
The Importance of Nurse Knowledge about Physical Examination
and Inform on Medical Record Facility Inpatient Patient: Case Study
in Sari Asih Hospital Karawaci Tangerang
Astri Annatasia
1
, M. Reza Hilm
y
1
, Rokiah Kusuma
p
rad
j
a
1
and Erlina Pus
p
italoka Mahadewi
2
1
Master Program Adminsitrasi Hospital (S2, Esa Unggul University Jakarta
2
Faculty of Health Sciences, Esa Unggul University Jakarta
Keywords: medical records, knowledge, inpatients.
Abstract: Based on the results of the observation in Sari Asih Hospital Karawaci Tangerang obtained medical record
of hospitalized records are still many empty is that in 2016 there are 296 (3.4%) patients and in 2017 there
are 405 (3.9%) patients. The incompleteness of medical record data mostly occurred on the accuracy of
patient identity (name, a medical record number, place of birth date, sex) that is 37 patients (9%); and
physical examination of 44 patients (11%), informed consent 47 (12%). The nurse's function as one of the
data inputs that make the documentation of nursing care actions will affect the quality of the patient's
medical records. The incompleteness of DRM is because there are still many nurses who have poor
knowledge (60%) about medical records.The purpose of this research is to determine the effect of
knowledge of nurses in filling out medical records on the completeness of medical records file of inpatients
(case study in Rs. Sari Asih Karawaci Tangerang). The design of this study is associative causal (causal)
with a quantitative approach. The object of this research is nurses in hospital wards as much,and samples
counted 25 people with purposive sampling technique. Data collection by using primary data in the form of
questionnaire/questionnaire and secondary data based on RM 2017 data which then analyzed by binary
logistic regression analysis.Based on the result of regression logistic binary statistical analysis, it is found
that the nurses' knowledge variable in the filling of the medical record has a significant effect on the
accuracy of the medical records file of the inpatients The better the nurse's knowledge,the more complete
the patient's medical record. Advice for hospitals to socialize, regularly monitor and evaluatenurses, about
the importance of completeness in filling the medical record.
1 BACKGROUND
Hospitals are health referrals that serve
outpatients, emergency and inpatient care with
various types of medical services and medical
support in a hospital service system. Serving the
patient is one of the hospital services, in accordance
with the Regulation of Medical Record (RM) in
accordance with the Regulation of the Minister of
Health of the Republic of Indonesia Number 269 /
Menkes / PER / III / 2008 dated 02 March 2008 on
Medical Record. Also described medical record is a
file containing records and documents about the
patient's identity, treatment examinations, actions
and other services that have been given to the
patient. Medical records should be in writing,
complete and clear or electronically.
There is already a fixed procedure (attached)
about the completeness of medical records data in
inpatient turned out from the observations in "RS
Sari Asih Tangerang" in the assembling in the
implementation of his duties generated data medical
records hospitalized records are still many empty.
RS Data. Sari Asih Karawaci Tangerang in 2016
showed 8,793 (14.7%) of inpatients from 59,993
patients overall, from 8,793 inpatients there were
296 (3.4%) patients with incomplete medical record
data. While in 2017 it showed an increase in
hospitalized patients to 10,308 out of 85,947 patients
as a whole, and from 10,308 inpatients there were
405 (3.9%) patients with incomplete medical record
data. The incompleteness of medical record data
mostly occurred in the patient accuracy of patient
identity (name, a medical record number, place of
birth date, sex) that is 37 patients (9%); and physical
Annatasia, A., Hilmy, M., Kusumapradja, R. and Puspitaloka Mahadewi, E.
The Importance of Nurse Knowledge about Physical Examination and Inform on Medical Record Facility Inpatient Patient: Case Study in Sari Asih Hospital Karawaci Tangerang.
DOI: 10.5220/0009950704910498
In Proceedings of the 1st International Conference on Recent Innovations (ICRI 2018), pages 491-498
ISBN: 978-989-758-458-9
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
491
examination 44 patients (11%), informed consent 47
(12%)
The nurse's function as input data made from the
nursing care actions performed will affect the poor
quality of information in the patient's medical
records. Better health data quality in the patient's
medical record can be reviewed by and therefore
requires a good knowledge of the nurse.
