
Translingual Neurostimulation in Late Residual Stage Cerebral Palsy
Children Treatment Affects Functional Brain Networks
A. Yu. Efimtsev
1
, T. S. Ignatova
2
, A. G. Trufanov
3
, A. G. Levchuk
1
, G. E. Trufanov
1
,
E. N. Kondratyeva
1
, N. Yu. Shmedyk
1
, A. M. Sarana
2,5
, S. G. Shcherbak
2,5
and Yu. P. Danilov
4
1
The Almazov National Medical Research Centre, St. Petersburg, Russian Federation
2
St. Petersburg State Healthcare Institution “City Hospital No. 40”, 197706, Borisova str., 9, St. Petersburg, Russia
3
Military Medical Academy n.a. S. M. Kirov, Akademika Lebedeva str., 6, St. Petersburg, Russia
4
Institute of Physiology n.a. I.P. Pavlov, Russian Academy of Sciences, Makarova Embankment, 6, St. Petersburg, Russia
5
St. Petersburg University, University Embankment 7-9, St. Petersburg, Russia
Keywords: Neuro-electrostimulation, Neuroimaging, Functional MRI, Cerebral Palsy.
Abstract: Management of cerebral palsy is an actual problem of modern medicine. A new direction of
neurorehabilitation, intensively discussed in modern science and practice, includes various types of electrical
stimulation. Constant stimulation of the nervous system is one of the most popular ways to activate neural
networks to activate the brain and initiate neuroplasticity processes. Participants in the experiment were
children with cerebral palsy, spastic diplegia form at the age of 6 to 19 (n = 6) (mean age - 17,9 ± 5,6 years).
All subjects underwent standard treatment, including massage, therapeutic gymnastics simulators, robotic
mechanotherapy, etc., which lasted 20-25 minutes with neurostimulation of the brain (using a PoNS device).
All subjects underwent a resting state functional MRI once before and twice - after neurostimulation course.
Results indicate positive dynamics in all subjects: most of them learned walking without aids, obtained
decreased muscle tonus and improvement in balance, coordination function were noted. Neurostimulation
with the PoNS device combined with curative gymnastics (focused exercises), improves the efficiency of
motor functions and the development of motor skills. Resting state functional MRI showed improvement in
brain networks. If performed properly, it can be an auxiliary method of objective control of treatment
effectiveness.
1 INTRODUCTION
In subjects with cerebral palsy, there are apparent
violations of equilibrium, the position of motion,
retention of the pose in space. Each function of the
human body is based on well-organized complex
neural networks, including numerous interconnected
structures (cortex, nuclei, neural clusters) located in
different levels of brain and spinal cord.
Collaboration and synchronization of human
performance in behavioral, cognitive and autonomic
functions. This close integration is especially
important in complex sensory and motor functions,
such as vision, hearing, balance, gait, speech.
Neurorehabilitation of children with cerebral
palsy is multicomponent and includes physiotherapy,
special massage therapy, treatment, special limb
treatment with different stitches, the use of fixing
devices for walking, special, facilitating the motor
activity of the child, and costumes. In modern
medicine, the problems of rehabilitation of children
with cerebral palsy are given particular attention. A
new direction of neurorehabilitation, intensively
discussed in contemporary science and practice, is the
use of various types of electrostimulation, as well as
their use in or in combination with existing
procedures. The most common among them - are
electrical stimulation of muscles and nerves, as well
as the spinal cord. Electrical stimulation was used to
treat spastic Erb-Duchenne paralysis in 1871. Since
the treatment of patients with spasticity by electrical
stimulation of the muscles and nerve structures, skin,
subcutaneous, epidural electrodes, as well as peroneal
implantations have been used (Morenko et al., 2015).
Despite the positive results achieved by an integrated
approach of treatment, the problem of rehabilitation
of children with cerebral palsy in the late residual
stage with persistent stereotypes remains unresolved.
Efimtsev, A., Ignatova, T., Trufanov, A., Levchuk, A., Trufanov, G., Kondratyeva, E., Shmedyk, N., Sarana, A., Shcherbak, S. and Danilov, Y.
Translingual Neurostimulation in Late Residual Stage Cerebral Palsy Children Treatment Affects Functional Brain Networks.
DOI: 10.5220/0007698205490556
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 549-556
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
549

The issue of restoring muscle control and complex
sensorimotor integration (balance, movement
coordination, body retention in space) has not been
given the necessary attention so far. Artificial
stimulation of the nervous system is one of the most
popular ways to activate neural networks to activate
the brain and initiate neuroplasticity processes
(Danilov et al., 2006).
