
Osteoarthritis of the Hip
Rudy Handoyo
Department of Physical Medicine and Rehabilitation, Dr. Kariadi General Hospital,
Faculty of Medicine, University of Diponegoro, Semarang, Indonesia
rud_hand@hotmail.com
Keywords: Osteoarthritis, Hip, Degenerative Joint.
Abstract: Osteoarthritis (OA), often referred to as “wear-and-tear” arthritis, or degenerative joint disease, is the
most common form of joint disorder. The effects of OA on the large joints of the lower extremities,
including the hips, can result in reduced mobility and marked physical impairment that can lead to loss of
independence and to increased use of health care services such as dependency in walking, stair climbing,
and rising from a seated position. Disease initiation and progression are caused by a combination of local
factors and systemic factors that vary between individuals and its progression caused by a combination of
endogenous and environmental risk factors. The management of hip OA included: 1. Pharmacological
treatment: analgesic, NSAID, duloxetine, opioid, intra articular injection. 2. Rehabilitation management:
joint rest, physical modalities, exercise, appropriate joint use, weight control, assistive devices and
orthosis, ergonomic and environmental adaptation, education, psychological intervention. 3. Surgery.
Medical rehabilitation goal such as: decrease pain/symptoms, increase range of motion, maintain the
strength of muscle, increase aerobic capacity, optimize daily function and minimize disability. Exercise
therapy should be the mainstay therapy when possible, with physical modalities utilized as an adjunct.
Evaluate and correct for abnormal biomechanics, using assistive devices and orthosis as necessary.
1 INTRODUCTION
Osteoarthritis (OA), often referred to as “wear-and-
tear” arthritis, or degenerative joint disease, is the
most common form of joint disorder. As a
degenerative disorder, OA can involve any joint, and
it primarily affects the articular cartilage and
surrounding tissues. The hip joint is one of the
body’s largest weight-bearing joints and is
commonly affected by OA. The OA process
involves progressive loss of articular cartilage,
subchondral cysts, osteophyte formation,
periarticular ligamentous laxity, muscle weakness,
and possible synovial inflammation (Lespasio et al.,
2018). The effects of OA on the large joints of the
lower extremities, including the hips, can result in
reduced mobility and marked physical impairment
that can lead to loss of independence and to
increased use of health care services such as
dependency in walking, stair climbing, and rising
from a seated position (Lespasio et al., 2018).
2 DISCUSSION
The reported prevalence of hip osteoarthritis varies
greatly due to differences in the definition of
osteoarthritis used (radiographic, symptomatic, or self-
reported) and the characteristics of the sample (Bennell,
2013). The prevalence rates varied from 0.9% to 45%.
Men and women showed similar overall prevalence:
11.5% for men and 11.6% for women. In contrast to
prevalence, information on the incidence of hip
osteoarthritis is limited, reflecting greater methodological
challenges. Cumulative incidence rates varying from
3.8% over 10 years to 33% over 8 years (Bennell, 2013).
The lifetime risk for symptomatic hip OA is 19% for
men and 29% for women (Suri et al., 2012).
2.1 Etiology and Risk Factors
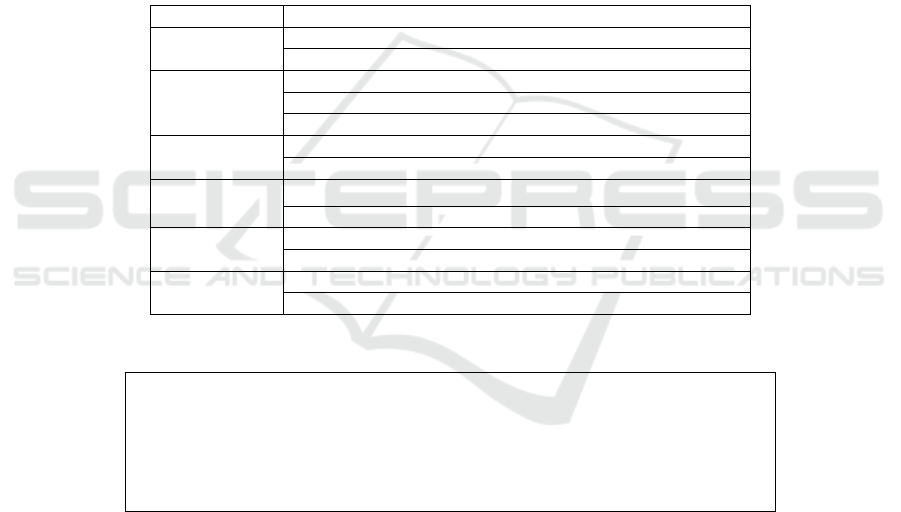
Disease initiation and progression are caused by a
combination of local factors and systemic factors
that vary between individuals (figure 1 and 2) and its
progression caused by a combination of endogenous
Handoyo, R.
