
Dysrhythmias in Congestive Heart Failure
Ledi Iksarina
1
and Halimuddin
2
1
Nursing Science Program, Faculty of Nursing, Universitas Syiah Kuala Banda Aceh, Indonesia
2
Department of Emergency and Critical Care Nursing, Faculty of Nursing, Universitas Syiah Kuala Banda Aceh, Indonesia
Keyword: Congestive Heart Failure, Sinus Dysrhythmia, Supraventricular Dysrhythmia, Ventricular Dysrhythmia,
Atrioventricular Block Conduction, Interventricular Block Conduction.
Abstract: Dysrhythmias is a clinical critical event which aggravate congestive heart failure. Dysrhythmia might be
caused the main heart failure nursing diagnose, decreased of cardiac output occurred, then early dysrhythmia
identification will help nurse to determine etiology and planning that will be given. Rhythm identification can
be done by electro-cardiogram (ECG). The study was to aim an illustration on congestive heart failure
dysrhythmia. This descriptive qualitative study was designed with secondary data retrospective study
(medical record) on 282 congestive heart failure patients who were hospitalized in dr. Zainoel Abidin Hospital
Banda Aceh. Data collection used ECG strip in first 24 hours and the result were written in the research sheet.
After whole data collected, it was found that Sinus Dysrhythmia was in 68 respondents (24,10%),
Supraventricular dysrhythmias in 51 respondents (18,10%), Ventricular Dysrhythmias in 10 respondents
(3,60%), Atrioventricular Block Conduction in 14 respondents (5,00%), Interventricular Block Conduction
in 18 respondents (6,40%), whereas 121 respondents (42,90%) had Normal Sinus Rhythm. Dysrhythmia
finding should not be the main indicator on detect problem that caused decrease of cardiac output, so nurse is
recommended to identify another condition that underlying the nursing diagnose has been labeled.
Cardiovascular nurse is suggested not to ignore normal rhythm in heart failure, meanwhile the nurse have to
identify another dysfunction underlying decreased of cardiac output.
1 INTRODUCTION
Cardiovascular diseases are the top cause of death in
the world. Based on data from WHO 2015 which
report in Top Ten Causes of Death 2017, heart disease
is in the top position with 54% of all causes mortality
in the world. Congestive heart failure is a condition
which increase high mortality rate caused by
cardiovascular. The clinical event that worsening
congestive heart failure is dysrhythmia. According to
the study conducted in Prof. Dr. R. Kandou Hospital,
Manado showed that 119 from 376 coronary artery
disease cases are belonging dysrhythmia, and 6 are
congestive heart failure with dysrhythmia. Mortality
rate caused by dysrhythmia also high, 35%
dysrhythmia was among 51-60 years old, 29% in 61-
70 years old, and 1% in 71-80 year old. It shows that
only 1% patient with dysrhythmia can survive up to
80 years old. (Kalangi, Jim and Joseph, 2016, p. 2).
Dysrhythmia is an emergency case as it
conduction disorder can influence cardiac output
which can change every second, then leading on
nutrient and oxygen circulation until critical
condition. An examination that can be done by nurse
to detect dysrhythmia is Electrocardiogram (ECG)
tapping.
Dysrhythmia which influences cardiac output
findings can direct the nurse to establish etiology of
nursing diagnose which has labeled, where the
exchange of heart beat and rhythm is one of criteria
in nursing diagnose, decreasing of cardiac output.
Accuracy in rhythm interpretation is very determined
patient’s live related intervention that will be given.
The dysrhythmia treatment purpose is to return the
rhythm and heart contraction effectivity, decrease of
anxiety, and also reduce high mortality rate caused by
cardiovascular (Smeltzer and Bare, 2003, p. 698;
Solikhah, 2015, p. 36).
The study aimed to identify rhythm illustration
that can occur in congestive heart failure, so the result
can give basic data regarding the possible
dysrhythmia in heart failure, facilitate nurse to
recognize the problem which makes hemodynamics
worse and determine the best treatment. Therefore,
Iksarina, L. and Halimuddin, .
