
A Wearable Real-time Human Activity Recognition System using
Biosensors Integrated into a Knee Bandage
Hui Liu and Tanja Schultz
Cognitive Systems Lab, University of Bremen, Germany
Keywords:
Biosensors, Biodevices, Human Activity Recognition, Rehabilitation Technology, Wearable Devices.
Abstract:
This work introduces an innovative wearable real-time Human Activity Recognition (HAR) system. The sys-
tem processes and decodes various biosignals that are captured from biosensors integrated into a knee bandage.
The presented work includes (1) the selection of an appropriate equipment in terms of devices and sensors to
capture human activity-related biosignals in real time, (2) the experimental tuning of system parameters which
balances recognition accuracy with real-time performance, (3) the intuitive visualization of biosignals as well
as n-best recognition results in the graphical user interfaces, and (4) the on-the-air extensions for rapid proto-
typing of applications. The presented system recognizes seven daily activities: sit, stand, stand up, sit down,
walk, turn left and turn right. The amount of activity classes to be recognized can be easily extended by the
”plug-and-play” function. To the best of our knowledge, this is the first work which demonstrates a real-time
HAR system using biosensors integrated into a knee bandage.
1 INTRODUCTION
Arthrosis is the most common joint disease and re-
sults in a perceptible reduction of life quality. Among
all forms of arthroses, gonarthrosis is accounted for
the largest proportion. Apart from the negative impact
on the quality of life for many individuals worldwide,
gonarthrosis leads to significant economic loss due to
surgeries, invalidity, sick leave and early retirement.
Recent studies demonstrate and evaluate the usage of
sensors and technical systems for the purpose of knee
rehabilitation, as for example after ligament injuries
(Yepes et al., 2017) and surgery (Naeemabadi et al.,
2018), to name a few. In an aging society, preven-
tion and early treatment become an increasingly im-
portant part, since joint replacement surgeries carry
secondary risks.
The mainstay of early treatment is an adequate
amount of proper movement. It results in muscular
stabilization and fosters functional maintenance of the
joints. Moreover, movement is fundamental for the
nutrition of both healthy and diseased cartilage. Nev-
ertheless, the knee joint with lesions should not be
overloaded by these movement to not re-activate or
further exacerbate gonarthrosis due to an inflamma-
tion of the joint. This would lead to even more pain
for the patient and worsens the overall conditions.
The overall goal of our work is to technically as-
sist the early treatment of gonarthrosis by discover-
ing the right dose of daily movement, which affects
the functionality of the joint positively while pre-
venting movement-caused overload of the diseased
joint. First steps towards this goal were carried out
by developing a technical system which continuously
tracks the dose of everyday activity movements us-
ing biosensors integrated into a knee bandage. The
results were documented in (Liu and Schultz, 2018),
in which we proposed the framework ASK (Activity
Signals Kit) for biosignal data acquisition, processing
and human activity recognition. The different features
of this framework were introduced in a pilot study
of person-dependent activity recognition based on a
small dataset of human everyday activities.
1.1 Human Activity Recognition
Human activity recognition (HAR) is intensively
studied and a large body of research shows results
of recognizing all kinds of human daily activities, in-
cluding running, sleeping or performing gestures.
For this purpose a large variety of biosignals are
captured by various sensors, e.g. (Mathie et al., 2003)
applied wearable triaxial accelerometers attached to
the waist to distinguish between rest (sit) and active
states (sit-to-stand; stand-to-sit and walk). Five bi-
axial accelerometers were used in (Bao and Intille,
Liu, H. and Schultz, T.
A Wearable Real-time Human Activity Recognition System using Biosensors Integrated into a Knee Bandage.
DOI: 10.5220/0007398800470055
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 47-55
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
47

2004) to recognize daily activities such as walking,
riding escalator and folding laundry. In (Kwapisz
et al., 2010) the authors placed an Android cell phone
with a simple accelerometer into the subjects’ pocket
and discriminated activities like walking, climbing,
sitting, standing and jogging. Furthermore, (Lukow-
icz et al., 2004) combined accelerometers with mi-
crophones to include a simple auditory scene analy-
sis. (De Leonardis et al., 2018) compared the recog-
nition performance of 5 classifiers based on machine
learning (K-Nearest Neighbor, Feedforward Neural
Network, Support Vector Machines, Na
¨
ıve Bayes and
Decision Tree) and analyzed advantages and disad-
vantages of their implementation onto a wearable and
real-time HAR system.
Muscle activities captured by ElectroMyoGraphy
(EMG) is another useful biosignal. It even provides
the option to predict a person’s motion intention prior
to actually moving a joint, like investigated in (Fleis-
cher and Reinicke, 2005) for the purpose of an actu-
ated orthosis. Moreover, some researchers like (Rowe
et al., 2000) and (Sutherland, 2002) applied electrogo-
niometers to study kinematics.
1.2 Goal of this Study
To achieve our overall goal of technical assisting the
early treatment of gonarthrosis using biosensors in-
tegrated into a knee bandage, we envision the con-
tributions to five research and development paths,
i.e. (1) to recognize daily activities based on person-
independent models, (2) to increase the amount of
recognized daily activities, (3) to compare and select
biosensors suitable for integration into a knee ban-
dage and for wearable application, (4) to improve the
activity recognition accuracy by further optimizing
the activity models and system parameters, and (5)
to implement a wearable real-time HAR system for
field studies. This paper focus on our efforts toward
the last item, i.e. the implementation of a wearable
real-time HAR system.