Osteoarthritis of the Hip.
DOI: 10.5220/0009061900370043
In Proceedings of the 11th National Congress and the 18th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation Association (KONAS XI and PIT XVIII PERDOSRI
2019), pages 37-43
ISBN: 978-989-758-409-1
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
37
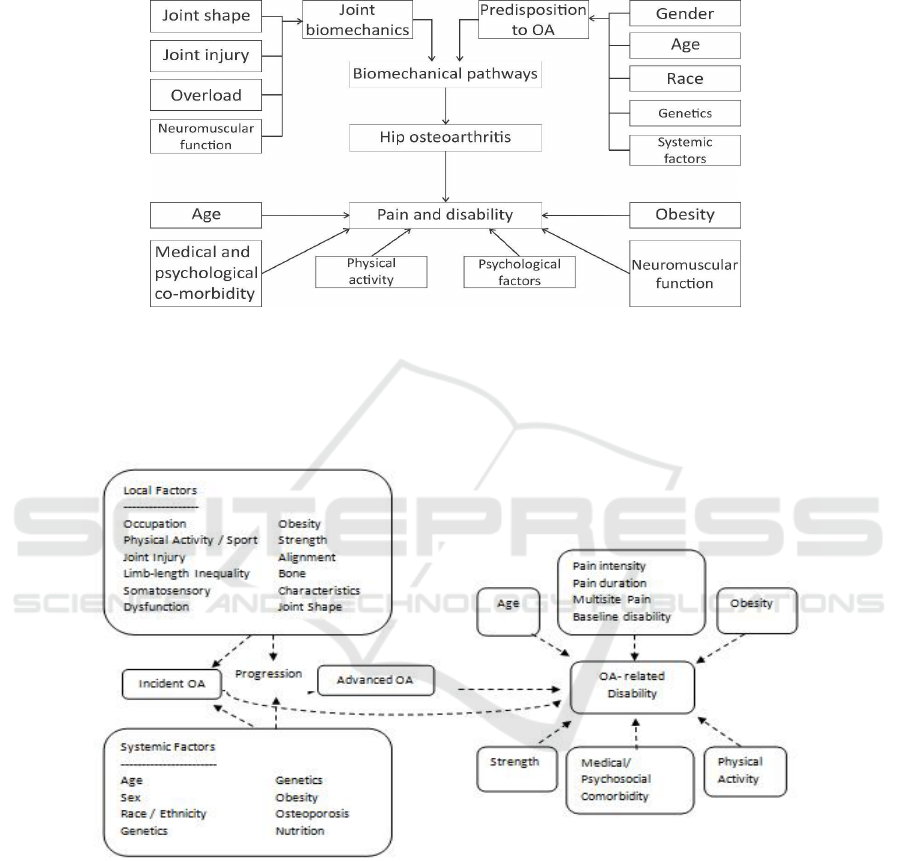
and environmental risk factors (Lohmander et al.,
2017).
Figure 1: Etiology and risk factor for hip osteoarthritis.
Figure 2: Risk factors for osteoarthritis and related disability.
