
Basic Occupational Health Service Management in SJSN Era: Case
Study at In-company Clinic PT X Indonesia
Ade Heryana
1
, Puteri Handayani
1
, Erlina Puspitaloka
1
and Amal Chalik Sjaaf
2
1
Public Health Department, Esa Unggul University, 9 Arjuna Utara, West Jakarta, Indonesia
2
Health Policy and Administration Department Faculty of Public Health Universitas Indonesia, Indonesia
Keywords: Occupational Health Service, Social Security, Office clinic service, Health security, Work injury security
Abstract: Background: This research composed on the primary thinking that implementation of the National Social
Security System or SJSN in Indonesia had changed the provision of basic occupational health service
(BOHS). In the middle of an occupational health service’s problem in Indonesia, the process of health
financing reform through SJSN had to stay on the track. With the in-company clinic of PT. X as a research
locus, researcher studied the implementation of SJSN to the provision of basic occupational health service at
big industries or big OHS Centre. Methodology: This research conducted with the qualitative method,
primary data collected by in-depth interview to the informant from Office clinic PT. X and six selected
informants from any field who linked to SJSN implementation on the provision of basic occupational health
service. Data analytic conducted with reducing, displaying and the formulating of conclusion process. The
results and conclusion: implementation of SJSN changed the provision of basic occupational health service
from the point of view such as health program, financing, human resources, facilities, and supporting factor
(management, information, regulation, and community empowerment). Government and BPJS as the
operator of SJSN should arrange the applicative solution in order to the provision of occupational health
service at office clinic stay in line with SJSN without the ignorance to occupational health and safety
standard.
1 INTRODUCTION
The implementation of National Social Security
System or SJSN (Sistem Jaminan Sosial Nasional)
that operated by “Badan Pengelola Jaminan Sosial”
or BPJS in January 2014 for BPJS Kesehatan and 1
July 2015 for BPJS Ketenagakerjaan, somewhat had
influenced to the provision of health program in
many fields, including on occupational health
service. The shifting on beneficial aspects led to
change in the company paid a premium. It is the
consequence of the compulsory to the company to
registered they workers at all of the social security
programs according to Indonesia Law Number 24 of
2004. This condition impacted the escalating of
workers wellness cost foremost to the company who
previously implemented a partial social security
program. At the side of human resources, it certainly
that healthcare forces will serve more workers in
primary care that led to the debriefing of sufficient
occupational health competence. Meanwhile, at
regulation aspects, several occupation health service
regulations have to in the same direction with the
regulation of workers health security and social
security.
According to Rantanen (2005) Basic
Occupational Health Services (BOHS) are “an effort
to provide access to occupational health service” that
applicated in the same direction as Alma Alta
principles. BOHS intended to the underserved
majority of workers of the world. The
implementation of SJSN supported this aims of
Alma Alta and basic function of BOHS that setting
out Universal Health Coverage on 2019.
The employer of employee organizes the BOHS
and provided by the public sector for the self-
employed and the informal sector (Rantanen, 2005).
This BOHS schematic was implemented in
Indonesia. Two ministries provided Occupational
Health Services for all workers in Indonesia i.e.
Ministery of Labour (MOL) and Ministry of Health
(MOH). MOL directs the employer of the employee.
Meanwhile MOH directs public sector and informal
sector on the implementation of BOHS. In practice,
2686
Heryana, A., Handayani, P., Puspitaloka, E. and Sjaaf, A.
Basic Occupational Health Service Management in SJSN Era: Case Study at In-company Clinic PT X Indonesia.
DOI: 10.5220/0009950526862692
In Proceedings of the 1st International Conference on Recent Innovations (ICRI 2018), pages 2686-2692
ISBN: 978-989-758-458-9
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

there is some overlaps responsibility between MOL
and MOH in fostering the BOHS. Implementation of
SJSN will worsen this ambiguity.
