
The Effect of Additional Inspiratory Muscle Strengtening on Aerobic
Exercise in Systemic Lupus Erythematosus: A Preliminary Study
Zayadi Zainuddin
1,2
, Marina Moeliono
1
, Novitri
1
, Laniyati Hamijoyo
3,4
, Irma Ruslina Defi
1
1
Physical Medicine and Rehabilitation Departement, Medical Faculty of Universitas Padjajaran, Bandung, Indonesia
2
Medical Program Study, Medical Faculty of Universitas Bengkulu, Bengkulu, Indonesia
3
Rheumatology Division, Internal Medicine Departement, Medical Faculty of Universitas Padjajaran, Bandung, Indonesia
4
Lupus Study Group, Imunology Study Centre, Medical Faculty of Universitas Padjajaran, Bandung, Indonesia
zay_adi@yahoo.co.id, mmmoeliono@yahoo.com, novitris@gmail.com, hamijoyo@yahoo.com, irmaruslina@gmail.com
Keywords: Inspiratory Muscle Strengthening, Aerobic Exercise, Systemic Lupus Erythematosus
Abstract: Background: Aerobic exercise, an effective and safe nonpharmacological treatment for systemic lupus
erythematosus (SLE), does not prevent muscle strength decline that has been proven to be predictor of
decreased functional capacity. A decrease of inspiratory muscle strength had been demonstrated in SLE.
This study aimed to explore the effect of adding inspiratory muscle strengtening (IMS) to aerobic exercise
in SLE patients. Method: A quasi experimental study with pre-post test was conducted. Study sample was
11 patients low lupus activity disease state (LLDAS), age 20-50 years, normal body mass index.
Interventions were aerobic exercise (3 times/week, moderate intensity, 20 minutes, using treadmill) and
IMS (3 times/week, low intensity, using respironic tresshold). The outcomes were inspiratory and handgrip
muscle strength, cardiopulmonal and handgrip muscle endurance. Results: The median of inspiratory
muscle strength (49.66 vs 65.00 cmH
2
O) and handgrip (11.00 vs 14.67 kilograms) increased (P<0.005)
significantly prior compared to after exercise. The median of cardiopulmonary endurance (432.00 vs 480.00
meters) also increased (P<0.005) significantly but not handgrip muscle endurance (1.50 vs 2.36 minutes).
Conclusion: The addition of inspiratory muscle strengtening to aerobic exercise did not only increase
cardiopulmonary function but also handgrip muscle strength which is usefull in daily activities.
1 INTRODUCTION
The decrease in physical fitness is common in
systemic lupus erythematosus (SLE). Balsamo et al.
showed that SLE patients walked shorter distances
on the six minute walking test (6MWT) and were
significantly associated with lower quality of life
(Balsamo, 2013). Another study, conducted by
Spinelli et al showed decreased in aerobic capacity
correlated with decreased cardiopulmonary
endurance of SLE patients (Spinelli et al, 2017).
Decreased skeletal muscle strength had also been
shown in SLE patients. Balsamo et al found that
premenopausal SLE patients with low disease
activity showed lower muscle strength and
functional capacity, and fatigue (Balsamo et al,
2013).
Many studies have been carried out related to
pharmacological and non-pharmacological
management strategies for SLE patients with
(Shaharir and Gordon, 2016). A systematic review
proved that aerobic exercise was an effective and
safe therapy in patients with mild to moderate
activity of SLE (Wu et al, 2017). Other study
showed that aerobic exercise was better than muscle
strengthening exercises in improving the quality of
life of SLE patients, although they still suggest the
addition of muscle strengthening exercises (Abrahão
et al, 2016). Soriano et al pointed out the importance
of muscle strengthening exercises, because lower
muscle strength has been shown to be a predictor of
decreased functional capacity over time in SLE
patients. (Soriano-Maldonado et al, 2016).