Knowledge of medical records, in this case, is
the knowledge of what should be accomplished in
the filling example of medical records other than
that how to create a medical record correctly in
accordance withPermenkes (2008) consisting of
patient identification, treatment examinations,
actions and other services that have been given to
the patient
Initial survey conducted by the researchers
resulted in data that there are still many nurses who
have poor knowledge (60%) about the medical
record.
The existence of this study is expected to
contribute or its application, especially for nurses
about the filling of medical records
This motivation is to improve the knowledge
about the medical record so that the quality of
medical record becomes better and better quality.
2 RESEARCH METHODS
This research method using research method
with a quantitative approach to know the significant
relationship between variables studied. The
technique used in this study is to determine the
sample size of the population is a purposive
sampling technique. Data analysis used binary
logistic regression analysis. Sari Asih Karawaci
Tangerang with one shot time horizon to study that
is research done with the previous study, week,
week, in order to answer the research question
OPERATIONAL DEFINITIONS VARIABLES
In this study the dependent variable (Y) is the
completeness of the medical record is a file
containing records and documents about the identity,
examination, treatment, action, and other services
that have been given to the patient in the form of
physical examination data and informed consent
with the instrument of the questionnaire based on
medical records of RS Sari Asih Tangerang in 2017
with interval scale. While the independent variable
(X) is the knowledge of the nurse that is knowledge
about what should be completed in the filling of
medical record file and Understanding the correct
way of writing medical records file in accordance
with Permenkes year 2008 with instrument is a
questionnaire consisting of 15 items of questions
with interval scale
2.1 Research Result
The result of research is shown in the frequency
distribution of respondent characteristics as follows:
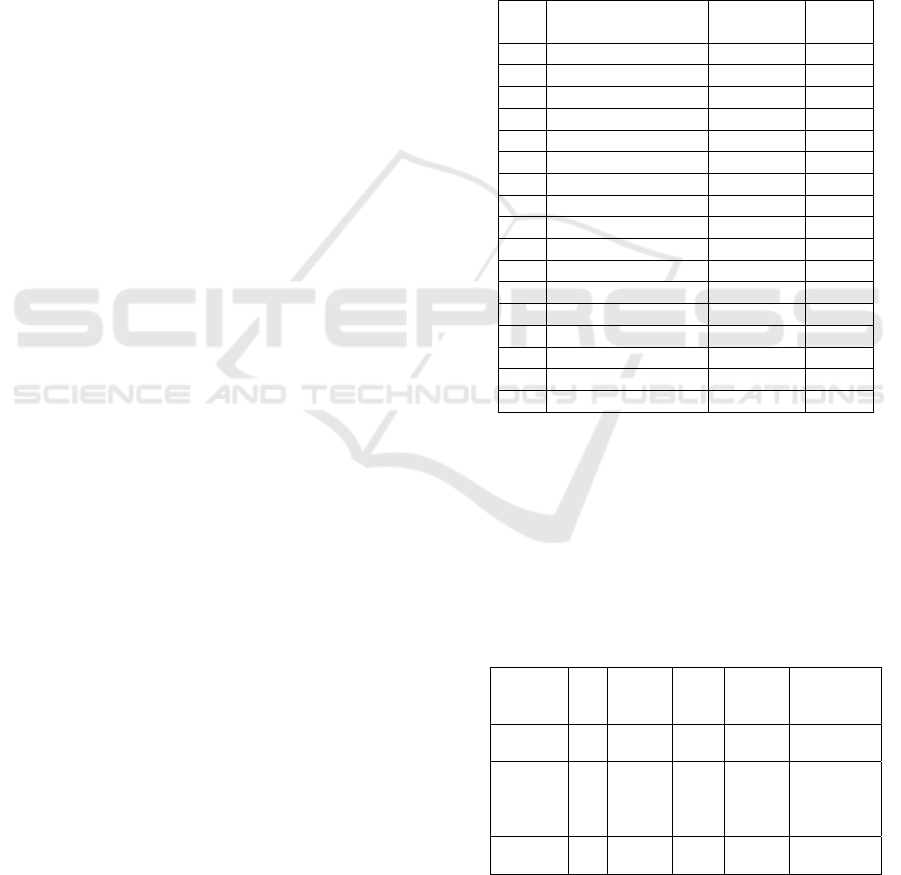
Table 1: Characteristics of Nurse RS Sari Asih Karawaci
Tangerang
No Characteristics of
Respondents
Amount %
1. Age
20-26 years old 6 24
27-40 years old 15 60
41-61 years old 4 16
2. Last education
SPK 0 0
DIII 13 52
S1 8 32
S2 4 16
3. Years Of Work
< 1 year 2 8
< 5 year 5 20
< 10 year 10 40
> 10 year 8 32
4. Gender
Man 7 28
Woman 18 72
Source: data that has been processed (2018)
Based on Table 4.1 above, respondents are
mostly aged 27-40 years, 60%, most respondents
have recent education DIII (52%), work-based
characteristics are mostly found <10 years (40%)
and most of them are female (72%).