In this study, we used the dataset introduced in
(Liu and Schultz, 2018) as training set. It consists
of biosignals from one male subject captured by two
accelerometers, four EMG sensors and one electro-
goniometer. The data are annotated, time-aligned and
segmented on single-activity level based on a semi-
automatic annotation mechanism using a push-button.
Although, this single-subject dataset is rather small
and by no means representative, we leverage these
data as pilot dataset to showcase the development of
an end-to-end wearable real-time human recognition
system rapidly. To our knowledge, there are no pub-
lished publicly available datasets yet which are suit-
able for real-time HAR using biosensors integrated
into a knee bandage. However, we are quite aware of
the limitations of this dataset, and are currently in the
process of recording a larger dataset covering many
activities from several subjects. First results of these
data recording efforts are presented in section 3.2.
To model human activities we followed the ap-
proach as described in (Rebelo et al., 2013) using
Hidden-Markov-Models (HMM). HMMs are widely
used to a variety of activity recognition tasks, such as
in (Lukowicz et al., 2004) and (Amma et al., 2010).
The former applies it to an assembly and maintenance
task, the latter presents a wearable system that en-
ables 3D handwriting recognition based on HMMs. In
this so-called Airwriting system the users write text
in the air as if they were using an imaginary black-
board, while the handwriting gestures are captured
wirelessly by accelerometers and gyroscopes attached
to the back of the hand.
Based on the training dataset and HMM modeling,
we design and implement a wearable real-time HAR
system using biosensors integrated into a knee ban-
dage, which is connected to an intuitive PC graphical
user interface.
2 EQUIPMENT AND SETUP
2.1 Knee Bandage
We use the Bauerfeind GenuTrain knee bandage
1
as
the wearable carrier of the biosensors (see Figure 1).
It consists of an anatomically contoured knit and an
integral, ring-shaped, functional visco-elastic cush-
ion, which offers active support for stabilization and
relief of the knee.
2.2 Devices
We chose the biosignalsplux Research Kits
2
as
recording device. One PLUX hub
3
records signals
from 8 channels (each up to 16 bits) simultaneously.
We used two hubs for recording the data and con-
nected the hubs via a cable which synchronizes sig-
nals between the hubs at the beginning of each record-
ing. This procedure ensures the synchronization of
sensor data during the entire recording session.
1
www.bauerfeind.de/en/products/supports-orthoses/kne
e-hip-thigh/genutrain.html
2
biosignalsplux.com/researcher
3
store.plux.info/components/263-8-channel-hub-82020
1701.html
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
48

Figure 1: Bauerfeind GenuTrain knee bandage.
2.3 Biosensors and Biosignals
Similar to (Mathie et al., 2003) and (Liu and Schultz,
2018), we used two triaxial accelerometers
4
, four
bipolar EMG sensors
5
and both channels of one biax-
ial electrogoniometer
6
, as they were proved to be ef-
fective and efficient. The sensors were placed onto the
bandage to capture muscles and positions most rele-
vant to activity recognition, as summarized in Table 1.
We used both channels of electrogoniometer to mea-
sure both the frontal and sagital plain since we intend
to recognize rotational movements of the knee joint
for example when walking a curve in the activities
”curve-left” and ”curve-right”.
Table 1: Sensor placement and captured muscles.
Sensor Position / Muscle
Accelerometer (upper) Thigh, proximal ventral
Accelerometer (lower) Shank, distal ventral
EMG1 Musculus vastus medialis
EMG2 Musculus tibialis anterior
EMG3 Musculus biceps femoris
EMG4 Musculus gastrocnemius
Electrogoniometer Knee of the right leg, lateral
The signals of all biosensors were recorded wire-
lessly at different sampling rate. Table 2 shows the
sampling rate of each sensor type.
From table 2 we can see, that accelerometer
and electrogoniometer signal are both slow signals,
4
biosignalsplux.com/acc-accelerometer
5
biosignalsplux.com/emg-electromyography
6
biosignalsplux.com/ang-goniometer
Table 2: Sampling rates of biosensors.
Sensor Sampling rate
Accelerometer 100Hz
Electrogoniometer 100Hz
Electromyography 1000Hz
while the nature of EMG signals require higher sam-
pling rates. Low-sampled channels at 100Hz are up-
sampled to 1000Hz to be synchronized and aligned
with high-sampled channels. Table 3 shows the ar-
rangement of the sensors on Hub1 and Hub2, respec-
tively.
Table 3: Channel layout of PLUX Hub1 (fast), Hub2 (slow).