Occupation Health Implementation Report 2013
from 26 provinces in Indonesia showed that about 3
million general disease cases and more than 4
hundred thousand health-related diseases cases at
workers. This information looks like Iceberg
Phenomenon, while many of non reported cases of
diseases. Jamsostek working injuries claim data
showed an increasing trend from 2010 to 2012. It is
elevated respectively from Rp 358.45 bio, Rp 401.2
bio, to Rp 504 bio. This condition led to the high
necessity of integrated BOHS with all disciplines,
not merely health and labour field, but also financing
and regulating.
In-company clinic PT X is a comprehensive
BOHS in cement big industries in Indonesia. These
OH services include prevention, curative, and
promotion & development services with the
multidisciplinary specialist team. From initial
discussion with the clinic manager, implementation
of SJSN influenced the financing of wellness cost
that company had double burden costing i.e. costing
for compulsory JKN insurance premium and costing
for OH clinic operation.
National health security (JKN) and Working
injuries security (JKK) as an inseparable part of
SJSN influenced the provision BOHS in Indonesia.
This research studied how the implementation of
SJSN led to In-company clinic adjusted their OH
service to their workers.
2 METHOD
This study arranged at In-company PT X, a leading
foreign capital company in the cement industry. This
company had operated health and safety
management according to OHSAS and provide
comprehensive basic occupational health services
include promotion, preventive, curative, and
rehabilitative program.
This research designed by a qualitative method
with data primary collected by in-depth interview
with selected informants from several institutions or
stakeholders who linked with OHS for workers, such
as an In-company clinic, BPJS Kesehatan, BPJS
Ketenagakerjaan, Ministry of Labour, Occupational
health physician association, and Workers
association. Informants selected based on criterion
and suitability, with purposive and snow-balling
sampling method. Data was managed by Miles and
Huberman method includes reducing, displaying,
and arranging a conclusion, supported by resources
and theoretical triangulation.
The variables were managed by the theoretical
framework of National Health System or SKN
including subsystem of Financing, Human resources,
Infrastructure, Supporting (People empowerment,
Information management, and Regulation), and
Health service program.
3 RESULTS
3.1 Health Service Program
PT X registered all of the workers in JKN program
under BPJS Kesehatan, but in “zero utility”
condition because the unexpected operating time of
service from health provider of BPJS Kesehatan,
meanwhile company kept using their existing
medical facility and program. The informant said
that this condition experienced by another company.
Fundamentally, the management of In-company
clinic welcomed to the implementation of SJSN, but
the service quality especially operating time service
has to improve. The loss of time due to waiting of
health service at health provider is a disadvantage
for the company (Informant-1).
Several companies in Indonesia suggested that
incompanion with BPJS Kesehatan will decrease
health service for the worker, i.e. the long queue of
service and time lose of work (Informant-2). Not of
all company objectionable to collaboration in health
service with BPJS Kesehatan (Informant-5).
There is miss-coordination between BPJS
Kesehatan and BPJS Ketenagakerjaan to provide
the promotive and preventive program. BPJS
Kesehatan provides this with the program for
general members of JKN such as Prolanis (chronic
disease program), early detection of cervical cancer,
etc. BPJS Ketenagakerjaan provides for workers
members of JKN such as safety riding training, SHE
training, the intervention of folic acid to reduce iron
deficiency anaemia. The follow up of this program
may provide by the ministry of health. (Informant 1,
4, and 5).
BPJS Kesehatan provided health promoting carry
forward PT Askes program that not yet based on
occupational risk. BPJS Ketenagakerjaan carries
forward PT Jamsostek program to provide health-
promoting based on occupational health thereby
medical check-up program confined to risk group
over 40 years and selected to the company who
obediently pay an insurance premium of working
injuries security. This program did not continue
Basic Occupational Health Service Management in SJSN Era: Case Study at In-company Clinic PT X Indonesia
2687

since JKN implemented by BPJS Kesehatan as an
operator. BPJS Kesehatan had the reasoning that
OHS is the responsibility of employers (Informant- 3
and 4).