Related to the respiratory muscles, Amra et al.
mentioned a decrease in maximal inspiratory
pressure (MIP) and maximal expiratory pressure
(MEP) in SLE patients (Amra et al, 2006). Currently,
there are no study related to IMS exercises in SLE
patients. While IMS exercises has been shown to be
safe and positive effect in health and also other
chronic disease populations such as multiple
sclerosis (Ray et al, 2013), sarcoidosis (Karadall et
162
Zainuddin, Z., Moeliono, M., Novitri, ., Hamijoyo, L. and Defi, I.
The Effect of Additional Inspiratory Muscle Strengtening on Aerobic Exercise in Systemic Lupus Erythematosus: A Preliminary Study.
DOI: 10.5220/0009066701620167
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 162-167
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
al, 2016) and chronic kidney disease (de Medeiros et
al, 2017).
This preliminary study aims to determine the
effect of additional IMS on aerobic exercise in SLE
patients.
2 METHOD
This study design was a quasi experimental with
pre-post test. The study was conducted September
2018-February 2019 at Departement of Physical
Medicine & Rehabilitation, Dr. Hasan Sadikin
General Hospital, Bandung. This study has obtained
ethical approval number
LB.04.01/A05/EC/314/XI/2018 from hospital ethics
committee.
Target population was SLE patients who had
routine medical treatment at Rheumatology Clinic,
Departement of Internal Medicine, Dr. Hasan
Sadikin General Hospital, Bandung. Sampling was
done consecutively. The sample size was obtained
by a 95% confidence level and 90% power of the
test.
Inclusion criteria were female, aged 20-50 years,
low lupus activity disease state (LLDAS) (Franklyn
et al., 2016), normal body mass index, and able to
walk independently. Exclusion criteria were history
of heart and lung disease, surgery on the thoracal
and or abdominal site, involved in aerobic exercise
and/or muscle strengthening in the last 6 months.
Elimination criteria were the subjects did not do
exercise 3 times consecutively for 1 week.
Interventions were aerobic exercise and
inspiratory muscle strengthening 3 times a week in,
12 weeks period. Aerobic exercise was given at
moderate intensity (40% of heart rate reserve/HRR),
20 minutes duration, using treadmill. IMS with a
mild intensity (30% of MIP), 5 sets, 10 repetitions
per set, using respironic tresshold.
Outcomes of this study were inspiratory and
other peripheral muscle (handgrip) strength which
represents strength output, cardiopulmonary and
peripheral muscle (handgrip) endurance which
represents endurance output. Handgrip muscle was
selected because while not directly involved in both
exercises. In addition, handgrip muscles could
represent overall body muscle performance.
Measurement of IMS was performed using a micro
respiratory pressure meter (RPM) and
cardiopulmonary endurance using a 6 minute walk
test (6MWT) while the strength and endurance of
handgrip using a jamar hand dynamometer.