Channel Sensor
1 Electromyography EMG 1
2 Electromyography EMG 2
3 Electromyography EMG 3
4 Electromyography EMG 4
5 -
6 -
7 -
PLUX Hub1 (fast)
8 -
1 Accelerometer (upper) X-axis
2 Accelerometer (upper) Y-axis
3 Accelerometer (upper) Z-axis
4 Electrogoniometer - sagital plain
5 Accelerometer (lower) X-axis
6 Accelerometer (lower) Y-axis
7 Accelerometer (lower) Z-axis
PLUX Hub2 (slow)
8 Electrogoniometer - frontal plain
2.4 ASK Framework
We continued to program under the framework of
ASK introduced in (Liu and Schultz, 2018) with a
graphical user interface. The ASK PC-software con-
nects and synchronizes several PLUX hubs easily to
subsequently collect data from all hubs simultane-
ously and continuously. In ”Recorder” mode and
semi-automatic ”Annotator” mode, all recorded data
are archived properly with date and time stamps for
further processing. In real-time ”Decoder” mode in-
troduced in section 4, the recorded data are used for
recognition in real-time.
3 EXPERIMENTAL STUDY
An experimental study was performed to compare
two scenarios: the recognition of human activities in
an offline scenario, aka without real-time limitations,
A Wearable Real-time Human Activity Recognition System using Biosensors Integrated into a Knee Bandage
49
and the adaptation of the recognition system to an on-
line scenario with limited processing time, for which
we trade recognition accuracy for decoding speed.
For this purpose we apply one seven-activities dataset
and one eighteen-activities dataset.
3.1 Seven-activities Dataset
We used the seven-activities dataset from (Liu and
Schultz, 2018) that contains four recording sessions
from one male subject as online dataset currently for
the real-time HAR system. In these recordings, seven
activities are organized in two categories, i.e. ”stay-
in-place” and ”move-around”, which results in two
activity lists for the data acquisition prompting pro-
tocol as follows:
• Activity List 1 ”Stay-in-place” (40 repetitions):
sit → sit-to-stand → stand → stand-to-sit.
• Activity List 2 ”Move-around” (25 Repetitions):
walk → curve-left → walk * (turn around) *
walk → curve-right → walk * (turn around).
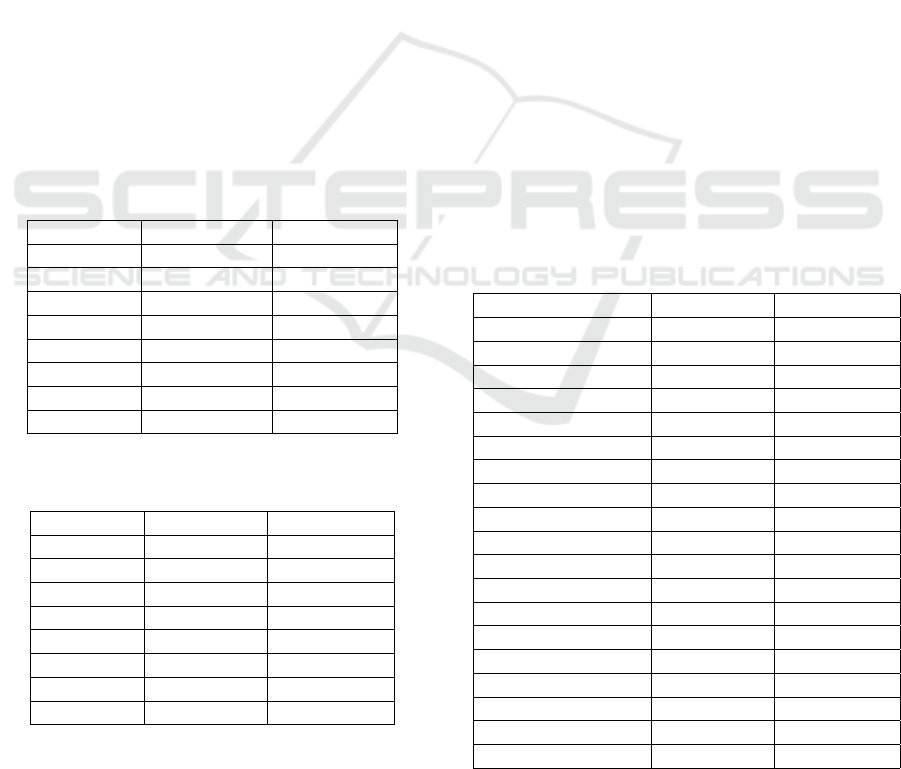
Table 4 and Table 5 gives occurrences, total effec-
tive length, minimum length and maximum length of
these seven activities.
Table 4: Occurrences and total length of the seven activities
in seven-activities dataset.
Activity Occurrences Total length
sit 25 79.92s
stand 23 81.41s
sit-to-stand 24 47.31s
stand-to-sit 23 44.11s
walk 67 172.93s
curve-left 17 61.96s
curve-right 16 66.25s
Total 195 553.87s
Table 5: Minimum and maximum length of the seven activ-
ities in seven-activities dataset.
Activity Min. length Max. length
sit 1.64s 7.78s
stand 1.49s 17.82s
sit-to-stand 1.44s 2.57s
stand-to-sit 1.19s 2.84s
walk 1.35s 4.57s
curve-left 1.81s 13.00s
curve-right 1.56s 18.12s
Global 1.19s 18.12s
We are aware that this dataset is very small and
is neither sufficiently nor necessarily large enough to
establish reliable recognition accuracies for daily ac-
tivities. However, the purpose here was to rapidly
prototype an end-to-end wearable real-time human
recognition system. The classification accuracy of
this dataset resulted in 97% (Liu and Schultz, 2018).