OHS program needs to expanding with
comprehensive and maturity manner in respect of
SJSN. In a short time, this program will not cover all
of the workers. For the first effort, it is necessary to
imparting health awareness to the workers and
increasing the quality of health services. (Informant-
1 and 7)
3.2 Health Financing
PT X agreed that the health financing scheme for
workers from JKN and this sound has beneficiary
for the company. However, some aspects need to be
considered. First BPJS Kesehatan should select the
financed health service for workers because of the
number of industrial sector in Indonesia. Second, the
assessment of incentive premium of Working
Injuries Securities by decreasing of work-related
diseases or injury cases is not suitable and unfair,
because for this time many companies had still
concealed the cases (Informant-6). BPJS
Ketenagakerjaan will reward premium work injury
security incentive to the company who is decreasing
work injury in the form of declining premium grade.
The regulation that is administering this incentive
had been n drafted in the form of Presidential
Regulation. Insurance premium that grouping by
business will be changed by occupational risk
(Informant-4).
In order to decrease work injury and work-
related disease, the financing of OHS was expected
to cover by BPJS Ketenagakerjaan with the selected
mechanism as an additional beneficiary in Work
Injury Security (JKK). For workers who had
injuries, this financing program should accompany
with JKK-RTW (JKK Ready to Work). Meanwhile
for workers who had no injuries the finance
allocated to the education program. These efforts in
order to decrease work-related diseases and work
injury claim or financing of BPJS Ketenagakerjaan,
but not explicitly stipulated in existing OHS
regulation (Informant-1, 2, and 3). There is some
concern that plan of drafting a regulation that
directing to deflecting OHS financing and security
from employers to BPJS Kesehatan will be
increasing security premium. (Informant-2)
3.3 Human Resources
All of the health forces at PT X had suitable
competences and sufficient amount of human
resources, therefore, there is no significant effect
from the implementation of SJSN. Hiperkes
certificate had embed to all of the health forces at
OHS clinic PT X (Informant-1).
It is necessary to upgrade the competence of
primary healthcare physicians with occupational
health. This idea according to the condition that the
curriculum of a medical school does not yet adopt
occupational health disciplines, and the
responsibility of primary health care physician
including promotive and preventive care, not only
curative care. Some aspects that should be
considered is the upgrading of amount and
competence of OH advisor physician (from Ministry
of Labour) especially in determine of work-related
diseases diagnose, and in-depth understanding by
BPJS Kesehatan about occupational health
(informant-1,2, and 4). Twelve functions of
occupational health physician according to Ministry
of Labour regulation No.03 of 1982 remain adapted
at the in-company clinic (Informant-2).
3.4 Infrastructure
In-house clinic PT X did not accompany the clinic
infrastructure with BPJS Kesehatan (as a health
provider of JKN) because there is concern about the
rejection of the selection of local health provider that
closed to the residence if the workers had registered
as a patient at the in-company clinic (Informant-6).
Some of the company have the perception that if
the workers had registered as BPJS Kesehatan
member, all of the cost to provide health service
(promotive, preventive, curative, and rehabilitative)
covering by JKN premium. This condition led to the
decision that some company will close their clinic if
registered their workers on the JKN Program. The
consequence from this situation, there is an
unnecessity position of company physician. To fix
this problem, the association of occupational
physician will set up the occupational health service
form with the government (informant-1 and 2).
The decision to close in-company clinic would
be said contradict with Indonesia Law No.01 of
1970 about Work Safety, and this led to impairment
of occupational health service. Informant suggested
the company clinic to accompany with BPJS
Kesehatan. To alleviate the restriction to be health
provider, BPJS Kesehatan provides tolerance time
for the company to adapt their infrastructure with the
ICRI 2018 - International Conference Recent Innovation
2688

regulation (Informant-2 and 5). As we know that the
requirements of clinic according to the ministry of
health regulation are criterion for general health
facility, not for specifically for occupational health
(Informant-2).
According to the above situation, it needs to provide
public; occupational health service facility includes
the requirements. It is not sufficient for BPJS
Ketenagakerjaan to arrange network provider that
provision of occupational health service with Public
Health Centre (Puskesmas) and Public occupational
health centre (BKKM) only, it should be
accompanied with the in-company clinic (Informant-
1,2,3, and 4).
Others proposed OHS system if some in-
company clinic determined to close are expansion of
BKKM in many areas, separating the OHS program
with BPJS Kesehatan at curative and company
physician as OH consultant responsible to promotive
and preventive, or arrange the special registration
counter for workers at Puskesmas (Informant 1, 2, 3,
and 4).
