
The Effect of Incentive Spirometry on Level of Fatigue and Creatine
Kinase in Chronic Spinal Cord Injury Patients
Rendra Sanjaya Yofa
1
, Farida Arisanti
1
,Vitriana Biben
2
, Indriati M.S Tobing
2
, Rosiana Pradanasari
2
1
Department of Physical Medicine and Rehabilitation, Hasan Sadikin General Hospital,
University of Padjadjaran, Bandung, Indonesia
2
Department of Physical Medicine and Rehabilitation,
Fatmawati General Hospital, Jakarta, Indonesia
!
Keywords: Creatine- Kinase, Fatigue Severity Scale, Inspiratory Muscle Training, Incentive Spirometry, Respiratory
Training, Spinal Cord Injury
Abstract: The reduced ability of the respiratory muscles in Spinal Cord Injury (SCI) patients is associated with the
physical fatigue. Incentive Spirometry (IS) breathing exercise can be used as a strategy to minimize the
fatigue through its effect improving bloodstream and oxygenation on the diaphragm and periphery muscles.
Creatine Kinase (CK) can be used to monitor muscle damage due to exercise or overtraining status. The
study was aimed to investigate the effect of IS on the level of fatigue and CK in blood. A quasi
interventional design with a pre- and posttest approach was done to eleven patients with chronic SCI
patients. It was measured the fatigue level using the Fatigue Severity Scale (FSS) before and after the
treatment. It was also measured the value of CK before treatment and after treatment in 2 and 4 weeks. There
was a significant decline in the FSS value, 35.45±9.699 to 25.36±11.918(p=0.007) after 4 weeks intervention. On
the other hand, there was a significant increase in CK value, from 111. 63±77.628 U/l to 146.36±81.185 U/l
(p=0.033), after 2 weeks intervention. However, it was not significant CK value was to be 127.45±82.117
U/l (p=0.168) after 2 weeks intervention. These findings showed IS breathing exercise after 4 weeks can
improve fatigue level and no muscle damage due to IS exercise in chronic SCI patients.
1 INTRODUCTION
Fatigue becomes one of the concerns in chronic SCI
patients (Lidal, 2013). There are two types of fatigue
following SCI, namely physical fatigue and chronic
fatigue. Physical fatigue is defined as intrinsic
muscular fatigue that occurs in muscles partially or
total paralyzed at the level of or below the spinal
cord lesion. Chronic fatigue is defined as a
debilitating condition involving multiple factors
including physical, psychological and aging
components (Craig, 2012). The incidence of fatigue
in SCI patients varied between 18–57% (Nooijen,
2015; Hammel, 2009).
After SCI, paralyzed skeletal muscle generally
becomes atrophic including respiratory muscle,
possesses lower tension generating capacity and is
less fatigue resistant. Muscle histochemical and
metabolic profile shifts toward type II (fast
glycolytic) fibers have been well documented
following SCI and may explain the problem of rapid
muscle fatigability in SCI survivor (Pola, 2014; Kim,
2017). This may lead to more rapid fatigue of the
respiratory pump in patients with SCI during
physical activity.
The cause of fatigue is probably multifactorial,
but a central role for changes in high-energy
phosphates (i.e., ATP and ADP) or accumulation of
by-products of rapid energy metabolism has been
postulated. A key enzyme for maintaining a constant
ATP/ADP ratio during rapid energy turnover is CK,
which catalyzes phosphate exchange between the
high free energy phosphates ATP and
phosphocreatine (PCr) via the reaction:
PCr + ADP+ H creatine (Cr)+ ATP (1)!
Yofa, R., Arisanti, F., Biben, V., Tobing, I. and Pradanasari, R.
The Effect of Incentive Spirometry on Level of Fatigue and Creatine Kinase in Chronic Spinal Cord Injury Patients.
DOI: 10.5220/0009087901910196
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 191-196
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
191

CK is employed to mark muscle injury that
occurs after an exercise. CK value is primarily used
to know whether there is an overload limit achieved
or instead, muscle adaptation has occurred. Muscle
damage regarding an exercise can occur due to
unaccustomed exercise or heavy exercise intensity.
