
Illness Perception of Schizophrenia among Schizophrenic Outpatients
Sri Novitayani
1
, Weena Chanchong
2
and Wandee Suttharangsee
2
1
Faculty of Nursing, Syiah Kuala University, Darussalam, Banda Aceh, 23111, Indonesia
2
Faculty of Nursing, Prince of Songkla University, Hatyai, Songkhla, 90110, Thailand
Keywords: Cognitive Illness Representation, Schizophrenia
Abstract: Schizophrenia as a chronic illness requires continuous treatment to prevent severe symptoms. The
schizophrenic patients must have appropriate coping in order to continuously follow the treatment that
determined by the medical team. Cognitive illness representation has a role in determining coping that is
chosen to deal with problems. It consists of identity, cause, timeline, consequences, and controllability
dimensions. Schizophrenic outpatients in this study had good identity because they labeled their symptoms
as a part of schizophrenia. However, majority of them had less perceived on schizophrenia as chronic and
cycle illness, negative consequences of schizophrenia, and treatment controlling schizophrenia. Majority of
them also had perceived that schizophrenia was caused by several causes. Temptation from AllAh SWT and
followed by stress or worry were the most patient’s perception as causes of schizophrenia. Overall
participant has experienced rehospitalization because of medication non-adherent. Therefore, we conclude
that cognitive illness representation may contribute to the behavior of taking medication as a coping strategy
in dealing schizophrenia. According to this, the researchers suggest that nurse should examine the
schizophrenic patient’s cognitive illness representation in order to know their views of schizophrenia, so the
nurse can predict the behavior that they will use to overcome the problem.
1 INTRODUCTION
Schizophrenia is a serious psychiatric disorder. It
causes disorganized and bizarre thoughts, emotion
behavior and perceptions which is manifested by
hallucination and delusion (Videbeck, 2011).
Individuals suffer schizophrenia while they have
psychotic symptom for at least six months
continuously, which is not related to health problems
or substance abuse, and seriously disrupt social and
occupational functioning (O’Brien et al., 2013). The
symptoms will get worse if patient doesn’t follow
treatment to deal schizophrenia. Therefore, the
patient has the appropriate coping strategies to
overcome problem because of schizophrenia.
Determining coping strategies that will be used
by individuals to cope the illness is influenced by the
individual’s perception of the illness (Tiemensma et
al., 2016). Poorer illness perceptions that individual
has are associated with increased involvement
maladaptive coping (Knowles, Cook, & Tribbick,
2013). Lobban et al. (2004) found that different
illness perceptions about schizophrenia including
identity, cause, timeline, consequences and
controllability dimension lead different behavioral as
coping strategies in order cope the problem (Lobban
et al., 2004). Those are suitable with framework of
Common Sense Model (CSM) that was developed
by Leventhal et. al. (1980).
The CSM illustrates how an individual takes
action in order to againts the threat of his/ her illness
(Kucukarslan, 2016). The framework of CSM
showed that individual’s behavior as coping that
used to overcome the problem of illness related to
individual’s perception about the illness (Leventhal
et al. 1980). The individual’s illness perception
could be changed anytime.
There is some coping strategies that should be
taken by schizophrenic patients to deal
schizophrenia. Adherence to medication is main
coping for schizophrenic patients in order to
manage their symptoms. Nicolino et al. (2011) found
that individual perceived about susceptibility of
illness, severity of illness, barrier of medication, and
benefit of medication can influence medication
adherence of schizophrenic patient. Study by Al-
Yahya and Fayad (2013) also found that
schizophrenic patients did not take their medication
242
Novitayani, S., Chanchong, W. and Suttharangsee, W.
Illness Perception of Schizophrenia among Schizophrenic Outpatients.
DOI: 10.5220/0008397000002442
In Proceedings of the Aceh International Nursing Conference (AINC 2018), pages 242-249
ISBN: 978-989-758-413-8
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

continously because they had lack insight about thier
illness, such as perceived that they have an organic
disorder or did not have psychological disorder
eventhought they have positive symptoms. So, the
wayof individual’s perception about their illness
influence their coping to deal the illness. A literature
review about medication adherence of schizophrenic
patients also found that medication adherence was
influenced by patient’s perception of illness
(Novitayani & Suttharangsee, 2012).
Medication adherence causes relaps in which
symptom may become severe. Literature review by
Emsley et al. (2013) found that high rate of relaps
occurs because of non-adherence in taking
medication after first period. Schizophrenic patients
who did not adhere to medication have risk 8 times
experiencing relapse compared to the patients who
adhered to medication (Maharani & Hardisal, 2016).