2 MATERIALS AND METHODS
2.1 Neurostimulation
An innovative alternative method of using peripheral
neurostimulation for neurorehabilitation was
presented by Yu. P. Danilov at the World Congress
on Psychophysiology in St. Petersburg in 2010. This
method was developed at the University of
Wisconsin, USA, in a laboratory headed by the
famous scientist Paul Bach-Rita, one of the founders
of the modern concept of neuroplasticity. In the
laboratory of haptic communication and
neurorehabilitation (TCNL), a device was developed
for electro-tactile stimulation of human skin, and in
the most densely innervated tactile region, the tongue
(Danilov et al., 2008). Electrotactic stimulation of the
tongue is, at the moment, the most effective and safest
stimulation of the central nervous system. The tongue
is the thinnest part relative to other surfaces of the
skin, saturated with various types of mechanical,
thermal and taste receptors, with the addition of free
nerve endings. This zone has a maximum density of
mechanoreceptors per unit area and has a minimum
two-point discrimination threshold: 0.5-1 mm for
mechanical stimulation and 0.25-0.5 mm for
electrical stimulation (Danilov et al., 2007). Two
main cranial nerves (branches of the trigeminal,
20,000-22,000 nerve fibers and the facial nerve,
3,000-6,000 nerve fibers) from the front surface of the
tongue transmit nerve impulses directly to the brain
stem structures. They activate the complex of the
trigeminal nerve (mesencephalic, sensory and spinal)
the largest nuclei of the trunk) and simultaneously
along the branch of the facial nerve the adjacent
nucleus of the solitary tract is stimulated. The
cochlear nuclei, the structures of the medulla and the
upper sections of the cervical spine (C2 and C3) are
activated directly also. The reticular formation of the
brain stem, the complex of vestibular nuclei and the
ventral part of the cerebellum fall into the zone of
secondary activation (Barbara et al., 2009). As you
know, the brain stem area has a massive accumulation
of neural nuclei (86), some of them are engaged in
autonomous regulation (blood circulation,
respiration), the other part - sensorimotor integration.
It is not necessary to exclude the possible secondary
activation of several common systems of
neurochemical regulation of brain activity, the nuclei
of which are located in the brain stem - noradrenergic,
dopaminergic, serotonergic and acetylcholinergic.
Descending paths regulating the activity of spinal
cord motoneurons, namely: the trigeminal-spinal,
solitary-spinal, and three vestibulo-spinal, directly
involved in the regulation of the activity of the lower
limbs and walking, come from the same area
(Mitchele et al., 2009). Intensive rhythmic
stimulation of existing neurons leads to the
corresponding activation of synaptic contacts and
axons, including the whole complex of pre- and
postsynaptic neurochemical mechanisms (Ignatova et
al., 2018). Phenomena such as long-term potentiation
or depression of neural networks may underlie the
effects observed when using electro-tactile
stimulation of the tongue. Long-term potentiation
(Long-term potentiation, LTP), as well as long-term
depression (Long-term inhibition, LTI), is the
enhancement or suppression of synaptic transmission
between two neurons that persists for a long time after
exposure to the synaptic pathway. LTP is involved in
the mechanisms of synaptic plasticity, providing the
nervous system of a living organism with the ability
to adapt to changing environmental conditions
(Patriat et al., 2013). Most neurophysiological
theorists believe that long-term potentiation together
with long-term depression underlies the cellular
mechanisms of memory and learning (Lomo, 2003).
At the moment, the device for electrotactile
stimulation is called PoNS (Portable
Neurostimulator), and its use for stimulation of the
brain in children with cerebral palsy is a new direction
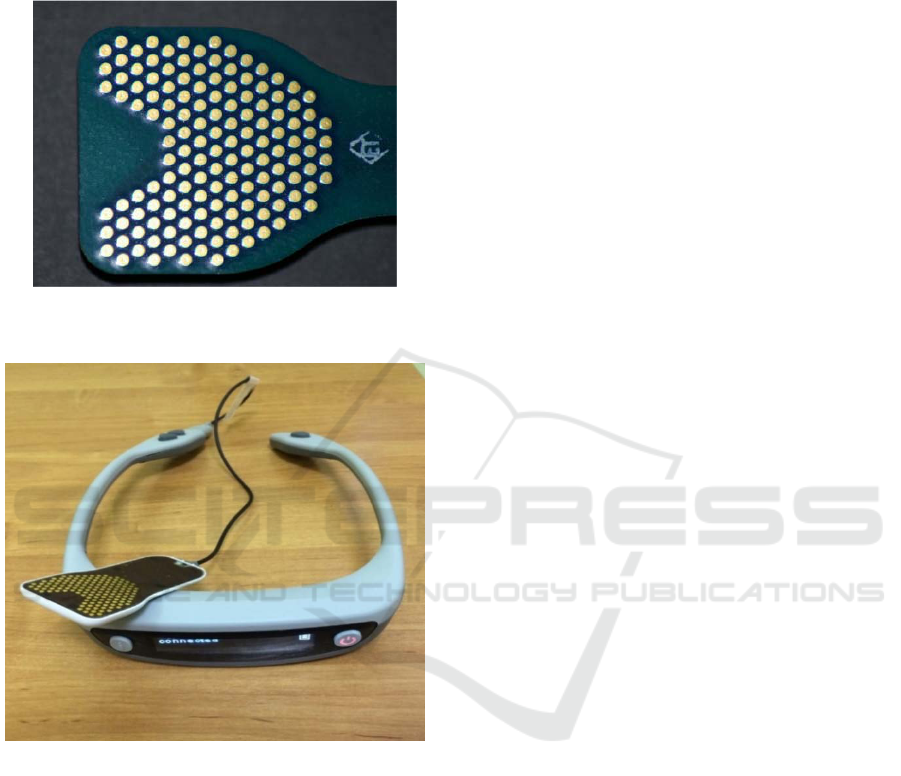
in neurorehabilitation. The matrix, in which are the
electrodes of irregular shape; optimized to stimulate
the most sensitive areas of language. The matrix itself
includes 143 electrodes divided into nine 16 -
electrode sectors (Fig.1). Within each segment, only
one electrode is active at a given time, and the rest are
grounded. Stimulation through one electrode occurs
simultaneously in nine sectors. The electrodes are
alternated with a frequency of 50 Hz. The incentive is
a triplet of rectangular pulses of microsecond
duration.
