
A Framework for Performance Management of Clinical Practice
Pilar Mata
1
, Craig Kuziemsky
2
and Liam Peyton
1
1
Faculty of Engineering, University of Ottawa, Ottawa, Canada
2
Telfer School of Management, University of Ottawa, Ottawa, Canada
Keywords: Evaluation and Use of Healthcare IT, Healthcare, Performance Management, Mobile Technologies for
Healthcare Applications, Software Systems in Medicine, Design and Development of Methodologies for
Healthcare IT.
Abstract: In this paper, we present a framework for performance management of clinical practice. The framework
defines a performance management participation model, which identifies the processes that need to be
managed at the micro, meso, and macro levels for a clinical practice, and which identifies the key actors and
tasks relevant to performance management. It defines a performance measurement model, which maps goals
and indicators to the performance management participation model. In addition, it includes a methodology
for implementation and evaluation of tools that can be integrated into care processes to support the data
collection and report notification tasks identified in the performance management participation model. We
revisit the case study of implementing a resident practice profile app, in light of the proposed framework, to
support performance management of a family health practice. We demonstrate how the framework is useful
for explaining why the use of the app was abandoned after two years of its introduction and, therefore, how
the framework is an improvement to our previous methodology for development of performance
management apps for clinical practice.
1 INTRODUCTION
Performance management frameworks are
implemented in healthcare organizations in response
to an increasing need for accountability and
transparency and to stimulate improvements in
quality of care (Marshall et al., 2018). Adoption of
performance management in the healthcare industry
is slower compared to other industries (Crema and
Verbano, 2013). One key reason for this is the
complexity of the healthcare system compared to
other domains. Healthcare delivery encompasses
multiple stakeholder groups (patients, families,
health plans, practitioners, communities, regulators,
etc.) and actors (Voelker et al., 2001; Lipsitz, 2012).
Synchronization of data, people, processes, and
technology is needed to achieve seamless integration
in support of performance management across
patient and healthcare providers routines (Avison
and Young, 2007; Benson, 2012).
We propose a performance management
framework for clinical practice that provides:
a. A performance management participation model,
which identifies the processes that need to be
managed at the micro, meso, and macro levels for a
clinical practice, and which identifies the key actors
and tasks relevant to performance management.
b. A performance measurement model which maps
goals and indicators to the performance management
participation model.
c. A methodology for implementation and
evaluation of tools that can be integrated into care
processes to support the data collection and report
notification tasks identified in the performance
management participation model.
The motivation for this framework, grew out of
previous work to create a development methodology
for performance monitoring apps (Mata et al., 2015).
The methodology was successful for quickly
developing user-friendly apps for collecting and
reporting on performance monitoring data. However,
organizational adoption was limited because it did
not provide a broad enough perspective on the
context in which the apps would be used as part of a
complete performance management system for an
entire clinical practice. We define a clinical practice
as a collection of processes that, together, support a
particular type of healthcare for a particular
286
Mata, P., Kuziemsky, C. and Peyton, L.
A Framework for Performance Management of Clinical Practice.
DOI: 10.5220/0007375902860293
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 286-293
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

community of patients. This work focuses on our
main research question of how to effectively and
efficiently guide the implementation and adoption of
performance management systems for a clinical
practice, considering the complexity of healthcare
systems. We revisit a case study of implementing a
resident practice profile app to support performance
management of a family health practice in order to
demonstrate the usefulness of our proposed
performance management framework.
2 BACKGROUND
Performance management involves systematic
planning, execution, monitoring and evaluation of
goals in order to improve business effectiveness
(Dresner, 2008).
(Marshall et al., 2018) review implementations
of healthcare quality report cards (also called report
cards or, performance cards) in the United States and
United Kingdom. Their work shows that although
reporting is perceived as a key factor for improving
accountability and quality in the health care system,
often there are challenges in engaging the
stakeholders on these initiatives.
The Sunnybrook Hospital in Ontario, published
its Balance Scorecard & Patient Safety Indicators in
June 2018, with the goal to increase transparency for
the community (Sunnybrook, 2018). The Balanced
Scorecard includes the dimensions: quality of patient
care, research and education, and sustainability and
accountability.