2.2 Variable Descriptive Satistics
Table 2: Results Descriptive Statistics Variable
Variabe
l
N Mini
mum
Ma
xim
um
Mean
Std
Deviation
Knowle
dge
25 6 15 11.40
2.90115
Complet
e
Medical
Record
25 32 37 36.12
1.56312
Vallid
(N)
25
Source: data that has been processed, SPSS 24
ICRI 2018 - International Conference Recent Innovation
492
Output table 4.2 above shows the value of N or
the amount of data to be studied amounted to 25
samples. The nurse's knowledge about the filling of
medical record file has mean or a mean value of
11.40 which means that the average knowledge of
the nurses is included in either category with a
maximum value of 15 and a minimum value of 6
With a standard deviation of 2.90115 it can be said
the average value of deviation of knowledge
variables is 2.9%. Furthermore, for medical record
completeness variable obtained mean or mean value
of 36.12 which means the average completeness of
medical records file included in the category either
with a maximum value of 37 and a minimum value
of 32. With the standard deviation 1.56312 can be
said the average value of deviation variable the
completeness of the medical record is 1.56%.
The descriptive results of each variable based on
the number of presentations are as follows :
StatisticsTest
1. ValidityTest:The test results of instrument
validity to 10 respondents are as follows:
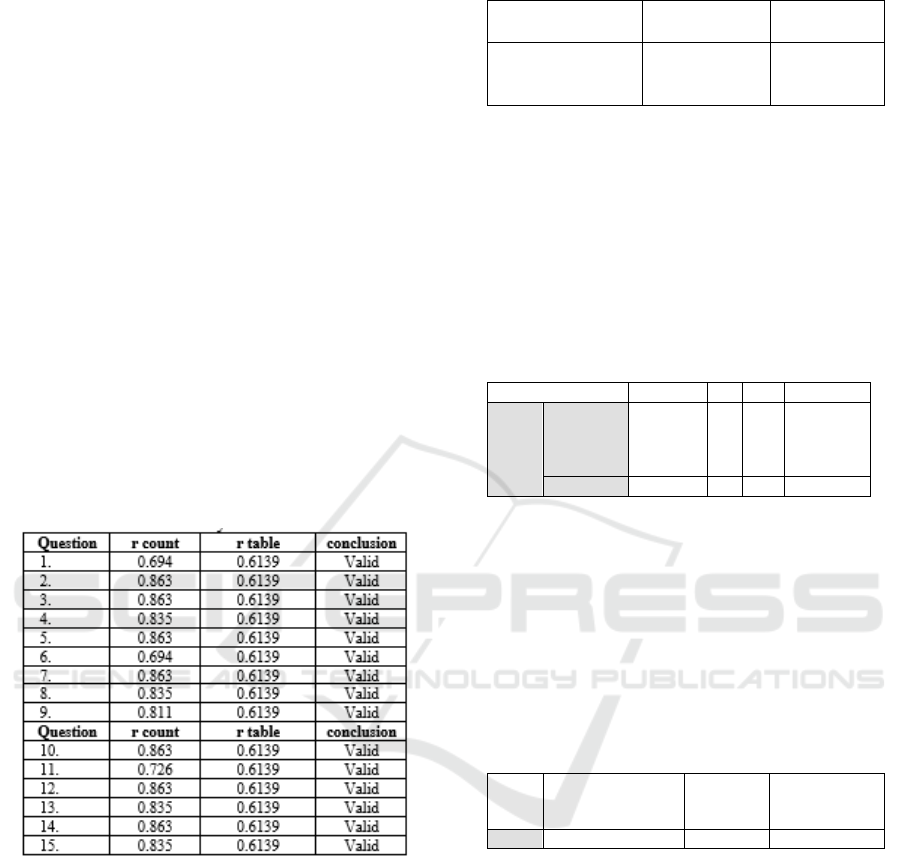
Table 3: Validity Test Results
Source: data that has been processed, SPSS 24
The table above shows that all the question items
in this study are valid. Where r table value with the
number of respondents (N = 10 or df (N-2) = 8) and
the significance level of 0.05 is 0.6139. The r
valueof the whole question is greater than r table,
which means the question items in the questionnaire
have met the validity requirements
2. ReliabilityTest
Next is the reliability test of the questionnaire by
taking 10 samples of Inpatient Patients BPJS Sari
Asih Ciledug Hospital is processed using a
computerized system with the softwareSPSS version
24 is:
Table 4: Reliability Test
Variable Cronbach’s
Alpha
Conclusion
Nurse Knowledge
About Medical
Record
0.975 Reliable
Source: Primary data that is processed (2018)
In table 4.4 it can be seen that the knowledge
variable of medical record file has Cronbach's Alpha
(α) above 0.60 so it can be said that all the concepts
of variable measuring of the questionnaire are
reliable which means that the questionnaire used in
this study is a reliable questionnaire to be analyzed
Furthermore.
1. Wald Test
Table 5: Wald Test
Wald df Sig. conclusion
Step 1
a
Medical
Record
Completen