Usually, schizophrenic patients should be admitted
to psychiatric hospital when they get relapse or have
severe symptoms. Based on study by Pratama et al.
(2015), 50% of schizophrenic patients in Psychiatric
Hospital Aceh who come to polyclinic have relapse
and 62,5% of the patients did not adhere to
medication.
Based on all above, researchers are interested to
identify the illness perception of schizophrenic
outpatients who have experienced rehospitalization.
The researchers conducted this study in Psychiatric
Hospital Aceh.
2 COMMON SENSE MODEL
The Common Sense Model is a framework of the
way to provide behavior as coping in dealing with
problems due to the illness. Leventhal et al. (1980)
developed Common Sense Model (CSM) that
consists of illness representation, coping and
appraisal. Initially, individual will provide illness
representation, cognitive and emotional illness
representations, based on information. Those illness
representations affect the coping strategies of
individuals with purpose to overcome the problem
regarding to the illness. Coping strategies will be set
up through behavior. Lastly, individuals evaluate
their coping if the coping is effective or not in facing
the problem because of the illness.
This study identifies cognitive illness
representation as part of illness representation. It
considered as a lay individual’s framework of
thoughts or belief about illness. Cognitive illness
representation consists of five dimensions including
identity, cause, timeline, consequences, and
controllability dimensions (Leventhal et al., 1980).
Identity refers to statements regarding belief about
the illness, label, and knowledge about its
symptoms. Cause refers to beliefs regarding the
factors that are responsible for causing the illness.
Timeline refers to belief about the course of the
illness (such as chronic, acute, etc.) and the time
scale of the illness symptoms (such as persistence,
temporary, etc.). Consequences refer to belief
regarding the impact of the illness on quality of life
of functional capacity. Controllability refers to belief
about the efficacy of treatment and personal coping
that may alter the illness.
Cognitive illness representation associated with a
danger control process (Leventhal et al., 1980). The
danger control process refers to how the individuals
perceived the threat of their illness and what they do
to overcome the illness.
3 METHODS
This study is descriptive design that conducted in
Aceh, Indonesia. The study aims to examine illness
perceptions, especially cognitive illness
representation, among schizophrenic outpatients
who come to the polyclinic in Aceh Psychiatric
Hospital. There are some objectives in this study as
following:
1. To identify illness perceptions of schizophrenic
outpatient on identity dimension
2. To identify illness perception of schizophrenic
outpatient on cause dimension
3. To identify illness perception of schizophrenic
outpatient on timeline dimension
4. To identify illness perception of schizophrenic
outpatient on consequences dimension
5. To identify illness perception of schizophrenic
outpatient on controllability dimension
2.1 Inclusion Criteria
Forty participants who participated in this study
were schizophrenic outpatients from polyclinic of
Aceh Psychiatric Hospital, Indonesia. The inclusion
criteria consist of suffering schizophrenia that is
diagnosed by the psychiatrists at the Aceh
Psychiatric Hospital, aged between 18 to 60 years
old, having hospitalization at least twice since
diagnosis, scoring of the Brief Psychiatric Rating
Scale (BPRS) less than 41, good communication,
and willing to participate in this study.
Illness Perception of Schizophrenia among Schizophrenic Outpatients
243

2.2 Instruments
Three instruments were used in this study. There are
the Brief Psychiatric Rating Scale (BPRS), the
Demographic Data Questionnaire (DDQ), and the
Cognitive Illness Representation Questionnaire for
Schizophrenia (CIRQS).
2.2.1 The Brief Psychiatric Rating Scale
(BPRS)
The BPRS was as screening tool to screen potential
patient in this study through assessing both their
positive and negative symptoms such as anxiety,
depression, hallucinations, suspiciousness, and other
unusual behavior. The BPRS was developed by
Overall and Gorham (Leucht, et al., 2005). The
BPRS has 18 items to assess psychiatric symptoms
with Likert scale from 1 (no present) to 7 (extremely
severe).
The BPRS divided into seven categories
involving normal (score 18), borderline ill (score 19-
30), mildly ill (score 31-40), moderately ill (score
41-52), markedly ill (Score 53-64), severely ill
(score 65-83), and extremely ill (score 84-126)
(Leucht, et al., 2005). In this study, the researcher
used BPRS score less that 41 which is consider as
normal (score 18), borderline ill (score 19-30) and
mildly ill (score 31-40) to recruit participants.
2.2.2 The Demographic Data Questionnaire
(DDQ)
The DDQ was developed by researchers with
purpose to measure demographic data. It consists of
age, gender, education level, occupation, monthly
income, number of hospitalization, and length of
illness.