The increase of CK value is related to the number of
type II muscle fiber in the muscle. As we know that
following SCI, become predominantly composed of
type II muscle fiber. The increase of CK value in
serum significantly occurs in the initial exercise
indicates that the exercise intensity exceeds muscle
capability. Exercise will affect the decrease
elevation of CK when it is done regularly in a
certain period. Such an effect is called a repeated
bout effect, indicating that there is muscle adaptation
towards the exercise. (Soon-Gi, 2015; Margaritelis,
2015).
The effects of respiratory training in SCI patients
are related to increased strength and endurance of
respiratory muscle fitness, as well as reduced
ventilation efforts required during training by the
process of adaptation. Respiratory training also
increases neural adaptation which is required to
coordinate muscle contractions synergistically,
thereby maximizing the respiratory muscle
activation. Increased respiratory muscle strength
directly correlates with reduced muscle fatigue due
to increased training capacity and tolerance, so
inspiratory muscle training (IMT) can be used as a
strategy to minimize respiratory fatigue (Sisto, 2014;
Hartz, 2018).
Incentive Spirometry is one of the assistive
devices of respiratory training which can be used to
maintain maximum inspiration by providing
feedback of predetermined air volume. A study
found that the use of IS in respiratory training with
additional abdominal drawing-in maneuver resulted
in improvement in pulmonary function of a patient
with SCI (Kim, 2017).
Several studies had investigated the effects of
IMT on fatigue. Bosnak-Guclu et al. conducted a
study of IMT using Inspiratory Muscle Trainer in
NYHA II-III congestive heart failure patients and
Turner et al conducted a study on asthma patients.
Both of these studies show positive effect in
reducing the fatigue (Bosnak-Guclu, 2011; Turner,
2011).
In this study, we provide IS breathing exercise to
investigate its effects on the level of fatigue and CK
value on chronic SCI patients in Sasana Bina Daksa
Budi Bhakti, Pondok Bambu, East Jakarta. The
severity of fatigue is assessed by the Fatigue
Severity Scale (FSS) questionnaire. It assesses a
person's perception of fatigue and its use has been
validated in patients with neuromuscular disease.
We hypothesized that IS breathing exercise can
improve fatique level and no more muscle damage
caused by IS breathing exercise after 4 weeks
intervention.
2 METHODS
This study used a quasi-interventional research
design with a pre- and posttest approach. The
samples were recruited from subjects who met the
inclusion criteria in population of chronic SCI
patients who occupied in the Social Care Center of
Sasana Bina Daksa Pondok Bambu, East Jakarta,
Indonesia.
The inclusion criteria are chronic SCI, aged 18 –
59 years old, paraplegic, no acute infection, stable
spinal structure, able to perform breathing muscle
training inspiration procedure for 30 minutes,
Hamilton Depression Score (HDS) less than 20,
Mini Mental State Examination (MMSE) score
between 22–30. Exclusion criteria unable to take a
deep breath due to pain, taking statin drug
and patients with vital capacity <10 mL/kg. The
subjects signed an informed consent to be included
in the study. After each set, a one-minute rest was
allowed.
The subjects signed informed consent in order to
be included in the study. All the subjects were given
respiratory muscle training with IS intensity from
residual capacity to total lung capacity. The IS
breathing exercise prescriptions are 5 days a week,
once a day, with total of five sets, with 10 repetitions
making up one set. After each set, a one-minute rest
was allowed.
The IS training program was conducted after
the subjects were given explanations of the exercise
device, watched a video about the use of the exercise
and familiarizing the device for 2 consecutive days.
To do the exercise, the subjects sat in reclining
chairs with their torso upright. The pulse oxymeter
was pinned to the subject's fingers as a tool to
monitor the general condition during training. The
IS was held with one hand in an upright sitting
position, mouthpiece was placed into the mouth
between the teeth with the lips clamped tightly
around the mouthpiece The subjects maintained a
maximal inspiration position for 3 to 5 seconds, and
then performed maximal expiration. This exercise
was performed for a total of five sets, with 10
repetitions making up one set. After each set, a one-
minute rest was allowed.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
192

The primary endpoint measurements included
fatigue evaluated with the FSS and CK level in
blood. FSS were assessed before and after
intervention, while the CK levels were examined
before intervention, after 2 weeks and 4 weeks
intervention (in 24 hours after exercising).
Numerical data including age were presented
with mean and standard deviations, maximum
values, and minimum values. The subjects’
characteristic data were presented in frequency
distribution tables. Categorical variables were
presented in percentage (%) and continuous
variables were presented in mean ± standard
deviation (SD). Statistical analysis was carried out
by performing normality test to determine that the
data were normally distributed or not normally
distributed.