ess
11.000 1 .006 Be
accepted
Constant 1.199 1 .000
Source: Primary data that is processed (2018)
Based on table 4.5 above can be seen that the
value of wald by 11,000 with the value of sig 0.000
<0.05 (5%), it can be concluded that the hypothesis
accepted the knowledge variable significantly affect
the completeness of the medical record file.
2. Coefficient of Determination Test Nagelkerke
R Square
Table 6: Nagelkerke R Square Test
Step -2 Log likelihood
Cox &
Snell R
Square
Nagelkerke R
Square
1 8.376
a
.486 .769
Source: Primary data that is processed (2018)
Based on the results of Nagelkerke R square test
obtained value of 0.769 which means then the
proportion of completeness of the medical record
file that can be explained by 76.9%. while the
remaining 23.1% can be explained by other
variables outside the research model such as
attitudes, beliefs, beliefs of values, physical
environment (facilities or health facilities), attitudes
and behavior of health workers or other officers.
The Importance of Nurse Knowledge about Physical Examination and Inform on Medical Record Facility Inpatient Patient: Case Study in
Sari Asih Hospital Karawaci Tangerang
493
3 DISCUSSION
3.1 Univariate Analysis
3.1.1 Nurse Knowledge in Charging Medical
Record Files
The knowledge that is discussed in this research
that is about a medical record that is knowing what
must be completed in filling out medical record file
and understand how to write medical record file
correctly in accordance with Permenkes year 2008
consisting of writing name, contact person address,
record number medical and patient age etc. (Shofari,
2006). According to Permenkes No. 269 In 2008, the
medical record is a file containing records and
documents such as patient identity, examination
results, a medication that has been given, and other
actions and services that have been given to the
patient. The purpose of the medical record is to
support the achievement of orderly administration in
order to improve health services. Without the
support of a proper medical record management
system, then the administrative order will not
succeed (Gondodiputro, 2007). The scale assessment
of knowledge categories based on Budiman and
Riyanto (2013) are grouped into two groups:
1) Knowledge level category Good value> 50%
2) Knowledge level category Less good value ≤ 50%
In this research obtained most of the knowledge
of nurses included in the good category as many as
20 people (80%). While as many as 5 people with
less good knowledge (20%) as for the score answer
each question item on the questionnaire knowledge
sheet as follows.