2.2.3 The Cognitive Illness Representation
Questionnaire for Schizophrenia
(CIRQS)
The CIRQS was used to assess cognitive illness
representation of mental health problem for
schizophrenic patients. The CIRQS was modified
from the IPQS that was developed by Lobban,
Barrowclough, and Steven (Lobban, Barrowclough,
& Jones, 2005). The CIRQS has five dimensions
including identity, cause, timeline, consequences,
and controllability dimensions. The format of the
CIRQS is a combination between dichotomous and
the Likert scale.
The identity dimension has several lists of
negative and positive symptoms. The item statement
of symptoms are scored from 0 to 1 (dichotomous)
with yes = 1 and no = 0 for having had symptoms
since the mental health problem occurred and scored
1 for each symptom if the subjects gave an answer in
the part of mental health problem. Cause, timeline
that consists of acute/chronic and cycle sub
dimensions, consequences, and controllability
dimensions had positive and negative statements
(21, 8, 9, and 4) with a 5-point Likert scale.
2.3 Validity and Reliability of The
Instruments
The content validity of the instruments were
evaluated by three experts including two lectures
from the Faculty of Nursing in Prince of Songkla
University and a lecture from the Faculty of Nursing
in Indonesia University. The researchers revised the
instruments based on suggestions from three experts.
The CIRQS had a good content validity index
(0.89).
The reliability of the CIRSQ, except symptoms,
was testes for internal consistency by using
Cronbach’s alpha coefficient. The CIRSQ was
accepted because the reliability value of Conbach’s
alpha coefficient was 0.81. For the symptoms, one
part of the identity dimension of CIRSQ, the
reliability was tested to examine inter-rater
agreement by using Kappa coefficient and the value
was 0.69. The kappa value of 0.69 was in substantial
agreement range between the first test and second
test (test-retest) (Landis & Koch, 1977 as cited in
Sim & Wright, 2005). The symptoms questionnaire
was accepted, because the reliability value of the
Kappa coefficient was greater than 0.4 (Sim &
Wright, 2005).
4 RESULTS
Descriptive statistic, especially frequencies and
percentages was used to analyze the data in this
study. Score of the BPRS among patients in this
study was in range 18 -30. All of the results in this
study will be explained more in detail as following.
4.1 Demographic Data
The results showed that majority of participants
were male (65%), age in adult category (95%),
senior high school (42.5%), and rehospitalization
from 2 until 5 times (70%). Mostly participants have
length of illness from 11 to 15 years (45%), and