Regular stimulation from the PoNS device,
activating vast areas of the brain, increases the
efficiency of existing neural networks, increases the
likelihood of the formation of new synaptic contacts
(synaptogenesis), enhances the brain's innate ability
to improve motor function. The goal of successful
NNSNT 2019 - Special Session on Non-invaisive Neuro-stimulation in Neurorehabilitation Tasks
550
neurorehabilitation with such stimulation is to restore
motor function or to teach new motor skills, achieved
by combining specialized exercises with extensive
brain activation using the PoNS device.
Figure 1: The PoNS device (Portable Neurostimulator), the
close-up of the matrix.
Figure 2: The PoNS device (Portable Neurostimulator).
The studies were conducted in patients with
peripheral and central vestibular disorders (Badke et
al., 2011; Chisholm et al., 2014; Bach-y-Rita, 2008;
Wildenberg et al., 2013) multiple sclerosis, stroke
(Wildenberg et al., 2011), TBI and spinal injuries
(Joseph et al., 2011; Kublanov, 2008; Kublanov et al.,
2018). The high efficiency of peripheral
neurostimulation was shown in combination with
specialized physiotherapy in restoring general motor
control of the body, balance, walking, speech, eye
movements, various aspects of sensorimotor
integration. Additional studies, using functional MRI,
unequivocally confirmed the presence of potent
activation of the brain stem and the ventral part of the
cerebellum during stimulation of the tongue, as well
as the presence of long-lasting aftereffect, the
preservation of foci of activity in the brain of subjects
for hours and even days after the last stimulation
(Efimtcev et al., 2018). Additional data analysis
showed that simultaneously with the activation of the
subcortical structures of the brain, the coefficients of
communication between the cortex areas of the brain
involved in integrative training processes also change
(Petrenko et al., 2017).
2.2 Participants
This study involved six children with a cerebrally
palsy, form of spastic diplegia. Patients with intact
intellect, no seizures in anamnesis. All children
obtained standard treatment, including massage,
medical gymnastics with simulators, robotic
mechanotherapy, hydrotherapy, and 10 daily sessions
of physical therapy, which lasted for 20-25 minutes
and neurostimulation of the brain (using the PoNS
device). Patients underwent functional MRI of the
brain before the start of and at the end of the course
of treatment using neurostimulation. The patients
were aged 8 to 14 years. Patients were evaluated by
standard scales GMFSC Scale (gross motor skills),
FMS (functional motor scale), Berg balance scale, the
Ashworth scale (spasticity).
All patients underwent resting state fMRI at three
timepoints - before the course of neurostimulation,
within 3 days after the end of the course of
neurostimulation, and in 1 month after
neurostimulation. The parameters of the pulse
sequence were: BOLD technique, repetition time
(TR) - 3000 ms, echo time (TE) - 30 ms, spin rotation
angle (FA) - 90°, FOV - 192 mm, matrix - 64 × 64,
slice thickness - 4.5 mm, the number of slices - 29,
the number of repetitions - 120, the scan time - 6
minutes. Patients were instructed to lie with their eyes
open (do not sleep), without fixing their gaze. Thus,
for all subjects, there were identical conditions of a
state of rest, and this had a minimal impact on the
visual and aural working networks of the brain.
Also, all patients underwent structural MRI with
obtaining T1 and T2 weighted images and FLAIR
(Fluid attenuated inversion-recovery) to exclude
brain tumors and other pathological morphological
changes. The T1-weighted gradient echo MP-RAGE
(Magnetization Prepared Rapid Acquired Gradient
Echoes) pulse sequence — a gradient echo with
magnetization preparation and fast collection — was
used to align fMRI images with the anatomical
structures of the brain. The main feature of this
sequence is its high resolution and isotropic voxel
with a volume of 1.2 mm
3
.
Translingual Neurostimulation in Late Residual Stage Cerebral Palsy Children Treatment Affects Functional Brain Networks
551
The parameters of the MP-RAGE pulse sequence
were: repetition time (TR) - 2300 ms, echo time (TE)
- 3 ms, spin rotation angle (FA) - 9 °, FOV - 240 ×
256 mm, matrix - 256 × 240, slice thickness - 1.2 mm,
the number of slices - 160, the number of repetitions
- 1, scanning time - 9 minutes. Details of the
parameters of all pulse sequences are presented in
Table 1.
Table 1: MRI Examination Protocol.
Pulse
sequence
Scan time Parameters
T2 TSE
(axial plane)
2 m. 30 s.