Despite the complexity of
implementing performance management systems
like Balanced Scorecard in healthcare organizations,
research shows some progress in this area.
Achieving a successful implementation of it requires
communication, commitment and, support from all
stakeholders and at all the different organizational
levels (Voelker et al., 2001).
While information technology is critical for
performance management in healthcare,
interoperability is an ongoing challenge for
healthcare information systems (HIS) (Kuziemsky
and Peyton, 2016). However, HIS to support
performance management must go beyond a single
technological solution. The complexity of healthcare
system means a single vendor cannot have the best
solution for all functions, even within a single
hospital (Gaynor et al., 2014).
There are different types of interoperability and
these can be grouped, at a high level, into three main
categories: technical, semantic and processes
interoperability (Benson, 2012).
Technical interoperability is defined as the
ability to move data from system A to system B
regardless of the meaning of what is being
exchanged (Benson, 2012). Technical
interoperability is achieved through mHealth and
eEhealth. “mHealth” is defined as the use of mobile
technologies in the healthcare industry to support
public and clinical care (Kahn et al., 2010), while
“eHealth” involves the use of any type of electronic
devices, e.g desktops, in the provision of health care
(Dicianno et al., 2015).
Semantic interoperability is defined as the ability
of sender and receiver to understand data without
ambiguity. It refers to the ability of two computer
systems to be able to interpret and understand data
that is exchanged (Benson, 2012). Standards
developed to support semantic interoperability
include HL7 and terminology models such as
Systematic Nomenclature of Medicine-Clinical
Terms (SNOMED-CT) and Logical Observation
Identifiers Names and Codes (LOINC) (Dixon et al.,
2014).
Process interoperability refers to the coordination
of business and work processes and common
understanding between human beings across a
network (Benson, 2012). The latter includes one of
the key dimensions in healthcare delivery - the
interpersonal nature of care delivery (Avison and
Young, 2007). Encounters between care providers
and patients (e.g doctors and patients, patient and
nurses, patient and therapists, nurses and doctors) to
discuss diagnosis, treatment options, treatment
progress, etc. is an important dimension to consider
in healthcare interoperability; however, the process
interoperability is often forgotten when designing
systems to support healthcare delivery.
Clinical performance management can be
approached in two ways. First, performance can be
seen as the outcome of a process. An example of
performance monitoring in this case would be
monitoring mortality rates. Second, clinical
performance can be seen at the process level, which
in the end, impacts outcome (Goddard et al., 2002).
An example of performance monitoring of a clinical
process would be monitoring a patient from
diagnosis to end of treatment to gain insights of
patient status and progress against goals.
Performance monitoring of clinical process can
facilitate timely actions during the treatment of the
condition.
Information, process and personnel issues can
contribute to gaps in data support for decision-
related processes in Canadian Healthcare
organization (Foshay and Kuziemsky, 2014). To
A Framework for Performance Management of Clinical Practice
287
address these issues organizations should employ a
process framework to define information needs
when implementing performance management
systems. Further, the impact of data on clinical
practice needs to be analysed in different user
contexts (Kuziemsky et al., 2014). A process
framework should distinguish between the micro
level (direct patient care), the meso level
(management and evaluation of care providers), and
the macro level (public health and regulatory
processes).
3 FRAMEWORK
In this section we describe the components of our
proposed framework for performance management
of a clinical practice (Figure 1). Research methods
used for the development of the framework include:
1) literature review 2) Gap analysis of existing
frameworks (Perlin et al., 2004; Parsons et al., 2012;
Voelker et al., 2001; Sullivan et al., 201; Potter et al.
2011) 3) Use of Design Science Method (Peffers et
al., 2007) for defining, designing, and building the
conceptual framework. The developed framework is
comprised of a performance management
participation model, a performance measurement
model, and a methodology for implementation and
evaluation of supporting tools.
Figure 1: Framework for Performance Management of
Clinical Practice.