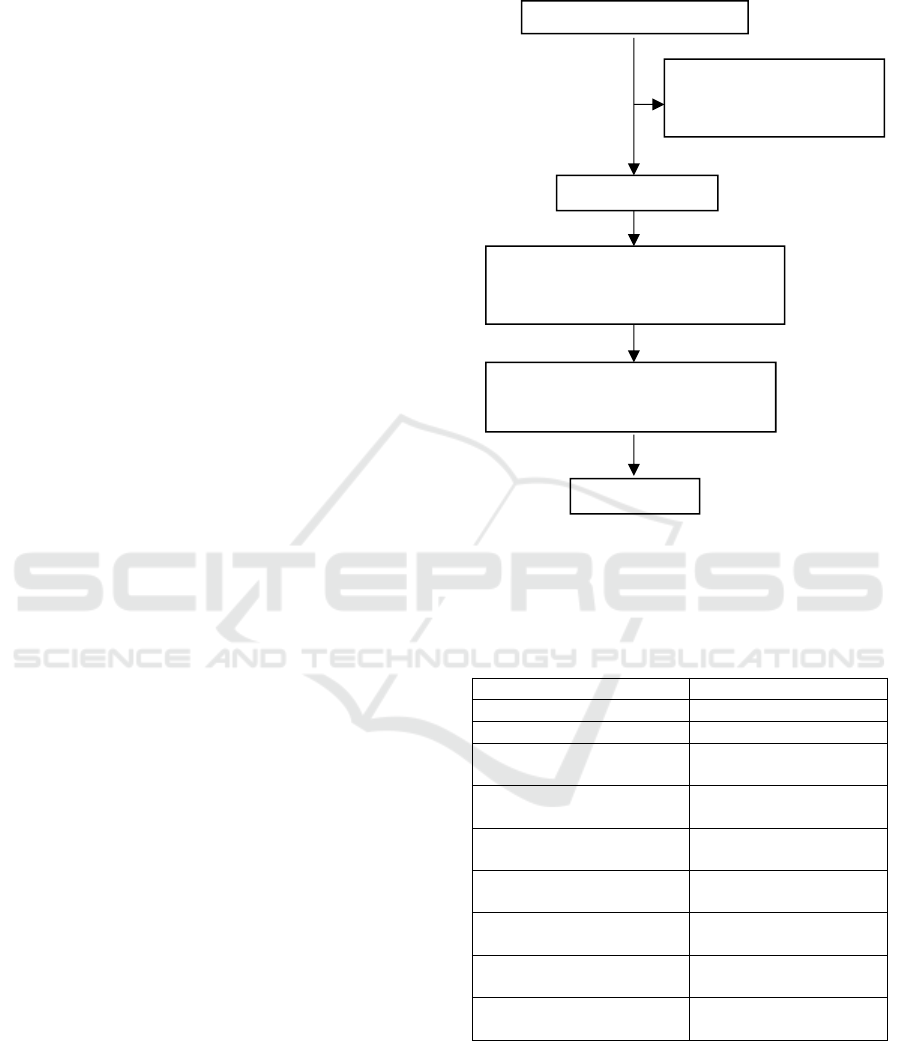
Figure 1: Research Pathway.
3 RESULT
3.1 Subject Characteristics
Table 1: Subject characteristics prior to exercise.
Characteristic
n=11
Age (years)
†
33.00 (22.00-49.00)
Body mass index °
21.36±2.440
Physical activity
(MET/week)
†
1040 (693-1400)
Duration of illness (years)
†
5.50 (1.33-18.33)
Corticosteroid dose use
(miligram/day)°
2.55 ± 0.93
Inspiratory muscle
sterngth (cmH
2
O)
†
49.66 (23.33-87.00)
Handgrip muscle strength
(kilograms)
†
11.00 (9.00-23.00)
Cardiopulmonal
endurance (meter)
†
432.00 (201.00-492.00)
Handgrip muscle
endurance (minute)
†
1.50 (1.09-3.18)
Note: n=number of samples; °=normal data distribution
using mean±deviation standard; †=abnormal data
distribution using median (range).
Table 1 showed the characteristics of the research
subjects were age 33.0 years with a fairly wide range
(22.00-49.00 years) and 5.50 years of duration
Assessed for eligibility (n=29)
Excluded (n=15)
Not meeting inclusion criteria (n=12)
Decline to participated (n=3)
Other reason = 0
Sample (n=14)
Allocated to intervention (n=14)
Received allocated intervention (n=14)
Did not received allocated intervention (n=0)
Loss of follow up (n=0)
Discontinued intervention (pregnance and
having another daily routine) (n=3)
Analysis (n=11)
The Effect of Additional Inspiratory Muscle Strengtening on Aerobic Exercise in Systemic Lupus Erythematosus: A Preliminary Study
163

disease with also wide range (1.33-18.33 years).
Range of age and duration of disease were left wide
because this study was the first study including
strengthening exercise in our hospital. At the end of
this study, these data and results will provide a basis
for future studies. In addition, based on International
Physical Activity Questionairre (IPAQ), the average
of physical activity of research subject was minimal
active.
