury.
Spinal Cord; 48: 393–399.
Battikha M, Sà L, Porter A, Taylor JA. 2014. Relationship
between pulmonary function and exercise capacity in
individuals with spinal cord injury: Am J Phys Med
Rehabil; 93: 413–421.
Berlowitz DJ, Tamplin J. 2013. Respiratory muscle
training for cervical spinal cord injury. Cochrane
Database Syst Rev: 1-42.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks
C, Laramee MT, et al. 2007. A multicenter
international study on the Spinal Cord Independence
Measure, version III: Rasch psychometric validation.
Spinal Cord; 45: 275–291.
Charlifue S, Post MW, Biering-Sorensen F, Catz A,
Dijkers M, Geyh S, et al. 2012. International Spinal
Cord Injury Quality of Life BasicData Set. Spinal
Cord; 50: 672–675.
Cowan RE, Callahan MK, Nash MS. 2012. The 6-min
push test is reliable and predicts low fitness in spinal
cord injury: Med Sci Sports Exerc; 44: 1993–2000.
Departemen Rehabilitasi Medik RSUP Fatmawati. 2015.
Data Pasien Rawat Jalan dan Inap Departemen
Rehabilitasi Medik RSUP Fatmawati Periode Januari-
December 2013-2014. DRM RSUP Fatmawati:
Jakarta.
Evans JA, Whitelaw WA. 2009. The assessment of
maximal respiratory mouth pressures in adults. Respir
CARE; 54: 12.
Galeiras VR, Rascado SP, Mourelo FM, Montoto MA,
Ferreiro VME. 2013. Respiratory management in the
patient with spinal cord injury. BioMed Res Int; 2013:
1–12.
Ginis KAM, Latimer AE, Hicks AL, Craven BC. 2005.
Development and evaluation of an activity measure for
people with spinal cord injury: Med Sci Sports Exerc;
37: 1099–1111.
Guyton AC, Hall JE. 2006. Pulmonary ventilation. In:
Textbook of medical physiology. 11th Ed.
Philadelphia: Elsevier Saunders pp 471-6.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C,
Bugaresti J, et al. 2003. Long-term exercise training in
persons with spinal cord injury: effects on strength,
arm ergometry performance, and psychological well-
being. Spinal Cord; 41: 34–43.
Johnson MA, Sharpe GR, Brown PI. 2007. Inspiratory
muscle training improves cycling time-trial
performance and anaerobic work capacity but not
critical power. Eur J Appl Physiol; 101: 761–770.
Kim CY, Lee JS, Kim HD, Lee DJ. 2017. Short-term
effects of respiratory muscle training combined with
the abdominal drawing-in maneuver on the decreased
pulmonary function of individuals with chronic spinal
cord injury: A pilot randomized controlled trial. J
Spinal Cord Med; 40: 17–25.
Kumar N. 2016. Respiratory care in traumatic spinal cord
injury. J Spine; 01.
McConnell A. 2013. Respiratory muscle training.
Edinburgh: Churchill Livingston
Miller MR. 2005. Standardization of spirometry. Eur
Respir J; 26: 319–338.
National Spinal Cord Injury Statistical Center. 2016.
Spinal cord injury (sci) facts and figures at a glance.
Cited from: http://www.nscisc.uab.edu/Public/Facts
2016.pdf on December 10th, 2017.
Paiva DN, Assmann LB, Bordin DF, Gass R, Jost RT,
Bernardo-Filho M, et al. 2015. Inspiratory muscle
training with threshold or incentive spirometry: Which
is the most effective? Rev Port Pneumol Engl Ed; 21:
76–81.
Postma K, Haisma JA, Hopman MTE, Bergen MP, Stam
HJ, Bussmann JB. 2014. Resistive inspiratory muscle
training in people with spinal cord injury during
inpatient rehabilitation: a randomized controlled trial.
Phys Ther; 94: 1709–1719.
Restrepo RD, Wettstein R, Wittnebel L, Tracy M.
Incentive spirometry: 2011. Respir Care; 56: 1600–
1604.
Schilero GJ, Spungen AM, Bauman WA, Radulovic M,
Lesser M. 2009. Pulmonary function and spinal cord
injury. Respir Physiol Neurobiol; 166: 129–141.
Sheel W, Reid WD, Townson A, Ayas N, Konnyu K.
2008. Effects of exercise training and inspiratory
muscle training in spinal cord injury: a systematic
review. J Spinal Cord Med; 31: 500–508.
Sisto SA, Evans N. 2014. Activity and fitness in spinal
cord injury: review and update. Curr Phys Med
Rehabil Rep; 2: 147–157.
Taylor JA. 2016. The physiology of exercise in spinal cord
injury. Massachusetts: Springer.
Tulsky DS, Pamela A. Kisala PA, Victorson D, Denise
DG, Heinemann AW, et al. 2015. Overview of the
spinal cord injury – quality of life (sci-qol)
measurement system. J Spinal Cord Med; 38 (3): 257-
69.
Effects of Inspiratory Muscle Training using Incentive Spirometer on Aerobic Capacity, Functional Performance, and Quality of Life of
Individuals with Chronic Paraplegia from Spinal Cord Injury: A Pilot Study
203