In the 'Performance Management Participation
Model' we identify which tasks are performed by
which actors in the context of a process, and then
model processes that need to be monitored for
performance management. This is done at a
conceptual level and includes identifying the actors,
tasks and task types for each process. The
participation model is intended to facilitate
discussion among stakeholders and achievement of a
common vision of the process in terms of
performance management. The 'Performance
Measurement Model' is used to define which goals
and indicators will be used for performance
management of each process, based on what report
notifications the actors need and for which processes
the reports are needed. Relationships between the
'Performance Management Participation Model' and
the 'Performance Measurement Model' imply
iterative cycles for the development of conceptual
models - mapping processes to goals, tasks to data
collection, data collection to indicators, indicators to
report notifications and report notifications to tasks.
Finally, tools used to implement performance
management of a clinical practice are identified and
mapped to data collection and report notification
tasks that use the tools to populate the performance
management model. Relationships are defined for
the processes at all organizational levels to ensure all
actors receive the appropriate information to
perform their tasks. Once data needs are clear (from
collecting and reporting), the next step in the
framework is a systematic approach to implementing
and evaluating tools that support the set of tasks
defined in the performance management
participation model. We update and integrate a
methodology for development of performance
monitoring apps (Mata et al., 2015).
4 CASE STUDY OF A RESIDENT
PRACTICE PROFILE FOR
FAMILY HEALTH
Resident Practice Profile (RPP) is a tool for tracking
patient encounters seen by medical residents in
Family Health, to ensure they gain competency
across a broad range of family health diagnoses, and
a diverse range of patients (based on age, gender,
and social circumstance). Residents log data for
patient encounters and the data is used to show
residents where residents are spending their time.
RPP was successfully developed as a user-friendly
app using a development methodology for
performance monitoring apps (Mata et al., 2015).
However, two years after its introduction, it was no
longer used by the organization.
In this case study, we take a broader view of
performance management for the clinical practice as
a whole in order to understand why RPP did not
succeed. Since RPP was developed previous to the
HEALTHINF 2019 - 12th International Conference on Health Informatics
288
proposed framework, we evaluate the app, using the
framework, to demonstrate how the framework can
be used to validate any existing tool within a
performance management system and how the
framework is an improvement to our previous
methodology (Mata et al., 2015) for development of
performance management apps for clinical practice.
In the following sections, based on our framework,
we evaluate the use of RPP to support performance
management of medical residents in a family health
practice.
4.1 Evaluation of RPP using the
Framework
4.1.1 Participation Model
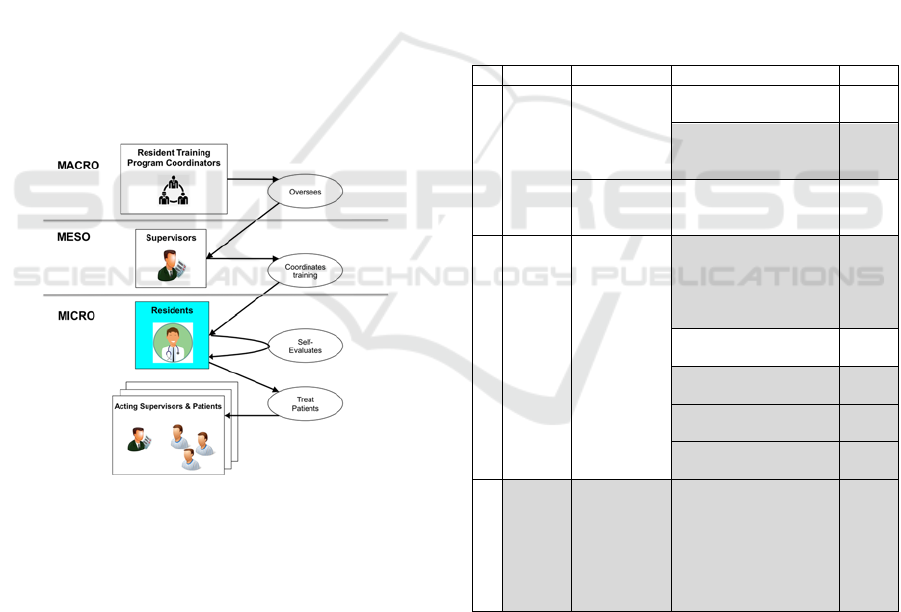
In this section, we identify processes, actors, tasks
and task types relevant for performance management
of medical residents in a family health practice.