Table 1 also showed the research subjects were
have good cardiopulmonal endurance but low
strength of the inspiratory and handgrip muscles.
These results indicate that SLE patients, although
they have good cardiopulmonary endurance, still
have low peripheral muscle strength including the
inspiratory and handgrip muscles. Good
cardiopulmonary endurance can be explained by the
fact that this group consisted of patients in LLDAS
category and minimaly active according to IPAQ.
Meanwhile, results showed low muscle strength.
Therefore, muscle strengthening is still needed in
SLE patients as an addition to aerobic exercise to
prevent decreased functional capacity.
In this study, IMS were chosen because it has
additional effect in improving oxygen supply to
peripheral muscles and also decrease the effects of
metaboreflexes on other peripheral muscles.
3.2 Effects of Additional Inspiratory
Muscles Strengthening in Aerobic
Exercise to Inspiratory and Other
Peripheral Muscle (Handgrip)
Strength
Table 2: Comparative characteristics of inspiratory and
handgrip muscle strength before and after exercise.
Note: n=number of samples; °=normal data distribution
using mean±deviation standard; †=abnormal data
distribution using median (range); *Wilcoxon test.
Table 2 showed the increase of inspiratory muscle
strength after administration of combination exercise
was significant (p <0.05). Not only inspiratory
muscle, but also other peripheral muscle such as
handgrip muscle strength increase significantly (p
<0.05) after adminsitration those combination
exercise.
3.3 Effects of Additional Inspiratory
Muscles Strengthening in Aerobic
Exercise to Cardiopulmonal and
Peripheral Muscle (Handgrip)
Endurance
Table 3: Comparison characteristics of cardiopulmonal
and handgrip muscle endurance before and after exercise.
Before
exercise
n=11
After
exercise
n=11
P
Cardio-
pulmonary
endurance
(meter)
†
432.00
(201.00-
492.00)
480.00
(384.00-
528.00)
0.003*
Handgrip
muscle
endurance
(minute)
††
1.50
(1.09-
3.18)
2.36
(1.37-
2.56)
0.075*
Note: n=number of samples; °=normal data distribution
using mean±deviation standard; †=abnormal data
distribution using median (range); *Wilcoxon test.
Table 3 showed the increase of cardiopulmonal
endurance was significantly (p<0.05) after
administration of combination exercise but not
significantly (p>0.05) on handgrip muscle endurance.
4 DISCUSSION
4.1 Effects of Additional Inspiratory
Muscles Strengthening in Aerobic
Exercise to Inspiratory and Other
Peripheral Muscle (Handgrip)
Strength
Muscle strength in SLE patients is generally lower
than normal. In this study, the inspiratory and
handgrip muscle strength was still low. The low
inspiratory muscle strength in our study was same
with study by Amra et al which showed low MIP
and MEP in 76 women with SLE who were followed
for 12 months (Amra et al, 2006). Another
autoimmune disease study by Weber et al,
rheumatoid atrhitis (RA), concluded that there was a
significant difference in respiratory muscle strength,
Before
exercise
n=11
After
exercise
n=11
P
Inspiratory
muscle
strength
(cmH
2
O)
†
49.66
(23.33-
87.00)
65.00
(44.30-
115.00)
0.0001*
Handgrip
muscle
strength
(kilogram)
†
11.00
(9.00-
23.00)
14.67
(9.33-
27.00)
0.016*
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
164

MIP (46.25 ± 17.67 vs 81.00 ± 19.69 cmH
2
O) and
MEP (58.75 ± 17.26 vs 78.00 ± 6.32 cmH
2
O)
between RA patients and healthy controls (Weber et
al, 2014).
The low strength of handgrip muscle in our study
was same with study by Balsamo et al which showed
low muscle strength in 25 premenopausal SLE
women with low disease activity compared to
healthy in both handgrip (24.2 ± 4.9 kg) and
quadriceps (47.4 ± 8.1 kg) (Balsamo et al, 2013).