3.5 Supporting
PT X still adapted the Ministry of Labour regulation
related to occupational health service and the
working memorandum between employer and
employee (PKB) as basic regulation in the provision
of health service. The regulation from the ministry
of health adapted incidentally if there is a program
from the district health office or Dinas Kesehatan,
such as immunization, surveillance, etc. For
supporting the OHS program, the Workers
Association has a significant role (Informant-6).
Indonesia government had drafted Presidential
Regulation about occupational health and Health
ministry regulation about Occupational Health
Program Station (Pos UKK). On the other side, there
is an effort from the government to harmonize the
stakeholders of OHS in Indonesia (Informant-1).
OHS information system should be improved to
precisely access information about work injury and
work-related disease. BPJS Ketenagakerjaan
proposed the innovation to improve the quality of
work-related disease data, i.e. reducing the step of
the fulfilment of claim documents, and extending the
access to informing work-related data not only by
employers but also involving workers and physician.
BPJS Ketenagakerjaan does not get a role in
reporting and finding the data of work-related
disease, but in setting the conclusion whether work-
related disease or not. The restriction in collecting
work-related disease data is the lack of basic data of
periodically health examination and pre-working
health examination. (Informant-4)
4 DISCUSSION
The urgency of OH promoting and preventing in
workplace stated by Healey and Walker (2009). The
workplace is the ideal place to improve a worker’s
health. Commonly workers take more than 40 hours
every week in the workplace and certainly getting a
role as the activist of health workers promoting.
Cost-benefit analysis of the outcomes of health
program such as chronic disease preventing program
show a significant financial result. In the beginning,
the cost of health is promoting and preventing sound
expensive, but it will make a high return if the
program is intensively implementing.
There is no uniformity of occupational health
promoting and preventing guidance in Indonesia. All
Indonesian company refer to three regulation or
guidance of OHS, i.e. Ministry of Labour regulation
No.80 of 1982, Ministry of health decree No.1758 of
2003, and Office clinic guidance from the ministry
of health. From this regulation, the researcher tries
to create a brief to provide OH promoting and
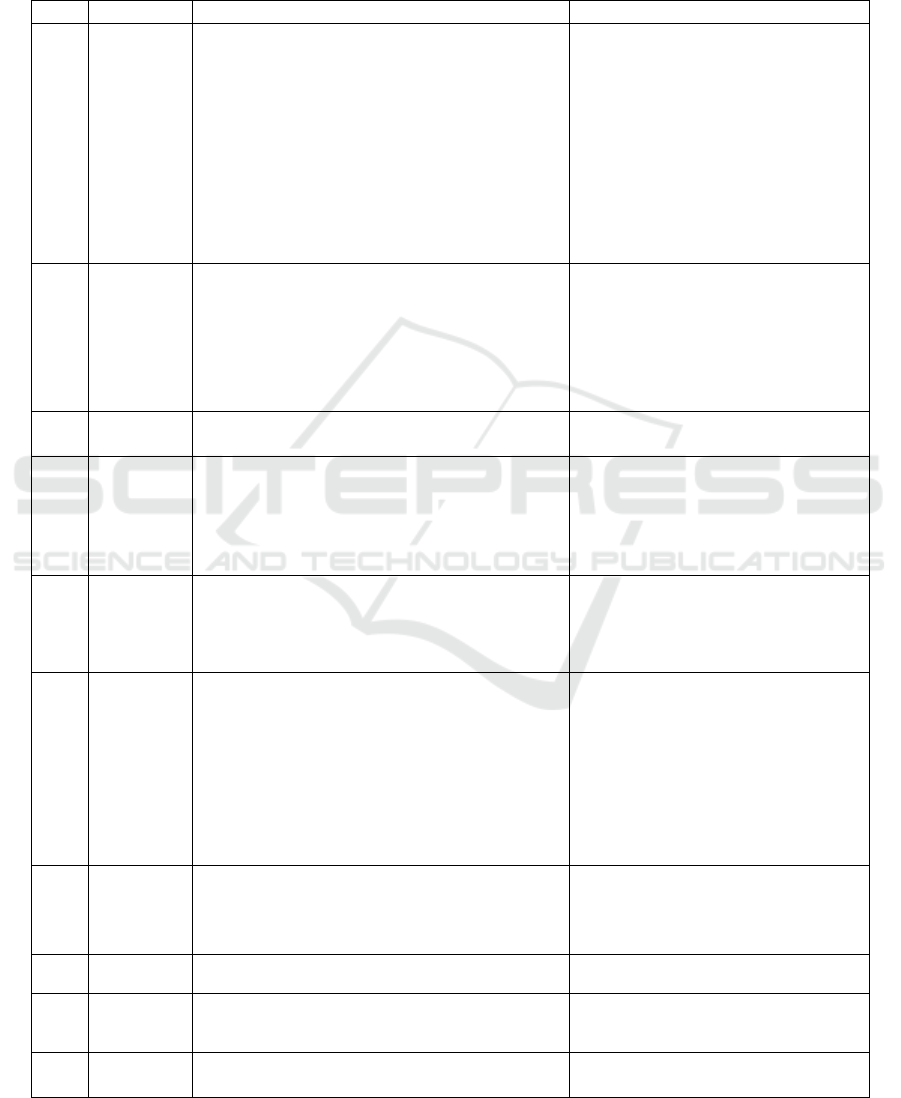
preventing, as shown in Table 1.