FOV – 220×220 mm, slice
thickness – 4.0 мм, TR –
6000 ms, ТЕ – 93 ms,
matrix – 320×320, slice
number
–
27
T2 TIRM
(axial plane)
4 m. 30 s.
FOV –199×220 mm, slice
thickness – 4.0 мм, TR –
9000 ms, ТЕ – 93 ms,
matrix – 256×232, slice
number
–
27
MPRAGE 9 m
FOV – 240×256 mm, slice
thickness – 1.2 мм, TR –
2300 ms, ТЕ – 3 ms, matrix
– 256×240, slice number –
160
BOLD FRMI
(resting state)
6 m
FOV – 192×192 mm, slice
thickness – 4.5 мм, TR –
3000 ms, ТЕ – 30 ms,
matrix – 64×64, slice
number
–
36
Statistical processing and evaluation of the results
of neuroimaging studies of each patient individually
and their group (rest fMRI data) was carried out using
the software package CONN v.18 (Functional
connectivity toolbox). The software was designed to
determine the relationships between various brain
regions, including the dynamic mode, statistical
mapping of activation zones, identifying the structure
of multiple rest networks and working functional
networks of the brain. We used analysis based on the
choice of the region of interest (ROI-to-ROI and
Seed-to-Voxel), as well as analysis based on graph
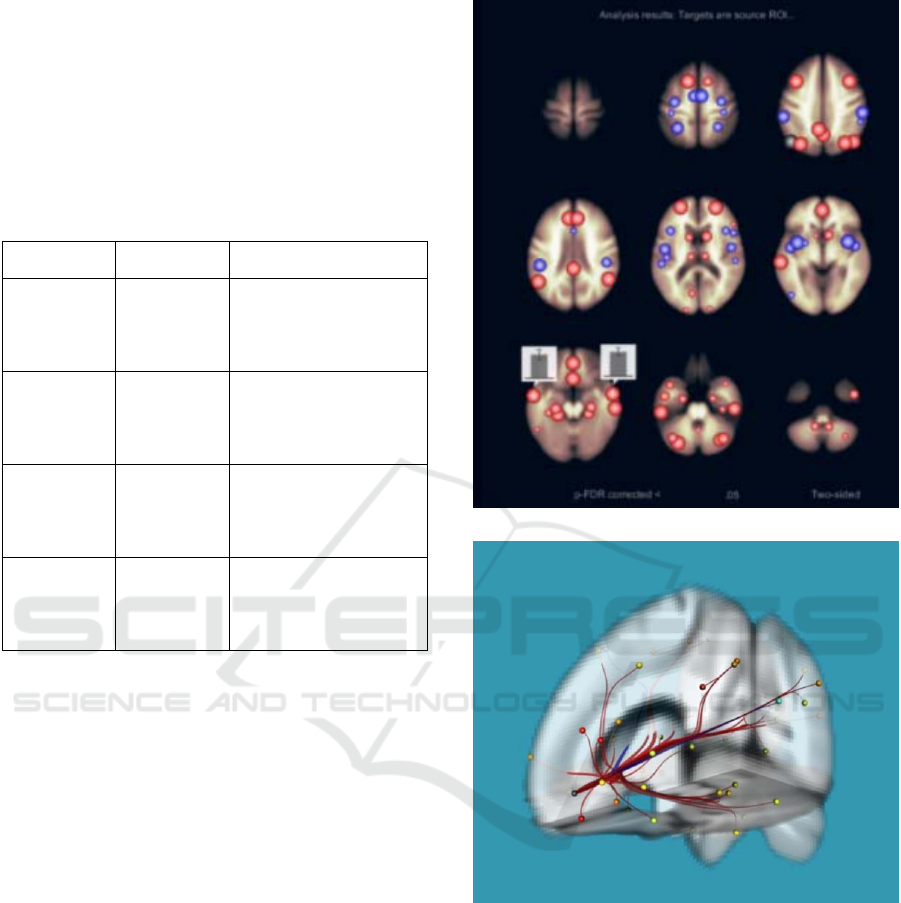
theory (Fig. 3).
3 RESULTS
The first patient before the course of treatment could
walk using multi-support canes within the room, and
used walkers for longer distances (500 meters or
more), after the course of treatment he mastered
walking using one single-support cane within the
room and at school, for longer distances uses multi
support sticks. Before the treatment, the second
patient used multi-support canes for walking within
a)
b)
Figure 3: Graphical representation of the results of
intergroup statistical analysis based on the choice of the
zone of interest (ROI-to-ROI): a - maps with a schematic
representation, combined with an anatomical atlas of the
brain; b - 3D reconstruction of the map of positive and
negative functional connections, combined with the
anatomical atlas of the brain.
the room, and on the street, the patient could not stand
on his own without support, after finishing the course
of treatment he learned to walk independently on a
flat surface (within the room), the patient can stand
on his own without a support and on the street uses
one single support cane. The third patient, before the
NNSNT 2019 - Special Session on Non-invaisive Neuro-stimulation in Neurorehabilitation Tasks
552
start of the course of treatment, used a walker within
the room to walk, a stroller was used at school and for
longer distances. After completing the course of
treatment, the patient has mastered multi-support
canes within the room, the walker is using at school
and can walk to the playground, and an active type
stroller is used for longer distances. Before the
treatment, the fourth patient walked using two single-
support canes within the premises and on the street,
could stand for several seconds without support, at the
end of the course of treatment he learned to walk
independently on a flat surface, he stands alone on the
street, using one single-bearing cane on the street.