Dysrhythmias in Congestive Heart Failure.
DOI: 10.5220/0008783200002442
In Proceedings of the Aceh International Nursing Conference (AINC 2018), pages 5-10
ISBN: 978-989-758-413-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
5
the author is interested in discussing the possible
rhythm in congestive heart failure.
2 METHODS
The study was a descriptive quantitative study with
retrospective design, which total sampling on 282
congestive heart failure patients aged between 57 to
60 years who were hospitalized around July and
December 2017 in the Intensive Cardiovascular Care
Unit and Integrated Cardiac Treatment Ward of dr.
Zainoel Abidin General Hospital, Banda Aceh.
Ethical approval was accepted from the Research
Ethic Committee of Nursing Faculty, Syiah Kuala
University.
3 RESULTS
3.1 Sample Characteristics
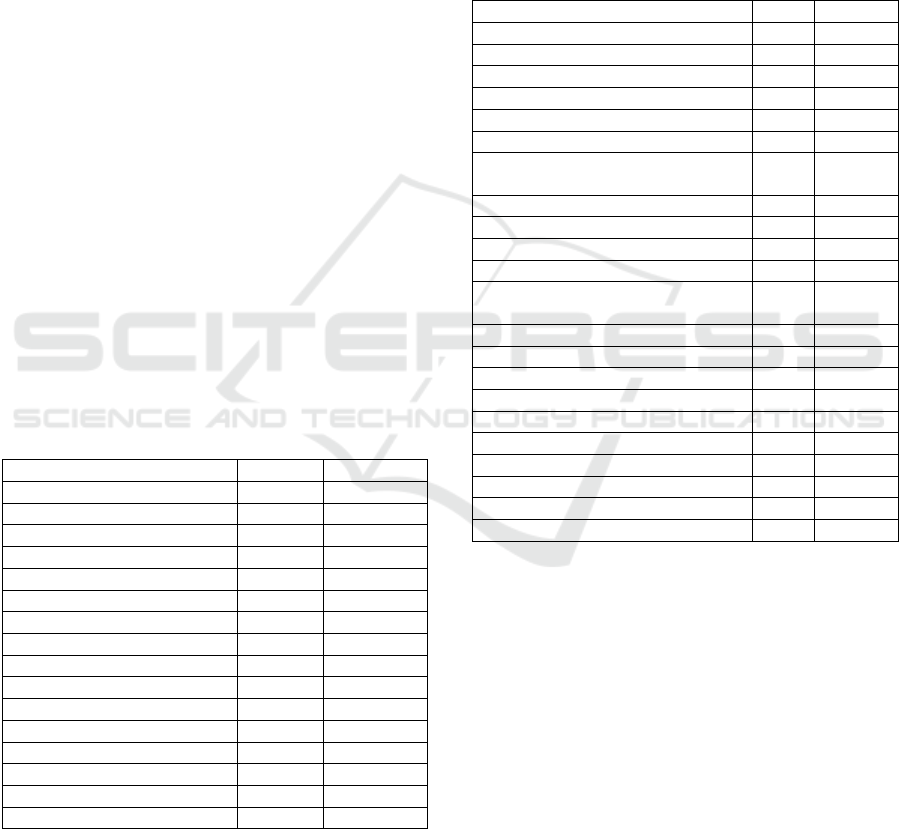
Sample characteristics are described in Table 1. The
table shows that male has higher risk of congestive
heart failure (63,80%) than female (36,2%), heart rate
mostly in normal range (66,90%). The sample of this
study are mostly congestive heart failure caused by
hypertension heart disease (32,3%).
Table 1: Characteristics of Congestive heart failure patients
(n=282).