Security fund allocation for promoting and
preventing program had suitable to SJSN principles,
i.e. cooperation (Gotong Royong) and mandatory
fund (Dana Amanat). Cooperation implemented by
the big companies that capable to provide own OHS
shall aid the small enterprise that incapable to
manage OHS. Mandatory fund implemented by
investing fund collected from BPJS members
utilized to themselves health service. However, there
is an Accountability principle, so, therefore, the
security fund is not allocated to all promoting and
preventing program. In other words, employers
should take responsibility to fund the OHS at the
workplace. How should this OHS financing
collaboration undertake? According to Table 2, we
recommend finance resources to provide promoting
and preventing program at the company.
5 CONCLUSION
OHS provision at in-company clinic PT X after the
implementing of SJSN not yet affect to the aspects
of OH program, financing, human resources,
infrastructure, and supporting matters. In-company
clinic PT X had registered all of the workers to the
Basic Occupational Health Service Management in SJSN Era: Case Study at In-company Clinic PT X Indonesia
2689

social security program, but particularly in health
security (JKN) still in “no utilize” position. PT X
had been waiting and assessing BPJS health service
quality development in order to make the beneficiary
for the company.
SJSN implementation would affect OH program
particularly in OH promoting and preventing
program, and OH financing that sourcing from BPJS
premium. Focus to promoting and preventing
program led to the recalculate the requirement of
human resources and infrastructure. On the other
side, it needs to improve supporting aspects such as
information management, regulation, and people
empowerment. From this study we recommend:
a. Identifying the uniformity of promoting and
preventing program at the in-company clinic
based on existing regulation (as shown in Table
1)
b. Identifying the alternative sources of OHS
financing after SJSN implements (as shown in
Table 2)
ACKNOWLEDGMENT
This study supervised by Prof. Amal Chalik Sjaaf,
SKM, DrPH from Health Administration and Policy
Faculty of Public Health Universitas Indonesia.
REFERENCES
Dewan Jaminan Sosial Nasional. (2014). Ringkasan
Peta Jalan Penyelenggaraan Jaminan Soial
Bidang Ketenagakerjaan 2014-2019. Jakarta:
DJSN.
DITJEN Bina Kesehatan Masyarakat Depkes RI.
(2007). Pedoman Klinik di Tempat Kerja
Perusahaan. Jakarta: Depkes RI.
Healey, B. J., and Walker, K. T. (2009). Introduction to
Occupational Health in Public Health Practice. New
Jersey: John Willey and Sons.