Figure 2 depicts actors, and processes for
performance management of residents at the
different organizational levels (macro, meso, and
micro).
Figure 2: Performance management of training of family
medicine residents – Actors and processes.
At the macro level, Residents Training Program
Coordinators oversee supervisors who coordinate
training for the family health practice. They must
ensure the program adheres to guidelines specified
by The College of Family Physicians of Canada.
At the meso level, supervisors coordinate
training tasks, assigning residents to various clinical
settings and providing feedback on training to ensure
residents are exposed to a variety of clinical
conditions and demographics that lead to successful
attainment of required competencies outlined in the
program curriculum.
At the micro level, residents work under the
supervision of acting supervisors at each clinical
location. Residents are responsible for keeping a log
of conditions seen during practice in order to
demonstrate their competence in all program
requirements - clinical domains and demographic
groups (Chamney et al., 2014). Residents are also
responsible for sharing logs with their supervisors
and flagging visits they want to discuss with their
supervisors to receive feedback and develop a
learning plan, if need be. Also, they are responsible
for proactively identifying and completing self-
learning opportunities. Supervisors use the
information provided by residents for guiding
training and correcting any deficiencies in practice,
e.g. assignment of residents to specific locations
where they can see more cases of a given clinical
condition, creating a learning plan, etc.
Table 1: RPP Performance Management Participation
Model.
Actors Process Tas
k
Type/Task Tool
Micro
Residents
Treat Patients
Data Collection: Log
every patient visi
t
RPP
Data Collection: Record
selected Patient field
note
Field
Note
Self-Evaluate
Report Notification:
Self-Evaluation with
RPP reports
RPP
Meso
Supervisors
Coordinates
Training
Data Collection:
Log Direct
observation/Complete
examination/procedure
or delivery o
b
served
Field
Note
Report Notification:
Review RPP Reports
RPP
Report Notification:
Review Field Note
Field
Note
Report Notification:
Provide Feedbac
k
Field
Note
Data Collection: Assess
level of competency
Field
Note
Macro
Program
Coordinators
Oversees
Report Notification:
Review compliance of
training program against
standards
Field
Note
In Table 1 we summarize processes, actors,
tasks, task types and tools by organizational levels
for RPP. Actors, tasks and task types shaded in grey
represent those that are not supported by the
implementation of RPP. Tasks in bold indicate those
that should have been supported by RPP when it was
implemented, but were not. The RPP app was
designed to be used by residents. As such, it was
A Framework for Performance Management of Clinical Practice
289
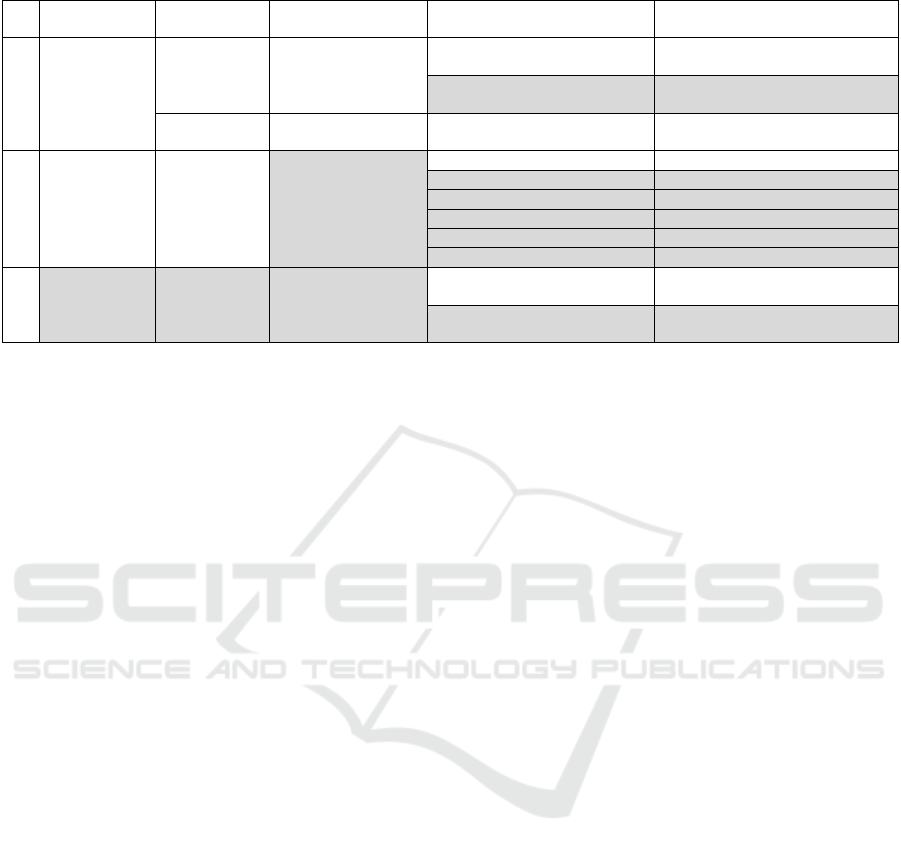
Table 2: RPP Performance Management Participation/Measurement Model.
