
Functional Outcomes of Elderly after Unilateral Diabetic Transtibial
Amputation: A Case Report
Elisabet Augustina, Melinda Harini
Department of Physical Medicine and Rehabilitation, Dr. Cipto Mangunkusumo National General Hospital,
Faculty of Medicine, University of Indonesia, Jakarta, Indonesia
Keywords: Functional, Elderly, Transtibial Amputation, Diabetes
Abstract: Foot ulceration is a major cause of morbidity in elderly with diabetes, as osteomyelitis and diabetic
gangrene lead to amputation. After undergoing transtibial amputation, patients were referred to
Rehabilitation Department for prosthesis prescription and rehabilitation to restore mobility and to
successfully reintegrate the patient into community. This study aims to identify the current patient’s
mobility, independence and mental status following amputations. This study was done between May 2017
and August 2018, four patients above 60 years old were referred to Medical Rehabilitation outpatient clinic
as candidates of prosthesis use after unilateral transtibial diabetic amputations. Mobility status, Barthel
Index, Mini Mental State Examination and Geriatric Depression Scale were evaluated through medical
records and interview. Two patients who completed rehabilitation programs, ambulate with prostheses
without obstacles and are mild dependent with current better mental status. Two patients who did not, are
moderate dependent ambulating with wheelchair. In conclusion, patients who completed rehabilitation were
more independent, ambulatory with prosthesis and have better mental status. Factors such as social living
conditions, initial cognitive and independence levels may be considered as functional outcome predictors.
Further investigation with better method and larger sample size is needed.
1 INTRODUCTION
Diabetes Mellitus (DM) is the leading cause of
nontraumatic lower extremity amputation in
worldwide. Approximately 15% of individuals with
DM develop a foot ulcer and a significant subset will
ultimately undergo amputation (Powers, 2015).
Every year more than one million people undergo a
lower limb amputation as consequence of
osteomyelitis and diabetic gangrene, which
calculates to a limb lost due to diabetes every 30
seconds in the world (Braun, 2014).
Diabetics have a 15-fold higher risk for lower
limb amputation. Risk factors for amputation among
diabetic patients include: male sex, diabetes more
than 10 years duration, peripheral neuropathy,
abnormal structure of foot (bony abnormalities,
callus, thickened nails), peripheral arterial disease,
smoking, history of previous ulcer or amputation
and poor glycemic control (Powers, 2015)
Transtibial amputation is the most common
amputation level seen in general practice. It is
performed one third of the way down tibia and a
posterior myocutaneous flap is used to cover the
residual tibia. At this length, the bulk of the posterior
compartment muscles are available for a flap
providing good soft tissue coverage over the distal
tibia and the primary vascular structures for the
lower limb are preserved in the flap (Clayton, 2009).
Rehabilitation management is crucial in the
postoperative period. Early mobilization facilitates
early functional improvements such as bed mobility,
transfers and mobilization to chair or wheelchair
(Lovegreen, 2015). Patients must be educated about
positioning, range of motion (ROM) and
strengthening exercises of the affected limb
(Frykberg, 2006). Initiation of aerobic exercise is
needed to increase endurance and cardiovascular
fitness. As the patient progress, focuses are more on
standing and balance in parallel bars and use of
walking aid (Brigham, 2011).
Prosthetic fitting and gait training can usually be
started within 3–6 weeks of surgery. Patients usually
ambulate independently within one month of starting
Augustina, E. and Harini, M.
Functional Outcomes of Elderly after Unilateral Diabetic Transtibial Amputation: A Case Report.
DOI: 10.5220/0009066301490153
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 149-153
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
149
therapy using prosthesis. The residual limb
continues to shrink during the first 6–8 months.
After completing the final prosthetic evaluation, the
patient will require a period of gait training under
the supervision of the physical therapist (Lovegreen,
2015).
Rehabilitation programs are designed to
endeavor restoring functional mobility and to
successfully reintegrating the patient into
community. Functional outcomes of amputees have
been reported to be associated with early
rehabilitation intervention and adherence rate of the
patients to rehabilitation (Kosse, 2013). Most
literature defines functional outcome only in terms
of prosthetic use, but general measures of functional
outcome with or without prosthesis are equally
important (Van Eijk, 2012).