The fifth patient, before the course of treatment, used
multi-support canes for walking, at the end of the
treatment course, he mastered walking within the
premises, relying on one single-bearing cane, and
using multi-support canes for longer distances.
One patient with the level of GMFSC
development 4, before the course of treatment, could
move around with the walker within the room, an
active type of stroller was used at school and on the
street. At the end of the course of treatment the patient
learned to walk using multi-support canes within the
room and at school for more long distance confidently
uses walkers. Also, all patients showed a decrease in
muscle tone and an improvement in balance and
coordinating function. The equilibrium
improvements estimated on the Berg scale ranged
from 2 to 7 units (4.5 on average), and as a percentage
of the initial state, the improvement was observed
from 12 to 70% (31% on average) (Fig. 4).
Figure 4: Berg scale (patients data).
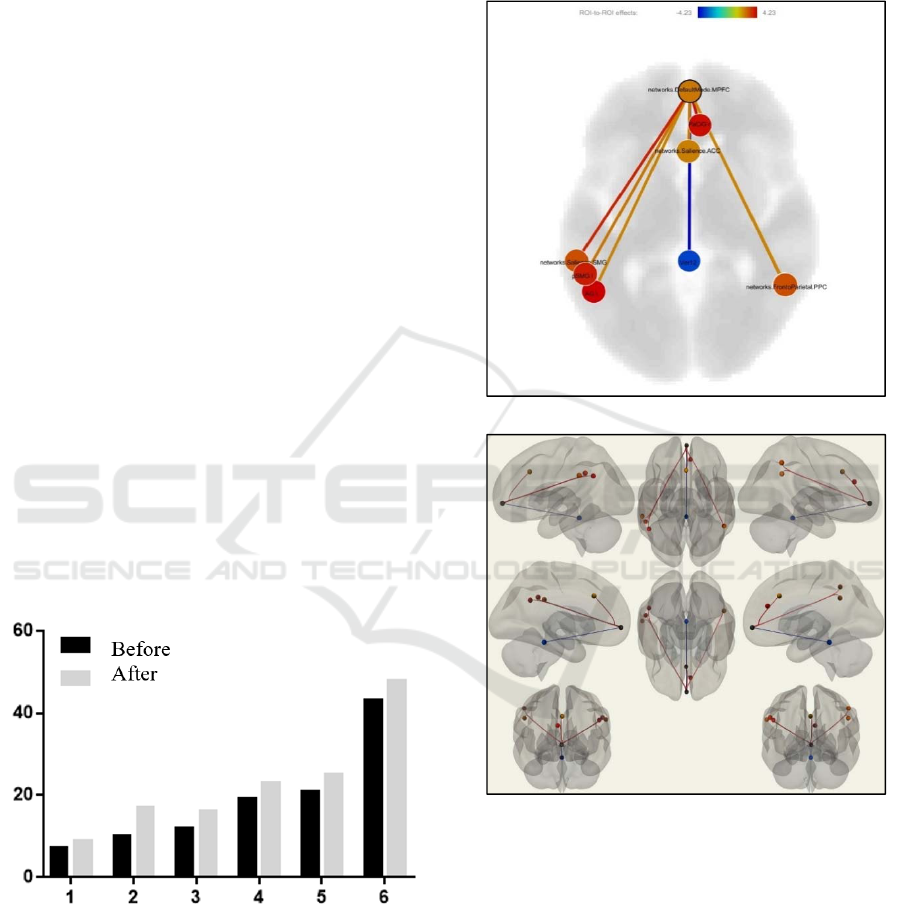
As the result of intergroup statistical analysis
(two-sample t-test, comparing the resting state in the
first and second timepoints), we noticed the
enhancement of the functional connections (FC) and
the interaction of the MPFC with the posterior
parietal cortex on the right, frontoparietal cortex,
anterior sections of cingulate cortex (ACC),
supramarginal and angular gyri on the left. All of
them are parts of a default mode network (DMN). At
the same time, we found decreased FC of MPFC and
the cerebellar worm (p FDR-corr. <0.05) (Fig. 5,
Table 2).
(a)
(b)
Figure 5: The result of a group comparison of patients in the
second and first timepoints. The areas of statistically
significant differences are shown: increase and decrease of
the functional connectivity in diagram (a) and on the 3D
model (b) (cont.).
When performing intergroup statistical analysis
(two-sample t-test, comparing the state of rest in the
first and third timepoints), the changes were less
expressed. The MPFC FC with the paracingulate gyri
on the right and the ACC intensified even more, and
the FC with the posterior occipital cortex on the left
decreased (p FDR-corr. <0.04) (Fig. 6, Table 3).