Actors Process Goals Indicators Task
Micro
Residents
Treat Patients
Ensure full
competency across
clinical domains and
population types
Total Visits Log every patient visit
Completed field notes and sent to
supervisors
Record selected patient field note
Self-Evaluates Close gaps in learning
Total visits flagged for
self-learning activities
Self-Evaluation with RPP reports
Meso
Supervisors
Coordinates
Training
Ensure graduated
residents is fully
competent
Total visits Reviews RPP reports
Field Notes completed Review Field Note
Field Notes completed Provide feedbac
k
Field notes signed off Assess level of competency
Total direct observations Assess level of competency
Level of competency achieved Asses level of competency
Macro
Program
Coordinators
Oversees
Ensure compliance of
program to standards
Total visits
Review compliance of training
program against standards
Average success rate: field notes
signed off/total field notes
Review compliance of training
program against standards
good for self-evaluation. However, the data was also
relevant to the supervisors of the residents. In the
original case study, it was assumed that supervisors
would review with the resident what patients they
were seeing, but procedures were not put in place to
do ensure this was done, nor was there any
mechanism for notifying and providing supervisors
with RPP reports relevant to a resident they were
supervising.
4.1.2 Measurement Model
The next component of the proposed framework
involves the development of a performance
measurement model. This includes definition of
goals to gauge progress and indicators for report
notifications. Table 2 summarizes the performance
measurement model for RPP. Goals and indicators
are grouped by organizational level. Goals and
indicators shaded in grey represent those that are not
supported by the implementation of RPP. Goals and
indicators in bold indicate those that should have
been supported by RPP when it was implemented,
but were not.
The most important aspect of the performance
measurement model in this case study is the clinical
practice as it relates to the training of medical
residents. The main questions to answer are; which
goals we need to measure, what report notifications
are needed for supporting and monitoring these
goals, which tasks are needed to collect data, and,
therefore, what data model (dimensions and
indicators) needs to be implemented.
With respect to the RPP tool, the main indicators
supported were total visits and total visits flagged
for self-learning activities. This included the ability
to analyse based on the age, gender and social
circumstances of patients. RPP was designed to
support actors, tasks, and goals at the micro level.
However, as is clear in Table 2, for effective
integration into a system of performance
management, RPP also needed to provide support
for actors at the meso and even the macro level.
Because RPP was not integrated at this level, its use
was not reinforced by supervisors. Therefore, there
was less interest from residents, and it was
eventually phased out of use in the family health
practice.
4.1.3 Methodology
The original methodology was intended for
development of a stand-alone app for performance
monitoring. We have updated the methodology, to
integrate it into a framework for performance
management across an entire clinical practice, with
the focus on the implementation and evaluation of a
set of tools to support data collection and reporting
tasks at all organizational levels (micro, meso,
macro).