Rantanen, J. (2005). Basic Occupational Health Service –
their Structure, Content, and Objectives. SJWEH
Supplements 2005 No.1
Republik Indonesia. (1992). Undang-Undang No.03 tahun
1992 tentang Jaminan Sosial Tenaga Kerja
Republik Indonesia. (2004). Undang-Undang No.40 tahun
2004 tentang Sistem Jaminan Sosial Nasional
Republik Indonesia. (2009). Undang-Undang No.36 tahun
2009 tentang Kesehatan
Republik Indonesia. (2011). Undang-Undang No.24 tahun
2011 tentang Badan Pengelola Jaminan Sosial
Republik Indonesia. (2013). Peraturan Pemerintah No.12
tahun 2013 tentang Jaminan Kesehatan
Republik Indonesia. (2012). Peraturan Presiden Nomor
72 tahun 2012 tentang Sistem Kesehatan Nasional
Republik Indonesia. (2013). Peraturan Menteri Kesehatan
Nomor 71 tahun 2013 tentang Pelayanan Kesehatan
pada Jaminan Kesehatan Nasional
Republik Indonesia (1980). Peraturan Menteri Tenaga
Kerja dan Transmigrasi Nomor 02/Men/1980 tentang
Pemeriksaan Kesehatan Tenaga Kerja dalam
Penyelenggaraan Keselamatan Kerja
Republik Indonesia (1980). Peraturan Menteri Tenaga
Kerja dan Transmigrasi Nomor 03/Men/1982 tentang
Pelayanan Kesehatan Kerja
Republik Indonesia (2003). Keputusan Menteri Kesehatan
No.1758/SK/XII/2003 tentang Standar Pelayanan
Kesehatan Kerja Dasar
Republik Indonesia. (2004). Keputusan Menteri
Kesehatan No.128/SK/II/2004 tentang Kebijakan
Dasar Pusat Kesehatan Masyarakat
Republik Indonesia (2012). Keputusan Menteri Tenaga
Kerja dan Transmigrasi Nomor 609 tahun 2012
tentang Pedoman Penyelesaian Kasus Kecelakaan
Kerja dan Penyakit Akibat Kerja
Republik Indonesia. (2008). Keputusan Ditjen Bina
Pengawas Ketenagakerjaan Kemenakertrans Nomor
22D tahun 2008 tentang Petunjuk Teknis
Penyelenggaraan Pelayanan Kesehatan Kerja
ICRI 2018 - International Conference Recent Innovation
2690
APPENDIX
Table 1: The Briefs of OH Promoting and Preventing based on Indonesia OHS Regulation
No.
Object
OH Promoting
OH Preventing
1
Workers
- Work adjust to workers fostering and controlling
- Workers health education (ie: workplace personal
hygiene)
- Health consultation (i.e work psychology, family
planning and others)
- Workers counseling (i.e Operating procedure,
occupation risk preventing, personal hygiene,
protecting equipment, nutrition, etc)
- Health promoting to reducing general disease, work-
related disease, and work injury
- Emergency training according to location,
procedure, and production process
- Sport and exercise
- Health workers surveillance
- Pre-working health exam
- Periodically health exam
- Back to work health exam
- General health exam
- Retirement or pre retirement health
examination
2
Employer
- Employer counseling (i.e Operating procedure,
occupation risk preventing, personal hygiene,
protecting equipment, nutrition, etc)
- Feedback for the regulation of OH
- Health promoting to reducing general disease, work-
related disease, and work injury
- Risk informing and educating, also advising about
risk preventing and controlling plan