Factors such as age, Mini Mental State
Examination (MMSE) and Barthel Index (BI)
preoperative and at admission to rehabilitation are
correlated significantly with later functional status
(Van Eijk, 2011). Less use of prosthesis is
significantly related to age, female sex, cognitive
impairment, level of physical disability, possession
of wheelchair and dissatisfaction (Bilodeau, 2000).
Status of ambulatory and mental have reciprocal
connection in elderly with prostheses (Coffey,
2012). Patients with impairment in several areas of
cognition including memory, attention and
concentration, visuospatial function and
organizational skills will face significant challenges
in learning how to mobilize with prosthesis (O’Neil
2008; O’Neil, 2009). Meanwhile, one study found
that years after major lower extremity amputation,
amputees who do not use prostheses have more
symptoms of depression than those who use (Remes,
2010).
The purpose of this case series was to follow-up
and identify the current mobility, independence and
mental status of elderly patients one to two years
after unilateral diabetic transtibial amputation.
2 METHODS
Between May 2017 and August 2018, four patients
older than 60 years old post unilateral transtibial
amputation due to diabetic gangrene, were referred
to Department of Medical Rehabilitation outpatient
clinic, Cipto Mangunkusumo National General
Hospital, Jakarta for prosthesis prescription and
rehabilitation. The patients came within 1-4 months
after surgery. Data is collected through medical
records and interview during home visit. Informed
consent was obtained from the patients.
Patients’ status of mobility, independence and
mental were evaluated at the first consultation and
reevaluated during home visit on August 2019.
Evaluation of mobility status is by observing and
asking how the patient ambulate in daily life and the
use of prosthesis or other ambulatory aids. BI-100 is
used to evaluate the independence level of activity
of daily living (ADL). Mental status is evaluated
using MMSE and Geriatric Depression Scale (GDS).
Medical history and social living condition are
collected through medical records, interview and
observation.
3 RESULTS
Table 1 shows the baseline characteristics of the
patients. Among the patients are three males and one
female, with age range 61–67 years old and
amputation onset range 12–24 months with left legs
as predominant sites.
Table 1: Patients’ Characteristics.
A B C D
Age* 62 61 65 67
Sex Male Male Male Female
Leg sites
Amputation
onset**
Left
24
Left
24
Right
17
Left
12
Post-operative
to
rehabilitation**
Rehabilitation
attendance***
3
58.3
1
100
3
100
4
66.7
*in years; **in months; ***in percent
Rehabilitation care included 30-45 minutes of
individual physical therapy, 2 times a week,
consisting of improving transferring, upper and
lower limb muscle strengthening, shaping residual
limb for prosthesis, range of motion exercise to
preventing flexion contracture of involved joint,
massage of soft tissue adhesions, preparing for
weight-bearing and prosthesis wearing. During
consultation and follow-up, patient and caregiver
were given education about stump care, positioning
(avoiding prolonged knee flexion), risk of fall, home
program and prosthesis use. There was no adverse
event, no history of new wound and hospital
readmission from all the patients.
Patient B and C completed the rehabilitation until
prosthesis fitting and training. Patient A and D did
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
150
not do rehabilitation regularly. However, all of them
eventually got prosthesis which consists of patellar
tendon bearing socket, supracondylar cuff
suspension, exoskeleton shank and solid ankle
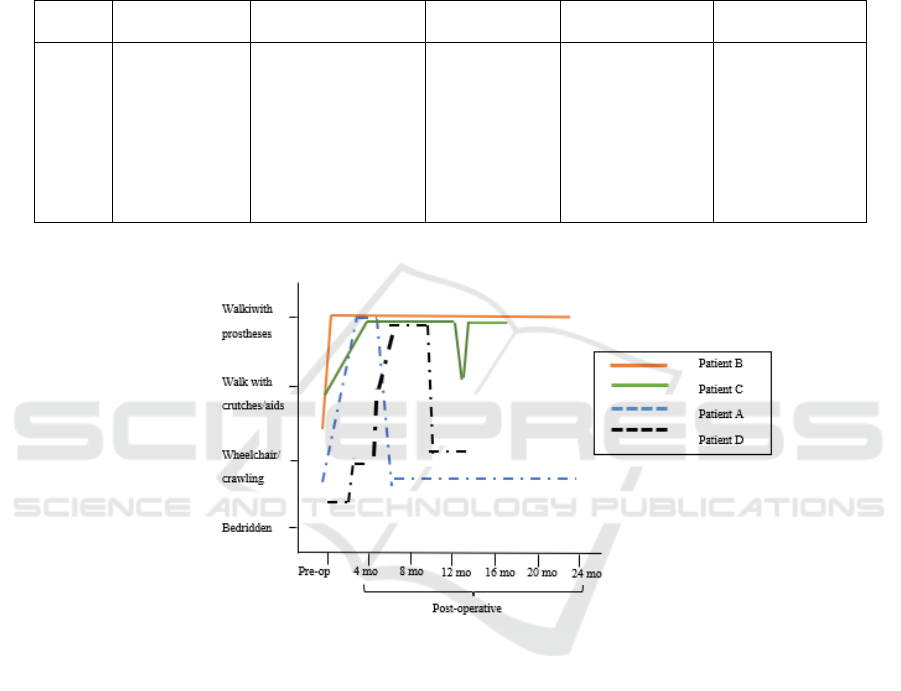
cushion heel foot. Table 2 shows comprehensive
geriatric assessment (CGA). The functional
outcomes (mobility, independence and mental
status) are compared between now and the first
consultation time. Figure 1 shows the progression of
patients’ mobility status between pre and
postoperative.