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
38
2.2 Signs And Symptoms
Pain:
o Progressively increasing
o Aggravated - movement; when hip is
loaded wrong or too long; cold weather
o Eased with continuous movement
o Commonly in groin/thigh, radiating to
buttocks or knee
o End-stage: Constant pain, night pain
Stiffness:
o Morning stiffness with end-stage
osteoarthritis, usually eased with movement
(<1 hour)
“Locking" of hip movement
Decreased range of motion - leading to joint
contractures and muscle atrophy
Crepitation with movement
Gait abnormalities - short limb gait, antalgic
gait, trendelenburg gait
Leg length discrepancy
Local inflammation
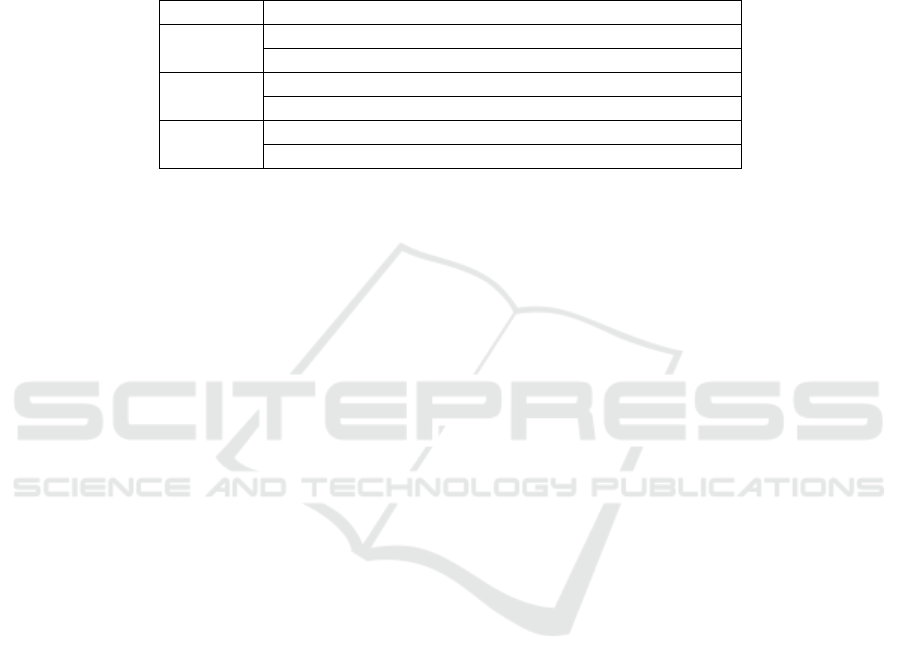
2.3 Criteria OA of The Hip
Table 1: Clinical (history, physical examination, laboratory) classification criteria for osteoarthritis of the hip, classification
tree format.
1
Hip pain
2a
And
Hip internal rotation < 15°
2b
And
ESR ≤ 45 mm/hour
(If ESR not available, substitute hip flexion ≤ 115°)
3a
Or
Hip internal rotation ≥ 15°
3b
And
Pain on hip internal rotation
3c
And
Morning stiffness of the hip ≤ 60 minutes
3d
And
Ages > 50 years
Hip pain
And
At least 2 of the following 3 features
ESR < 20 mm/hour
Radiographic femoral or acetabular osteophytes
Radiographic joint space narrowing (superior, axial, and/or medial)
Figure 3: Combined Clinical (history, physical examination, laboratory) and radiographic classification criteria for
osteoarthritis of the hip, traditional format.
2.4 Diagnosis
History
Physical examination
X-ray
CT scan
MRI
2.5 Management and The Goal
Pharmacological treatment:
o Analgesic: paracetamol
o NSAID
o Duloxetine
o Opioid: Tramadol
o Intra articular injection: corticosteroid
Rehabilitation management:
(Marks, 2015 ; Stemberger and Kerschan, 2013)
Osteoarthritis of the Hip
39
o Joint rest
o Physical modalities
o Exercise
o Appropriate joint use
o Weight control
o Assistive devices and orthosis
o Ergonomic and environmental adaptation
o Education
o Psychological intervention
o Surgery: Total Hip Replacement
Table 2: Combined clinical (history, physical examination, laboratory) and radiographic classification criteria for
osteoarthritis of the hip, classification tree format.
1
Hip pain
2
And
Femoral and/or acetabular osteophytes on radiograph
3a
Or
ESR ≤ 20 mm/hour
3b
And
Axial joint space narrowing on radiograph
The goal of Medical Rehabilitation are to decrease
pain/symptoms, Maintain and increase range of
motion, Maintain the strength of muscle, Increase
aerobic capacity, Optimize daily function, and
Minimize disability (Talmage and Lemke, 2001;
Hanada, 2003)
2.5.1 Joint Rest
In hip pain patients automatically tend to rest more,
but it will be better to advise patients with this
condition to get rest periods of 20 - 60 minutes
duration. Such rest periods allow the cartilage to
rehydrate. Although there is little scientific
evidence that rest or joint unloading might be
effective in preserving or improving the mobility
and work capacity of persons with osteoarthritis,
relief of pain is usually said to be proportional to the
amount of protection from weight bearing (Marks,
2015).