Characteristics f %
Gender
Male 180 63,80
Female 102 36,20
Heart Rate (bpm)
<60 19 6,80
60-100 188 66,90
>100 75 26,70
Causes of Heart Failure
Valvular Heart Disease 54 19,10
Systolic Heart Failure 1 0,40
Diastolic Heart Failure 20 7,10
Coronary Artery Disease 88 31,20
Hypertension Heart Disease 91 32,30
Rheumatic heart Disease 2 0,7
Dilatative Cardiomiophaty 13 4,6
Unidentified 13 4,6
3.2 Rhythm Congestive Heart Failure
Patients
Table 2 shows normal rhythm take 42,90% from
whole samples. In Sinus Dysrhythmia the most
rhythm is tachycardia (16,7 %), than bradycardia
(4,60%) and arrhythmia (2,80%). Atrial fibrillation is
the most rhythm in supraventricular dysrhythmia
(14,20%), while premature ventricle contraction is
the most rhythm in ventricle dysrhythmia. In other
dysrhythmia, first degree AV block is the most
rhythm in AV block conduction (4,60%) and right
bundle branch block is the most rhythm in
interventricle block conduction (3,90%).
Table 2: Congestive heart failure patient based on rhythm
(n=282).
Type of Rhythm f %
Normal Sinus Rhythm 121 42,90
Sinus Dysrhythmia 8 2,80
Arrhythmia sinus
Tachycardia sinus 47 16,70
Bradycardia sinus 13 4,60
Supraventricular Dysrhythmia
Paroxismal Supraventricular
Tachycardia (PSVT)
4 1,40
Premature Atrium Contraction (PAC) 4 1,40
Atrial Fibrillation (AF) 40 14,20
Atrial Flutter 3 1,10
Ventricular Dysrhythmia
Premature Ventricle Contraction
(PVC)
9 3,20
Ventricle Tachycardia (VT) 1 0,40
Ventricle Fibrillation (VF) 0 0
Atrioventricular Block Conduction
1st degree AV Block 13 4,60
2nd degree AV Block, Wenckebach 0 0
2nd degree AV Block, Mobitz Type II 1 0,40
3rd degree AV Block 0 0
Interventricular Block Conduction
Right Bundle Branch Block (RBBB) 1 3,90
Left Bundle Branch Block (LBBB) 7 2,50
4 DISCUSSIONS
The result shows that the higher age makes the higher
risk of congestive heart failure. The result is
supported by an epidemiology study which state that
the average age of congestive heart failure patients in
South East Asia is 60 years old (Sakata and
Shimokawa, 2013, p. 2211). On the study conducted
by Rusinaru et al in France, the average of age from
368 samples were in late elderly group that is 69-85
years old. The range of age on its study is higher
because France has high rate of life expectancy and
the criteria of samples is patients whose low of
ejection fraction significantly (Rusinaru et al., 2008,
p. 568). Higher of age cause heart valvular stiffness
and hypertrophy, decreasing myocardium and blood
AINC 2018 - Aceh International Nursing Conference
6

vessels elasticity and worsening calcium and lipid
calcification in the artery and vein. Even function is
maintained in normal condition, cardiovascular
system is unable to survive in responding high of load
on compensating circulation needed for long time.
Cardiac output maximum will reduced up to 20%
since 20 until 80 year old (Smeltzer and Bare, 2003,
p. 191).
Risk of congestive heart failure was higher in
male than female (i.e 63,2% on male and 36,8% on
female). The percentage was widely caused by
cigarette and caffeine consumption in male is higher
than female, especially in Aceh. Similarly with the
study conducted by Maulidta (2014) where male has
63,3% encounter coronary artery disease which
trigger heart failure, this was caused by male not
having estrogen hormone which effect atherosclerotic
formation, meanwhile female had estrogen hormone
that prevent atherosclerotic formation or other harm
condition to the blood vessels (Maulidta, 2014, p. 58).
An epidemiology study by Sakata & Shimokawa
showed that 50-70% congestive heart failure patient
in Asia were male (Sakata and Shimokawa, 2013, p.
2211).
In other ways, based on the study was conducted
by Fachrunnisa, Nurchayati, and Arneliwati (2015)
showed that female was more widely in risk on
congestive heart failure (53,3%). In the study most of
respondents were female whose age more than 45
years old which were dominantly menopause.