Andrew et al also conducted studies related to
muscle strength in 146 SLE patients showed low
handgrip (22.7 ± 6.0 kg) and extensors (44.5 ± 15.7
kg) and knee flexors (29.9 ± 11.2 kg) muscle
strength (Andrews et al, 2015).
The low muscle strength can be caused by
inactivity and corticosteroids resulting changes in
muscle pathology. Muscle pathological changes in
SLE patients include myositis, vasculitis, type 2
muscle atrophy, thickening of blood vessel walls,
and vacuolar myopathy (Jakati et al, 2015). Vascular
changes interfere oxygen (O
2
) transport from arteries
to muscles or from muscle capillaries to
mitochondria (Silva AG, 2015).
This study result showed significantly increasing
of the inspiratory muscle strength after
administration combination exercises. This results
can be explained by the specifics of the strengtening
exercise itself that increase muscle properties,
namely recruitment of motor units and proportion of
muscle fibers (Bausek et al, 2013; McConnell, 2013).
This study result showed significant in increasing
of the strength of handgrip muscle although no
specific exercise was given specifically. This effect
can be explained by crossover training from exercise
combination. How strengthening of certain muscles
can cause increased strength of other muscles.
Zhang et al obtained significant handgrip muscle
strength in a combination intervention of aerobic
exercise and muscle strengthening for 8 weeks
compared to aerobic exercise alone in middle-aged
and elderly women (Zhang T et al, 2015).
Another effect of additional inspiratory muscle
strengthening is improvement in pulmonary
mechanical ventilation so it enable increased lung
volume and capacity which have impact on
increasing oxygen supply in peripheral muscles. So,
the increasing of handgrip muscle strength can also
be explained as a result of increased lung function
and respiratory muscle strength. Smith and Son
study found that handgrip strength has a strong
correlation with lung function as measured by
spirometry (Smith et al, 2018; Son et al, 2018).
The mechanism which underlying the correlation
of respiratory and other peripheral muscles is the
effect of metaboreflex. This metaboreflex increased
sympathetic activity in peripheral muscles including
the handgrip muscles to be more earlier fatigue.
Decrease of this metoboreflex can prevent early
fatigue in peripheral muscles so it increase
peripheral muscle performance (Bausek et al, 2013).
4.2 Effects of Additional Inspiratory
Muscles Strengthening in Aerobic
Exercise to Cardiopulmonal and
Peripheral Muscle (Handgrip)
Endurance
Cardiopulmonary endurance in SLE patients is
generally low compared to normal, but this study
showed these patient has good cardiopulmonary
endurance prior to exercise. This study is different
from previous study by Pinto et al which showed
lower cardiopulmonary endurance values with
VO
2
max (12.8±3.6 ml/kg/ min) compared to healthy
controls (14.6±4.6 ml/kg/min) (Pinto et al, 2016).
The difference probably because our research
subjects were categorized as LLDAS, who have low
disease activity and low dose of corticosteroid. The
other factor is that according to the IPAQ, subjects
in this study are categorized as minimally active, not
inactive, which could explain the state of
cardiopulmonary endurance in this study.
Low cardiopulmonary endurance depends on
multiorgan involving heart, lungs and peripheral
muscles. Disturbances in O
2
transport to muscle or
O
2
diffusion transport from muscle capillaries to the
mitochondria are determinants of cardiopulmonary
endurance in SLE patients. Deconditioning of
peripheral muscles is also believed to cause a
decrease in aerobic capacity in SLE patients. Other
factors such as the use of corticosteroids can
negatively impact the capillary number and
myofibril mass thereby contributing to the decrease
in aerobic capacity (Pinto et al., 2016; Silva AG,
2015).
