
Effect of Timing of First Postnatal Check on Neonatal Death in
Indonesia: Analysis of IDHS 2002-2003, 2007, and 2012 with
Retrospective Cohort Study
Ira Marti Ayu
1
, Asri Adisasmita
2
, Decy Situngkir
1
and Ratna Djuwita
2
1
Departement of Public Health, Faculty of Health Sciences, Universitas Esa Unggul
2
Department of Epidemiology, Faculty of Public Health, University of Indonesia
Keywords: Neonatal death; Postnatal, Survival, Cohort Study
Abstract: Many of under-five death occurs during the neonatal period. The first week of life after birth, especially the
first day of life is the most vulnerable time for child survival. Neonatal period accounts for more than one
third (over 44%) in under five death. In Indonesia, Neonatal Mortality Rate in 2012 is 19 per 1000 livebirth.
One of the intervention to increasing of neonatal survival is by the timing of first postnatal check-up but from
the previous study showed inconsistent effect. The objective of this study was to identifythe effect timing of
the first postnatal check-up for the newborn on neonatal survival. This study used the data from 2002-2003,
2007, and 2012 IDHS. The design of this study was a retrospective cohort study and assessed the association
of factors related to neonatal death used survival analysis by Cox regression.A total of 35.985 live birth
singleton in IDHS 2002-2003, 2007 and 2012 were analyzed. Multivariate analysis showed that Babies who
received a first postnatal check-up by health professional ≥24 hours up to 7 days after birth has a significant
protective effect on neonatal death (HR=0,09;95%CI: 0,04-0,23). The study also found other finding that birth
weight (HR=13,23; 95%:5,47-32,04)and pregnancy complication (HR=1,66; 95%CI: 1,17-2,36) were
significant associated with neonatal death.In order to get the more accurate timing of first postnatal check-up,
it recommended observing the timing of postnatal check-up directly.
1 INTRODUCTION
One of dimension Human Development Index is long
and healthy life (Badan Pusat Statistik, 2018).
Globally life expectancy at birth in 2013 is 70,8. It
means every child was born in 2013 will survive until
70-71 years(UNDP, 2014). 138 million children born
every year in 2013, but many of them did not survive
like life expectancy estimation. Even over 6,3 million
die before their fifth birthday(UNICEF, WHO, World
Bank, and UN Population Division, 2014).
Many of under-five death occurs during the
neonatal period. Neonatal period (first 28 days after
birth) is the most vulnerable time for child survival
(UNICEF, WHO, World Bank, and UN Population
Division, 2014). Neonatal period account more than
one third (over 44%) in under five death (UNICEF,
2014), two third in child mortality (Mathews et al.,
2000), and three-quarters neonatal death occur in the
first week of life (Lawn et al., 2005). In Jimma zone,
Southwest Ethiopia, Neonatal Mortality Rate was
35,5 per 1000 live birth, and 69,1% die at the first
week of life(Debelew et al., 2014). It showed that it
needs the high-quality care of childbirth(Lawn et al.,
2014).
In Indonesia, Neonatal Mortality Rate in 2012 is
19 per 1000 livebirth(BKKBN et al., 2013). Between
1997-2002, 54,7% infant death occurred in the
neonatal period and it estimates 29,9% occurred in the
first day of life dan 75,6% in the first week of life
(Titaley et al., 2008).
Increasing of neonatal survival can be done by
preventing the cause of death. Many of cause of
neonatal death is preventable with low cost and low-
level technology (Lawn et al., 2005;Darmstadt et al.,
2005)so that it can be implemented in low and
middle-income countries like Indonesia. One of
intervention to improve neonatal survival is postnatal
check for a newborn. WHO recommendation on
timing first postnatal check-up is at least 24 hours
after birth in a health facility and as early as possible
within 24 hours after birth at home(WHO, 2014a).
First postnatal check-up must be done as early as
2680
Marti Ayu, I., Adisasmita, A., Situngkir, D. and Djuwita, R.
Effect of Timing of First Postnatal Check on Neonatal Death in Indonesia: Analysis of IDHS 2002-2003, 2007, and 2012 with Retrospective Cohort Study.
DOI: 10.5220/0009950326802685
In Proceedings of the 1st International Conference on Recent Innovations (ICRI 2018), pages 2680-2685
ISBN: 978-989-758-458-9
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

possible so professional birth attendant can promote
healthy behavior likes exclusive breastfeeding, early
detection and referral of complication, pneumonia
case management and hypothermia prevention
management including kangaroo mother care for low
birth weight baby (Kerber et al., 2007;Darmstadt et
al., 2005).