occupation (87.5%).
AINC 2018 - Aceh International Nursing Conference
244
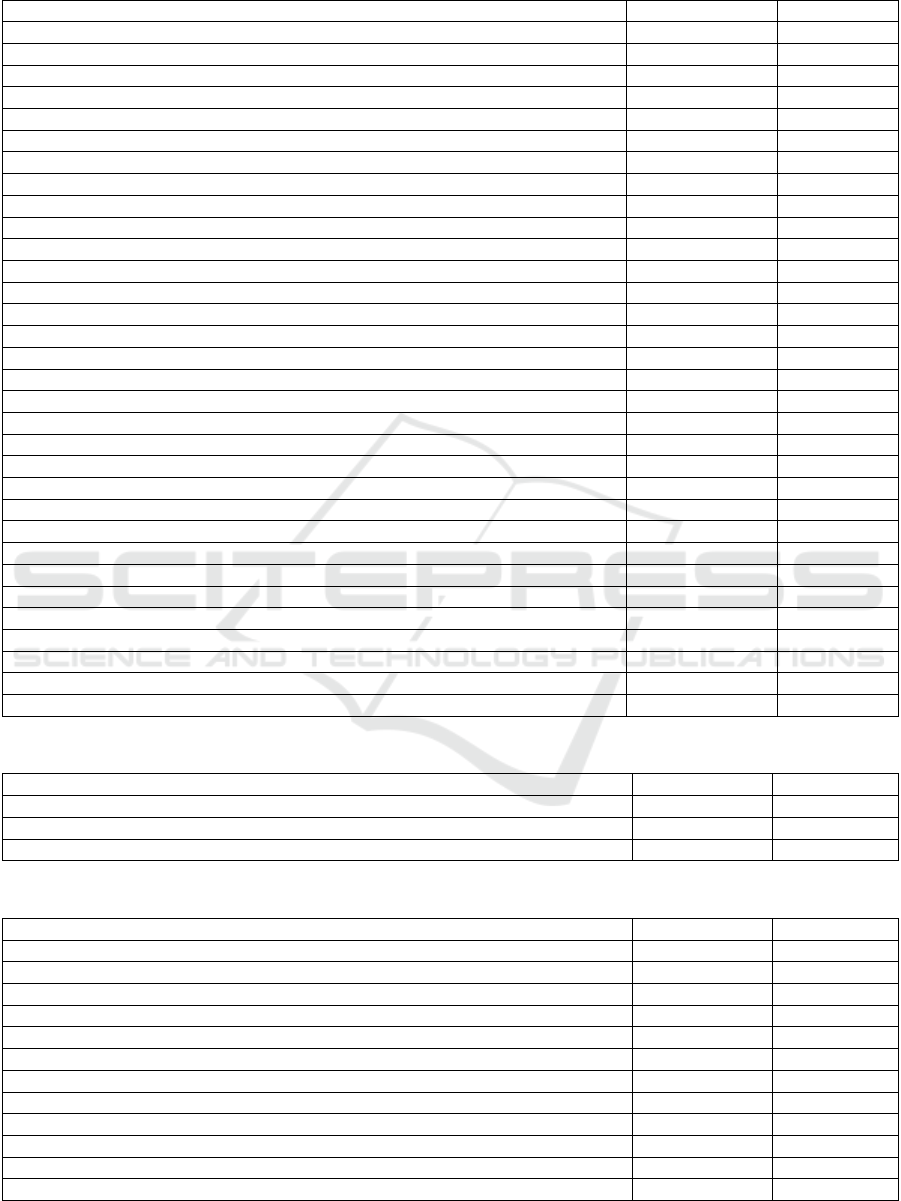
Table 1: Frequency and percentage of the participants by demographic data.
Characteristic N %
Age
Mildly Adult (18 – 25 years old) 2 5
Adult (26 – 65 years old) 28 95
Gender
Male 26 65
Female 14 35
Educational level
No formal education 1 2.5
Elementary school 5 12.5
Junior high school 9 22.5
Senior high school 17 42.5
University 6 15
Others 1 2.5
Occupation
Yes 25 62.5
No 15 37.5
Monthly income (IDR)
No income 15 37.5
300,000 – 1,000,000 17 42.5
> 1,000,000 8 20
Rehospitalization
2 – 5 times 28 70
6 – 10 times 8 20
11 – 15 times 4 10
Length of illness
1 – 5 years 3 7.5
6 – 10 years 7 17.5
11 – 15 years 18 45
16 – 20 years 6 15
21 – 25 years 4 10
31 – 35 years 1 2.5
41 – 45 years 1 2.5
Table 2: Frequency and percentage of the participants by identity level.
Identity level (proportion score) n %
Low identity (0 – 0.33) 2 5.0
Moderate identity (0.34 – 0.67) 5 12.5
High identity (0.68 – 1) 33 82.5
Table 3: Frequency and percentage of the participants by cause dimension.
Causes of schizophrenia n %
Stress or worry 27 67.50
A gem or virus 4 10.00
Chance or bad luck 11 27.50
Allah SWT 29 72.50
Family problems 23 57.50
Alcohol 6 15.00
My Personality 12 30.00
Death of a loved one 7 17.50
Thinking about things too much 26 65.00
Being bullied by others 15 37.50
Hereditary; it runs in my family 7 17.50
Poor medical care in my past 15 37.50
Illness Perception of Schizophrenia among Schizophrenic Outpatients
245
Causes of schizophrenia n %
My own behavior 13 32.50
Money worries 23 57.50
Overwork 8 20.00
Taking illicit drugs 7 17.50
Brain damage or abnormality 8 20.00
Chemical imbalance in the brain 5 12.50
My mental attitude, for example, thinking about life negatively 9 22.50
A trauma; something disturbing or shocking that happened in my life 15 37.50
Black magic 14 35.00
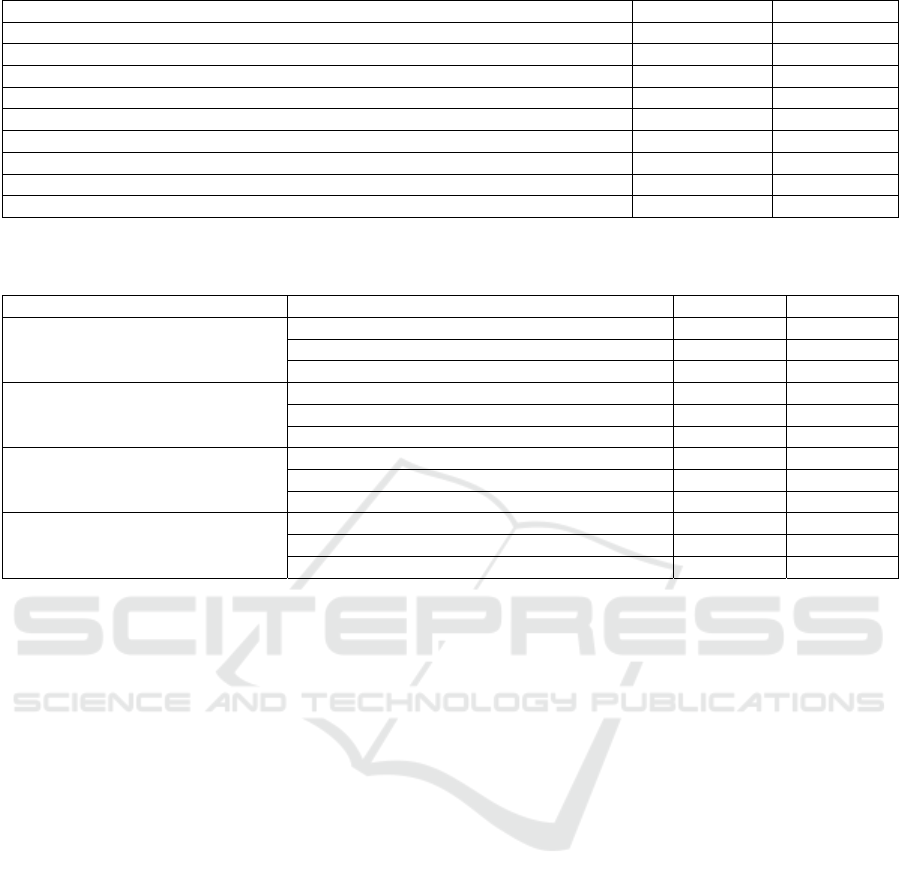
Table 4: Frequency and percentage of the participants by chronic sub-dimension, cycle sub-dimension, consequences
dimension, and controllability dimension.
Categories n %
chronic sub-dimension
Strongly perceived 6 15
Less perceived 30 75
No perceived 4 10
cycle sub-dimension
Strongly perceived 9 22.5
Less perceived 25 62.5
No perceived 6 15
consequences dimension.
Strongly perceived 13 32.5
Less perceived 25 62.5
No perceived 2 5
controllability dimension
Strongly perceived 17 42.5
Less perceived 23 57.5
No perceived 0 00.0
4.2 Cognitive Illness Representation
4.2.1 Identity Dimension
Most of participants had high identity level (82.5%).
High identity has similar meaning with good
identity. It means the participants can identify their