This research showed significant result in
increase of cardiopulmonary endurance after
administration combination exercises. This study is
in line with the Miossi et al conducted study in 24
inactive SLE patients showed cardiac effect after 12
weeks of aerobic exercise with a treadmill for 30
minutes and resistance in the form of bench press,
leg press, leg extension, seated row, squat, and
crunches for 30-45 minutes (Miossi et al., 2012). In
our study, the strengthening exercise targeted only
The Effect of Additional Inspiratory Muscle Strengtening on Aerobic Exercise in Systemic Lupus Erythematosus: A Preliminary Study
165

the inspiratory muscle. Result of this study shows
that adding one exercise can benefit SLE patients.
The physiological mechanism responsible for
increasing of aerobic capacity are due to changes in
the central component (cardio-pulmonary) and
peripheral components (muscle). Cardiac output
increases after exercise through increased stroke
volume as a result of increased myocardial
contractility. Exercise can reduce the sympathetic
effect so that peripheral resistance decreases.
Exercise can also increase diffusion capacity of O
2
as a result of larger lung volume and alveolar-
capillary surface area that develops. The capacity of
muscle blood flow also increases with exercise due
to vascular remodeling in the form of capillary
angiogenesis and or changes in vascular resistance
(Kisner and Colby, 2012; Kraemer et al, 2012).
This study shows the increase of handgrip
muscle endurance after exercise combination.
Handgrip endurance was also assessed because the
function of the handgrip is not only measured by
handgrip strength. Handgrip function is needed for
SLE patients in daily activities besides
cardiopulmonary endurance for mobilization. The
increase of hangdrip endurance can be explained by
crossover training effect of these combination
exercise. The crossover effect showed that pasien
not only able to get results that are consistent to the
specificity of training, but also improve performance
in one type of exercise by training using another
type (Kraemer et al, 2012).
Although there is increasing of handgrip muscle
endurance, but not significantly different. This result
might be due to insufficient cross training effects of
exercise combination, because the inspiratory and
handgrip muscle strength in this study were still low
compared to normal. Another factor is sarcopenia,
which can occur in chronic inflammatory diseases
such as in SLE patients that were not measured in
this study. The diagnosis of sarcopenia should be
based on decreased muscle mass and strength
and/or lower physical performance. Therefore,
nutritional evaluation is also needed because it
affects the muscle mass itself.
Further research is needed to assess the
sarcopenia and nutritional on this new exercise
protocol in SLE patients. Another research is also
needed to define how much role of inspiratory
muscle strengthening compared to aerobic exercise
in providing a positive effect on this results.
5 CONCLUSION
The addition of inspiratory muscle strenghtening on
aerobic exercise not only increases the
cardiopulmonary function but also impacts on the
other functional performance, including handgrip
which is usefull for daily activities. Further research
is needed to explore other functional effects of this
additional inspiratory muscle strengtening to aerobic
exercise in SLE patients.
ACKNOWLEDGEMENTS
This works was supported by the Indonesia
Endownment Fund for Education, Ministry of
Finance of the Republic of Indonesia. There is no
conflict of interest, none of the authors have any
conflicts of interest to declare.
REFERENCE
Abrahão, M.I., Gomiero, A.B., Peccin, M.S., Grande, A.J.,
Trevisani, V.F.M., 2016. Cardiovascular training vs.
resistance training for improving quality of life and
physical function in patients with systemic lupus
erythematosus: a randomized controlled trial. Scand. J.
Rheumatol. 45, 197–201.
https://doi.org/10.3109/03009742.2015.1094126
Amra, B., Mirzaei, M.R., Bonakdar, Z.S., Golshan, M.,
2006. Respiratory Muscle Function and Spirometry in
Patients with Systemic Lupus Erythematosus.
Tanaffos. 5 (4), 53-58.
Andrews, J.S., Trupin, L., Schmajuk, G., Barton, J.,
Margaretten, M., Yazdany, J., Yelin, E.H., Katz, P.P.,
2015. Muscle Strength and Changes in Physical
Function in Women With Systemic Lupus
Erythematosus: SLE and Physical Function in Women.