The first postnatal checkup is cost-effective and
cost-efficient intervention so it can be used in low and
middle-incomecountries. However, the first postnatal
check-up within two days after birth is only 48%
(WHO, 2014b). In India, only 48,3% newborn
received a first postnatal check-up within 24 hours
after birth (Singh et al., 2012). While in Indonesia in
2012 only 40,5% newborn receive their first postnatal
check-up at less than 24 hours after birth (BKKBN et
al., 2013). It shows that the intervention coverage still
low, whereas this intervention was implemented with
high coverage (99%), it can save the life of newborn
over 41%-72% (Darmstadt et al., 2005).
Effect of timing postnatal check up on neonatal
death has variation result. The previous study by
Baqui et al. show that the risk of neonatal mortality
had a protective effect 0,33 times compared with
newborn did not first receive a postnatalcheck-
up(Baqui et al., 2009). However,Titaley and Dibley
study in Indonesia found that postnatal care is not
related to newborn survival (Titaley and Dibley,
2012). Singla et al. study in India also found that there
was no significant difference in neonatal mortality
among infant received first postnatal check-up within
24 hours compared to infant did not receive a first
postnatal check-up within 24 hours after birth (Singh
et al., 2012).
In Indonesia, neonatal death is still a problem.
Prevention of neonatal death can be done by applying
postnatal check-upas early as possible after birth.A
postnatalcheck-up is used to detect any illness of
danger sign for the baby after birth, so the treatment
can be done as early as possible to prevent death.A
postnatalcheck-up is a cost-effective and cost-
efficient intervention with low cost and low-
leveltechnology so that it can be implemented in a
developing country likes Indonesia. However, there
is inconsistent result about effect timing of first
postnatal on neonatal death, so a study needs to be
done to know the effect of timing first postnatal
check-up in neonatal death.
2 RESEARCH METHOD
This study used secondary data of Indonesia
Demographic and Health Survey (IDHS) in 2002-
2003, 2007, and 2012. This study used a retrospective
cohort study. The subject of this study was women in
reproductive age (15-49 years) and used household
and women questionnaires. IDHS used multi-stage
sampling such as cluster sampling, stratified
sampling, systematic sampling, until simple random
sampling (SRS). First, the sampleis clustered by
choosing provinces in Indonesia. Second, every
province is stratified by rural and urban area,and
every level of stratum has census blocks (CB). In
urban are, CBis chosen by systematic
sampling,andevery CB is chosen 25 households
randomly. In a rural area, there arethreestages to
choose a household sample. First, choosing sub-
district with Probability Proportional to Size (PPS) of
the household. Second, every selected sub-district
take CB by systematic sampling, and every CB is
chosen 25 households randomly
Time to event was the dependent variable, timing
of first postnatal check-up as the independent
variable. The timing of first postnatal check-up is
categorized as received a first postnatal check-up by
health professional <24 hours after birth, received a
first postnatal check-up by health professional ≥24
hours up to 7 days after birth and did not receive first
postnatal check-up or receive postnatal checkup >7
days. This study also considers about potential
confounding factor, such as type residence, maternal
education, maternal age delivery, parity, household
wealth index, desire for pregnancy, delivery
complication, birth weight, antenatal care services,
mode of delivery, place of delivery, delivery
attendant. The data were analyzed with survival
analysis with Cox regression test and analysis using
SPSS and complex sample. This study also presented
probability survival with KaplanMeier curve.
3 RESULTS
There was 35985 live birth singleton infant, of which
353 (0,1%) babies die in the neonatal period. Based on
the data there was an increasing probability of
neonatal survival from IDHS 2022-2003 (98,5%),
IDHS 2007 (98,8%) and IDHS 2012 (98,9%) and
probability survival overall (99,0%) (Figure 1).