In Section 4.3 we introduce the ”plug-and-play” func-
tion, which allows for easy on-the-fly extensions to
more activity classes and more training data. We col-
lected a larger dataset of eighteen activities (see be-
low), which will become online for real-time recogni-
tion after validation in further work.
3.2 Eighteen-activities Dataset
We continued to record a new larger dataset of eigh-
teen activities from seven male subjects under the
framework of (Liu and Schultz, 2018). Beside the in-
crease of the number of activities, we also extended
the types of sensors and biosignals: Four types of ad-
ditional biosensors were included, i.e. one airborne
microphone, one piezoelectric microphone, two gyro-
scope and one force sensor. The fusion of biosignals
allows the study of sensor comparison and selection
for the purpose of reliable activity recognition. This
eighteen-activities dataset has not been used for real-
time recognition system yet.
Table 6 and Table 7 gives occurrences, total effec-
tive length, minimum length and maximum length of
these eighteen activities.
Table 6: Occurrence and total length of the eighteen activi-
ties in eighteen-activities dataset.
Activity Occurrence Total length
sit 47 123.75s
stand 46 127.70s
sit-to-stand 45 30.94s
stand-to-sit 53 72.90s
stair-up 55 190.45s
stair-down 57 181.96s
walk 220 554.07s
curve-left-step 57 143.09s
curve-left-spin 46 109.15s
curve-right-step 51 67.51s
curve-right-spin 48 41.50s
run 97 151.27s
v-cut-left 53 43.76
v-cut-right 55 61.75s
lateral-shuffle-left 53 97.54s
lateral-shuffle-right 52 90.42s
jump-one-leg 59 61.36s
jump-two-leg 63 63.40s
Total 1157 2212.52s
Most of the activities in this table are self-
explanatory, a few may needs some explanation:
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
50
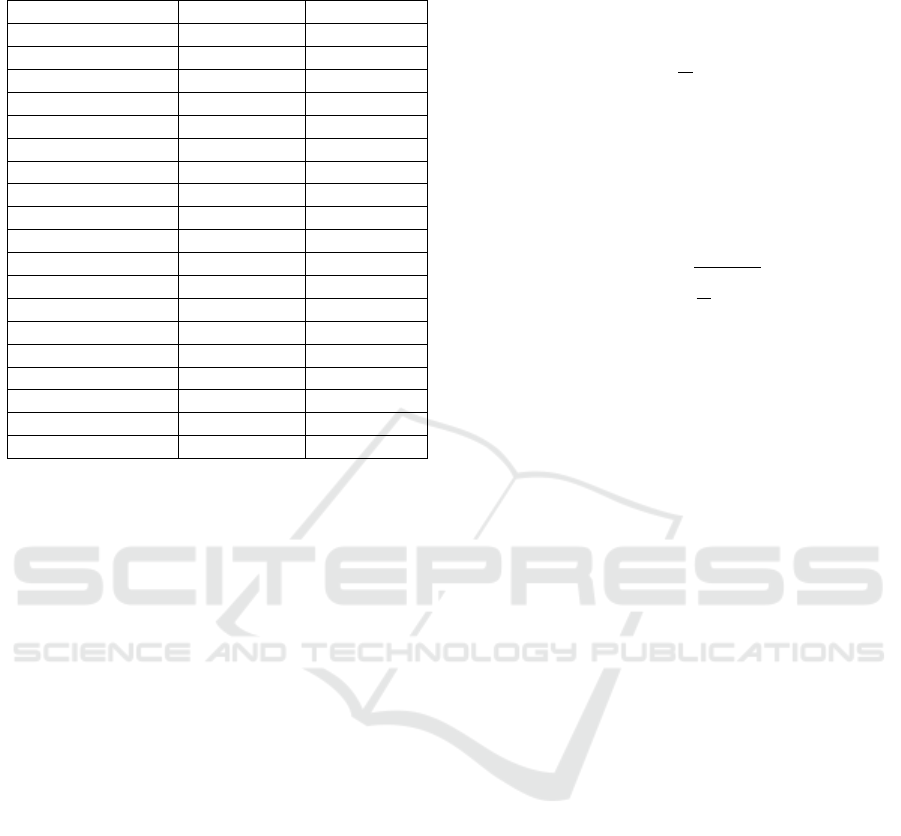
Table 7: Minimum and Maximum length of the eighteen
activities in eighteen-activities dataset.
Activity Min. Length Max. length
sit 0.86s 4.69s
stand 1.36s 4.73s
sit-to-stand 0.15s 1.30s
stand-to-sit 0.56s 3.10s
stair-up 1.59s 4.93s
stair-down 1.37s 4.86s
walk 1.18s 4.78s
curve-left-step 1.10 3.87s
curve-left-spin 1.25s 3.39s
curve-right-step 0.54s 3.19s
curve-right-spin 0.28s 1.88s
run 0.64s 2.74s
v-cut-left 0.29s 2.08s
v-cut-right 0.35s 2.37s
lateral-scuffle-left 0.73s 4.11s
lateral-scuffle-right 0.75s 3.98s
jump-one-leg 0.33s 2.85s
jump-two-leg 0.51s 1.63s
Global 0.15s 4.93s
• Curve-left/right-step vs. curve-left/right-spin:
”step” means that the subject makes a big 90
◦
turn
with several walking steps, while ”spin” suggests
a fast 90
◦
turning of the body like the parade com-
mand ”right turn” or ”right face”.