Translingual Neurostimulation in Late Residual Stage Cerebral Palsy Children Treatment Affects Functional Brain Networks
553
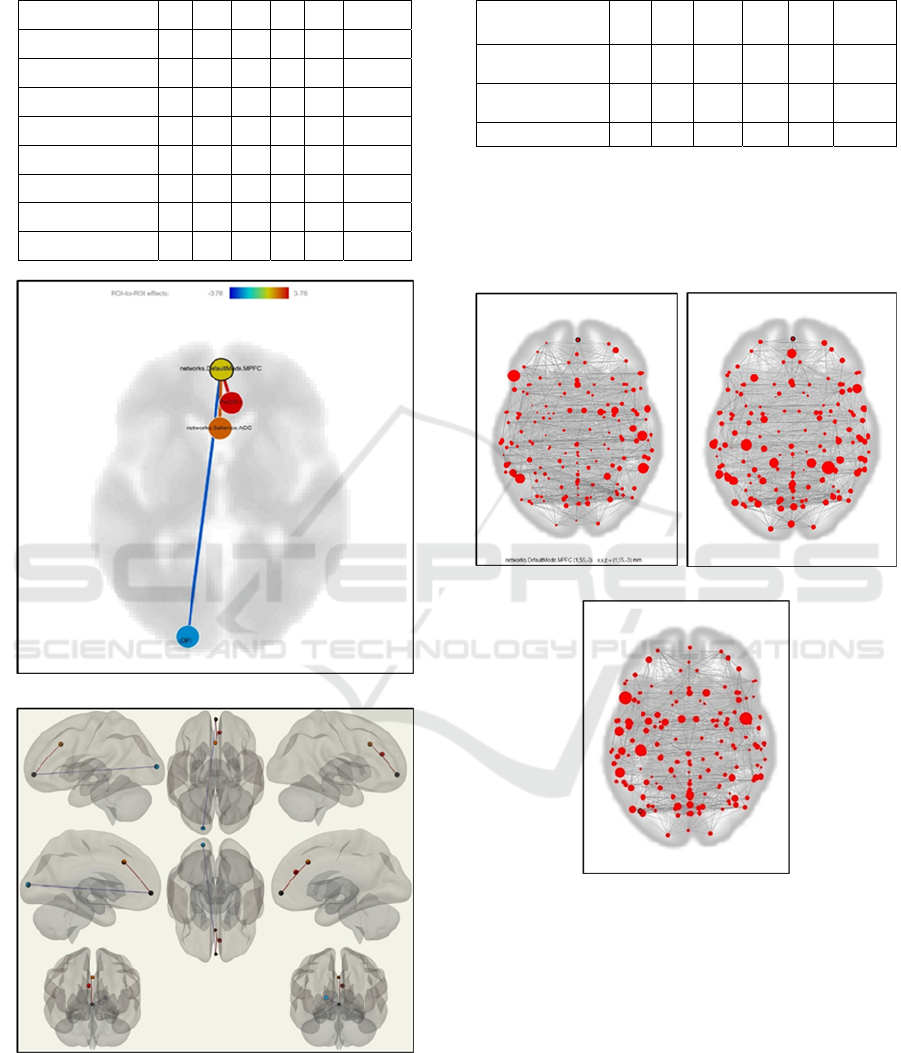
Table 2: The results of a group comparison of patients in
the second and first timepoint.
(a)
(b)
Figure 6: The result of a group comparison of patients in the
third and first timepoint. The areas of statistically
significant differences are shown: increase and decrease of
the functional connectivity in diagram (a) and on the 3D
model (b).
Table 3: The results of group comparison of patients in the
second and first timepoint.
When performing analysis based on graph theory,
global efficiency has become more expressed at the
second and third timepoints, compared to the first
timepoint (p FDR-corr.<0.05 for each time point)
(Fig. 7).
a b
c
Figure 7: The result of the analysis based on graph theory
at different timepoints: a – the first timepoint (before the
course of treatment), b – the second timepoint (immediately
after the course of treatment), c – the third timepoint
(delayed study).
4 DISCUSSION
The simultaneous combination of TLNS with
specialized exercises allows to influence all
components of motor activity: central (cortical),
Brain area
Hemis
phere
T Voxels
% of
atlas
Volume
mm
3
MNI
coordinates
(x,y,z)
atlas.Ver12 (Vermis 1 2)
-4.23
41 87 328 1,-40,-11
atlas.PaCiG r (Paracingulate Gy*ght)
r
3.96
213 16 1704 7,37,23
networks.Salience.SMG (L) (-
60,*,31)
l
3.73
416 44 3328 -60,-39,-31
atlas.AG r (Angular Gyrus Right)
r
2.98
630 43 5040 54,-50,-17
atlas.pSMG l (Supramarginal
Gyr*eft)
l
2.63
431 41 3448 -55,-46,33
networks.Salience.ACC (0,22,35)
2.52
147 6 1176 0,21,-15
atlas.AG l (Angular Gyrus Left)
l
2.42
334 35 2672 -50,-56,30
networks.FrontalParietal.PPC
(R)*,45)
r
2.37
52,-52,32
Brain area
Hemisp
here
T Voxels
% of
atlas
Volume
mm
3
MNI
coordinates
(x,y,z)
atlas.PaCiG r (Paracingulate
Gy*ght)
r
3.76
102 8 816 7,37,23
networks.Salience.ACC
(0,22,35)
2.74
250 10 2000 0,22,35
atlas.OP l (Occipital Pole Left) l
-2.66
171 6 1368 -17,-97,7
NNSNT 2019 - Special Session on Non-invaisive Neuro-stimulation in Neurorehabilitation Tasks
554

subcortical (basal ganglia, cerebellum, brain stem),
spinal cord centers. Thus, multilevel
neurostimulation allows activating not only muscle
control (decrease in tone) but also such complex
sensorimotor functions as balance and movement
coordination when walking, which, in combination
with physical rehabilitation, helps to master and
develop new motor skills quickly.