Effect of Timing of First Postnatal Check on Neonatal Death in Indonesia: Analysis of IDHS 2002-2003, 2007, and 2012 with Retrospective
Cohort Study
2681
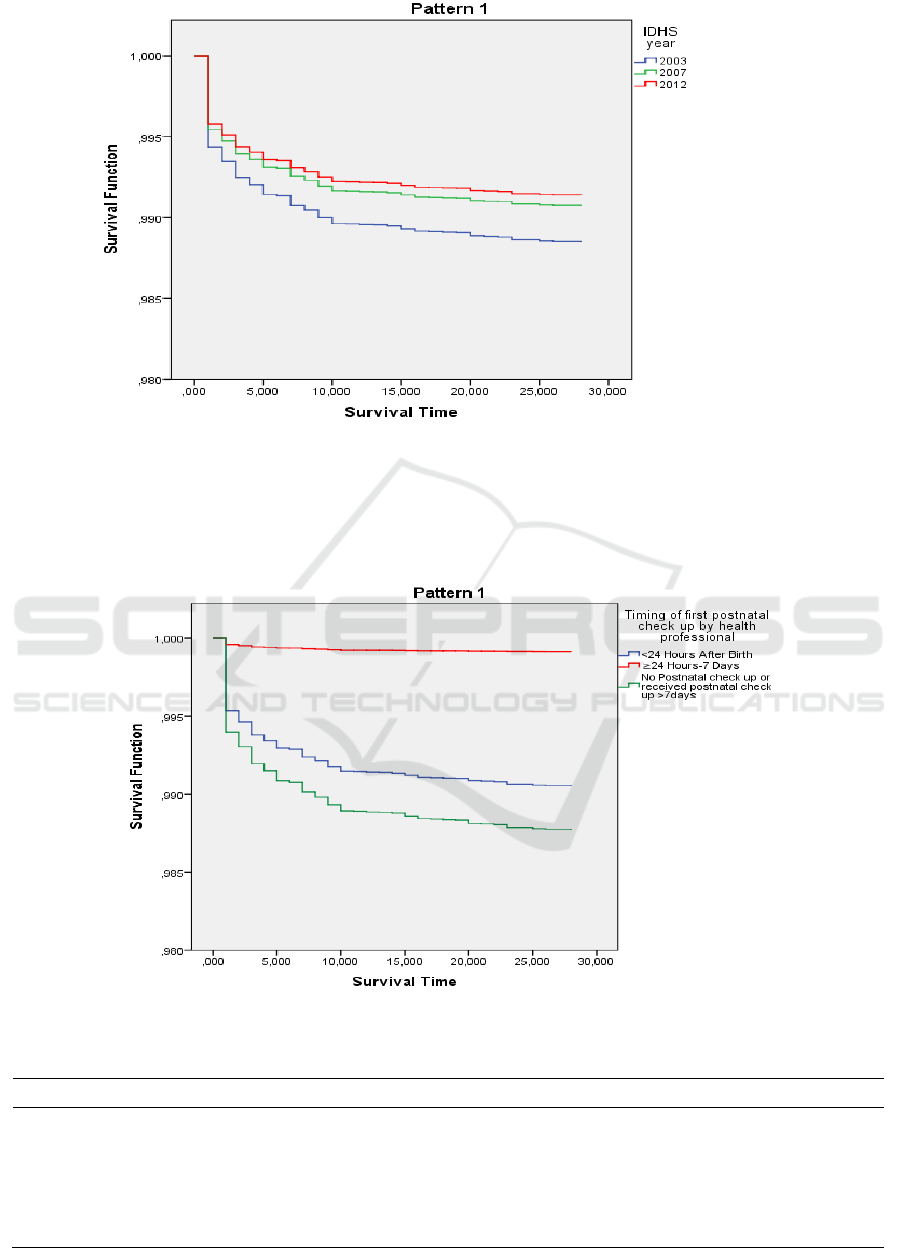
Figure 1: Neonatal survival probability curve based on IDHS
The probability of neonatal survival based on the
timing of postnatal check-up is highest in babies who
received first postnatal check-up by health
professional ≥ 24 hours up to 7 days after birth
(99,1%). Moreover, the lowest probability is in babies
who did not receive a first postnatal check-up or
receive a postnatalcheck-up but >7 days after birth
(Figure 2).
Figure 2: Neonatal survival probability curve based on timing first postnatal check up
Table 1: Bivariate and multivariate analysis
Variable HR Crude HR Adjusted
Timing Of First Postnatal Check Up (By Health
Professional)
<24 Hours After Birth 1(Reference)
≥24 Hours-7 Days 0,09 (0,04-0,23)*
0,09 (0,04-0,23)*
No Postnatal check up Or received postnatal
check up>7days
1,30 (0,95-1,77)**
1,004 (0,64-1,58)
ICRI 2018 - International Conference Recent Innovation
2682

Table 1: Bivariate and multivariate analysis (cont.).