Muscles around a painful joint are thought to
fatigue more readily than muscles of a healthy pain
free joint, and can work more effectively if they are
not fatigued, protection from weight bearing appear
to influence the work capacity of individuals with
hip osteoarthritis. Rest can reduce or minimize joint
inflammation and protect an inflamed osteoarthritic
joint from further damage. Patients are advised to
make appropriate planning of activities and
avoidance of prolonged or repetitive activities
(Marks, 2015).
2.5.2 Physical Modality
To relieve pain transiently and to aid muscle
relaxation particularly during an acute flare of the
disease, and to treat associated inflammatory
conditions ice therapy or transcutaneous electrical
nerve stimulation can be considered. In mild sub-
acute or chronic disease phases, such modalities:
short wave diathermy and ultrasound applications,
may help to facilitate joint mobilization and
stretching procedures needed to maintain or increase
hip joint range of motion (Marks, 2015).
2.5.3 Exercise
Exercise is designed to reduce or prevent muscle
weakness and atrophy, maintain joint range of
motion, and improve endurance. The
implementation of exercises should not be stressful
or injurious to the joints. Since joint stiffness, pain,
disability and muscle weakness are related in
patients with hip osteoarthritis a series of carefully
graded non-weight bearing isometric strengthening
exercises carried out on a daily basis to improve hip
abductor and hip extensor muscle strength and
endurance. Once muscle spasm and any evidence of
joint inflammation have subsided, these exercises
might be progressed to pain free isotonic exercises
performed thrice weekly. Progressing too rapidly
could worsen pain, likely discouraging patients to
continue training. On the other hand, too light
exercise may remain ineffective (Uusi et al., 2017).
Well designed non-weight bearing or partial
weight bearing low-impact walking and conditioning
exercises performed within the limits of pain and
motion on a stationary bicycle, or in a warm pool
(temperature 30˚C -34˚C) and swimming exercises
in water, have all been shown to promote
functioning in those with no signs of acute
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
40

inflammation. The re-education of postural control
and balance is important to prevent fall (Marks,
2015), because falls, which can cause further
traumatic hip joint damage, are so common in
people with hip osteoarthritis.
Safety of an intervention is an important point.
In general, exercise is safe and well tolerated by
most patients with lower limb OA. However, the
patient has to be informed that disease activity can
vary from day-to-day, and that signs of excessive
exercise stress include joint pain during activity,
pain lasting more than 1–2 hour after exercise,
swelling, fatigue, and weakness (Stemberger et al.,
2013).
2.5.4 Appropriate Joint Use
Patients should be advised to avoid prolonged static
activities, contact sports, repetitive high impact
loading or over-exercising. Patients also should try
to carry out activities as ease and comfortable as
possible, and avoid rapid walking or needless stair
climbing. Hip joint stresses may also be lessened by
limiting the weight of loads carried (Marks, 2015).
2.5.5 Weight Control
The maintenance of an optimal body weight or the
implementation of a weight reduction program for
overweight or obese patients may reduce
unwarranted stresses on an osteoarthritic hip joint.
Another potential problem related to obesity that
could destroy articular cartilage, or cause greater
axial loading than the hip joint can accommodate
(Marks, 2015).
2.5.6 Assistive Device and Orthosis
It has been widely reported that people with hip
osteoarthritis who have unsteady gait or advanced
disease, may improve their functional capacity and
acquire some protection from untoward mechanical
perturbations of the affected joint through the use of
crutches, canes, walkers, or braces. It is further
believed that footwear designed to absorb shock,
shoes that give good support, shoes that have thin
non-slip soles, or the use of corrective foot orthotics
such as a heel lift in one shoe—if leg lengths are
unequal—may prove beneficial, while dress aids,
such as a long shoe horn or stocking stretcher, may
help to facilitate those daily activities that require
bending and reaching (Marks, 2015).