Data distribution were discovered using the
Shapiro Wilks test since the samples were less than
50. Paired t test was used to compare FSS variables
between before and after the intervention since the
data were normally distributed. Wilcoxon test was
used to compare CK before and after 2 weeks and to
compare before and after 4 weeks intervention since
the data were not distributed normally. Significance
of the statistical test results was determined based on
p value (<0.05). All procedures were performed
using the SPSS for Windows version.
The study was approved by the Ethics
Committee of Padjadjaran University, Bandung,
Indonesia with ethical numbers of 0318050767. All
data and information of the subjects will be kept
confidentially.
3 RESULTS
The study enrolled 11 chronic SCI patients. Mean
age of the subjects was 44 years old. Number of
male subjects (90.9 %) were higher than female
subjects. The subjects had SCI approximately 260
months due to trauma (90. 9%) (Table 1). Most of
the subjects had complete SCI (81.8 %). Based on
body mass index (BMI), the subjects was mostly
underweight (63.6 %) with an average of 18.72
kg/m2 without any other complications of chronic
SCI. Occupation of the subjects was mostly
craftspeople. Eighty one percents of the subjects had
smoking history. In addition, there was no subject
has pressures sore and did not consume medicines
which could influence CK levels. The mean of pre-
and post-training FSS scores were respectively 35.45
± 9.699 and 25.36 ± 11.918. There was a significant
improvement in the FSS after the intervention (table
2, p = 0.007). For The CK value, there was a
significant increase after 2 weeks intervention (table
3, p=0.033), but there was no significant increase
after the 4 weeks intervention (table 4, p =0.168).
4 DISCUSSIONS
From baseline data in table 1, the mean age of the
patient is 44 y.o. with 10 male patients and 1 female
patient. Based on international data, male accounts
for eighty-one percent of new SCI cases and the
average age at injury is 42 years old. In developing
countries, SCI is more frequent in male than female,
with a male: female ratio of 10: 1 to 6.69: 1. The
high incidence of SCI in male is associated with the
higher activity of men in the community, moreover,
men do dangerous activities more frequently than
women (WHO, 2013).
The lower FSS score in our study after four
weeks intervention with IS (Table 2) demonstrated
that the level of fatigue was reduced significantly.
Several studies had investigated the effects of
IMT on fatigue but never been done in individuals
with SCI. Bosnak-Guclu et al. conducted a study of
IMT using Inspiratory Muscle Trainer in NYHA II-
III congestive heart failure patients, dividing the
study subjects into two groups: the treatment group
(receiving 40% dose of MIP) and the control group
(receiving 15% dose of MIP). A statistically
significant (p≤0.0001) reduction in FSS score was
demonstrated in both treatment and control group
(p=0.008). However, the difference in FSS reduction
between these groups was not statistically
significant, indicating that low-dose Inspiratory
Muscle Trainer gives the same effect in reducing
fatigue perceptions. Bosnak-Guclu et al. concluded
that the IMT using Inspiratory Muscle Trainer may
increase peripheral blood flow, peripheral muscle
strength and exercise capacity, thereby reducing the
severity of fatigue in daily activities and training
(Bosnak-Guclu, 2011).