Variable HR Crude HR Adjusted
Birth Weight
≥2500 1(Reference)
<2500 8,29 (5,55-12,38)* 13,23(5,47-32,04)*
Not Weighted 3,58 (2,46-5,21)* 4,17(2,32-7,521)*
Don’t Know 14,25(5,91-34,31)* 8,06(5,42-11,99)*
Maternal Age Of Delivery
12-19 1(Reference)
20-35 1,17 (0,70-1,95)
>35 1,91 (1,25-2,91)*
Parity
Primiparous 1(Reference)
Multiparrous 0,96 (0,67-1,38)
Grandmultiparous 2,02 (1,26-3,22)*
Desire For Pregnancy
Wanted Then 1(Reference)
Wanted No More 1,23 (0,79-1,89)
Dont Know 2,130E-009(,083E-009-4,188E-009)*
Antenatal Care (ANC) Visit
≥4 And According To Standard 1(Reference)
< 4 1,69 (1,21-2,38)*
No ANC 3,40 (1,84-6,28)*
Don’t Know 0,89 (0,33-2,42)
Pregnancy Complication
No 1(Reference) 1
Yes 2,65 (1,85-3,80)* 1,66 (1,17-2,36)*
Dont Know 2,074E-009 (9,423E-010-4,564E-
009)*
1,83 (0,99-3,39)*
Delivery Attendant
Health Professional 1(Reference) 1
TBA/ Others 1,32 (0,93-1,87)** 0,61 (0,31-1,22)
Don’t Know 2,205E-009 (5,894E-010-8,248E-
009)*
2,566E-009
(6,002E-010-
1,098E-008)
Place Of Delivery
Hospital 1(Reference)
Other Health Facility 0,33 (0,21-0,54)*
Home 0,65 (0,44-0,97)*
Dont Know 1,82 (0,20-14,46)
Mode Of Delivery
Non-Caesarean Section 1(Reference)
Caesarean Section 1,62 (0,95-2,77)**
Don’t Know 0,13 (0,02-0,92)*
Delivery Complication
No 1(Reference)
Yes 1,72 (1,21-2,45)*
Don’t Know 3,63 (2,09-6,28)*
Maternal Education
Higher Education Level 1(Reference) 1
Lower Education Level 1,98 (1,16-3,37)* 1.51 (0,85-2,68)
Type Of Residence
Urban 1(Reference)
Rural 1,14 (0,84-1,56)
Wealth Status
Rich (Q4-Q5) 1(Reference)
Poor (Q1-Q3) 1,26 (0,89-1,78)**
* p value <0,05
**p-value <0,025
Effect of Timing of First Postnatal Check on Neonatal Death in Indonesia: Analysis of IDHS 2002-2003, 2007, and 2012 with Retrospective
Cohort Study
2683

According to Table 1, the Multivariate analysis
showed that birth weight and delivery and pregnancy
complication were significantly associated with
neonatal death. Babies who received first postnatal
check-up by health professional ≥24 hours up to 7
days after birth has a significant protective effect on
neonatal death.
4 DISCUSSION
There was 353 neonatal death, of which 283 (80,2%)
occur in the early neonatal period (first week of life)
and 173 (49,0%) in the first day of life. It means most
of the neonatal death occurred in the first week (early
neonatal period) and especially on the first day of
life(Oza et al., 2014). There was an improvement of
neonatal survival from IDHS 2002-2003, 2007 and
2012. This due to an effort to improve maternal and
child health like a continuum of care services.
Continuum of care is integrated service delivery for
mother and children from pre-pregnancy to delivery,
the immediate postnatal period and childhood(WHO,
2011). Pregnancy health service cannotbe separated
with delivery, postnatal period and newborn health
services. Quality of antenatal care services will affect
maternal and fetus during pregnancy, and for baby and
maternal after delivery (Kemenkes RI, 2010).
This study found that pregnancy complication and
birth weight have significant associated with neonatal
death. In developing countries, more than 9 million
babies die every year before birth and during the first
week of life due to a complication during delivery
(Yego et al., 2013). Pregnant women from developing
countries are 36 times more likely suffer a
pregnancycomplication than pregnant women in
developed countries (WHO, 2015). Severe
hypertension, anemia, postpartum hemorrhage,
puerperal fever, abruptio placentae, diabetes mellitus,
are pregnancy complication (Nwankwo et al., 2013).
