
Cesarean Section Avoidance based on Obstetric Hemorrhagic Risk:
A Decision Support System
Juliano S. Gaspar, Marcelo R. S. Junior, Regina A. L. P. Lopes and Zilma S. N. Reis
Faculdade de Medicina da Universidade Federal de Minas Gerais, Belo Horizonte, Brazil
Keywords: Obstetric Hemorrhage, Robson Classification, Cesarean Section, Decision Support System.
Abstract: Introduction: The junction of postpartum hemorrhage (PPH) and cesarean section (C-section) is a potential
burden to take into account as a strategy to avoid unnecessary, and dangerous interventions. Despite most of
the maternal death could have been prevented, rates are unacceptably high. According to the WHO, the rates
of C-section are above recommended. The hypertension and PPH are the leading causes of maternal death
worldwide. Aim: This study propose to analyze the association between C-section and PPH in a electronic
health record (EHR) database and subsequently implementing an algorithm to assist health professionals in
the avoidance of unnecessary C-section based on the estimation of obstetric hemorrhagic risk. Methods:
Statistical analysis was performed using SISMater® database within 9,412 records about admissions to
childbirth. The C-section rates associated with the occurrence of obstetric hemorrhage reported in the EHR
was used to analysis. To implement the algorithm, the WHO and American College of Obstetricians and
Gynecologists (ACOG) recommendations were used. The decision rules were developed to estimate the
hemorrhagic risk score within the 10 groups proposed by the Robson classification. Discussion: It's
expected that the system will help to reduce unnecessary C-section rates and prevent PPH, providing better
conditions of prognosis for mother and her newborn.
1 INTRODUCTION
Rising cesarean deliveries is a worrisome reality in
the world. Many women worldwide are delivering
by cesarean section (C-section) without a clear
medical indication (WHO, 2009). Compared with
vaginal birth, delivery a child by C-section is
independently associated with additional risk of
maternal morbidity and mortality, even by elective
surgery (Villar, 2006). Last delivery by C-section
increases risk of severe maternal morbidity
regardless the mode of birth in the current
pregnancy, among them postpartum hemorrhage
(Villar, 2006).
In accordance with the United Nations'
Sustainable Development Goals (SDG) agreed in
2015, the reduction of unnecessary C-sections is
supported by 3rd goal, good healthy and well-being.
The goal 3 is to ensure healthy lives and promoting
the well-being for all at all ages is essential to
sustainable development (UN, 2018). Among the
actions, the recommendation of the use of quality
standards in obstetric care has been proposed as it
may improve maternal and child health. The
monitoring of proportion of women undergoing C-
section in the health facility according to Robson
classification groups is part of the best practices in
obstetrician (WHO, 2016). This classification groups
pregnant women based on their obstetric
characteristics, thus provide the systematic analysis
of C-section rates and comparing similar profile
institutions (WHO, 2015). The data collection
process and C-section rates analysis by clusters
helps institutions to evaluate the medical indicated
reasons for C-sections and propose actions to avoid
unnecessary surgeries (WHO, 2015). The model
proposed by Robson classify all women admitted for
delivery in ten homogeneous groups, based on
distinct characteristics of each individual woman
and her gestation instead of focusing on the
indication of the operative birth, and takes into
account: single or multiple gestation; parity and
presence of previous C-Section; presentation; form
of onset or C-Section before labor and gestational
age at birth (Robson, 2001).
In its turn, hemorrhagic complications in
pregnancy are associated with severe maternal
morbidity, as well as being one of the frequent
Gaspar, J., S. Junior, M., Lopes, R. and Reis, Z.
Cesarean Section Avoidance based on Obstetric Hemorrhagic Risk: A Decision Support System.
DOI: 10.5220/0007373802810285
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 281-285
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
281
causes of preventable maternal mortality, according
to world statistics (WHO, 2015b). The PPH is
characterized as cumulative blood loss greater than
1000 mL with signs and symptoms hypovolemia
within 24 hours of the labor process (ACOG, 2017).
It has been considered the leading cause of maternal
mortality in low-income countries and the primary
cause of nearly a quarter of all maternal deaths
globally (WHO, 2014). In developing countries
around 1.2% of deliveries are associated with PPH
(WHO, 2015).