2.5.7 Ergonomic and Environmental
Adaptations
Adaptations to the home environment may further
relieve some unwarranted hip joint stresses that
could otherwise hasten hip joint damage. Joint
protection during functional activities may also be
enhanced by the use of raised toilet seats, grab bars
next to toilets and in tubs or shower facilities and
using adapted aid to do the activity of daily living
(Talmage and Lemke., 2001). Arm rests on chairs
and higher chairs may also prove beneficial for
people with end stage hip osteoarthritis who are not
candidates for surgery (Marks, 2015).
2.5.8 Education
For people with hip osteoarthritis, education about
their condition, and their role in its management, is a
vital first step towards lessening their level of
functional disability and decreasing their pain. They
may experience an overall improvement in life
quality when compared to those receiving no form
of education (Marks, 2015).
2.5.9 Psychological Intervention
Hip osteoarthritis can become a chronic pain and
make the patients get depression condition and need
psychological support to face the pain.
11,12
One study
found that patients whose spouses were involved in
their program had less pain and psychological
disability compared with patients whose spouses did
not participate (Talmage and Lemke., 2001).
2.5.10 Evidence Based and
Recommendation
Most frequently recommended for exercise is
aquatic exercise and biking because provide
cardiovascular training without putting undue stress
on the joint of lower extremity, so to prevent the
inflammation and increasing the pain (Talmage and
Lemke, 2001). The benefits such as increased
aerobic capacity, increased endurance, increased
muscular strength, assistance with weight loss,
psychological benefit: decreased stress, depression
and give socialization for that activity. Cochrane T
at al. (2005) reported: Group-based exercise in water
over 1 year can produce significant reduction in pain
and improvement in physical function in older adults
with lower limb OA, and may be a useful adjunct in
the management of hip and/or knee OA (Cochrane et
al., 2005). Fransen M et al. (2014) reported the
Osteoarthritis of the Hip
41
conclusions: Pooling the results of 10 RCTs
demonstrated that land-based therapeutic exercise
programs can reduce pain and improve physical
function among people with symptomatic hip OA
(Fransen et al., 2014). Larmer PJ (2014) conclude
that exercise and education is important thing in the
management of OA hip (Larmer et al., 2014).
Fernades L et al (EULAR - 2013) give 11
recommendation for the non pharmacological
management of knee and hip osteoarthritis such as
biopsychosocial approach, education, exercise,
weight loss, life style changes, walking aid
(Fernandes, 2013).
Table 3: Pharmacological recommendation for the initial management of hip OA.
We conditionally recommend that patients with hip OA should use one of the following:
Acetaminophen
Oral NSAIDs
Tramadol
Intra articular corticosteroid injections
We conditionally recommend that patients with hip OA should not use one of the following:
Chondroitin sulfat
Glucosamine
We have no recommendation regarding the use of the following:
Topical NSAIDs
Intra articular hyaluronate injection
Duloxetine
Opioid analgesics
*No strong recommendation were made for the initial pharmacologic management of hip osteoarthritis (OA). For
patients who have an inadequate response to initial pharmacologic management see the Results for alternative
strategies. NSAIDs: non steroidal anti inflammatory drug
Table 4: Non Pharmacological recommendations for the management of hip OA
We strongly recommend that patients with hip OA should do the following:
Participate in cardiovascular and /or resistance land based exercise
Participate in aquatic exercise
Lose weight (for persons who are overweight)
We conditionally recommend that patients with hip OA should do the following:
Participate in self-management programs
Receive manual therapy in combination with supervised exercise
Receive psychological intervention
Be instructed in the use of thermal agents
Receive walking aids, as needed
We have no recommendation regarding the following:
Participation in balance exercises, either alone or in combination with strengthening exercise
Participation in Tai Chi
Receive manual therapy alone
Table 5: Recommendations for hip OA: non pharmacological therapies.
Land-based exercise
1A
2A
Aquatic exercise
1A
2A
Lose Weight
1A
2A
Self-management program
1B
X
Manual therapy and physiotherapy
1B
X
Psychological intervention
1B
X
Thermal agents
1B
2B
Walking aids
1B
2B
Balance exercises
1C
X
Tai Chi
1C
X
Manual therapy alone
1C
X
Electrotherapy
X
2B
Therapeutic ultrasound
X
2B
Pulsed magnetic field therapy
X
2B
KONAS XI and PIT XVIII PERDOSRI 2019 - The 11th National Congress and The 18th Annual Scientific Meeting of Indonesian Physical
Medicine and Rehabilitation Association
42
Acupuncture
X
2B
Ergotherapy
X
2B
Manual massage
X
X
Mudpacks
X
X
Manual LD
X
X
A.