The Effect of Incentive Spirometry on Level of Fatigue and Creatine Kinase in Chronic Spinal Cord Injury Patients
193
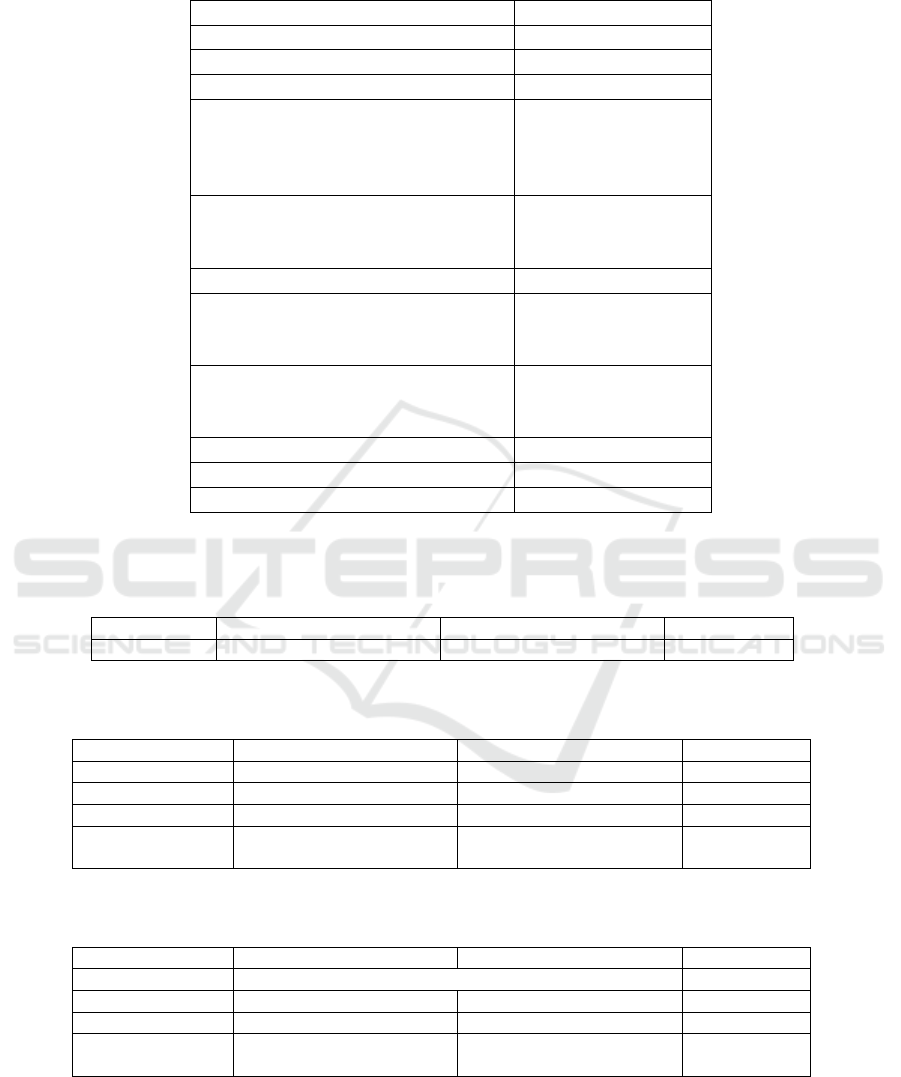
Table 1: Characteristics of subjects.
Variables
n=11
Age (year-old)
44.27±7.695
Gender (male/female)
10 (90.9%) / 1(9.1%)
Bodyweight (kilogram)
51.09±6.64
BMI
Underweight
Normal
Overweight
18.72±2.17
7(63.6%)
3(27.3%)
1(9.1%)
Vocational
Craftsman
Mechanics
10(90.9%)
1(9.1%)
Smoking status
9(81.8%)
Medication
Mecobalamin
No
1(9.1%)
10(90.9%)
Pressure sores history
Yes
No
11(100%)
0(0%)
AIS classification (complete/incomplete)
10 (90.9%) / 1(9.1%)
MMSE>24
11(100%)
HDS<20
11(100%)
Categoric data are expressed as number/frequency and percentage, numeral data as mean±standar deviation. BMI, body
mass index; AIS, American Spinal Injury Association Impairment Scale.
Table 2: Fatigue Severity Scale (FSS) before and after the intervention.
Before Intervention
After Intervention
P value
Mean±SD
35.45±9.699
25.36±11.918
0.007**
**p value<0,05: statistically significant different. SD = Standard Deviation.
Table 3: CK value before and after 2 weeks intervention.
Variable
Before Intervention
2 Weeks after Intervention
P value
CK Value (U/l)
0.033**
Mean±SD
111.63±77,628
146.36±81.185
Median
84.00
145.00
Range
(Min- Max)
53.00-335.00
64.00-321.00
**p value<0,05: statistically significant different. SD = Standard Deviation.
Table 4: CK value before and after 4 weeks intervention.