In this context, was created Zero Maternal
Deaths by Hemorrhage project by the World Health
Organization (WHO) and Pan American Health
Organization (PAHO), which target to implement in
Latin America a set of interventions based on
scientific evidence to organize and simplify the care
on obstetric hemorrhagic emergencies (PAHO,
2018). In addition to this proposal, the ACOG
recommends cautious observation of the variables
associated with the risk of PPH, from the history of
labor to the puerperium (ACOG, 2017).
The intercession between the risk of PPH and the
C-section specific conditions it's still an incipient
theme. Computerized solutions that directly support
medical decisions in care scenarios have the
potential to mitigate risks and consequently reduce
the complications associated with PPH.
The aim of this study is to analyze the
association between C-section and PPH in a
electronic health record (EHR) database and
subsequently implementing an algorithm to assist
health professionals in the avoidance of unnecessary
C-section based on the estimation of obstetric
hemorrhagic risk.
2 METHODS
This is an interdisciplinary study between medicine
and computer science. It involves two steps: firstly,
were statistically analyzed the EHR about
admissions to childbirth; subsequently, an algorithm
was developed to estimate the obstetric hemorrhage
risk within each of the 10 groups proposed in the
Robson classification. The study was approved by
the Ethics Committee of UFMG (CAAE-Brazil
10286913.3.0000.5149).
2.1 Step 1: Data Analysis
Was made a retrospective EHR database analysis.
Comprise all admissions to childbirth occurred from
January 2014 to June 2018 (9,412 records), at
Hospital das Clínicas of Universidade Federal de
Minas Gerais, Brazil. Statistical analysis was
performed using SISMater® database, a non-profit
obstetric information system, developed by the same
researchers team, used since 2012 in this maternity
hospital (Gaspar, 2013).
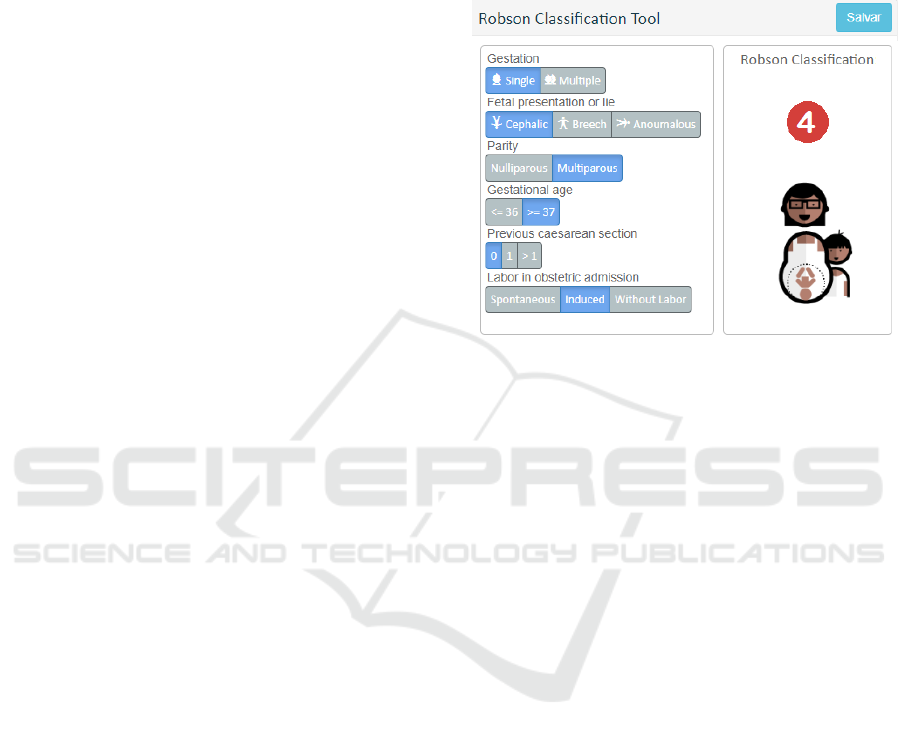
Figure 1: SISMater Robson Classification Tool.