all symptoms as part of mental illness or
schizophrenia.
In this study, majority schizophrenic patients had
perceived the symptoms that they experienced were
part of the condition as well as schizophrenia. The
previous study by Lobban, Barrowclough, & Jones
(2004) showed that the symptoms that were suffered
by schizophrenic were identified as a mental health
problem.
The result of the current study in table 2 could be
happen because majority schizophrenic patients had
suffered schizophrenia more than five years and
rehospitalized to psychiatric hospital, so they were
aware and more understand about their symptoms
related to mental illness. A qualitative study by
Guner (2014) also found that schizophrenic patients
can define their symptom and they were aware that
they experienced the symptoms as part of
schizophrenia.
The gender may influence this result. Ward and
Besson (2012) reported that overall patients with
mental health problem that all of them are men
labeled the symptoms as mental health problem. In
this study, majority of participants were men.
While the schizophrenic patients belief that their
symptoms is attributed to mental health problem or
schizophrenia, they could be decided to take
medication as doctor prescribed in order to reduce
the symptoms. According to literature by Lobban et
al. (2003), patient with mental illness were more
likely to take medication adherence while they had
labeled that their mental illness as viewed from their
symptoms is a mental illness.
4.2.2 Cause Dimension
According to CIRQS, there were 21 causes of
schizophrenia. The result showed that majority
participants perceived temptation from Allah SWT
(72.5%), and stress or worry (67.5%) as causes of
their mental health problem, schizophrenia. All of
participants had perceived cause of schizophrenia
more than one.
The exactly cause of schizophrenia is unknown
until now. However, there is some cause that may
affect someone suffering schizophrenia (University
of Maryland Medical Center [UMMC], 2011). In
AINC 2018 - Aceh International Nursing Conference
246

this study, each participant had perceived more than
one the cause of mental health problem or
schizophrenia. In the first rank, participants had
perceived temptation or test from Allah SWT as
cause of their mental health problem or
schizophrenia. It can be happen because of all
participants are Muslim. The Islamic view of the
disease is a test or temptation given by Allah SWT
and if we are patient in facing it, our previous sins
will be erased. In Surah Al Baqarah (155), Allah
SWT says that we will indeed give you test, with
little fear, hunger, lack of wealth, soul and fruits.