Variable
Before Intervention
2 Weeks after Intervention
P value
CK Value (U/l)
0.168
Mean±SD
111.63±77.628
127.45±82.117
Median
84.00
119.00
Range
(Min- Max)
53.00-335.00
56.00-338.00
SD = Standard Deviation.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
194

Duruturk et al. conducted a study on asthma
patients. The study subjects were divided into two
groups: the treatment group (receiving a 50% dose
of IMT) for 6 weeks and the control group
(receiving respiratory training only). A significant
reduction in the FSS score was only demonstrated in
the treatment group (p = 0.028). Positive impacts
were also seen in respiratory muscle strength,
exercise capacity and quality of life in asthma
patients. Increased respiratory muscle strength is
believed to have a dyspnea-reducing-effect during
training due to the reduced need for required
oxygen. The reduction of required respiratory effort
leads to the reduction of required energy thereby
reducing the severity of fatigue in a person (Durutur,
2018). The results of our study demonstrated that
respiratory training using IS significantly reduced
the severity of fatigue in individuals with SCI after
four weeks of intervention. Respiratory muscles are
vital and play an important role in performing
training. Having strong, long-lasting respiratory
muscles may increase exercise capacity because they
improve lung function, delay fatigue in respiratory
muscles, and increase blood flow to respiratory
muscle tissues as well as other peripheral muscles.
The association between respiratory muscle function
and fatigue had been investigated by Ray et al. They
investigated the association between respiratory
muscle function and fatigue in 37 multiple sclerosis
patients with mild to moderate disability (still able to
ambulate). There was a negative correlation between
respiratory muscle strength (MIP and MEP) and
fatigue perception using Modified Fatigue Impact
Scale (MFIS) questionnaire (Ray, 2015).
Following the CK value in this study, a
significant statistical increase occurred in this study
after 2 weeks intervention (table 3) and became not
significant statistical increase of CK value after 4
weeks intervention (table 4). This is following the
literature stating that increased CK value usually
happens in the initial weeks of exercise indicating
that the initial exercise intensity is given exceeds
muscle capability. This is based on the exercise
principle that in order to give a strengthening effect,
overload exercise intensity should be given. After 4
weeks intervention, CK value increase occurred
insignificantly. This indicates that there has been
muscle adaptation towards the exercise. Several
works of literature mentioned that muscle adaptation
can occur in the third week of the exercise, depends
on the exercise intensity and muscle condition (Ray,
2015; Magal, 2010).
Research on the effect of exercise on CK value
in blood of SCI patient has been done by Robergs et
al., in 1993. They conducted research on CK and
endothelin level of SCI patient (level C7-L1)
through bicycle exercise added by Functional
Electrical Stimulation (FES). The exercise was done
three a week by comparing the CK enzyme and
endothelin level before the exercise, the first week,
the third week, the sixth week and the twelfth week
of the exercise. There was a significant increase of
CK level each week, however, since the third week
on, the increase of CK was not as much as the first
week. This indicated that muscle adaptation started
in the third week of exercise.
Barroso et al performed research on the effect of
regular elbow flexor eccentric exercise. One of the
markers used was the CK examination. The result of
the research indicated that there was a significant
increase in CK value in the first week, while in the
fourth and sixth week, the increase was less. This is
called a repeated-bout effect mechanism which is the
effect of muscle adaptation towards the exercise.
The repeated-bout effect has a protective effect on
the muscle, thus during such condition, muscle
damage will not happen, or even it happened, the
effect will be minimal. Repeated-bout effect
involved a combination of neural, mechanical and
adaptation of cellular. Barroso et al concluded that
there was protection effect towards the effect of
myofibril structure so that it will prevent the
occurrence of muscle damage in the fourth week
(Barroso, 2010). Research conducted by Chen et al
indicated that there was significant muscle damage
for the first two weeks of elbow eccentric exercise,
and it started to decrease in the third week. After the
fourth week of the exercise, the effect of muscle
damage became insignificant. This can be explained
by the occurrence of neural adaptation in the form of
motor unit recruitment efficiency, firing
synchronization increase from the motor unit and the
increase of low type muscle fiber ratio (Chen, 2009).
The limitation of this study did not assess several
factors that may influence the level of fatigue such
as pain, sleep problem, nutrition, the effort of
coping, activity level and spasticity severity.
5 CONCLUSIONS
Four-week respiratory training with IS was effective
at reducing the severity of fatigue in individuals with
SCI. This study also obtained results that there was
no significant increase in the value of CK after 4
week intervention which indicates that the muscles
have adapted to exercise so that there is no longer
any effect of muscle damage due to exercise. Thus,
The Effect of Incentive Spirometry on Level of Fatigue and Creatine Kinase in Chronic Spinal Cord Injury Patients
195

respiratory training with IS was one of the safety and
effective strategies to reduce fatigue in individuals
with SCI.