All admissions to childbirth categorized in the 10
groups proposed by Robson classification and the
respective C-section rates were obtained from
system (figure 1) and associated with the occurrence
of obstetric hemorrhage reported in the EHR. The
Pearson chi-square test, Odds Ratio (OR) with 95%
confidence interval (95% CI) estimated the
association between C-section and obstetric
hemorrhage.
2.2 Step 2: Algorithm Implementation
In the second stage was developed and implemented
an algorithm to estimate the obstetric hemorrhage
risk within each of the 10 groups proposed in the
Robson classification, based on the Obstetric
Hemorrhage Risk Assessment Table (table 1)
(ACOG, 2017).
The risk algorithm is calculated from the sum of
the proposed Obstetric Hemorrhage Risk score
(OHR) in Table 2. The OHR indicates if the
pregnant woman has no previous risk (OHR = 0),
with low risk (OHR = 1), medium risk (OHR = 2 or
3) or high risk (OHR = 4) of obstetric hemorrhage
(Figure 2).
The PHP and JavaScript languages were used to
continue the pre-existing implementations in the
legacy software already used in the hospital.
HEALTHINF 2019 - 12th International Conference on Health Informatics
282
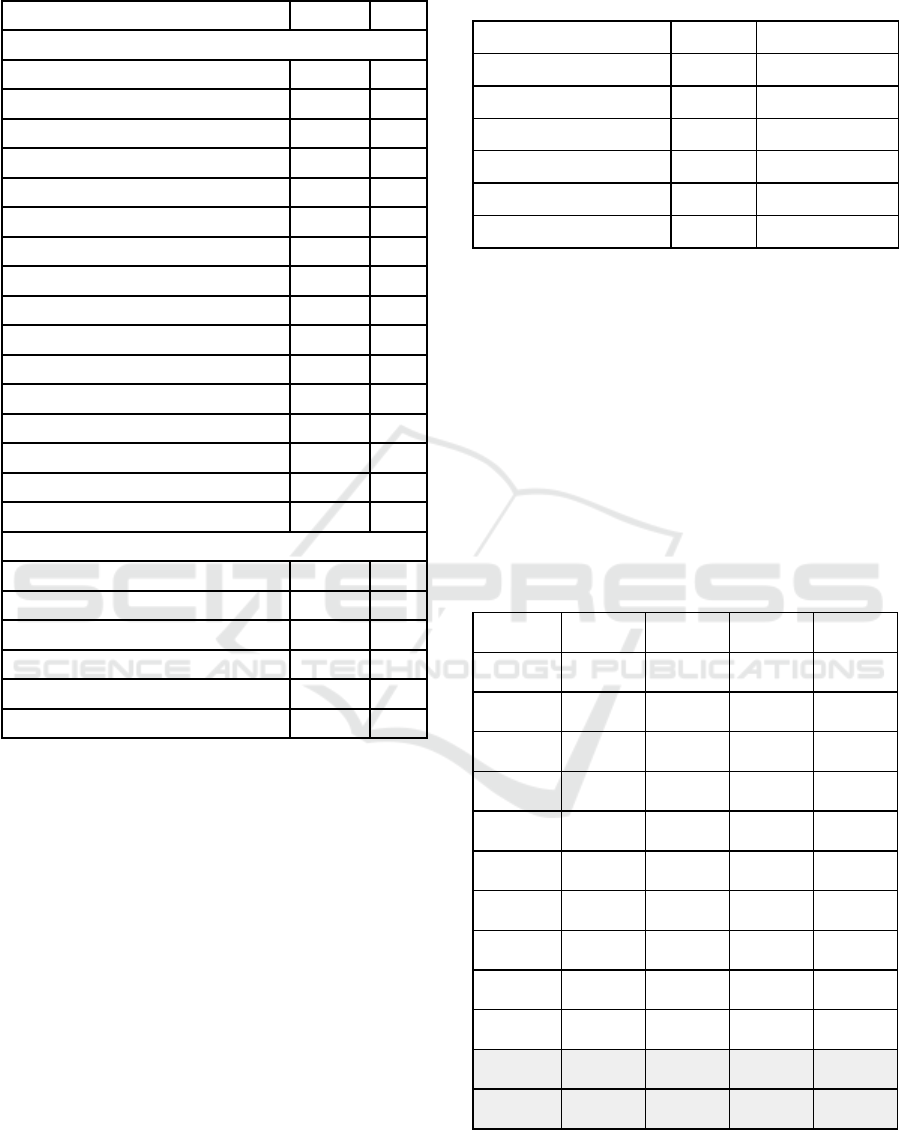
Table 1: Obstetric hemorrhage risk assessment.