• Lateral-shuffle-left/right: these two activities
are often used by tennis, soccer and basketball
players. The subject starts with left/right foot
moving left/right laterally and the other foot fol-
lowing, and continues shuffling in the same direc-
tion for the desired amount of time.
• V-cut-left/right: these two activities mean that
the subject changes his/her direction by roughly
90
◦
at jogging speed.
3.3 Feature Extraction and Modeling
For training and decoding the biosignals captured by
the biosensors need to be preprocessed.
First, the biosignals are windowed using a rect-
angular window function with overlapping windows.
Second, a mean normalization is applied to the ac-
celeration and EMG signals to reduce the impact of
Earth acceleration and to set the baseline of the EMG
signals to zero. Then, the EMG signal is rectified, a
widely adopted signal processing method for muscle
activities.
Subsequently, features were extracted for each of
the resulting windows. We denote the number of sam-
ples per window by N and the samples in the window
by (x
1
, ..., x
N
). We adopted the features from (Rebelo
et al., 2013) extracting for each window the average
for the accelerometer and electrogoniometer signal,
defined as:
avg =
1
N
N
∑
n=1
x
n
, (1)
We extracted also average for the four types of
additional signal from the airborne microphone, the
piezoelectric microphone, the gyroscopes and the
force sensor.
For the EMG signal we extracted for each window
the Root Mean Square:
RMS =
s
1
N
N
∑
k=1
x
2
n
(2)
Features of different biosignals can be combined
by early or late fusion, i.e. the feature vectors of sin-
gle biosignal streams are either concatenated to form
one multi-biosignal feature vector (early fusion) or
recognition is performed on single biosignal feature
vectors and the combination is done on decision level
(late fusion). Our framework allows for both fusion
strategies, in this work we rely on early fusion which
showed to outperform the late fusion strategy in the
context of real-time HAR.
3.4 Parameter Tuning and Decoding
Similar to (Liu and Schultz, 2018) we applied our
HMM-based in-house decoder BioKIT to modelling
and recognizing the described activities. Among
others BioKIT supports the training of Gaussian-
Mixture-Models (GMMs) to model the HMM emis-
sion probabilities. Each activity consists of a fixed
number of HMM states, where each state is modeled
by a mixture of Gaussians.
Based on the eighteen-activities dataset and the
automatically generated reference labels for each seg-
ment using the semi-automatic annotation function,
we iteratively optimized the number of HMM states
and Gaussian mixtures per each HMM state.
Figure 2 and Figure 3 demonstrate examples of
tuning different parameters in cross validation experi-
ments with the configuration of 10ms window length,
5ms overlap and 21-dimensional normalized feature
vectors.
Due to the limited data quantity we stopped evalu-
ating the number of gaussians at 10 in order to achieve
reliable results. Similar experiments for tuning dif-
ferent parameters were executed thoroughly and we
arrived at a conclusion that the application of eight
HMM states and ten Gaussians offers the best recog-
nition results.
A Wearable Real-time Human Activity Recognition System using Biosensors Integrated into a Knee Bandage
51
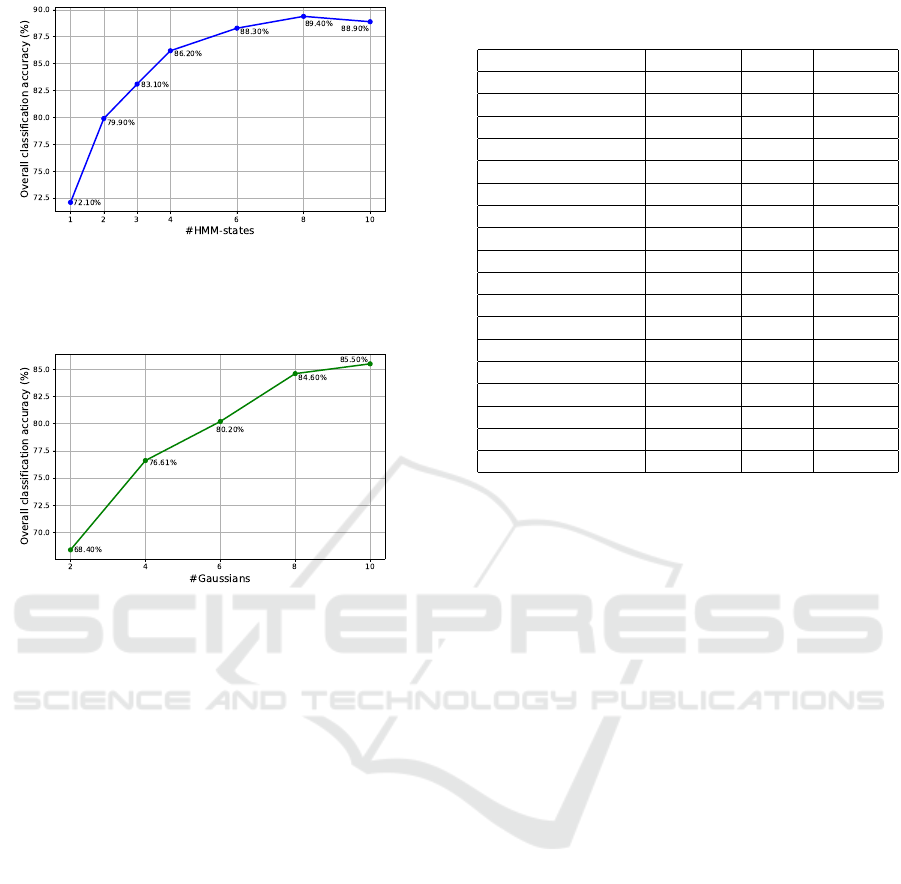
Figure 2: Parameter tuning: number of HMM states. Win-
dow length: 10ms; overlap: 5ms; dimension of normalized
feature vectors: 21; number of Gaussians per each HMM
state: 5.