Table 2: Comprehensive Geriatric Assessment.
Patient Preoperative
Mobility Level
Current Mobility
Level*
Barthel Index
Then Now
MMSE
Then Now Δ
Geriatric
Depression Scale
A
B
C
D
Out: wheelchair
In: bedridden
Out: wheelchair
In: crutches
Out: crutches
In: crutches
Out: wheelchair
In: bedridden
Out: wheelchair
In: crawling/hopping
Out: prosthesis
In: prosthesis
Out: prosthesis
In: crutches
Out: wheelchair
In: wheelchair
52 68
92 98
88 92
66 64
27 24 3
28 28 0
29 27 2
24 19 5
9
2
4
7
*Out= outdoor; In=indoor
Figure 1: Mobility Status Progression.
4 DISCUSSION
Inspired by ICF (International Classification of
Functioning, Disability and Health) model, aspects
of health conditions, body structures and functions,
personal and environmental factors were evaluated
in this case-series. This study emphasizes on
mobility, independence of ADL and cognitive status
as body functions and presence of family support as
the environmental factors.
The importance of following-up mobility status
of elderly patients after lower limb amputation is
because mobility is the key component of
independent living, enabling the performance of
activities of daily living (Bilodeau, 2000; Geertzen,
2005). In this study, we found among four patients
with unilateral transtibial amputation due to
diabetes, two of them still ambulate with prosthesis
without obstacles. The other two patients only used
the prostheses first couple months because they felt
heavy and uncomfortable so they prefer wheelchair.
Patient A used to be bedridden for 3 weeks prior
to amputation. After getting prosthesis, he
complained of unfitness resulting skin excoriation
on stump but refused to repair due to financial
problem (as it is not covered by national health
insurance). Patient D was bedridden about 2 months
before amputation because refusing the idea of
amputation and seeking for alternative treatment, but
then post amputation, she gained ability on wheeling
and partially using walker before getting prostheses.
She apparently used prosthesis less than four months
Functional Outcomes of Elderly after Unilateral Diabetic Transtibial Amputation: A Case Report
151

and gradually became dominant wheelchair user, as
she found it easier and less fatigue.
The patients who no longer use the prostheses
apparently attended less than 70% of rehabilitation
sessions. They have similarities, in which they only
live with spouses who are also elderly with
disabilities. Patient A’s wife is a 60-year-old female
with obesity, knee pain, hypertension and frequent
headache, while patient D’s husband is a 78-year old
male with hearing problems and history of ischemic
stroke. They could only go to hospital if their
children or relative had time to accompany them.
Not only difficulty to access and caregiver, financial
issue also plays role. Rather than attending
rehabilitation, patient A prefers accompanying his
wife working (as street seller), as he quit working
few months pre-amputation. On the other side, two
patients who use prostheses attended rehabilitation
regularly because they have supports from spouses,
children or grandchildren who live together with the
patients.
Family support is an important facilitator of the
regaining ability to function by enabling social
participation and encouraging self-care. This fact
was evidenced by several studies in which
individuals receiving greater social support present
better health conditions, physical and psychological
performance, in addition to greater adherence of the
treatment (Junior, 2017). A study proved that
adherence to rehabilitation has significant benefit,
where patients who attended more than 80%
scheduled sessions, the mean muscle power score in
each side of the upper and lower limbs was
significantly better and degree of dependency
improved following rehabilitation (AlSofyani,
2016).