Risk Factors
Risk
OHR
Prenatal and antepartum
Hematocrit < 30%
low
1
Prior cesarean
medium
2
Uterine surgery
medium
2
Multiple laparotomies
medium
2
Multiple gestation
medium
2
More than 4 previous deliveries
medium
2
Postpartum haemorrhage
medium
2
Large fibroids
medium
2
Estimated fetal weight > 4000g
medium
2
Obesity
medium
2
Placenta Previa
high
4
Acretism or Percretism
high
4
Platelet count < 70.000
high
4
Active Bleeding
high
4
Known Coagulopathy
high
4
Two or more medium risk factors
high
4
Labor and intrapartum
Chorioamnionitis
medium
2
Prolonged use of oxytocin (>24 hours)
medium
2
Extended 2nd stage
medium
2
Magnesium sulfate
medium
2
Recent active bleeding (at delivery)
high
4
Two or more medium risk factors
high
4
Fonte: ACOG, 2018. Obstetric Hemorrhage.
OHR = hemorrhage obstetric risk score
3 RESULTS
3.1 Data Analysis
Between January 2014 and June 2018, occurred
9,412 births in the maternity hospital. Were
excluded 69 records due to lack of information. The
missing information was vaginal birth or C-section,
single or multiple gestation, parity and presence of
previous C-section, fetal presentation, form of onset
or C-section before labor, gestational age at birth,
crucial data for Robson classification algorithm.
Considering the valid records (9343 records), the
cesarean rates, the maternal hemorrhage outcomes,
maternal death and maternal near miss, fetal death
and neonatal death are presented (Table 2).
Table 2: Childbirth record between 2014 and 2018 at the
maternity hospital.
Outcomes
N
C-section
Childbirth admissions
9343
3.441 (36.8%)
Obstetric hemorrhage
315
151 (47.9%)
Maternal death
6
5 (83.3%)
Maternal near miss
42
31 (73.8%)
Fetal death
297
50 (16.8%)
Neonatal death
295
143(48.5%)
N = Childbirths admissions number
Table 3 shows the association between cesarean
surgery and hemorrhage intrapartum and postpartum
in all cases (p<0.001), had the highest chance of
PPH (OR=1.les nossos amigos estavam 599)
associated with C-section. When analyzing the 10
groups by Robson classification separately, were
verified the significant association between cesarean
surgery and hemorrhage within groups 3, 4 and 10
(p=0.010, p=0.036 and p<0.001). Lastly, when
compared the 1 to 4 combined groups the
association also was verified (p<0.001).
Table 3: Association between C-section and obstetric
hemorrhage within the 10 Robson classification groups.
Group
N
P-value
Odds
ratio
CI 95%
G1
1771
0.186
1.539
0.812 -
2.918
G2
1292
0.920
1.026
0.618 -
1.702
G3
1878
0.010*
3.586
1.347 -
9.549
G4
928
0.036*
2.076
1.049 -
4.109
G5
1443
0.823
0.914
0.416 -
2.007
G6
263
0.749
1.425
0.163 -
12.445
G7
281
0.302
0.448
0.098 -
2.055
G8
192
0.373
0.070
0.418 -
10.249
G9
47
0.915
1.182
0.054 -
25.652
G10
1248
<0.001*
21.293
13.743 -
32.991
All groups
9412
<0.001*
1.599
1.276 -
2.004
G1-G4
5869
<0.001*
1.908
1.398 -
2.622
N = Childbirths admissions, CI = Confidence interval
* Significant association with Pearson Chi-square Test
Cesarean Section Avoidance based on Obstetric Hemorrhagic Risk: A Decision Support System
283
3.2 Algorithm Implementation
Figure 2: Obstetric hemorrhagic risk algorithm flow.