REFERENCES
Barroso R, Roschel H, Ugrinowitsch C, Arau´jo R,
Nosaka K, Tricoli V. 2010. Effect of eccentric
contraction velocity on muscle damage in repeated
bouts of elbow flexor exercise. Appl. Physiol. Nutr.
Metab; 35(4): 534–540.
Bosnak-Guclu M, Arikan H, Savci S, Inal-Ince D,
Tulumen E, Aytemir K et al. 2011. Effects of
inspiratory muscle training in patients with heart
failure. Respir Med; 105(11):1671–1681.
Chen TC, Chen HL, Lin MJ, Wu CJ, Nosaka K. 2009.
Muscle damage responses of the elbow flexors to four
maximal eccentric exercise bouts performed every 4
weeks. European Journal of Applied Physiology;
106(2) : 267–275.
Craig A, Tran Y, Wijesuriya N, Middleton J. 2012.
Fatigue and tiredness in people with spinal cord injury.
Journal of Psychosomatic Research; 73(3): 205-210.
Durutur N, Acar M, Doğrul MI. 2018. Effect of
Inspiratory Muscle Training in the Management of
Patients With Asthma: A Randomized Controlled
Trial. Journal of Cardiopulmonary Rehabilitation and
Prevention; 38(3): 198-203
Hammell KW, Miller WC, Forwell SJ, Forman BE,
Jacobsen BA. 2009. Fatigue and spinal cord injury: a
qualitative analysis. Spinal Cord; 47(1): 44–49.
Hartz CS, Sindorf MAG, Lopes CR, Batista J, Moreno
MA. 2018. Effect of Inspiratory Muscle Training on
Performance of Handball Athletes. Journal of Human
Kinetics; 63: 43-51.
Kim CY, Lee JS, Kim HD, Lee DJ. 2017. Short-term
effect of respiratory muscle traineing combined with
the abdominal drawing-in maneuver on the decreased
pulmonary function of individuals with chronic spinal
cord injury: A pilot randomized controlled trial. The
Journal of Spinal Cord Medicine; 40(1): 17-25.
Lidal IB, Jensen AE, Larsen TW, Stanghelle JK. 2013.
Fatigue in persons who have lived with spinal cord
injury for >20 years. Spinal Cord; 51(2): 103 -108.
Magal M, Dumke CL, Urbiztondo ZG, Cavill MJ, Triplett
NT, Quindry JC et al. 2010. Relationship between
serum creatine kinase activity following exercise-
induced muscle damage and muscle fibre composition.
Journal of Sports Sciences; 28(3): 257–266.
Margaritelis NV, Theodorou AA, Baltzopoulos
V, Maganaris CN, Paschalis V, Kyparos A et al. 2015.
Muscle damage and inflammation after eccentric
exercise: can the repeated bout effect be removed?
Physiol Rep; 3(12): 1-12.
Nooijen CF, Vogels S, Bongers-Janssen HM, Bergen
MP, Stam HJ , van den Berg-Emons HJ. 2015. Fatigue
in persons with subacute spinal cord injury who are
dependent on a manual wheelchair. Spinal Cord;
53(10): 758–762.
Polla B, D’Antona G, Bottinelli R, Reggiani C. 2014.
Respiratory muscle fibres: specialisation and
plasticity. Thorax; 59(9): 808–817.
Ray AD, Mahoney MC, Fisher NM. 2015. Measures of
respiratory function correlate with fatigue in
ambulatory persons with multiple sclerosis. Disabil
Rehabil; 37(26): 2407 - 2412.
Sisto SA, Evans N. 2014. Activity and Fitness in Spinal
Cord Injury: Review and Update. Current Physical
Medicine and Rehabilitation Report; 2(3): 147–157.
Soon-Gi B, Do-Jin K. 2015. Effect of Low Intensity
Aerobic Exercise and Postural Correction Exercise on
Fatigue Substance and Aging Hormone. Indian Journal
of Science and Technology; 8(27) :1-4.
Turner LA, Mickleborough TD, McConnell AK, Stager
JM, Tecklenburg-Lund S, Lindley MR. 2011. Effect of
inspiratory muscle training on exercise tolerance in
asthmatic individuals; 43(11): 2031-2038.
World Health Organization. 2013. International
perspective on spinal cord injury. Malta: WHO
Library Cataloguing-in-Publication Data.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
196