Table 7: Respondents answer Score
No Question Score (%)
1. At least the things that should be
included in the medical record
are identity, anamnesis, physical
examination, and diagnosis
15 60
2. Medical Records on the patient's
physical examination include
information such as inspection,
palpation, percussion and
auscultation
21 84
3. Medical Record regarding the
physical examination of the
patient contains the patient's
nursing history
23 92
4. Medical Record regarding the
physical examination of the
patient at least contains the
height of the body (TB), weight
23 92
No Question Score (%)
(BB), temperature, and
pulse/pulse frequency.
5. Medical Record results have to
be complete within 24 hours
after the patient is treated and
before the surgery
22 88
6. Medical Record physical
examination contains the history
and the course of the patient's
illness
23 92
7. Medical Record physical
examination contains diagnosis
and patient laboratory results
22 88
8. In the Medical Record form of
Informed consent contains the
consent of the medical treatment
signed by the patient/family of
the patient concerned
beforecertainactions/therapies
9 36
9. In the Medical Record form of
Informed consent contains the
consent obtained by a physician
before any medical examination,
treatment, and medical action to
be performed for the patient's
healing
16 64
10. The Medical Record form
informed consent contains the
patient's identity (Name, date of
birth, Gender, address, ID / ID /
SIM, no phone)
23 92
11. The Medical Record form
informed consent form must be
signed by the patient/patient's
family 24 hours before any
medical action is taken
22 88
12. The Medical Record form
informed consent form is known
and signed by both witnesses,
the nurse acting as one of the
witnesses
21 84
13. The Medical Record form
informed consent form must be
stamped
14 56
14. The Medical Record form
informed consent form is not
required for emergency patients
who are not accompanied by the
patient's family
7 28
15. The Medical Record form
informed consent form must be
signed by the physician as the
person in charge of the written
information
24
96
Source: Primary data that is processed (2018)
Fromdata can be seen for the medical record
physical examination of the lowest score on the item
question 1 with a score of 15 (60%) ie at least things
that should be included in the medical record is
identity, anamnesis, physical examination and
diagnosis when for file recording especially in
inpatients must contain at least about the identity of
ICRI 2018 - International Conference Recent Innovation
494

the data, date and time, the results of the history, the
results of physical examination, investigation,
diagnosis, management plan, treatment, observation
record, home summary, name and sign of doctor /
dentist for dental cases equipped with odontogram.
Further scores on item no. 2 of 21 (84%) with RM
note notes regarding physical examination of the
patient include information in the form of
inspection, palpation, percussion and auscultation.
Though it should be information of RM physical
examination not only that but also include an
examination of the head to toe which contains the
result of the check of vital signs (temperature, blood
pressure, pulse, respiratory rate) and basicbiometric
(TB, BB, Pain).
As for the informed consent, the lowest score on
item no 14 (7%) is the RM informed consent form
not required for emergency patients who are not
accompanied by the patient's family. In this
question, many nurses who assume in emergency
conditions must continue to fill in informed consent.
Whereas according to Permenkes No 209 / Menkes /
Per / III / 2008 in Article 4 paragraph (1) that no
informed consent needed in emergencies. However,
if an action has been taken to rescue the emergency,
the physician is obliged after that to explain to the
patient or immediate family.
The next lowest score on item 8 with a score of 9
(36%) with the question on the RM form of
Informed consent contains the consent of the
medical treatment signed by the patient/family of the
patient before any specific action/therapyis
performed. Many nurses consider informed consent
only for certain therapies. Whereas informed consent
is written and oral consent which is done for all
medical actions in normal circumstances and
emergency situations.
Overall nurse knowledge about RM physical
examination and informed consent included in good
category, this can be seen from the mean value of
11.40.
The results of this study in line with research
conducted by Agus Siswanto in 2012 obtained the
results of nurse knowledge about the regulation of
medical record in the category very good 43.6%,
both 25.5%, quite 23.6%, and less 7.3% . Another
study conducted by Ardika (2012) found that 11
people (73.3%) who know medical records in either
category.
The low score on statement item # 1 concerning
the inclusion of minimal data on medical record
documents is very fatal because most respondents
answered wrongly (60%). Similarly, question no 2 is
about RM records on physical examination of the
patient. This proves that there are still many nurses
who do not know about the procedure of filling the
medical record correctly. According to the medical
record document, researchers should be given
sufficiently detailed data, as this relates to treatment
and care to the patient and the implementation of
further examination to the patient. As for the
informed consent the lowest score on item No. 8 and
14. This indicates that many nurses who do not
understand the use of informed consent.