Arthritis Care Res. 67, 1070–1077.
https://doi.org/10.1002/acr.22560
Balsamo, S., 2013. The quality of life of patients with
lupus erythematosus influences cardiovascular
capacity in 6-minute walk test. Rev Brass Reumatol.
53 (1), 75-78. https://doi.org/ 10.1590/S0482-
50042013000100008
Balsamo, S., da Mota, L.M.H., de Carvalho, J.F.,
Nascimento, D. da C., Tibana, R.A., Santos de
Santana, F., Moreno, R.L., Gualano, B., dos Santos-
Neto, L., 2013. Low dynamic muscle strength and its
associations with fatigue, functional performance, and
quality of life in premenopausal patients with systemic
lupus erythematosus and low disease activity: a case–
control study. BMC Musculoskelet. Disord. 14.
https://doi.org/10.1186/1471-2474-14-263
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
166

Bausek, N., Berlin, T., Aldarondo, S., 2013. The power
and potential of respiratory muscle training.
Respiratory muscle training. Churchill Livingstone.
United Kingdom. 97-131
De Medeiros, A.I.C., Fuzari, H.K.B., Rattesa, C., Brandão,
D.C., de Melo Marinho, P.É., 2017. Inspiratory muscle
training improves respiratory muscle strength,
functional capacity and quality of life in patients with
chronic kidney disease: a systematic review. J.
Physiother. 63, 76–83.
https://doi.org/10.1016/j.jphys.2017.02.016
Franklyn, K., Lau, C.S., Navarra, S.V., Louthrenoo, W.,
Lateef, A., Hamijoyo, L., Wahono, C.S., Chen, S.L.,
Jin, O., Morton, S., Hoi, A., Huq, M., Nikpour, M.,
Morand, E.F., 2016. Definition and initial validation
of a Lupus Low Disease Activity State (LLDAS). Ann.
Rheum. Dis. 75, 1615–1621.
https://doi.org/10.1136/annrheumdis-2015-207726
Jakati, S., Rajasekhar, L., Uppin, M., Challa, S., 2015.
SLE myopathy: a clinicopathological study. Int. J.
Rheum. Dis. 18, 886–891.
https://doi.org/10.1111/1756-185X.12592
Karadall, M.N., Bo nak-Guclu, M., Camc o lu, B.,
Kokturk, N., Turkta, H., 2016. Effects of Inspiratory
Muscle Training in Subjects With Sarcoidosis: A
Randomized Controlled Clinical Trial. Respir. Care 61,
483–494. https://doi.org/10.4187/respcare.04312
Kisner C., Colby LA., 2012. Therapeutic Exercise:
Foundations and Techniques. F. A. Davis. Philadelpia,
6
th
edition.
Kraemer W.J., Fleck S.J., Deschenes MR., 2012. Exercise
Physiology: Integrated from Theory to Practical
Applications. Lippincott Williams & Wilkins Health.
Baltimore
McConnell, A., 2013. Functional benefits of respiratory
muscle training, in: Respiratory Muscle Training.
Elsevier, pp. 97–131. https://doi.org/10.1016/B978-0-
7020-5020-6.00004-2
Miossi, R., Benatti, F.B., de Sá Pinto, A.L., Lima, F.R.,
Borba, E.F., LPrado, D.M., Perandini, L.A., Gualano,
B., Bonfá, E., Roschel, H., 2012. Exercise training
counterbalances chronotropic incompetence and
delayed heart rate recovery in systemic lupus
erythematosus: A randomized trial. Arthritis Care Res.
n/a-n/a. https://doi.org/10.1002/acr.21678
Pinto, A.J., Miyake, C.N.H., Benatti, F.B., Silva, C.A.,
Sallum, A.M.E., Borba, E., de Sá-Pinto, A.L., Bonfá,
E., Gualano, B., 2016. Reduced Aerobic Capacity and
Quality of Life in Physically Inactive Patients With
Systemic Lupus Erythematosus With Mild or Inactive
Disease: Aerobic Capacity and Quality of Life in SLE.