The positive effects persisted (or decreased, but
slightly) during the many months of interruption (up
to one year) between the courses of therapy, which is
confirmed by our fMRI study. It shows that the
dynamical changes in brain during the course are
obvious, and there were also improvements a month
later, though they were not so significant compared to
the second one, the clinical condition of the patients
confirms this fact. They did not have negative
dynamics. This allowed us to consistently improve
the symptoms, being studied, with each subsequent
course, i.e. neurostimulation gives to rehabilitation a
cumulative (accumulative) effect.
It is traditionally considered that a child with
cerebral palsy reaches half of its potential to develop
motor skills by the age of 5 years and the maximum
possible development by 7 years. The potential
achieved remains at the same level or may even
worsen with age. In our experiments, all children
were over the age of 7 years. These results can
significantly expand both the scope of this technology
in the rehabilitation of children with cerebral palsy
and improve the prediction of the effectiveness of the
therapy used for older children.
Brain TLNS enhances the effect of physical
rehabilitation, activating vast areas of the brain,
increases the efficiency of existing neural networks,
increases the likelihood of new synaptic contacts
(synaptogenesis), enhances the brain's innate ability
to improve motor function. The fMRI data alone
confirms that the human brain is plastic at any age and
is capable of an amazing reorganization, the
mechanisms of which we are just beginning to
explore. The dynamics of changes in DMN and
functional connections between the first and second
timepoints turned out to be more vivid than between
the first and third timepoints. That probably indicates
a delayed rehabilitation effect.
5 CONCLUSION
Taking into the attention the limited and minimal
intensity of training, the main task of the study was
limited to the formation of new motor skills. The
patient in 10 sessions had to form a new motor skill,
consolidate it and use it in everyday life. Based on
these considerations, it is clear why the index of
general motor control (FMS scale) has statistically
significantly improved. Since the development of
motor control skills was the task of training, besides
general improvement in functional connectivity,
certain parts of motor neural networks improved their
level of functional activity as a result of
neurostimulation. This technique is innovative in the
field of neurostimulation, non-invasive, safe and easy
to use. Indeed, the daily 20-minute stimulation of the
tongue for two weeks increases the innate ability of
the brain to improve motor function, contributes to
the formation of new motor skills.
The use of neurostimulation using the PoNS
device, in combination with therapeutic exercises
(targeted exercises), can improve the efficiency of the
recovery of motor functions and the development of
motor skills.
The use of resting state functional MRI allows to
obtain data without having to perform special tasks
for children, which simplifies the method of objective
monitoring, as well as it provides better and more
detailed information about the functional state of the
brain than with task-based fMRI. This pilot study data
allows to consider the fMRI technology as the
objective tool for the neuro-electrostimulation
mechanisms investigation. The data could also form
new treatment techniques of the non-invasive multi-
electrode neck neural structures neurostimulation
application for treatment of the psychiatric and
neurological disorders, exactly – disorders
accompanied by the neurodegeneration (Alzheimer
disease, Parkinson disease, dementia), consequences
of the brain traumas, neurotoxic actions, depressive
and anxiety disorders, strokes.
ACKNOWLEDGEMENTS
The work was supported by Act 211 Government of
the Russian Federation, contract № 02.A03.21.0006.
The authors thank Ivan Brak, Elena Filimonova and
Eugenia Kobeleva for participation in the data
processing.
REFERENCES
Arkady J. Diseases of the nervous system in children / M.:
BINOM, 2013; 568 s
Morenko E.S., Vissarionov S.V., Umnov V.V.,
Monoshkina T.R., Gerasimenko Yu.P., Baindurashvili
A.G. Functional and spinal stimulation in complex
Translingual Neurostimulation in Late Residual Stage Cerebral Palsy Children Treatment Affects Functional Brain Networks
555

rehabilitation with cerebral palsy // Vedical Sciency;
2015; 2: 40-46.
Danilov, Y. P., Tyler, M. E., Kaczmarek K. A. Vestibular
sensory substitution using tongue electrotactile display.
Human Haptic Perception: Basics and Applications.
Birkhauser Basel Switzerland, 2008; 467-480.
Danilov, Y.P., M.E. Tyler, K.L. Skinner, R.A. Hogle, and
P. Bachy-Rita. Efficacy of electrotactile vestibular
substitution in patients with peripheral and central
vestibular loss // J Vestib Res; 2007; 17: 119–130.
Danilov, Y.P., Tyler M.E., Skinner K.L., Bach-y-Rita P.,
Efficacy of electrotactile vestibular substitution in
patients with bilateral vestibular and central balance
loss // Conf Proc IEEE Eng Med Biol Soc; 2006: 6605–
6609.