The nurse as one of the medical record personnel
has the responsibility to evaluate the quality of the
medical record itself to ensure consistency and
completeness of the content. Therefore, the RM
report, in this case, the physical examination and
informed consent is in full condition and contains all
positive and negative discovery data.
According to the researcher the good level of
knowledge by the nurse this is caused by 60% age of
respondents are in the range of 27-40 years it shows
the nurse at productive age to produce good
performance besides the highest nurse education
level is DIII (52%) and work experience <10 years
(40%) this is also a good input for nurse knowledge
because education influences the learning process,
the higher the education of a person the easier it is
for the person to receive the information. With
higher education then one will tend to get
information both from others and from the mass
media. The more information that goes in,the more
knowledge gained about health. Knowledge is
closely related to education where it is expected that
someone with higher education then the person will
be more knowledgeable. Further experience or high
work can increase the knowledge of nurses because
experience as a source of knowledge is a way to
obtain the truth of knowledge by repeating the
knowledge gained in solving problems faced in the
past so that with long service can develop a person's
ability to increase knowledge.
Also, nurses who have a good knowledge of
medical records (80%) are nurses who are always
active to find out about SOP filling the medical
record. While 20% of nurses with knowledge of
filling the medical record is not good, this is
according to the researcher because the nurses are
not active to seek information about medical records
either ask through RM officers, doctors, midwives,
verifieretc. and never participate in training and
workshop about medical record. Nurses who do not
yet have a good knowledge of medical records are
usually new nurses who have not been input from
long-standing nurses with good experience in filling
out medical record data. According to Notoatmodjo
The Importance of Nurse Knowledge about Physical Examination and Inform on Medical Record Facility Inpatient Patient: Case Study in
Sari Asih Hospital Karawaci Tangerang
495

(2010), the source of certain knowledge possessed
and controlled by a person is obtained through
experience, both individually and in society.
3.1.2 Medical Record Completeness
Medical records according to the Indonesian
Minister of Health Regulation 269 / MENKES /
PER / III / 2008 are files containing records and
documents on identities, checks, medications,
actions and other services that have been provided to
patients. The completeness of medical records is of
great importance because the complete medical
resume in addition to maintaining the quality of
medical records is also used for the administration of
insurance claims (Anggraini, 2013)
Referred to the completeness of medical records
in this study is the completeness of medical records
documents viewed regarding clinical examination
and informed consent.
Based on this research, the researcher get the
result of the contents of the medical record
document of inpatient patient of BPJS in Asari
Karawaci Hospital of Tangerang in 2017, is as
follows: from 25 samples of medical record
document there are 18 medical record documents
complete with percentage 72%, while medical
record which is incomplete there are 7 with a
percentage of 28%.
The result of this research is in line with the
research conducted by Ardika (2012) which is 10
documents RM (66,7%) that fulfill the complete
category.
Physical examination is a physical examination
in the whole body of the client's examination,or only
a certain part is deemed necessary, to obtain
systematic and comprehensive data to ensure/prove
the results of anamnesis, determine the problem and
plan appropriate nursing actions for the client (Dewi
Sartika, 2010)
In this research for Medical Record Form of
Physical Examination there are 5 RM files of patient
with incomplete field that is on:
(1) High Body Examination (TB)
Height is a measure of the size of a human
body in height measured in pure state of height
from heel to head without any other object being
measured (Setyapranomo 2017).
In this research data Medical record TB
incomplete according to the researchers, this is
because there are still nurses who are not
disciplined in the filling fil records RM record
(2) Mental Status
The mental status examination includes
mental status assessment, awareness assessment,
psychomotor activity assessment, orientation
assessment, perceptual assessment, form and
thought content assessment, mood and affective
assessment, impulse control assessment, reality
valuation assessment, insight assessment,
functional ability assessment (MOH, 2010)
In this research medical record data mental
status incomplete according to the researchers
this is because there are still nurses who are not
disciplined in the filling completelyMedical
record.