Figure 3: Parameter tuning: number of Gaussians per each
HMM state. Window length: 10ms; overlap: 5ms; dimen-
sion of normalized feature vectors: 21; number of HMM
states: 2.
Using these current best performing parameters,
the overall person-dependent recognition accuracy
achieves almost 90%. Figure 4 illustrates the recog-
nition results in percentage from one cross validation
experiment in confusion matrix. Table 8 gives the cri-
teria Precision, Recall and F-Score in average of each
activity in cross validation experiments.
As can be seen in Figure 4 and Table 8, ac-
tivities ”jump-one-leg”, ”jump-two-leg”, ”lateral-
shuffle-right” and ”stair-up” were correctly recog-
nized in every experiment.
Recently we applied feature vector stacking fol-
lowed by a linear discrimination analysis and further
improved the results to roughly 95% recognition ac-
curacy. In addition, a merge-split algorithm is planned
to be applied for adaptive determination of the opti-
mal number of gaussians per state. Additional work
to further improve the performance is under way.
Table 8: Criteria Precision, Recall and F-Score in average
of each activity from cross validation experiments.
Activity Precision Recall F-Score
sit 0.85 0.78 0.81
stand 0.90 0.75 0.81
sit-to-stand 0.95 1.00 0.97
stand-to-sit 0.96 1 0.98
stair-up 1.00 1.00 1.00
stair-down 0.96 1.00 0.98
walk 0.92 0.88 0.90
curve-left-step 0.79 0.83 0.80
curve-left-spin 0.71 0.91 0.78
curve-right-step 0.95 0.88 0.91
curve-right-spin 0.80 1.00 0.89
run 0.90 0.86 0.87
v-cut-left 0.66 0.70 0.64
v-cut-right 0.5 0.56 0.50
lateral-shuffle-left 0.96 0.96 0.95
lateral-shuffle-right 1.00 1.00 1.00
jump-one-leg 1.00 1.00 1.00
jump-two-leg 1.00 1.00 1.00
4 WEARABLE REAL-TIME HAR
SYSTEM
We developed a wearable real-time HAR system and
used the above described seven-activities dataset (sec-
tion 3.1) to investigate the end-to-end system perfor-
mance.
4.1 Balance Accuracy versus Speed
From Table 5 we can see, that no activity in this
dataset is shorter than 1.9 seconds. This a-priori infor-
mation let us to decide the window length and window
overlap length and these two lengths were optimized
to balance recognition accuracy versus processing de-
lay. The activities in the seven-activities dataset were
modeled with one HMM state per activity and a longer
window length was chosen. A shorter step-size re-
sults in a shorter delay of the recognition outcomes,
but the interim recognition results may fluctuate due
to temporary search errors. On the other hand, longer
delay due to long step-sizes contradicts the character-
istics of a real-time system, though it generates more
accurate interim recognition results. Based on exper-
iments we chose a balancing setting of 400ms win-
dow length with 200ms window overlap. These val-
ues gave satisfactory recognition results with a barely
noticeable delay within 1 second.
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
52
Figure 4: Confusion matrix of recognition results in percentage from one cross validation experiment.
4.2 Graphical User Interface (GUI) and
Customization
After model training, the system starts recording data
continuously from the biosensors integrated into the
knee bandage. We implemented this new functional-
ity with graphical user interface (GUI) in ASK PC-
software (Liu and Schultz, 2018) to continuously out-
put the recognition results as well as to visualize the
biosignals. The latter feature enables the user to mon-
itor the biosignal recording while the former feature
may serve as input to post-processing steps and to
inform down-stream applications. The recorded data
are displayed serially on the left-hand side of the in-
terface display, and the n-best (usually we set n as 3)
recognition results in terms of activity classes asso-
ciated with the calculated probabilities indicated by
length of bars are shown on the right-hand side of the
interface display (see Figure 5).
The GUI allows to switch biosignals and activi-
ties on and off for the real-time activity recognition.
This way, it is very straight-forward to quickly test the
sensors and system properties during system develop-
ment and evaluation (see Figure 6).