Barbara Susan Robinson, PT, DPT, Jeanne L. Cook, PT,vs,
Cynthia McCormick Richburg, PhP, CCC-A, and
Stephen Pria, PT, MPT. Use of an Electotactile
Vestibular Substitution System to Facilitate Balance
fnd Gait of an Individual with Gentamicin- Induced
Bilateral Vestibular Hypofunction and Bilateral
Transtibial Amputation // JNPT 2009;33 150-159.
Mitchele E., Jacquelin G. and Yuri P. Danilov. Spatial
Vapping of Eltctrotactile Sensation Threshold and
Intersty Range jn the Human Tongue: Initial Results.
IEEE Engineering in Medicine and Biology Society.
Conference 2009:559-62
Lomo T. The discovery of long-term potentiation // Philos
Trans R Soc Lond B Biol Sci; 2003: 17-20.
Badke MB, Sherman J, Boyne P, Page S,Dunning K.
Tongue-based biofeedback for balance in stroke:results
of an 8-week pilot study // Arch Phys Med Rehabil,
2011; 92 (13); 64-70.
Amanda E Chisholm, Raza Naseem Malik, Jean-Sébastien
Blouin, Jaimie Borisoff, Susan Forwell Tania Lam.
Feasibility of sensory tongue stimulation combined
with task-specific therapy in people with spinal cord
injury // Journal of NeuroEngineering and
Rehabilitation, 2014; 11; 96.
Bach-y-Rita P. Late postacute neurologic rehabilitation:
Neuroscience, engineering, and clinical programs //
Arch Phys Med Rehabil; 200; 84:1100–1108.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M. Altered Cоnnectivity of the Balance
Proccessing Network After Tongue Stimulation in
Balance-Impaired Individuals // Brain Connectivity;
2013; 3 (1): 87-97.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M. High-resolution fMRI defects
neuromodulation of individual brainstem nuclei by
electrical tongue stimulation in balance-impaired
individuals // Neuroimage; 2011; 56 (4): 2129-2137.
Wildenberg J., Tyler M.E., Danilov Y.P., Kaczmarek K.,
Meyerand M. Electical Tongue Stimulation Normalires
Activity Within the Motion-Sensitive Brain Networt in
Balance-Impaired Subjects as Revealed by Group
Indtpendent Component Analysis // Brain connectivity;
2011; 1 (3): 255-265.
Bach-y-Rita P. Theoretical basis for brain plasticity after a
TBI // Brain Inj; 2003; 17: 643–651.
Joseph C. Wildenberg, Mitchell E.Tyler, Yuri P. Danilov,
Kurt A. Kaczmarek, Mary E. Meyerand High-
resolution fMRI detects neuromodulation of individual
brainstem nuclei by electrical tongue stimulation in
balance-impaired individuals// Journal Neurolmage 56
(2011) 2129-2137.
Kublanov V.S. A hardware-software system for diagnosis
and correction of autonomic dysfunctions // Biomedical
Engineering, 2008. – Vol. 42, № 4. – pp. 206-212
Kublanov V.S., Babich M.V., Petrenko T.S. New Principles
for the Organization of Neurorehabilitation //
Biomedical Engineering, 2018. –Vol. 52, № 1. – pp. 9-
13.
Kublanov V.S., Babich M.V., Dolganov A.Y. Research
Article: Mobile Hardware-Information System for
Neuro-Electrostimulation. – Hindawi. Mobile
Information Systems. – Volume 2018. – Article ID
2168307. – 7 pages.
Petrenko T., Kublanov V., Retyunskiy K. The role of
neuroplasticity in the treatment of cognitive
impairments by means multifactor neuro-
electrostimulation of the segmental level of the
autonomic nervous system. – European Psychiatry,
2017. – Vol. 41. – page S770.
Efimtcev A., Kublanov V., Aftanas L., Petrenko T.,
Danilenko K., Maria R., Babich M., Dolganov A. and
Sokolov A. Investigation of the Neuro-
electrostimulation Mechanisms by Means of the
Functional MRI: Case Study. – Proceedings of the 11th
International Joint Conference on Biomedical
Engineering Systems and Technologies – Volume 3:
NENT, 2018. – ISBN 978-989-758-279-0, pages 319-
324.
Ignatova T., Kolbin V., Scherbak S., Sarana A., Sokolov A.,
Trufanov G., Semibratov N., Ryzhkov A., Efimtsev A.
and Danilov Y. Translingual Neurostimulation in
Treatment of Children with Cerebral Palsy in the Late
Residual Stage. Case Study. In Proceedings of the 11th
International Joint Conference on Biomedical
Engineering Systems and Technologies - Volume 3:
NENT, 2018. ISBN 978-989-758-279-0, pages 332-
337.
Rémi Patriat, Erin K. Molloy, Timothy B. Meier, Gregory
R. Kirk, Veena A. Nair, Mary E. Meyerand, Vivek
Prabhakaran, Rasmus M. Birn. The effect of resting
condition on resting-state fMRI reliability and
consistency: A comparison between resting with eyes
open, closed, and fixated. NeuroImage. – Volume 78. –
2013. Pages 463-473.
NNSNT 2019 - Special Session on Non-invaisive Neuro-stimulation in Neurorehabilitation Tasks
556