This is also supported by the words of the prophet
Muhammad SAW that a Muslim is struck by an
unpleasant, sick or other thing, and Allah SWT will
erase his mistakes, and his sin will fall as leaves falls
down from the tree (Muttafaq’alaih Hadist). In
Islamic psychology, Islam views personality as a
unity of body and mind aspects, so individual seek
answers to each question through the mind by using
their energy and abilities in the physical world in a
constructive way and satisfied with the answer they
find because it is based on the word of Allah SWT
(All of Surah in Al-Qur’an), philosophy and science
(Ashy, 1999). Therefore, participants feel confident
to belief that Schizophrenia or mental health
problem is the will from Allah SWT as a test.
The second rank is stress or worry. Another
study by Hussain and colleagues (2017) found that
most of schizophrenic patients strongly belief on
stress or worry, family problems, lack of friends or
people who care me, thinking about thing too much,
money worries and lack of sleep as cause of mental
health problem. Stress that is experienced by
individual in crisis situation in their life is a critical
factor in development of brain dysfunction against
psychotic susceptibility (Green et al., 2014). Stress
increases neurotransmitter of dopamine (Fortinash &
Worret, 2004) that causes the appearance of
psychotic symptoms which indicate schizophrenia
(Videbeck, 2011).
4.2.3 Timeline Dimension
Timeline dimension consist of chronic and cycle
sub- dimensions. Based on table 4, the result showed
that majority respondents had less perceived of
mental health problem or schizophrenia as a chronic
illness (75%).
The same result also found in cycle sub-
dimension like showed in table 4. Majority
respondents had less perceived of mental health
problem or schizophrenia as a cycle illness (62.5%).
Based on the results, most of the participants had
less perceived that schizophrenia is a chronic and
cycle illness. It means the participants belief that
schizophrenia would last for short time. Another
study also showed the same result that the
schizophrenic patients were less belief on
schizophrenia as chronic and cycle illness (Wall et
al., 2017). Hussain and colleagues (2017) found that
general schizophrenic patients were unsure about
mental health problem as chronic and cycle illness.
Based on study in Turki, even though some
schizophrenic patients had perceived schizophrenia
as chronic illness, most of the patients did not
exactly understand about the course of schizophrenia
(Guner, 2014). In most cases, mental illness is
viewed as an acute illness that it will occur in
particular situation like after individual experiences
stressful of their life events (Petrie et al., 2008).
The way of schizophrenic patients’ beliefs about
the course of schizophrenia will influence their
behavior to face the health problem from
schizophrenia, such as taking medication. The
previous study found that perceiving an illness
condition as chronic was significantly associated
with medication adherence (Aflakseir, 2013).
4.2.1 Consequences Dimension
The result in table 4 showed that majority
participants had less perceived of negative
consequences of the mental health problem or
schizophrenia (62.5%).
The consequences dimension involves beliefs
about negative impact of mental health problem on
the individual’s personal life, financial, and
relationship with others (such as family, social). The
participants perceived that mental health problem or
schizophrenia had negative consequences in to their
life process, however, most of them still had less
perceived on negative consequences of its.
Similar result also found in study by Wall and
colleagues (2017). In that study, schizophrenic
patients adopted that schizophrenia has less negative
consequences on physical, social and psychological
functioning. Schizophrenic patients in Mexican
believed that the schizophrenia affect their life, but
the study did not explore more about kind of
consequences that changed their life because of
their mental health problem (Gomez-de-Regil,
2015). In the other hand, study by Hussain et al.
(2017) is not only reported schizophrenic patients’
beliefs about negative consequences because of
mental health problem, but also defined in detail
kind of consequences that they experienced (such as
Illness Perception of Schizophrenia among Schizophrenic Outpatients
247

their daily activity, money, and relationship) based
on the contain of the questionnaire used in that
study.
In the present study, some participants had no
income because they did not have occupation
(37.5%). The rest of participants had occupation;
however, their income is insufficient to meet their
own needs (table 1). Thus, the data of monthly
income in table 1 supported the negative
consequences on financial problem in consequences
dimension (statement no. 1 “I do not have any job
because of my mental health problems” and
statement no. 3 “My mental health problems have
financial consequences for me”).
The severe symptoms make schizophrenic
patients difficult to maintain their function and
relationship with other as negative consequences
(Nicolino et al., 2011). Therefore, we can conclude
that schizophrenic patient’s perception about
consequences focus on the patient’s condition when
the patient has severe symptoms.