Figure 3 shows the updated methodology, with
changes highlighted in Bold. This included defining
clearly who needed to not only use the app for data
collection, but also who needed to see reports
created from the data collected. Adoption criteria
were extended beyond ease of use, to also include an
understanding of the full context for performance
management in which the app would be used.
New components highlighted in red were also
added to the methodology. This included selecting
which tools were available and could be used, and
carefully mapping all tasks (both data collection and
report notification) that needed to be supported by
the tool. The new methodology provides better gui-
HEALTHINF 2019 - 12th International Conference on Health Informatics
290
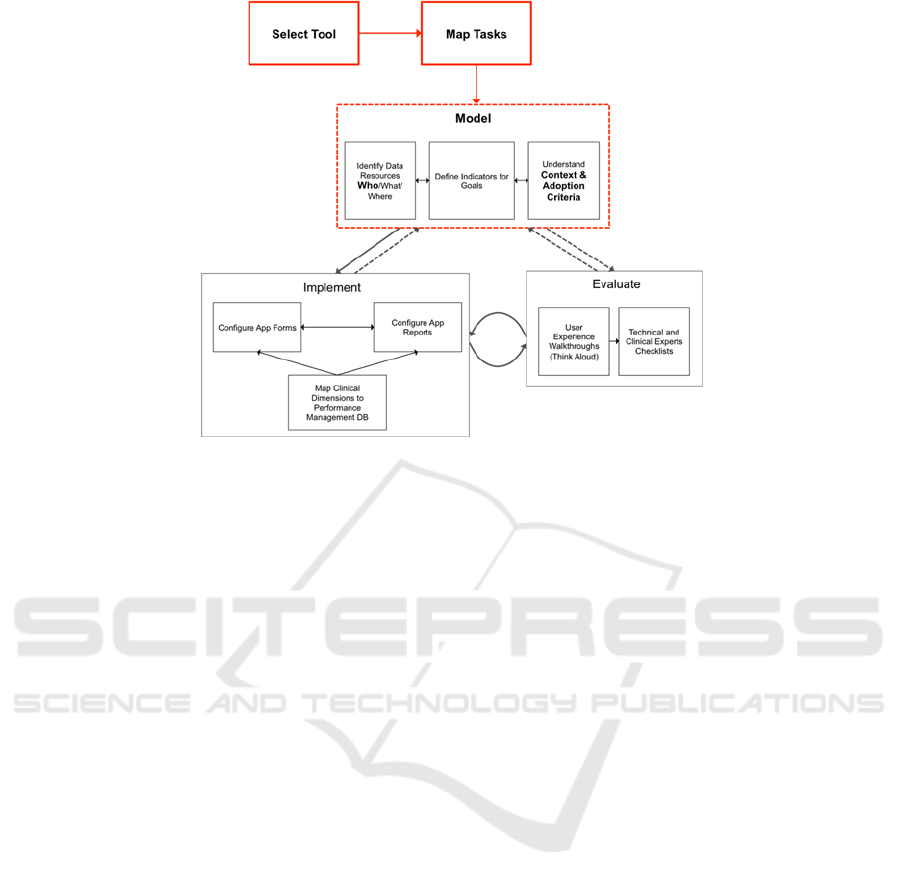
Figure 3: Updated Methodology for Implementation and Evaluation of Tool Support.
dance for understanding who uses the data (actors
that receive report notifications), the context in
which data is used, and what drives adoption
criteria.
4.1.4 Results
After analysing the design of RPP in light of the
framework, we identified that the main focus for the
development of RPP was on monitoring the process
at the micro level by providing residents with a
supporting tool for guiding self-learning activities.
RPP was also useful for providing residents and
program coordinators information about number of
clinical conditions seen by demographic groups as
well as procedures performed. However, the tool
was not used to support supervisors in their task of
providing feedback to residents, designing a plan to
correct any deficiencies identified during training or
completing a formal evaluation of training.
We can say that with our framework, a more
complete view of RPP is given within the context of
supporting performance management of the family
health practice across all levels (micro, meso, and
macro). In the original case study, RPP was
implemented and adopted with some success at the
resident level (micro). Residents found RPP reports
useful for self-assessment and for guiding self-
learning activities.However, the performance
management participation model clearly highlights
the need to provide RPP reports to supervisors for
the tasks of providing feedback to residents or
creating learning plans to address identified gaps in
practice. Report notifications were not implemented
and review of reports was exclusively driven by the
self- motivation of participants of the study.