Birth weight is the weight of baby which weighed
within an hour after birth (Muslihatun, 2010). In
developing countries, almost half (48,7%) of babies
born not weighed and from those who weight only
14% were born with low birth weight (Blanc and
Wardlaw, 2005). According to WHO, babies born
with low birth weight are caused by preterm birth or
small gestational age (SGA) or both (World Health
Organization and others, 2011). The incidence rate of
neonatal mortality with low birth weight is six times
higher than for neonatal mortality with normal weight
(Incidence Rate Ratio=6,4) (Slyker et al., 2014). A
case-control study at the Hawasa University Hospital
showed that baby with very low birth weight, and low
birth weight was 3,95 times increased risk of early
neonatal death than normal weight (Bayou and
Berhan, 2012).
After controlling covariate variables, there was no
associated between babies who did not receive a first
postnatal check-up or receive postnatal checkup >7
days with neonatal survival. The adjusted Hazard ratio
on babies who received postnatal check-up by health
professional ≥24 hours up to 7 days after birth has a
significant protective effect on neonatal death
(HR=0,0995%CI: 0,04-0,23)
The result of this study indicates that babies who
receive postnatal check-up by health professional < 24
hours after birth did not prevent neonatal death
compared with babies who receive a postnatalcheck-
up ≥24 hours-7 days. It was contrary with the study
Baqui et al. (2009) and Singh et al. (2014). Babies who
did not check up were 3,03 times (95%CI;0,23-0,46)
more likely to die than babies who checked up in the
first day of life (Baqui et al., 2009). Also, babies who
checked up in the first week by a health professional
or not were associated with the decline of neonatal
mortality (OR: 0,51; 95%CI: 0,35-0,75; OR 0,34;
95%CI 0,30-0,38) (Singh et al., 2014).
The result of this can not prove that babies who
receive first postnatal check-up by health professional
≥24 hours have a protectiveeffect on neonatal death.
This is contrary to the objective of this study. The
babies who received checked than ≥24 hours can
influence babies’ life because it cannot detect any
illness of danger sign as early as possible. It is because
there is a limitation of the secondary data. First, when
we used secondary data, we cannot control the quality
of collection data, and there is missing data. Second,
there is a recall bias because the respondentwas asked
about something that happens5 years ago. Mother who
asked about the timing of first postnatal check-up can
not remind the timing exactly. For further study
The study also found others finding that birth
weight, and pregnancy complication can prevent
neonatal death. So to improve neonatal survival, it
needs to prevent risk factors of low birth weight
during pregnancy and also prevent pregnancy
complication through adequate antenatal care.
5 CONCLUSION
The result of this study is babies who receive first
postnatal check-up by health professional longer than
≥24 hours has a protectiveeffect on neonatal death
because of the limitation of secondary data. It
isrecommendedfor further studyto observe the timing
ICRI 2018 - International Conference Recent Innovation
2684

of postnatal check-up directly, so the result is more
accurate.
REFERENCES
Badan Pusat Statistik(2018). Badan Pusat Statistik [WWW
Document]. Available at:
https://www.bps.go.id/subject/26/indeks-
Pembangunan-manusia.html (accessed 7.11.18).
Baqui, A.H., Ahmed, S., Arifeen, S.E., Darmstadt, G.L.,
Rosecrans, A.M., Mannan, I., Rahman, S.M., Begum,
N., Mahmud, A., Seraji, H.R., and others.(2009). Effect
of timing of first postnatal care home visit on neonatal
mortality in Bangladesh: an observational cohort
study. BMJ 339.
Bayou, G., and Berhan, Y.(2012). Perinatal mortality and
associated risk factors: a case-control study. Ethiopian
journal of health sciences, 22(3).
BKKBN, BPS, Kemenkes RI, ICF International.(2013).
Survei Demografi dan Kesehatan Indonesia tahun
2012. Jakarta, Indonesia : BKKBN, BPS, Kemendkes
RI, ICF International.
Blanc, A. K., and Wardlaw, T. (2005). Monitoring low birth
weight: an evaluation of international estimates and an
updated estimation procedure. Bulletin of the World
Health Organization, 83: 178-185d.
Darmstadt, G. L., Bhutta, Z. A., Cousens, S., Adam, T.,
Walker, N., De Bernis, L., and Lancet Neonatal
Survival Steering Team. (2005). Evidence-based, cost-
effective interventions: how many newborn babies can
we save?. The Lancet, 365(9463): 977-988.
Debelew, G. T., Afework, M. F., and Yalew, A. W. (2014).
Determinants and causes of neonatal mortality in
Jimma zone, southwest Ethiopia: a multilevel analysis
of prospective follow up study. PLoS One, 9(9):
e107184.
Kemenkes RI.(2010). Pedoman Pelayanan Antenatal
Terpadu. Jakarta: Direktorat Jenderal Bina Kesehatan
Masyarakat.