Menopause caused the reduction of estrogen hormone
and High Density Lipoprotein (HDL) which leading
atherosclerosis was easier to form in blood vessels.
Moreover female psychological is tend to
maladaptive and makes them easier attack to disease
(Fachrunnisa, Nurchayati and Arneliwati, 2015, p.
1099). In terms of etiology that underlying heart
failure, both coronary artery disease or hypertension,
male was higher on percentage that is 81,9%, so risk
of heart failure is higher than female (Farissa, 2012,
p. 37).
Samples’ heart rate in this study was dominantly
in normal range, that is 192 samples (67,1%). Even
though some kind of dysrhythmia such as
supraventricular dysrhythmia or ventricular
dysrhythmia were frequently happen, the heart rate
was possible in normal range. The result of the study
also showed heart rate can increase over normal rate
(24,8%) or decrease under normal rate (6%).
Normal heart rate is including in compensatory
system to maintain cardiac output in normal levels.
One of compensation system is enhances sympathetic
activity reflexively to the heart which makes
effectivity of heart contractibility increase
(Sherwood, 2013, p. 353). Sympathetic and
epinephrine stimulation will increase heart
contractibility through increased contraction strength
in each end diastolic volume. It makes heart
contraction stronger and eject more blood out of
heart. Furthermore, sympathetic stimulation will
enhance vein back flows where the vein constriction
and let the higher blood volume from vessel to the
heart, then increasing end diastolic volume and
subsequently cardiac output will increase (Sherwood,
2013, p. 351).
Hypertension and coronary artery disease are two
highest causes congestive heart failure. This
statement is supported by some studies that show both
conditions enhance the risk of heart failure. Based on
study which was conducted by Halimuddin (2010),
33,3% congestive heart failure patients from his
samples are caused by hypertension and coronary
artery disease. As a study conducted by Kaneko et al
(2014) in Japan, there was 60% from 17.517 samples
were hypertension and coronary artery disease
(Halimuddin, 2013, p. 98; Kaneko et al., 2014, p.
188). In another study which conducted by Kaneko to
see the relation between clinical characteristics with
morbidity and mortality rate of congestive heart
failure through fraction and ejection shows that
hypertension is one of some factors that aggravate
ejection fraction of congestive heart failure besides
aging, dyslipidemia, and adherent of treatment
(Kaneko et al., 2013, p. 108).
Normal Sinus Rhythm (NSR) is the most widely
rhythm in this study, with normal ejection fraction
and heart rate.Most of heart failure especially
congestive heart failure show a normal maintained
condition from any compensatory system
(asymptomatic heart failure). Continuously
compensation episode will cause remodeling
structural of heart and culminate to symptomatic heart
failure. Symptomatic heart failure will arise if it is
followed by precipitations factors such as infection
(bacteria or virus), arrhythmia, infarct, anemia,
hyperthyroid and pregnancy, over of activity,
emotional, imbalance of salt diet, and disease
progressivity (Panggabean, 2014, p. 1132).
Normal rhythm in congestive heart failure shows
compensation system work to maintain cardiac
output. Continuously compensation makes heart
work heavier and leading the changes of cardiac
structure. Normal rhythm findings are not showing a
safe condition because it is temporally. This normal
condition also caused by effect of recent treatment
and medicine consumption. Pharmacological such as
anti-arrhythmias are used as front liner to prevent left
ventricle dysfunction. However considering drug
Dysrhythmias in Congestive Heart Failure
7

utilization is needed since the side effect makes
patient worsen (Hsu, 2007, p. 46).
Sinus dysrhythmia is a rhythm disorder that
widely happen in congestive heart failure patients.
Rhythm of sinus dysrhythmia is dominantly sinus
tachycardia. Mostly caused by hypertensive heart
disease and coronary artery disease with decreasing
ejection fraction.
Sinus tachycardia signed by heart rate rapidity
over than 100 and reach 180 beat per minute (bpm).