4.3 On-the-Fly Extensions
After we successfully tested our real-time HAR sys-
tem using the seven-activities dataset, we imple-
mented a new function named ”plug-and-play”. This
function can be understood literally: we can load
new activity sensor data on-the-fly, retrain the activity
models, and restart the recognition process automat-
ically with the updated activity models. The ”plug-
and-play” function has several benefits and the fol-
lowing three use cases:
Providing more Training Data for an existing
Activity. In (Liu and Schultz, 2018) we presented a
framework name ASK of data acquisition and semi-
automatic annotation. The real-time HAR system is
also an extension of this framework. Therefore, we
could use the ”annotator mode” (See Figure 6) to
record more data, such as ”stand-to-sit”, and at the
same time generate annotation labels on them (See
Figure 7). These new data will automatically be used
next time for training the real-time HAR system, that
A Wearable Real-time Human Activity Recognition System using Biosensors Integrated into a Knee Bandage
53
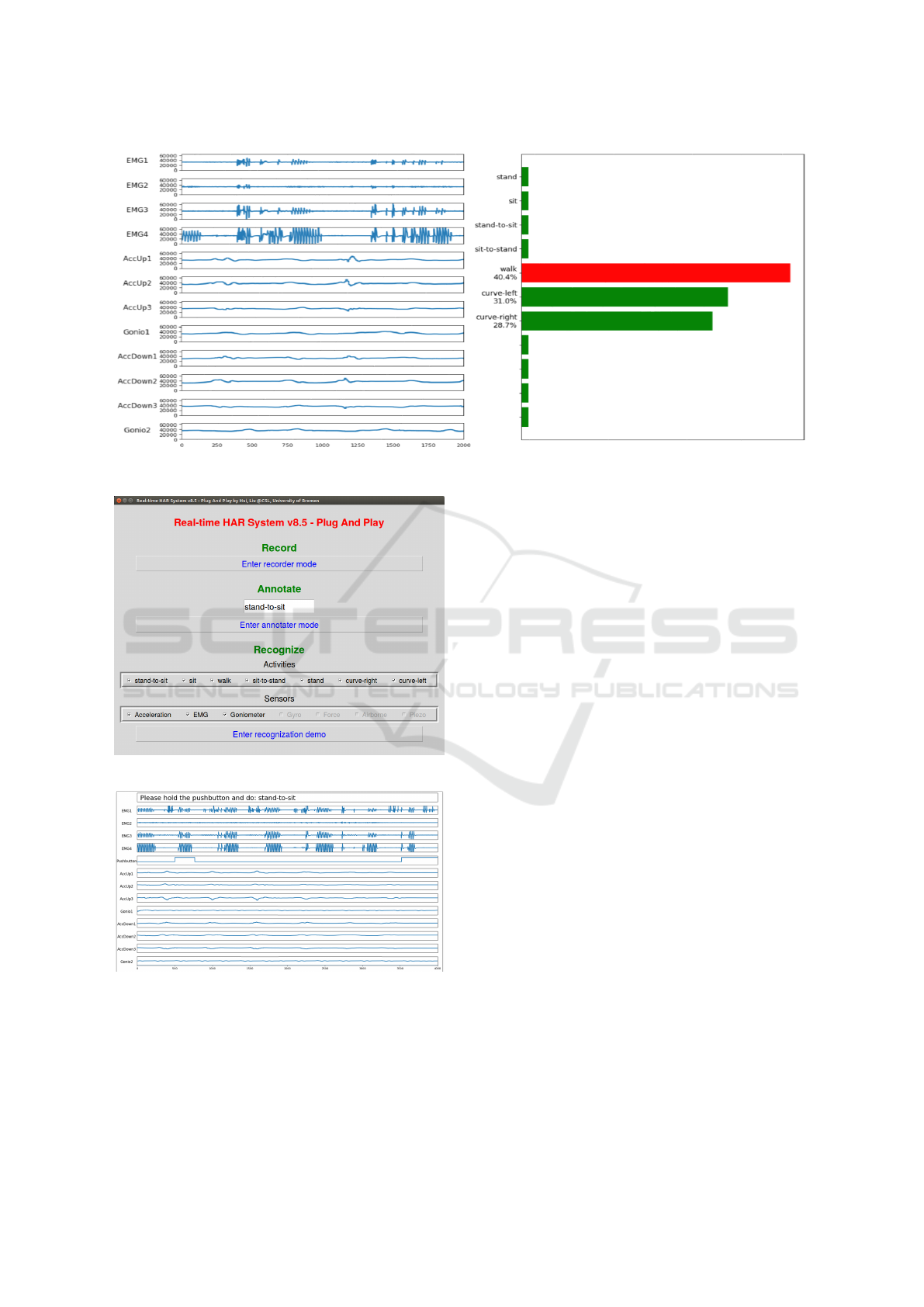
Figure 5: Screenshot: the performance of the real-time HAR system.
Figure 6: Screenshot: sensor and activity selection menu.
Figure 7: Screenshot: ASK software with annotation mode:
the next activity to do is ”stand-to-sit”.
is to say, we ”plug” more data and ”play” with an im-
proved recognition system.
Increase the Activity Classes to be recognized.