Kerber, K.J., de Graft-Johnson, J.E., Bhutta, Z.A., Okong,
P., Starrs, A., and Lawn, J.E.(2007). Continuum of care
for maternal, newborn, and child health: from a slogan
to service delivery. The Lancet, 370: 1358–1369.
Lawn, J. E., Blencowe, H., Oza, S., You, D., Lee, A. C.,
Waiswa, P., ... and Mathers, C. (2014). Every Newborn:
progress, priorities, and potential beyond survival. The
Lancet, 384(9938): 189-205.
Lawn, J. E., Cousens, S., Zupan, J., and Lancet Neonatal
Survival Steering Team. (2005). 4 million neonatal
deaths: when? Where? Why? The Lancet, 365(9462):
891-900.
Mathews, T. J., Curtin, S. C., and MacDorman, M. F.
(2000). Infant mortality statistics from the 1998 period
linked birth/infant death data set. National vital
statistics reports, 48(12): 1-125.
Muslihatun, W.N. (2010). Asuhan neonatus bayi dan
balita. Fitramaya, Yogyakarta.
Nwankwo, T. O., Aniebue, U. U., Ezenkwele, E., and
Nwafor, M. I. (2013). Pregnancy outcome and factors
affecting vaginal delivery of twins at University of
Nigeria Teaching Hospital, Enugu. Nigerian journal of
clinical practice, 16(4).
Oza, S., Cousens, S. N., and Lawn, J. E. (2014). Estimation
of daily risk of neonatal death, including the day of birth,
in 186 countries in 2013: a vital-registration and
modeling-based study. The Lancet Global Health,
2(11): e635-e644.
Singh, A., Yadav, A., and Singh, A. (2012). Utilization of
postnatal care for newborns and its association with
neonatal mortality in India: an analytical appraisal. BMC
pregnancy and childbirth, 12(1): 33.
Singh, K., Brodish, P., and Haney, E. (2014). Postnatal care
by provider type and neonatal death in sub-Saharan
Africa: a multilevel analysis. BMC public health, 14(1):
941.
Slyker, J. A., Patterson, J., Ambler, G., Richardson, B. A.,
Maleche-Obimbo, E., Bosire, R., ... and John-Stewart,
G. (2014). Correlates and outcomes of preterm birth,
low birth weight, and small for gestational age in HIV-
exposed uninfected infants. BMC pregnancy and
childbirth, 14(1): 7.
Titaley, C. R., Dibley, M. J., Agho, K., Roberts, C. L., and
Hall, J. (2008). Determinants of neonatal mortality in
Indonesia. BMC public health, 8(1): 232.
Titaley, C. R., and Dibley, M. J. (2012). Antenatal iron/folic
acid supplements, but not postnatal care, prevent
neonatal deaths in Indonesia: analysis of Indonesia
Demographic and Health Surveys 2002/2003–2007 (a
retrospective cohort study). BMJ Open, 2(6): e001399.
UNDP.(2014). Human development report 2014: Sustaining
human progress: Reducing vulnerabilities and building
resilience. United Nations Development Programme,
New York.
UNICEF.(2014). Committing to Child Survival : A Promise
Renewed. United Nations Children’s Fund, New York.
UNICEF, WHO, World Bank, and UN Population
Division.(2014). Levels and Trends in Child Mortality
2014. New York, USA : UNICEF, WHO, World Bank,
& UN Population Division.
WHO.(2015). Pregnancy-related complications [WWW
Document]. WHO. Available at: http://www.who.int/
surgery/challenges/esc_pregnancycomp/en/ (accessed
6.16.15).
WHO.(2014a). WHO recommendations on the postnatal
care of the mother and newborn. World Health
Organization, Geneva.
WHO.(2014b). World Health Statistic 2014. World Health
Organization, Geneva.
WHO.(2011). WHO | PMNCH Fact Sheet: RMNCH
Continuum of care [WWW Document]. WHO.
Available at: http://www.who.int/pmnch/about/
continuum_of_care/en/ (accessed 7.12.18).
Yego, F., Williams, J. S., Byles, J., Nyongesa, P., Aruasa, W.,
and D'Este, C. (2013). A retrospective analysis of
maternal and neonatal mortality at a teaching and referral
hospital in Kenya. Reproductive health, 10(1): 13.
Effect of Timing of First Postnatal Check on Neonatal Death in Indonesia: Analysis of IDHS 2002-2003, 2007, and 2012 with Retrospective
Cohort Study
2685