During sinus tachycardia, Sino Atrium Node (SA
Node) release impulse between 100 and 180 beat per
minute, but the rapidity can slower along with aging
and activity. Sinus tachycardia is divided into two,
appropriate tachycardia and inappropriate
tachycardia. Appropriate tachycardia is caused by
body stress response such as activity, anxiety, fever,
thyrotoxicosis, hypovolemia, or drug toxicities to
maintain cardiac output. Meanwhile inappropriate
tachycardia is caused by vagal system dysfunction or
disorder in the SA node (Yamin, Harun and Makmun,
2014, p. 1346).
Sinus tachycardia in congestive heart failure is
supported by some factors such as structural
abnormality, metabolic dysfunction, and medication.
Structural abnormalities for instance myocardium
injury which disturb electricity current impulse
toward ventricles and cardiomegaly which increase
preload and afterload that cause prolonged
repolarization cyclic. Metabolic dysfunction that
underlying tachycardia in congestive heart failure
involves neurohormonal activation which conduce
increasing of adrenaline and noradrenaline hormone
plasm, also be responsible of beta-blocker and
Angiotensin Converting Enzyme (ACE) effect on
sudden death, the study explained that significantly
enhancement of norepinephrine is related to
arrhythmias cases (Masarone et al., 2017, p. 2).
Sinus tachycardia commonly found in heart
failure patients caused by hypertension and coronary
artery disease (Raka, Danes and Supit, 2015, p. 755).
It is supported by a study was conducted by Kalangi,
Jim, and Joseph (2016) where the high risk causes
arrhythmias is hypertension (41%), meanwhile the
study mention that sinus bradycardia rhythm is the
most commonly sinus dysrhythmias in congestive
heart failure (65%) especially heart failure ed causa
coronary artery disease (Kalangi, Jim and Joseph,
2016).
Heart failure as a clinical syndrome regarding
heart inability to supply adequate of blood to systemic
will execute compensation effort to maintain cardiac
output by many ways, one of them is with enhance
heart contractility. By increasing heart contractility,
the heart rate will be accelerated, but this sympathetic
stimulation could not persist since heart no more
responsive to the nor-epinephrine stimulation.
Continuously compensation makes heart works
heavier and will contort heart structure, it be
worsening by aging which causes heart inability to
compensate well, it is showed by even heart rate and
contractility increase but ejection fraction still low. In
other side, bradycardia is commonly happen in
congestive heart failure, it is caused by any
dysfunction on SA node that makes inadequate
amount of impulse to the atrium or caused by obstacle
which makes the impulse cannot reach the ventricles
(Masarone et al., 2017, p. 4).
Supraventricular dysrhythmias in congestive
heart failure is most widely Atrial Fibrillation (AF)
rhythm that is 40 respondents (14,2%). The
dysrhythmia is mostly caused by valvular heart
disease (20 respondents) and have low ejection
fraction on 28 respondents who were examined their
echocardiography.
Impulse deliver synchronization is the most
important to create an effective heart blood pump. In
fibrillation, heart cells contraction and excitation are
randomly and unsynchronized. Atrial fibrillation is
signed with rapid, irregular, and uncoordinated atrial
depolarization (unclear P wave) which leading
disruption of atrium contraction. The irregularity of
atrial contraction induces the irregularity impulse to
the AV node and causes ventricles rhythm is
irregular. Some ventricle pulsation will be closer and
also elongate, when two ventricle pulsations are
closer than the ventricle preload will getting shorter
and the product of preload decrease, if the preload
decrease so the next contraction will be weak.
Sometimes, the ventricle contractions is too weak to
pump out blood from heart and causes brachialis vein
is impalpable (Sherwood, 2013, p. 335,340).