In this study, we found that BI score of patients
using prostheses was higher at initial compared to
the wheelchair patients and it increased at the
current condition. On the other side, the first
wheelchair patient has increased BI score but still
categorized as moderate dependent. The second
wheelchair patient in fact becomes more dependent
in ADL. This is highly possibly related to the
decrease of cognition. She has the highest decline of
MMSE score among four of them. The two
wheelchair patients are also categorized as probable
depression based on GDS.
This finding is similar with one study (Van Eijk,
2011) that found patients who completed
rehabilitation had increase of BI between first
admitted to rehabilitation and one year in the
afterwards (p=0.000), where patients who did not
complete had no significant increase (p=0.932). In
contrast, different from this result, previous studies
found that pre-operative functional is the most
important in predicting walking ability and
prosthesis use after lower limb amputation, where
post-operative functional status does not seem to be
related. It is also recommended that evaluation of
ambulation is useful rather than global functional
assessment (Sansam. 2009).
Studies also established significant relation
between cognitive abilities with the functional level
and prediction of prosthetic use, as learning skills
are important in order to adequately use prosthesis
(Lee, 2018; Van Eijk, 2012). Using MMSE,
cognitive status at 2-4 weeks after amputation was
found to predict 20% of variance in mobility at 8-14
months post lower limb amputation (Coffey, 2012).
The cognitive domains such as: memory, executive
function, visuospatial cognition and language
fluency are considered to be sensitive (Lee, 2018).
Depression following amputation in elderly,
based on one study, appeared had no statistically
significant relationship with prosthesis use
(Bilodeau, 2000). Factors associated with depressive
symptoms in lower limb amputees are female sex,
lack of social support, unemployment, shorter time
since amputation, smoking status and pain
(Hawamdeh, 2008). Both wheelchair patients have
similar risk factors: lack of support from family and
being unemployed. Additional risk factors are
smoking for patient A (as he still smokes
occasionally) and female gender for patient D.
This is the first follow-up case series about
functional outcomes of elderly transtibial amputation
due to diabetes. In this small case series, we note
limitation that this study only involved small
numbers of patients, thus making it difficult to
generalize the results for elderly amputees. This is
because we only recruited and followed-up elderly
transtibial amputees from Physical Medicine and
Rehabilitation residents’ case reports from 2017 to
2018. The other study limitation is related to the use
of functional outcome parameters. This study only
used status of prosthesis use, BI, MMSE and GDS.
One meta-analysis (Fortington, 2012) states that
there is still no standard of predictors or functional
outcome measures of lower limb geriatric amputees.
Further more comprehensive parameters involving
physical, mental and social aspects should be
utilized (Lee, 2018; Schoppen, 2003).
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
152

5 CONCLUSIONS
In conclusion, patients who completed rehabilitation
are more independent, ambulatory with prostheses
and have better mental status. Factors such as
MMSE and BI, as well as patient’s social living
conditions may be considered as functional outcome
predictors for the elderly patients undergoing
diabetic transtibial amputation. The predictors could
assist in determining suitability prosthetic or
ambulatory aids use, ascertaining appropriate and
realistic goals so that maximal mobility and
independence are achieved. In this case, further
investigation with better method and larger sample
size is needed.
REFERENCES
AlSofyani, M.A., AlHarthi, A.S., Farahat, F.M.,
Abuznadah, T. 2016. Impact of rehabilitation
programs on dependency and functional performance
of patients with major lower limb amputations, Saudi
Med J, 37(10), pp.1109–13.
Bilodeau, S., Hebert, R., Desrosiers, J. 2000. Lower limb
prosthesis utilization by elderly amputees, Prosthet
Orthot Int, 24(2), pp.126–32.
Braun, L.Z., Fisk, W.A., Levtof, H., Kirsner, R.S.,
Isseroff, R.R. 2014. Diabetic foot ulcer: an evidence-
based treatment update, Am J Clin Dermatol, 15,
pp.267–81.
Brigham and Women’s Hospital. 2011. Department of
Rehabilitation Services. Standard of care: lower
extremity amputation.