4.2.1 Controllability Dimension
According to table 4, there were slightly different
percentage perception of schizophrenic patients
between less perceived and strongly perceived on
the effectiveness of treatment in order to manage the
symptoms of mental health problem. The result
showed that 57.5% of participants had less perceive
of positive perception about controllability followed
by strongly perceived (42.5%).
Controllability dimension explores patients’
beliefs about how medication controlling the
symptoms and preventing negative consequences
that figures in the questionnaire. Generally,
schizophrenic patients consider that the treatment is
helpful to their illness (Gomez-de-Regil, 2015).
However, schizophrenic patients were unsure about
if treatment can overcome the mental health
problems (Hussain et al., 2017). Other study
reported that schizophrenic patient’s perception
about the efficacy of treatment was having some
control on their schizophrenic symptoms (Lobban, et
al., 2004).
While schizophrenic patients had strongly
perceived on the efficacy of medication in managing
symptoms of schizophrenia, the patients will adhere
to medication and follow rehabilitation program as
continuously based on team medical prescribed
(Petrie, et al., 2008). So, it is important to
schizophrenic patients strongly believe on efficacy
of treatment in controlling their severe symptoms to
be stable condition. Other than that, the patients
should be able to control the side effects from the
medication that they take. Therefore, they will
continuously take medication as prescribed.
5 CONCLUSIONS
Coping strategy that individual’s used has
influenced by individual‘s illness perception,
specifically cognitive illness representation. In this
study, overall all of participants had experienced
rehospitalization more than two times because they
did not take medication as prescribe. This may be
influenced by their illness perception about
schizophrenia. Most participants had less perceived
that the treatment could not manage the symptoms
so that they did not take medication regularly as
prescribed. Moreover, most participants also had
less perceived on negative consequences in their
personal life, financial, and relationship with other
caused by schizophrenia. So, they may feel that it is
not important to treat schizophrenia through taking
medication continuously. Then, most participants
had less perceived on schizophrenia as a long-term
illness, so they may take medication only when they
experience symptoms or the symptoms getting
worse. Furthermore, they also had perceived that
schizophrenia is caused by multiple factors and
almost all of them able to identify the symptoms as a
part of schizophrenia. Therefore, it is important to
examine patient’s illness perception in order to
predict their coping that they used to face the illness.
If their illness perception has gaps, misperception or
confusion with the concept of schizophrenia, their
coping will not suitable to overcome the problem of
schizophenia. In this situation, the nurse can provide
intervention that can change the patient’s illness
perception in accordance with the concept of
schizophrenia.
ACKNOWLEDGEMENTS
We would like to express sincere gratitude and deep
appreciation to the people who have contributed
throughout this study. A specially thank to Director
of the Aceh Psychiatric Hospital, Aceh Province,
Indonesia, who allowed this study to be undertaken
in the hospital. Moreover, acknowledge also giving
to the schizophrenic patients who participated in this
study.
AINC 2018 - Aceh International Nursing Conference
248

REFERENCES
Aflakseir, A. (2013). Predicting medication adherence
based on illness perceptions in a sample of Iranian
older adults. Middle East Journal of Age and Ageing,
10, pp. 3-7.
Al-Yahya, N.M. and Fayad, E.M. (2013). Medication
adherence of clients complaining of schizophrenia in
Saudi Arabia. World Applied Sciences Journal, 28(5),
pp. 600-607. doi: 10.5829/idosi.wasj.2013.28.05.812
56.
Ashy, M.A. (1999). Health and illness from an islamic
perspective. Journal of Religion and Health, 38(3), pp.
241-257
Emsley, R., Chiliza, B., Asmal, L. and Harvey,B. (2013).
The nature of elapse in schizophrenia. BMC
Psychiatric, 13, 50. http://www.biomedcentral.com/14
71-244x/13/50
Fortinash, K.M. and Worret, P.A.H. (2004). Psychiatric
mental health nursing, ed.3th. St. Louis: Elsevier
Mosby.
Green M.J., Girshkin, L., Teroganova, N. and Quide, Y.
(2014). Stress, schizophrenia and bipolar disorder.
Behavioral Neurobiology of Stress-Related Disorder,
pp. 217-235
Gomez-de-Regil, L. (2015). Insight and illness perception
in Mexican patients with psychosis. Schizophrenia
Research: Cognition, 2, pp. 33-38.
Guner, P. (2014). Illness perception in Turkish
schizophrenia patients: A qualitative explore study.