Atrial fibrillation findings in congestive heart
failure patients is also reported in study conducted by
Velderrabano et al (2016), there were 20 respondents
(33,3%) from 60 samples with supraventricular
dysrhythmia were atrial fibrillation and closely
related to high risk of chronic kidney disease. They
also explained that AF will impact on long of stay
especially in intensive care unit (Valderrábano et al.,
2016, p. 7). Hsu (2007) and Kaneko et al (2014)
mentioned that AF is highly responsible to congestive
heart failure and the hospitalization duration, but it is
not as main factor the high of mortality rate in
congestive heart failure. AF also influence the left
ventricle dysfunction and its ejection fraction,
specifically on AF with Rapid Ventricular Response
(AF RVR) which the pulse is over than 100 bpm. Low
AINC 2018 - Aceh International Nursing Conference
8

ejection fraction on AF RVR is caused by left
ventricle dysfunction as impact of atrial contractility
dysfunction which is leading Atrioventricular
desynchronizing or the irregularity of ventricles (Hsu,
2007, p. 46; Kaneko et al., 2014, p.
187).Desynchronizing impulse deliver from SA node
causes impulse deliver to the ventricles worse. It will
make ventricle pump moves randomly, signed by
irregular QRS waves, leading the blood volume is not
sufficient to fulfill body circulation need.
Premature Ventricle Contraction (PVC) is most
ventricular dysrhythmia which occur in congestive
heart failure. Ventricular dysrhythmia dominantly on
congestive heart failure which caused by coronary
artery disease and valvular heart disease and have low
ejection fraction level.
Ventricular extrasystole/premature ventricle
contraction/PVC is mostly caused by ischemia, acute
myocardial infarction, heart failure, prolonged QT
syndrome, digitalis toxicity, hypokalemia,
myocarditis, cardiomyopathy or mitral valve relapse.
Emergence of this rhythm should threated based on
the etiology, even it is asymptomatic, because this
rhythm aggravation cause ventricular fibrillation
(VF) or ventricular tachycardia (VT) (Yamin, Harun
and Makmun, 2014, p. 1360). The worsening of PVC
dysrhythmias becomes VT / VF is significantly
influences cardiac output because of fast heart rate
and loss of synchronization mechanism between
atrial and ventricle contraction. Not only that,
ventricle fibrillation causes effective contraction stop
spontaneously and ventricle will vibrating
uncoordinatedly. (DeBeasi, 2003, p. 598).
Recent study which is conducted by Kalangi, Jim,
and Joseph proves that premature ventricle
contraction could happen in almost all coronary artery
disease such as stabled angina pectoris (SAP) 21%,
old myocardial infarction (OMI) 33%, unstable
angina pectoris (UAP) 25%, and NSTEMI (15%), it
is dominantly on male in above 50 year old. (Kalangi
et al., 2016, p. 4 – 5).
Ventricular dysrhythmia presents in congestive
heart failure belonging kidney disorder can increase
the glomerulus filtration rate (GFR) and hemoglobin
amount in blood. In cardiac structure, this condition
causes left ventricle mass index and coronary calcium
enhancement which leading diastolic dysfunction,
ventricular hypertrophy, also coronary artery
calcification. The increasing hemoglobin and
decrease of ejection fraction such condition above is
need to identify the relations between clinical data,
laboratory, and another cardiovascular parameters
(Bonato, Lemos, Cassiolato, & Canziani, 2013, p. 3 -
4). PVC presents can asymptomatic so control the
balances of electrolyte and exposure of infection
agents, and pharmacological optimization are very
suggested (Masarone et al., 2017, p. 8).
Ventricular dysrhythmia is a rhythm disorder
which the impulse source possibility from ventricular
ectopic pulse and produce the premature pulsation or
irregular high rapidity. High rate of ventricle pulse
(ventricle tachycardia) in long time can ending with
ventricle fibrillation, therefore filling and emptying
ventricle episode will be ineffective.
In this study, atrioventricular block conduction
(AV) dysrhythmia is dominantly with first degree
atrioventricular block conduction that is 13
respondents or 4,6% from sample. AV block
conduction is widely experienced by congestive heart
failure with coronary artery disease and low ejection
fraction. This dysrhythmia is very important because
can leading severer block heart conduction (Smeltzer
and Bare, 2002, p. 762). Meanwhile Yamin in Sudoyo
(2014) explained that first degree AV block is not
need early treatment and have a good prognosis. In
another study shows that the patient with UAP,
NSTEMI, and STEMI have first degree AV block
(Kalangi et al., 2016, p. 5 – 6). First degree AV block
also experienced by inferior myocardial infarct.