Clayton, W., Elasy, T.A. 2009. A review of the
pathophysiology, classification and treatment of foot
ulcers in diabetic patients, Clinical Diabetes, 27(2),
pp.52-7.
Coffey, L., O’Keefe, F., Gallagher, P., Desmond, D.,
Lombard-Vance, R. 2012. Cognitive functioning n
persons with lower limb amputations: a review.
Disabil Rehabil, 34(23):1950–64.
Fortington, L.V., Rommers, G.M., Geertzen, J.H.B.,
Postema, K., Dijkstra, P.U. 2012. Mobility in elderly
people with a lower limb amputation. JAMDA, 13,
pp.319–25.
Frykberg, R.G., Zgonis, T., Armstrong, D.G., Driver,
V.R., Giurini, J.M., Kravitz, S.R. 2006. Diabetic foot
disorder: a clinical practice guideline. The Journal of
Foot Ankle Surgery, 45(5), pp.2–52.
Geertzen, J.H.B., Bosmans, J.C., Van Der Schans, C.P.
2005. Claimed walking distance of lower limb
amputees. Disabil Rehabil, 27, pp.101–104.
Hawamdeh, Z.M., Othman, YS., Ibrahim, A.I. 2008.
Assessment of anxiety and depression after lower limb
amputation in Jordanian patients. Neuropsyhiatr Dis
Treat, 4(3), pp.627–33.
Junior, E.G., Knabben, R.J., da Luz, S.C.T. 2017.
Portraying the amputation of lower limbs: an approach
using ICF, Fisioter Mov, 30(1), pp.97–106.
Kosse, N.M., Dutmer, A.L., Dasenbrock, L., Bauer, J.M.,
Lamoth, C.J. 2013. Effectiveness and feasibility of
early physical rehabilitation programs for geriatric
hospitalized patients: a systematic review. BMC
Geriatr, 13, pp.107.
Lee, D.J., Costello, M.C. 2018. The effect of cognitive
impairment on prostheses use in older adults who
underwent amputation due to vascular-related
etiology: a systematic review of the literature, Prosthet
Orthot Int, 42(2), 144–52.
Lovegreen, W., Murphy, D.P., Smith, W.K., Steven, P.,
Webster, J. 2015. Lower limb amputation. In: Cifu
D.X Braddom’s Physical Medicine and Rehabilitation,
5th ed, Netherland: Elsevier, pp.191–232.
O’Neil, B.F. 2008. Cognition and mobility rehabilitation
following lower limb amputation. In: Gallagher, P.,
Desmond, D., McLahlan, M., eds. Psychoprosthetics.,
London: Springer, pp.53–65.
O’Neil, B.F., Evans, J.J. 2009. Memory and executive
function predict mobility rehabilitation outcome after
lower-limb amputation. Disabil Rehabil, 31(13),
pp.1083–91.
Powers A.C. 2015. Diabetes mellitus: diagnosis,
classification and pathophysiology. In: Kasper D.L
Harrison’s principles of internal medicine, 19th ed,
USA: McGraw-Hill Medical Publishing Division,
pp.2399-407.
Remes, L., Isoaho, R., Vahlberg, T. 2010. Quality of life
three years after major lower extremity amputation
due to peripheral arterial disease, Aging Clin Exp Res,
22, pp.395.
Sansam, K., Neumann, V., O’Connor, R., Bhakta, B.
2009. Predicting walking ability following lower limb
amputation, J Rehabil Med, 41, pp.593–603.
Schoppen, T., Boonstra, A., Groothoff, J.W., de Vries, J.,
Goeken, L.M, Wisma, W.H. 2003. Physical, mental
and social predictors of functional outcome in
unilateral lower-limb amputees, Arch Phys Med
Rehabil, 84, pp.803–810.
Van Eijk, M.S., Van der Linde, H., Buijck, B.I., Zuidema,
S.U., Koopmans, R.T. 2011. Geriatric rehabilitation of
lower limb amputees: a multicenter study, Disability
and Rehabilitation, 34(2), pp.145 – 50.
Van Eijk, M.S., Van der Linde, H., Buijck, B., Geurts, A.,
Zuidema, S., Koopmans, R. 2012. Predicting
prosthetic use in elderly patients after major lower
limb amputation, Prosthet Orthot Int, 36(1), pp.45–52
Functional Outcomes of Elderly after Unilateral Diabetic Transtibial Amputation: A Case Report
153