The performance measurement model also
clearly indicates that total visits, especially as
broken down to support training related to diversity
of patients (age, gender, social circumstance) is
relevant to coordinators at the macro level.
Finally, the updates to the methodology for
implementing and evaluating tools would have more
clearly established the adoption criteria for
evaluating tools in the context of selecting what
tools would be mapped to what tasks for the overall
success of performance management in the family
health practice.
This is the essential factor that explains why RPP
was abandoned even though it was an easy-to-use
app. The fact that the app complied with user
requirements at the individual level (micro level)
was not a sufficient condition to drive adoption of
RPP as a tool for supporting key actors and tasks
relevant to performance management at the meso
and macro levels. The adoption of RPP at the micro
level was exclusively driven by the motivational
aspect of residents who saw value in using the app
for self-assessment of their practice and for guiding
self-learning activities.
The use case provides evidence on the
importance to approach performance management
from a broad enough organizational perspective and
within the context in which the apps would be used,
in order to address information needs of stakeholders
and ensure adoption of the proposed system. Results
A Framework for Performance Management of Clinical Practice
291

of the case study will be used to cross-validate the
usefulness of the framework with clinical experts,
other researchers and for different clinical practices.
5 CONCLUSIONS
In this paper we demonstrate the importance of
having a clear understanding of areas that need to be
addressed for effective implementation of tools and
apps that support performance management of a
clinical practice. The findings we presented here
suggest that defining processes, actors, and
performance management tasks across all
organizational levels (micro, meso, and macro) are
key to ensure adoption of performance management
systems for a clinical practice. Our framework
provides a systematic approach to gain consensus
about who needs to manage performance, what
needs to be monitored, how performance will be
reported to key actors, and how to evaluate tools to
systematically support performance management of
a clinical practice.
One limitation of this work is that we used our
framework to retrospectively evaluate the
deployment of one stand-alone app. Although it let
us highlight missing areas for deployment of the app
and why the app was only adopted, with some
success, at the micro level, more research needs to
be done to confirm the framework can also be used
for guiding the design and implementation of a
performance management system for an entire
clinical practice.
ACKNOWLEDGEMENTS
This research was supported by NSERC Discovery
and CREATE initiatives and Ontario Graduate
Scholarship funding.
REFERENCES
Avison, D. and Young, T. (2007) ‘Time to rethink health
care and ICT?’, Commun. ACM, 50(6), pp. 69–74.
Benson, T. (2012) ‘Principles of health interoperability
HL7 and SNOMED. Chapter 2: Why interoperability
is hard.’, in. Springer Science & Business Media
(Principles of health interoperability HL7 and
SNOMED.).
Chamney, A., Mata, P., Viner, G., Archibald, D. and
Peyton, L. (2014) ‘Development of a Resident Practice
Profile in a Business Intelligence Application
Framework’, Procedia Computer Science, 37(0), pp.
266–273.
Crema, M. and Verbano, C. (2013) ‘Future developments
in health care performance management’, Journal of
Multidisciplinary Healthcare, 6, pp. 415–421.
Dicianno, B. E., Parmanto, B., Fairman, A. D., Crytzer, T.
M., Daihua, X. Y., Pramana, G., Coughenour, D. and
Petrazzi, A. A. (2015) ‘Perspectives on the evolution
of mobile (mHealth) technologies and application to
rehabilitation’, Physical therapy. American Physical
Therapy Association, 95(3), pp. 397–405.
Dixon, B. E., Vreeman, D. J. and Grannis, S. J. (2014)
‘The long road to semantic interoperability in support
of public health: experiences from two states’, Journal
of biomedical informatics. Elsevier, 49, pp. 3–8.
Dresner, H. (2008) The performance management
revolution: Business results through insight and
action. John Wiley & Sons.
Foshay, N. and Kuziemsky, C. (2014) ‘Towards an
implementation framework for business intelligence in
healthcare’, International Journal of Information
Management, 34(1), pp. 20–27.