Strong. B Moderate. C Unable to recommend. X not mentioned
3 CONCLUSIONS
Practice points Rehabilitation of musculoskeletal
degenerative conditions should be patient-centered
and active participation should be emphasized
(Stemberger et al., 2013). Exercise therapy should
be the mainstay therapy when possible, with
physical modalities utilized as an adjunct. Evaluate
and correct for abnormal biomechanics, using
assistive devices and orthosis as necessary. Pain-
related fear will trigger avoidance of specific
movements and physical activity in general, called
fear of movement, which in turn will lead to
deconditioning. In other words, the muscles are
getting weaker, cardiovascular capacity will
decrease and as a result, not only is pain aggravated
(Hanada, 2003), but disability, lower quality of life
and depression are also observed (Marks, 2015 ;
Stemberger et al., 2013).
REFERENCES
Lespasio MJ, Sultan AA, Piuzzi NS, et al. 2018. Hip
osteoarthritis: A primer. Perm J, 22:17-084. DOI:
https://doi.org/10.7812/TPP/17-084
Bennell K.2013. Physiotherapy management of hip
osteoarthritis. Journal of Physiotherapy, 59: 145-57.
Suri P, Morgenroth DC, Hunter DJ. 2012. Epidemiology
of osteoarthritis and associated comorbidities. Physical
Medicine and Rehabilitation, 4: S10-S19
Lohmander LS, Englund PM, Dahl LL, Roos EM. 2007.
The long-term consequence of anterior cruciate
Ligament and meniscus injuries: osteoarthritis.
American Journal of Sports Medicine, 35: 1756-79
Marks R. 2015. Non-operative management of hip
osteoarthritis. Pain Studies and Treatment, 3: 7-22.
http://dx.doi.org/10.4236/pst.2015.32002
Stemberger R, Kerschan-Schindl K. 2013. Osteoarthritis:
physical medicine and rehabilitation –
nonpharmacological management. Wien Med
Wochenschr, 163:228–235. DOI 10.1007/s10354-013-
0181-9
Talmage DM, Lemke CL. 2001. Common conditions of
the lower extremity. In: Bougie JD, Morgenthal AP,
eds. The aging body. Conservative management of
common neuromusculoskeletal conditions. New York:
McGraw-Hill Companies, 205-42
Hanada EY. 2003. Efficacy of rehabilitative therapy in
regional musculoskeletal condition. Best Practice &
Research Clinical Rheumatology, 17: 151-66
Uusi_Rasi K., et al., 2017. Exercise training in treatment
and rehabilitation of hip osteoarthritis: a 12-week pilot
trial. Journal of Osteoporosis, 1-7
Talmage DM, Lemke CL. 2001. Common conditions of
the lower extremity. In: Bougie JD, Morgenthal AP,
eds. The aging body. Conservative management of
common neuromusculoskeletal conditions. New York:
McGraw-Hill Companies, 205-42
Nadler SF. 2004. Non pharmacologic management of pain.
JAOA, 11(8): 6-12
Cochrane T, Davey RC, Matthes Edwards SM. 2005.
Randomised controlled trial of the cost-effectiveness
of water-based therapy for lower limb osteoarthritis.
Health Technol Assess, 9(31):iii-1v, 1x-xi,1-114
Fransen M, McConnell S, Hernandez-Molina G,
Reichenbach S. 2014. Exercise for osteoarthritis of the
hip. Cochrane Database of Systematic Reviews, Issue
4. Art. No.: CD007912. DOI:
10.1002/14651858.CD007912.pub2.
Larmer PJ., et al., 2014. Systematic review of guidelines
for the physical management of osteoarthritis.
Archives of Physical Medicine and Rehabilitation,
95:375-89
Fernandes L. 2013. EULAR recommendations for the
non-pharmacological core management of hip and
knee osteoarthritis. Ann Rheum Dis, 72:1125–1135.
doi:10.1136/annrheumdis-2012-202745
Hochberg MC., et al., 2012. American college of
rheumatology 2012 recommendations for the use of
nonpharmacologic and pharmacologic therapies in
osteoarthritis of the hand, hip, and knee. Arthritis Care
& Research, 64: 465-74
Osteoarthritis of the Hip
43