3
Working
process
- Identifying the type of jobs for inventing potential
risk and hazard
4
Work-
related
disease and
Work injury
- General disease and work-related
disease preventing
- Dominant general disease, Work-related
disease, and Work injury surveillance
- Work injury preventing
5
Occupationa
l risk and
harzard
- Potential risk identification, assessment, evaluating,
and controlling
- Health and safety risk assessment
- Health & satety risk and hazard
management and controlling
- Work environment or workplace
monitoring
6
Work
environment
- Work environment fostering and controlling
- Workplace planning and designing advice
- Industrial sanitation consultation
- Workplace potential risk identified and asssessment
- Healthy workplace, work process and work
environment maintenance
- Sanitary equipment fostering and controlling
- Work environment improvement
facilitating or recommending (i.e
ventilation, liquid waste treatment,
ergonomic improvement, etc)
- Work environment hazard improvement
(physic, chemist, biology, psychosocial,
ergonomic)
- Occupation Health surveillance, work
environment monitoring, and biological
monitoring)
7
Occupationa
l or
Working
nutrition
- Nutrition and workplace food management advising
- Good house-keeping practice
- Occupational nutrition improvement, diet balance &
healthy food maintenance, and cafetaria hygiene
- Inspection of water quality and hygienist
food and or food handler
8
OH officer
- Emergency training based on location, working
procedure, and production process
9
OH
equipment
- OH equipment fostering and controlling
- Required protecting equipment selecting advice
- Protecting equipment sample
procurement and application
10
OH
Procedure
- OH planning orientation
- Emergency response procedure and
disaster management
Basic Occupational Health Service Management in SJSN Era: Case Study at In-company Clinic PT X Indonesia
2691
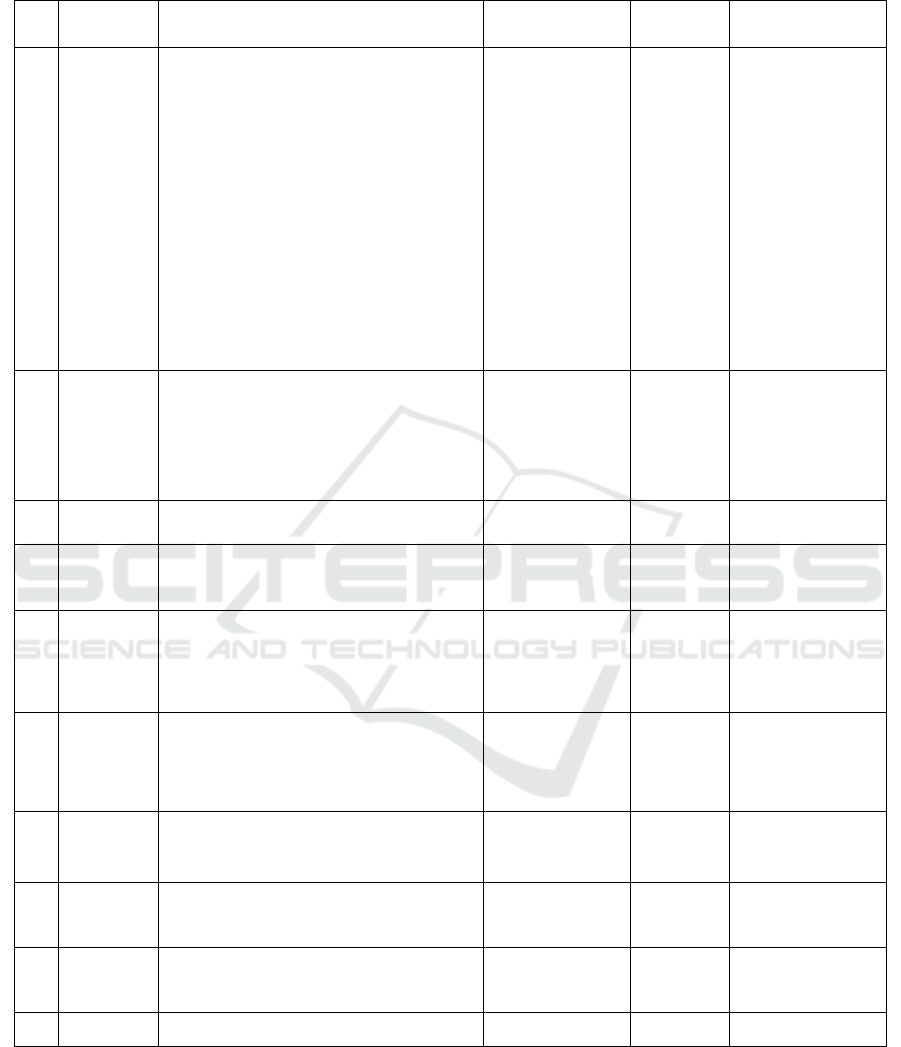
Table 2: Recommendation of OHS Promoting and Preventing Activity at In-company Clinic include frequency, unit cost,
and financing
No
Object
Promoting or Preventing Program
Frequent
Unit Cost
for every
Source of Financing
1
Workers
- Working adjust to workers fostering and
controlling
- Workers health education (ie: workplace personal
hygiene)
- Health consultation (i.e work psychology, family
planning and others)
- Emergency training according to location,
procedure, and production process
- Workers counseling (i.e Operating procedure,
occupation risk preventing, personal hygiene,
protecting equipment, nutrition, etc)
- Health promoting to reducing general disease,
work-related disease, and work injury
- Sport and exercise
- Health workers surveillance
- Pre-working health exam
- Periodically health exam
- Back to work health exam
- General health exam
- Retirement or pre retirement health examination
- Every year
- Every year
- Every year (after
periodically health
exam.)