Electrically, conduction line obstacles from sinus
node to AV node causes impulse cannot separately
well to the next conduction line.
Interventricular block conduction in congestive
heart failure is dominantly with Right Bundle Branch
Block (RBBB). Samples are mostly caused by valvular
heart disease and have low of ejection fraction.
Conduction block on RBBB is a conduction disorder
condition in right branch conduction system. Patients
with RBBB commonly asymptomatic, but if it find the
syncope and other conduction disorder like AV block,
so additional pacemaker is need to considered (Yamin
et al., 2014, p.1362).
Conduction deceleration which caused by
obstacles in bundle his branch makes ventricle
muscles unable to pump out the blood effectively,
sometimes the deceleration also causes the ventricle
pacemaker take over the role to produce its own
impulse and makes premature contraction or
vibrating of ventricle.
5 CONCLUSIONS
Based on the result of this study, we can conclude that
congestive heart failures are dominantly on male;
mostly caused by hypertension and coronary artery
disease, have sinus rhythm with heart rate, and
Dysrhythmias in Congestive Heart Failure
9

ejection fraction in normal range. The rhythm finding
in congestive heart failure are as follows:
a. Sinus dysrhythmias is the most widely
dysrhythmia in congestive heart failure. The
dominant rhythm is sinus tachycardia,
b. Supraventricular dysrhythmia is dominantly with
atrial fibrillation
c. Rhythm of ventricular dysrhythmia is premature
ventricle contraction (PVC)
d. Rhythm of atrioventricular block conduction is
dominantly with first degree atrioventricular
block conduction, and
e. Rhythm of interventricular block conduction is
dominantly with Right Bundle Branch Block
(RBBB)
It is recommended to nurses that not to make a
rhythm as a main indicator to determine the etiology
decrease of cardiac output, in addition nurses are
expected not to ignore the normal rhythm and more
assess the underlying causing the cardiac output
decrease. For further research is expected to study
further regarding dysrhythmia in congestive heart
failure and the effective nursing interventions to
return heart pump effectively.
REFERENCES
Bonato, F. O. B. et al. (2013) ‘Prevalence of Ventricular
Arrhythmia and Its Associated Factors in Nondialyzed
Chronic Kidney Disease Patients’, PLoS ONE, 8(6), pp.
1–7. doi: 10.1371/journal.pone.0066036.
DeBeasi, L. C. (2003) ‘Siklus Jantung’, in Price, S. A. and
Wilson, L. M. (eds) Patofisiologi: Konsep Klinis
Proses-proses Penyakit. 6th edn. Jakarta: EGC, p. 536.
Fachrunnisa, Nurchayati, S. and Arneliwati (2015) ‘Faktor-
faktor Yang Berhubungan Dengan Kualitas Tidur
Pasien Congestive Heart Failure’, Journal of medical,
2(2), pp. 1094–1105.
Farissa, I. P. (2012) Komplikasi Pada Pasien Infark
Miokard Akut St- Komplikasi Pada Pasien Infark
Miokard Akut St-. Universitas Diponegoro.
Halimuddin (2013) ‘Pengaruh Model Aktivitas dan Latihan
Intensitas Ringan Klien Gagal Jantung terhadap
Tekanan Darah’, Idea Nursing Journal, 3(3), pp. 93–
104.
Hsu, L.-F. S. skripsi/jcdd-04-00003. pd. (2007)
‘Developments in the Management of Atrial
Arrhythmias in Congestive Heart Failure’, Asia-Pasific
Cardiology, 1(120071), pp. 46–48.
Kalangi, C. S., Jim, E. L. and Joseph, V. F. F. (2016)
‘Gambaran aritmia pada pasien penyakit jantung
koroner di RSUP Prof . Dr . R . D . Kandou Manado’,
Journal e-Clinic, 4(2), pp. 1–9.