Figure 2 shows an algorithm scheme that classify the
pregnant women in the 10 groups proposed by
Robson. The algorithm recommends the avoidability
of c-section within each group: lower expectation of
c-section (groups 1-4), previous c-section group (5),
higher expectation of c-section (groups 6-10). After,
based on the factors read, the algorithm calculates
the hemorrhage obstetric risk.
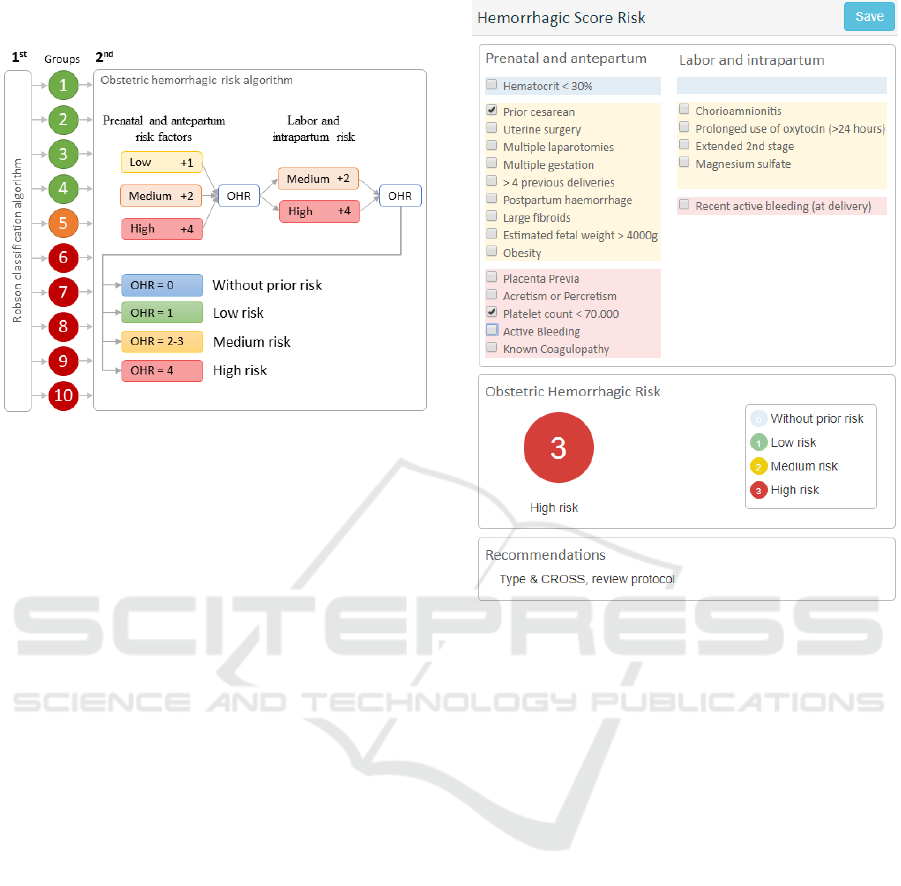
Figure 3 presents the developed interface that
contemplates the data entry for the obstetric
hemorrhagic risk algorithm proposed in this study.
The interface presents the risk factors separated
by severity, as well as the calculated Risk Score (0 -
3). At the end, displayed the standard procedures
should be taken by the team of professionals.
4 DISCUSSION
Obstetric complications demand well-prepared
health professionals identify obstetric risks and
manage critical situations using evidence-based
bundles (PAHO, 2018). Current data analysis
contributed revealing different chances of PPH,
according to the Robson Ten Group Classification
System (RTGC). So, the junction of already reported
variables associated with the risk of PPH, from the
history of labor to the puerperium (ACOG, 2017)
with the RTGC can be an advantage to support
timely decisions at birth.
For instance, pregnant women classified as G3,
G4 or G10 had more PPH when delivered by C-
Figure 3: Obstetric hemorrhagic risk interface.
section in comparison with vaginal birth. Special
attention for multiparity, independent known risk
factor for the uterine atony (Rossen et al., 2010),
even if without previous C-section had chance 3.586
(G3) and 2.076 (G4) higher of PPH. Algorithm
implementation is supposed to alert PPH risk when
term gestation in multiparous women became a C-
section prior the labor or during artificially
contractions induction. Group 10, all singleton,
cephalic, ≤ 36 weeks, (including previous CS) had
the highest chance of PPH associated with C-
section, OR=21,293. Even with low-evitability of
the cesarean, G10 group deserves more precautions
and careful managing to avoid PPH and improve
maternal outcomes.