- Every year
- Based on required
- Based on required
- Every week
- Based on required
- Based on required
- Every year
- Based on required
- Based on required
- Based on required
- In-
company
clinic
- In-
company
clinic
- Day
- In-
company
clinic
- Session
- Session
- Session
- Session
- Worker
- Worker
- Worker
- Worker
- Worker
- BPJS
Ketenagakerjaan
- BPJS
Ketenagakerjaan
- Employers
- BPJS
Ketenagakerjaan
- Employers
- BPJS
Ketenagakerjaan
- Employers
- Employers
- Workers
- Employers
- Employers
- Employers
- Employers
2
Employers
- Employer counseling (i.e Operating procedure,
occupation risk preventing, personal hygiene,
protecting equipment, nutrition, etc) and Feedback
for the regulation of OHS
- Health promoting to reducing general disease, work-
related disease, and work injury and Risk informing
and educating, also advising about risk preventing
and controlling plan
- Every 2 years
- Every 2 years
- Session for
several
company
- Session for
several
company
- BPJS Ketenagakerjaan
- BPJS Ketenagakerjaan
3
Working
process
- Identifying the type of jobs for inventing potential
risk and hazard
- Every year
- Company
- BPJS
Ketenagakerjaan
4
Work-
related
disease and
work injury
- Predominant general disease, Work-related disease,
and Work injury surveillance
- Based on required
- Case of
disease
- Employers
5
Occupationa
l risk and
hazard
- Potential risk identification, assessment, evaluating,
and controlling
- Health and safety risk assessment
- Health & satety risk and hazard management and
controlling
- Work environment or workplace monitoring
- Based on required
- Based on required
- Based on required
- Based on required
- Case by case
- Case by case
- Case by case
- Case by case
- Employers
- Employers
- Employers
- Employers
6
Work
environment
- Healthy workplace, work process and work
environment maintenance and consultation
- Industrial sanitation consultation
- Workplace potential risk identified and asssessment
- Occupation Health surveillance, work environment
monitoring, and biological monitoring)
- Every year
- Every year
- Every year
- Every year
- Company
- Company
- Company
- Company
- BPJS Ketenagakerjaan
- BPJS Ketenagakerjaan
- BPJS Ketenagakerjaan
- BPJS Ketenagakerjaan
7
Occupationa
l nutrition
and food
- Nutrition and workplace food management advising
- Good house-keeping practice consultation
- Inspection of water quality and hygienist food and
or food handler
- Every year
- Every year
- Every year
- Company
- Company
- Company
- Employers
- Employers
- Employers
8
OH Officer
- Emergency training based on location, working
procedure, and production process
- OH training
- Every year
- Every year
- Officer
- Officer
- BPJS
Ketenagakerjaan
- BPJS
Ketenagakerjaan
9
OH
equipments
- OH equipment fostering and controlling
- Required protecting equipment selecting advice
- Once after BPJS
registered
- Once after BPJS
registered
- Company
- Company
- BPJS
Ketenagakerjaan
- BPJS
Ketenagakerjaan
10
OH
procedure
- OH planning orientation concultation
- Once after BPJS
registered
- Company
- BPJS
Ketenagakerjaan
ICRI 2018 - International Conference Recent Innovation
2692