Even the recognition of new activities are enabled
most simply. We just need to type a new activity
name, such as ”lie down”, in the text-box, re-run ”an-
notator mode”, record and label a minimum of 12 in-
stances of ”lie down”. These steps take about five
minutes, when finished the real-time HAR system is
started with the new activity ”lie down” already pre-
pared to be recognized.
Enable the Study of Person-independent Real-
time HAR System. Similar to the first usage, we can
record more data for existing activities from different
subjects, the system will then serve automatically as
a person-independent HAR system, provided that we
continue to study proper model configuration and pa-
rameters for person-independent application.
5 CONCLUSIONS
In this paper we brought forward a wearable real-
time Human Activity Recognition (HAR) system us-
ing biosensors integrated into a knee bandage that
capture a variety of biosignals related to human ev-
eryday activities. This HAR system opens up new av-
enues for computer-aided assistive rehabilitation sys-
tems using wearable medical appliances. To the best
of our knowledge, this is the first work which imple-
ments a real-time HAR system using biosensors inte-
grated into a knee bandage.
The paper describes the biosensors and devices
that capture biosignals related to human activities, the
design and implementation of a software platform in-
tegrating methods for modeling, training, and recog-
nition of human activities based on biosignals recog-
nition and a graphical interface to interact with a user.
The final HAR system recognizes human daily activ-
ities in real-time with performances above 90% accu-
BIODEVICES 2019 - 12th International Conference on Biomedical Electronics and Devices
54

racy and a barely noticeable delay. It further provides
a ”plug-and-play” function for on-the-fly extensions
such as enabling the recognition of unseen activities.
Further work will be devoted to improve the recogni-
tion performance in a person-independent setting on a
larger set of activities, and to integrate the HAR out-
put into an assistive rehabilitation system for people
suffering gonarthrosis.
REFERENCES
Amma, C., Gehrig, D., and Schultz, T. (2010). Airwrit-
ing recognition using wearable motion sensors. In
First Augmented Human International Conference,
page 10. ACM.
Bao, L. and Intille, S. S. (2004). Activity recognition from
user-annotated acceleration data. In Pervasive com-
puting, pages 1–17. Springer.
De Leonardis, G., Rosati, S., Balestra, G., Agostini, V.,
Panero, E., Gastaldi, L., and Knaflitz, M. (2018). Hu-
man activity recognition by wearable sensors: Com-
parison of different classifiers for real-time applica-
tions. In 2018 IEEE International Symposium on
Medical Measurements and Applications (MeMeA),
pages 1–6. IEEE.
Fleischer, C. and Reinicke, C. (2005). Predicting the in-
tended motion with emg signals for an exoskeleton
orthosis controller. In 2005 IEEE/RSJ International
Conference on Intelligent Robots and Systems (IROS
2005), pages 2029–2034.
Kwapisz, J. R., Weiss, G. M., and Moore, S. A. (2010).
Activity recognition using cell phone accelerometers.
In Proceedings of the Fourth International Workshop
on Knowledge Discovery from Sensor Data, pages 10–
18.
Liu, H. and Schultz, T. (2018). Ask: A framework for data
acquisition and activity recognition. In 11th Interna-
tional Conference on Bio-inspired Systems and Signal
Processing, Madeira, Portugal, pages 262–268.
Lukowicz, P., Ward, J. A., Junker, H., St
¨
ager, M., Tr
¨
oster,
G., Atrash, A., and Starner, T. (2004). Recognizing
workshop activity using body worn microphones and
accelerometers. In In Pervasive Computing, pages 18–
32.
Mathie, M., Coster, A., Lovell, N., and Celler, B. (2003).
Detection of daily physical activities using a triaxial
accelerometer. In Medical and Biological Engineer-
ing and Computing. 41(3):296—301.
Naeemabadi, M. R., Dinesen, B., Andersen, O. K., Najafi,
S., and Hansen, J. (2018). Evaluating accuracy and us-
ability of microsoft kinect sensors and wearable sen-
sor for tele knee rehabilitation after knee operation.
In 11th International Conference on Biomedical Elec-
tronics and Devices, Biodevices 2018.
Rebelo, D., Amma, C., Gamboa, H., and Schultz, T. (2013).
Activity recognition for an intelligent knee orthosis.
In 6th International Conference on Bio-inspired Sys-
tems and Signal Processing, pages 368–371. BIOSIG-
NALS 2013.
Rowe, P., Myles, C., Walker, C., and Nutton, R. (2000).
Knee joint kinematics in gait and other functional ac-
tivities measured using exible electrogoniometry: how
much knee motion is sucient for normal daily life?
Gait & posture, 12(2):143—-155.
Sutherland, D. H. (2002). The evolution of clinical
gait analysis: Part ii kinematics. Gait & Posture,
16(2):159–179.
Yepes, J. C., Saldarriaga, A., V
´
elez, J. M., P
´
erez, V. Z.,
and Betancur, M. J. (2017). A hardware-in-the-loop
simulation study of a mechatronic system for anterior
cruciate ligament injuries rehabilitation. In BIODE-
VICES, pages 69–80.
A Wearable Real-time Human Activity Recognition System using Biosensors Integrated into a Knee Bandage
55