ACKNOWLEDGEMENTS
This project was financially supported by
Coordenação de Aperfeiçoamento de Pessoal de
Nível Superior (CAPES), Skinage project,
Ministério da Saúde do Brasil and Obstetrics and
Gynecology Department of Faculdade de Medicina
da UFMG.
HEALTHINF 2019 - 12th International Conference on Health Informatics
284

REFERENCES
ACOG, 2017. Committee on Practice Bulletins-Obstetrics.
Practice Bulletin No. 183: Postpartum Hemorrhage.
Obstet Gynecol. 2017 Oct;130(4):e168-e186.
ACOG, 2018. Obstetric Hemorrhage. Available from:
https://www.acog.org/About-ACOG/ACOG-
Districts/District-II/SMI-OB-Hemorrhage. Access in:
21/20/2018.
Gaspar J, Chagas J, Osanan GC, Cruz-Correa R, Reis
ZSN, editors. Maternal and neonatal healthcare
information system: development of an obstetric
electronic health record and healthcare indicators
dashboard. International Conference on Information
Technology in Bio-and Medical Informatics; 2013:
Springer.
PAHO, 2018. Plan of action to accelerate the reduction in
maternal mortality and severe maternal morbidity:
Final Report. 162nd Session of the executive
committee. Washington, USA. June 2018. Available
from:
http://iris.paho.org/xmlui/bitstream/handle/123456789
/49240/CE162-INF-12-e.pdf. Access in: 21/20/2018.
Robson, M. 2001. Classification of caesarean sections.
Fetal and Maternal Medicine Review, 12(01), jan
2001. doi: 10.1017/s0965539501000122.
Rossen, Janne et al. 2010. Is there an increase of
postpartum hemorrhage, and is severe hemorrhage
associated with more frequent use of obstetric
interventions?. Acta obstetricia et gynecologica
Scandinavica, v. 89, n. 10, p. 1248-1255, 2010.
UN, 2018. About the Sustainable Development Goals.
Available from:
https://www.un.org/sustainabledevelopment/sustainabl
e-development-goals/. Access in: 21/20/2018.
Villar, 2006. Villar J et al. Cesarean delivery rates and
pregnancy outcomes: the 2005 WHO global survey on
maternal and perinatal health in Latin America. The
Lancet 2006;367(9525):1819-29.
WHO, 2009. Rising caesarean deliveries in Latin
America: how best to monitor rates and risks.
WHO/RHR/09.05. Available from:
Http://apps.who.int/iris/bitstream/handle/10665/70034
/WHO_RHR_09.05_eng.pdf. Access in: 21/20/2018.
WHO, 2014. Organização Mundial de Saúde.
Recomendações da OMS para a prevenção e
tratamento da hemorragia pós-parto. Avenue Appia
20, CH-1211 Geneva 27 Suíça; Available from:
http://apps.who.int/iris/bitstream/handle/10665/75411/
9789248548505_por.pdf. Access in: 21/20/2018.
WHO, 2015. World Health Organization. "WHO
statement on caesarean section rates." (2015).
Available from:
http://apps.who.int/iris/bitstream/handle/10665/16144
2/WHO_RHR_15.02_eng.pdf.
WHO, 2015b. World health statistics 2015. Luxembourg:
WHO Library Cataloguing-in-Publication Data; 2015.
Available from:
http://www.who.int/gho/publications/world_health_sta
tistics/EN_WHS2015_TOC.pdf. Access in:
21/20/2018.
WHO, 2016. Standards for improving quality of maternal
and newborn care in health facilities. ISBN
9789241511216. Available from:
http://apps.who.int/iris/bitstream/handle/10665/24915
5/9789241511216-eng.pdf. Access in: 21/20/2018.
Cesarean Section Avoidance based on Obstetric Hemorrhagic Risk: A Decision Support System
285