Gaynor, M., Yu, F., Andrus, C. H., Bradner, S. and Rawn,
J. (2014) ‘A general framework for interoperability
with applications to healthcare’, Health Policy and
Technology. Elsevier, 3(1), pp. 3–12.
Goddard, M., Davies, H. T., Dawson, D., Mannion, R. and
McInnes, F. (2002) ‘Clinical performance
measurement: part 1--getting the best out of it’,
Journal of the Royal Society of Medicine. The Royal
Society of Medicine, 95(10), pp. 508–510.
Kahn, J. G., Yang, J. S. and Kahn, J. S. (2010) ‘“Mobile”
health needs and opportunities in developing
countries’, Health Affairs. Health Affairs, 29(2), pp.
254–261.
Kuziemsky, C.E. and Peyton, L., 2016 (2016) ‘A
framework for understanding process interoperability
and health information technology’, Health Policy and
Technology, 5(2), pp. 196–203.
Kuziemsky, C. E., Monkman, H., Petersen, C., Weber, J.,
Borycki, E. M., Adams, S. and Collins, S. (2014) ‘Big
Data in Healthcare - Defining the Digital Persona
through User Contexts from the Micro to the Macro.
Contribution of the IMIA Organizational and Social
Issues WG’, Yearbook of medical informatics, 9(1),
pp. 82–89.
Lipsitz, L. A. (2012) ‘Understanding Health Care as a
Complex System: The Foundation for Unintended
Consequences’, JAMA, 308(3), pp. 243–244.
Marshall, M. N., Shekelle, P. G., Davies, H. T. O. and
Smith, P. C. (2018) ‘Public Reporting On Quality In
The United States And The United Kingdom In both
countries the imperatives of accountability and quality
improvement make the wider development and
implementation of report cards inevitable’. Available
at: www.ncqa.org. (Accessed: 22 July 2018).
Mata, P., Chamney, A., Viner, G., Archibald, D. and
Peyton, L. (2015) ‘A development framework for
mobile healthcare monitoring apps’, Personal and
Ubiquitous Computing. Springer London, 19(3–4), pp.
HEALTHINF 2019 - 12th International Conference on Health Informatics
292

623–633.
Parsons, A., Mccullough, C., Wang, J. and Shih, S. (2012)
‘Validity of electronic health record-derived quality
measurement for performance monitoring’, J Am Med
Inform Assoc, 19, pp. 604–609.
Peffers, K., Tuunanen, T., Rothenberger, M. A. and
Chatterjee, S. (2007) ‘A Design Science Research
Methodology for Information Systems Research’,
Journal of Management Information Systems, 24(3),
pp. 45–77.
Perlin, J. B., Kolodner, R. M. and Roswell, R. H. (2004)
‘The Veterans Health Administration: quality, value,
accountability, and information as transforming
strategies for patient-centered care’, The American
journal of managed care, 10(11 Pt 2), p. 828.
Potter, K., Fulk, G. D., Salem, Y. and Sullivan, J. (2011)
‘Outcome Measures in Neurological Physical Therapy
Practice: Part I. Making Sound Decisions’, Journal of
Neurologic Physical Therapy, 35(2), pp. 57–64.
Sullivan, J. E., Andrews, A. W., Lanzino, D., Peron, A.
and Potter, K. A. (2011) ‘Outcome Measures in
Neurological Physical Therapy Practice: Part II. A
Patient-Centered Process’, Journal of Neurologic
Physical Therapy, 35(2), pp. 65–74.
Sunnybrook, H. S. C. (2018) Sunnybrook’s Strategic
Balanced Scorecard. Available at:
https://sunnybrook.ca/uploads/1/welcome/strategy/bal
anced_scorecard_june-2018-release.pdf (Accessed: 28
July 2018).
Voelker, K. E., Rakich, J. S. and French, G. R. (2001)
‘The Balanced Scorecard in Healthcare Organizations:
A Performance Measurement and Strategic Planning
Methodology’, Hospital Topics, 79(3), pp. 13–24.
A Framework for Performance Management of Clinical Practice
293