Kaneko, H. et al. (2013) ‘Clinical characteristics and long-
term clinical outcomes of Japanese heart failure patients
with preserved versus reduced left ventricular ejection
fraction: A prospective cohort of Shinken Database
2004-2011’, Journal of Cardiology. Japanese College
of Cardiology, 62(2), pp. 102–109. doi:
10.1016/j.jjcc.2013.03.013.
Kaneko, H. et al. (2014) ‘Impact of atrial fibrillation on
long-term clinical outcomes in outpatients with heart
failure’, Journal of Arrhythmia. Elsevier, 30(3), pp.
186–191. doi: 10.1016/j.joa.2013.10.002.
Masarone, D. et al. (2017) ‘Management of Arrhythmias in
Heart Failure’, Journal of Cardiovascular Development
and Disease, 4(3), pp. 1–20. doi: 10.3390/jcdd4010003.
Maulidta (2014) ‘Gambaran Karakteristik Pasien CHF di
Instalasi Rawat Jalan RSUD Tugurejo Semarang’,
Mutiara Medika, 15(1), pp. 54–58. Available at:
https://media.neliti.com/media/publications/156736-
ID-gambaran-karakteristik-pasien-chf-di-ins.pdf.
Panggabean, M. M. (2014) ‘Gagal Jantung’, in Sudoyo, A.
W. et al. (eds) Buku Ajar Ilmu Penyakit Dalam Jilid I.
6th edn. Jakarta: Interna Publishing, pp. 1132–1135.
Raka, I. M. S. K., Danes, V. R. and Supit, W. (2015)
‘Gambaran Aktivitas Listrik Jantung Pasien Rawat Inap
dengan Congestive Heart Failure ( CHF ) di Irina F-
Jantung RSUP Prof. DR. R. Kandao Manado’, Jurnal
e-Biomedik, 3(3), pp. 753–756.
Rusinaru, D. et al. (2008) ‘Effect of atrial fibrillation on
long-term survival in patients hospitalised for heart
failure with preserved ejection fraction’, European
Journal of Heart Failure, 10(6), pp. 566–572. doi:
10.1016/j.ejheart.2008.04.002.
Sakata, Y. and Shimokawa, H. (2013) ‘Epidemiology of
heart failure in Asia’, Circulation, 9(77), pp. 2209–
2217. Available at:
https://www.ncbi.nlm.nih.gov/pubmed/23955345.
Sherwood, L. (2013) Fisiologi Manusia: Dari Sel ke
Sistem. 8th edn. Edited by H. Octavius, A. A. Mohede,
and D. Ramadhani. Jakarta: EGC.
Smeltzer, S. C. and Bare, B. G. (2002) Buku Ajar
Keperawatan Medikal-Bedah. 8th edn. Edited by E.
Pakaryaningsih and M. Ester. Jakarta: EGC.
Smeltzer, S. C. and Bare, B. G. (2003) Brunner &
Suddarth’s Textbook of Medical-Surgical Nursing. 10th
edn. Philadelphia: Lippincott-Raven Publisher.
Solikhah, M. (2015) ‘Deteksi Aritmia pada
Elektrokardiogram dengan Metode Jaringan Syaraf
Tiruan Kelas Jamak menggunakan Fitur Interval RR ,
Lebar QRS , dan Gradien Gelombang R’, Jurnal Fisika
dan Aplikasinya, 11(8), pp. 36–40.
Valderrábano, R. J. et al. (2016) ‘Risk factors and clinical
outcomes of arrhythmias in the medical intensive care
unit’, Journal of Intensive Care. Journal of Intensive
Care, 4(1), pp. 1–10. doi: 10.1186/s40560-016-0131-x.
Yamin, M., Harun, S. and Makmun, L. H. (2014)
‘Elektrofisiologi’, in Sudoyo, A. W. et al. (eds) Ilmu
Penyakit Dalam Jilid I Ed. 6. 6th edn. Jakarta: Interna
Publishing, pp. 1325–1333.
AINC 2018 - Aceh International Nursing Conference
10