(3) Genital Devices
Genitalia Physical Examination is to find out
whether the client has a problem with genitalia
(vital tool) both internally and externally.
According to researchers physical
examination of the patient's genitals can make
the client feel ashamed,sonurses should take a
quiet approach. The gynecological examination
is a difficult experience for the patient. Also,
there are cultural restrictions.Therefore there are
still nurses who do not perform a physical
examination of the genitals in patients.
Next, on the Informed Consent form,6 RM
patient files are incomplete which include:
(1) No identity (KTP/SIM) of the patient
(2) TTL family members (* authorized)
(3) No identity (KTP/SIM) of family member (*
authorized)
(4) Signature of the witness of the patient
Informed consent is incomplete according
to the researcher because the patient/family
of the patient did not complete the form at the
time of consultation. Therefore the nurse
should be careful and careful inquiries and
should ensure that questions asked on the
form are clear and understandable by the
patient
3.1.3 Nurse Knowledge in Charging Medical
Record on Medical Files Record
Completeness
Based on the results of research that has been
described previously it is obtained data that there is a
significant influence between nurse knowledge
variables in the filling of medical records to the
completeness of medical records file it can be seen
in table 4.3 that is obtained wald value of 11,000
with the value of sig 0.000 <0.05 (5% ), then the
influence of knowledge variable with the
ICRI 2018 - International Conference Recent Innovation
496

completeness of medical record is 76.9% this is
proven by the test of nagelkerke R square (Table
4.5). While the remaining 23.1% affect the
completeness of medical records by other variables
that are not examined such as attitudes, beliefs,
beliefs values, physical environment (facilities or
health facilities), attitudes and behavior of health
workers or other officers.
The results of this study are in line with research
conducted by Utami (2016) which states that there is
a meaningful relationship between nurse knowledge
about the medical record with the completeness of
nursing note at the inpatient installation at Al AT-
Turots Al-Islamy Sleman General Hospital (p =
0.006). Another study conducted by Agung Personal
(2011) suggests that low-knowledge nurses risk
6.280 times greater for incomplete documentation.
According to the Minister of Health Number 269
of 2008, the documentation of medical record file is
started when the patient is admitted to the inpatient
ward, the receiving nurse must fill out the recording
form starting from the identity (name and patient RM
number), the report should include data assessment,
diagnosis, nursing actions, and the execution and
evaluation of actions when carrying them out, then
continued with authentication (affixing doctor's name
and signature). The medical record resume is
completed by the nurse as soon as the patient is
declared allowed to go home by the doctor, or go
home at his request, or dies. From this, it can be
concluded the completeness of medical records file is
very important to support the performance of health
practice. Ardika (2012) states the completeness of
documenting the medical record is influenced by
various factors such as educational background,
length of service, knowledge, skills, motivation,
psychological and so forth.
Of the 7 incomplete medical record documents,
were analyzed further without the use of statistical
tests and obtained results that nurses filled the
document with an uneven distribution of age from 22
to 33 years old and they were mostly graduates from
nursing school (SPK). The data obtained on the
educational background of the research samples
showed 48% were graduates of undergraduate
nursing (S1) and S2 they have knowledge about the
good medical record and complete the documentation
of nursing care completely.
While the other 52% who are graduates from the
SPK, nursing academy (DIII) and perform the
process of documentation with different levels of
completeness. This difference in completeness may
be due to the lack of knowledge, awareness and
motivation of the nurse to complete the
documentation process. Also, SPK education and
academy is a beginner profession education so that in
the implementation of its work requires experience
and training enough to be able to do the job well.
Knowledge is very important in forming one's
behavior, hence from the result of this research
indicate that the better the nurse’knowledge about
filling of medical record file hence more complete
data of patient medical record. Therefore, for RS
Sari Asih Karawaci Tangerang to maintain and even
improve the knowledge of medical record officer for
the implementation of hospital management system
by conducting training or seminar related to the
medical record.