Arthritis Care Res. 68, 1780–1786.
https://doi.org/10.1002/acr.22905
Ray, A.D., Udhoji, S., Mashtare, T.L., Fisher, N.M., 2013.
A Combined Inspiratory and Expiratory Muscle
Training Program Improves Respiratory Muscle
Strength and Fatigue in Multiple Sclerosis. Arch. Phys.
Med. Rehabil. 94, 1964–1970.
https://doi.org/10.1016/j.apmr.2013.05.005
Shaharir, S., Gordon, C., 2016. Constitutional Symptoms
and Fatigue in Systemic Lupus Erythematosus, in:
Systemic Lupus Erythematosus. Elsevier, pp. 317–324.
https://doi.org/10.1016/B978-0-12-801917-7.00037-1
Silva AG, P.D., 2015. Impaired Aerobic Capacity in
Systemic Lupus Erythematosus Patients: What are the
Physiological Mechanisms. Rheumatol. Curr. Res. s6.
https://doi.org/10.4172/2161-1149.S6-008
Smith, M.P., Standl, M., Berdel, D., von Berg, A., Bauer,
C.-P., Schikowski, T., Koletzko, S., Lehmann, I.,
Krämer, U., Heinrich, J., Schulz, H., 2018. Handgrip
strength is associated with improved spirometry in
adolescents. PLOS ONE 13, e0194560.
https://doi.org/10.1371/journal.pone.0194560
Son, D.-H., Yoo, J.-W., Cho, M.-R., Lee, Y.-J., 2018.
Relationship Between Handgrip Strength and
Pulmonary Function in Apparently Healthy Older
Women: Handgrip strength and pulmonary function. J.
Am. Geriatr. Soc. 66, 1367–1371.
https://doi.org/10.1111/jgs.15410
Soriano-Maldonado, A., Vargas-Hitos, J., Sabio, J., 2016.
Cardiovascular training vs. resistance training for
improving quality of life and physical function in
patients with systemic lupus erythematosus: a
randomized controlled trial: comments on the article
by Abrãhao et al. Scand. J. Rheumatol. 45, 253–254.
https://doi.org/10.3109/03009742.2016.1138319
Spinelli, F., Truglia, S., Colasanti, T., Pecani, A.,
Ceccarelli, F., Miranda, F., Mancini, R., Perricone, C.,
Pendolino, M., Alessandri, C., Valesini, G., Conti, F.,
2017. SAT0283 Antibodies to carbamylated vimentin
in patients with systemc lupus erythematosus are
associated with renal involvenment. BMJ Publishing
Group Ltd and European League Against Rheumatism,
pp. 880.1-880. https://doi.org/10.1136/annrheumdis-
2017-eular.5819
Weber, F.M., Iop, R. da R., Shiratori, A.P., Domenech,
S.C., Borges Júnior, N.G., Gevaerd, M. da S., 2014.
Reduction of respiratory muscle strength in subjects
with rheumatoid arthritis. Acta Fisiátrica 21.
https://doi.org/10.5935/0104-7795.20140036
Wu, M.-L., Yu, K.-H., Tsai, J.-C., 2017. The Effectiveness
of Exercise in Adults With Systemic Lupus
Erythematosus: A Systematic Review and Meta-
Analysis to Guide Evidence-Based Practice: Meta-
Analysis of Exercise in SLE. Worldviews Evid. Based
Nurs. 14, 306–315. https://doi.org/10.1111/wvn.12221
Zhang, T., Liu. H., Shu. Y., 2015. Effects of aerobic
exercise and strength training on the hand grip
strength and functional fitness in the middle aged and
elder women. Chinese Journal of Rehabilitation
Medicine. Available from
http://en.cnki.com.cn/Article_en/CJFDTOTAL-
ZGKF201512010.htm (accessed 7.7.19).
The Effect of Additional Inspiratory Muscle Strengtening on Aerobic Exercise in Systemic Lupus Erythematosus: A Preliminary Study
167