3 CONCLUSION
Based on the results of research on the Influence
of Nurses' Knowledge in Filling Medical Records
Against Completeness of Medical Record Files
Inpatient Patients at RS. Sari Asih Karawaci
Tangerang Year 2017, it can be concluded as the
most of the knowledge of nurses in the filling of
medical records file included in good category
(80%), then most of the completeness of medical
records file of inpatients included in complete
category (72%). The result of the statistical test
showed that there was significant influence between
the nurse knowledge variable in filling the medical
record to the completeness of the medical record
file. This was proved by the wald test value of
11,000 and the sig value 0.000 <0.05
The nurse's knowledge about charging RM will
affect the quality of the medical record which
ultimately also affect the hospital administration.
Because as the main objective of the medical record
is to support the achievement of the administrative
order to improve health service in the hospital,
without support by a system of medical record
management good and correct, orderly hospital
administration will not succeed as expected. Also,
incomplete medical record data resulted in delays
from Claim payments submitted by the Hospital
which will also affect the hospital operations is the
obstruction of Hospital cash flow (cashflow).
4 IMPLICATIONS
1. There should be an education, workshop
training, and seminar related to medical record
to improve the knowledge of the nurse
The Importance of Nurse Knowledge about Physical Examination and Inform on Medical Record Facility Inpatient Patient: Case Study in
Sari Asih Hospital Karawaci Tangerang
497

2. The nursing perception among nursing staff
about filling the completeness of medical
records file so that all nurses can perform their
duty well according to SOP.
3. Nurses should be careful and careful inquiries
and should ensure that questions asked on the
informed consent form are clear and
understood by the patient
4. Preferably for newly employed nurses from the
beginning of the orientation given the
knowledge and advance about the importance
of the completeness of the inpatient medical
record file
5. To the management of RS to activate the
function of medical record committee in charge
of planning, implementation, supervision,
controlling, audit and assessment of medical
service quality according to the guideline of the
medical record of MOHRI so as to improve the
quality of hospital service.
5 SUGGESTION
1. Need to do further research to find other factors
that influence the completeness of the patient's
medical record
2. Nurses are expected to carry out a fixed
procedure or SOP on filling in the
completeness of the existing medical records
file
3. For the management of Sari Asih Hospital
Karawaci Tangerang to socialize,
regularlymonitor and evaluate to health
workers, especially nurses, about the
importance of completeness in filling medical
records.
4. For the hospital to provide work motivation to
the nurses in the treatment room about the
importance of the completeness of medical
record files
5. For further researcher need to dig further
information related to medical record
completeness by taking all indicator in filling
in the medical record of inpatient (for example
identity, anamnesis, investigation etc) so that
can get good analysis result
REFERENCES
Great, Private. Analysis of Influence Factor Knowledge,
Motivation, and Perception Nurses About Room Head
Supervision Against the Implementation of Nursing
Care Documentation in Inpatient Room of Kelet
Hospital. Central Java Province in Jepara. Semarang:
Faculty of Public Health. UNDIP; 2009
Ardika. Relationship between Nurses' Knowledge of
Medical Records with Completeness of Nursing
Records. Semarang: Diponegoro University
Semarang. 2012
Dewi, Sartika. Physical examination.
http://nursingbegin.com/tag/pemeriksaan-
phisik/(online) accessed 07 February. 2018. Jakarta.
2010
Gondodiputro. Medical Records And Health Information
System In Primary Health Care Facilities Puskesmas.
E-Journal of Public Health Sciences Faculty of
Medicine, Padjadjaran University of Bandung. 2007
Notoatmodjo. Health Research Methodology. Jakarta:
Rineka Cipta. 2010
Permenkes No. 269 / Menkes / Per / III / 2008. About
Medical Record. Jakarta: 2008
Shofari B. Management of Medical Record Service System
at the Hospital. Jakarta: Rineka Cipta.2006
Utami, Sri. Knowledge Level Relationships About Medical
Records With Completed Filling Of Nursing Notes On
Inpatient Installations At At-Turots Hospital Al Islamy
Sleman. Yogyakarta. E-journal. Retrieved on February
2, 2018. http://www.permataindonesia.ac.id/wp-
content/uploads/2016/08/06. -Journal-PI_Utami-
Amalina-Fahmi.pdf. Journal of Permata Indonesia.
Volume 7, Number 1, May 2016. 2016.
ICRI 2018 - International Conference Recent Innovation
498