Archivesof Psychiatric Nursing, 28, pp. 405-412
Hussain, S., Imran, N., Hotiana, U.A., Mazhar, N. and
Asif, A. (2017). Illness perceptions in patients of
schizophreni: A preliminary investigation from
Lahore, Pakistan. Pak J Med Sci, 33(4), pp. 829-834.
doi: https://doi.org/10.12669/pjms.334.13128.
Knowles, S.R., Cook, S.I. and Tribbick, D. (2013).
Relationship between health status, illness perceptions,
coping strategies and psychological morbidity: A
preliminary study with IBD stoma patients. Journal of
Crohn’s and Colitis, 7(10), pp. e471-e478.
https://doi.org/10.1016/j.crohns.2013.02.022.
Kucukarslan, S.N. (2016). Using the Common Sense
Model in daily clinical practice for improving
medication adherence. Journal of Science
Communication, 23(5), pp. 227-230.
Leucht, S., Kane, J.M., Kissling, W., Hamann, J., Etschel,
E. and Engel, R. (2005). Clinical implication of brief
psychiatric rating scale score. The British Journal of
Psychiatry, 187, pp. 366-371. doi: 10.1192/bjp.187.4.3
66
Leventhal, H., Meyer, D. and Nerenz, D. (1980). The
common sense representation of illness danger. In S.
Rachman (Ed.), Medical psychology. (vol.2). New
York: Pergamon. Retrieved from http://www.academi
a.edu/259452/The_Common_Sense_Representation_of_Ill
ness_Danger.
Lobban, F., Barrowclough, C. and Jones, S. (2003). A
review of the role of illness models in severe mental
illness. Clinical Psychology Review, 23, pp. 171-196.
doi: 10.1016/S0272-7358(02)00230-1
Lobban, F., Barrowclough, C. and Jones, S. (2004). The
impact of beliefs about mental health problem and
coping on outcome in schizophrenia. Psychological
Medicine, 34, pp. 1165-1176. doi: 10.1017/s00332917
0400203x.
Lobban, F., Barrowclough, C. and Jones, S. (2005).
Assessing cognitive representations of mental health
problem. I. The illness perception questionnaire for
schizophrenia. British Journal of Clinical Psychology,
44, pp. 147-162. doi: 10.1348/014466504X19497
Maharani, R.. and Hardisal. (2016). Faktor yang
berhubungan dengan kekambuhan penderita
skizofrenia di Rumah Sakit Jiwa Tampan Provinsi
Riau. Menara Ilmu, 77(2), pp. 150-160.
Nicolino, P.S., Vedana, K.G.G., Miasso, A.I., Cardoso, L.
and Galera, S.A.F. (2011). Schizophrenia: Adherence
to treatment and belief about the disorder and the drug
treatment. Revisa da Escpola de Enfermagen da USP,
45, pp. 706-713.
Novitayani, S. and Suttharangsee, W. (2012). Medication
Adherence of Patients with Schizophrenia: A
Literature Review. In Proceeding of the Kunming
International Nursing Conference on Modern Nursing
Practice in Multicultural Societies, pp. 308 - 318
O’Brien, P.G., Kennedy, W.Z. and Ballard, K.A. (2013).
Keperawatan kesehatan jiwa psikiatrik: teori &
praktik. Jakarta: EGC. pp. 335
Pratama, Y., Syahrial and Ishak, S. (2015). Hubungan
keluarga pasien terhadap kekambuhan skizofrenia di
Bandan Layanan umum Daerah (BLUD) Rumah Sakit
Jiwa Aceh. Jurnal Kedokteran Syiah Kuala 15(2), pp.
77-86
Sim, J. and Wright, C.C. (2005). The kappa statistic in
reliability studies: Use, interpretation, and sample size
requirements. Physical Therapy, 85, pp. 257-268.
Tiemensma, I., Gaab, E., Voorhaar, M., Asijee, G. and
Kaptein, A.A. (2016). Illness perceptions and coping
determine quality of life in COPD patients.
International Journal of Chronic Obstructive
Pulmonary Diease, 11, pp. 2001-2007. doi:
10.2147/COPD.S109227.
Univerity of Maryland Medical Center. (2011).
Schizophrenia-causes. Retrieved from http://www.um
m.edu/patiented/articles/what_causes_schizophrenia_0
00047_2.htm
Videbeck, S.L. (2011). Psychiatric mental health nursing
(5th ed.). Philadelphia, PA: Lippincott Williams &
Wilkins.
Wall, E.L.E., Mirfin, D., White, S. and Mezey, G.C.
(2017). Perception of schizophrenia in forensic and
general adult psychiatry patients. The Journal of
Forensic Psychiatriy & Psychology, 28(3), pp. 357-
367.
Ward, E.C. and Besson, D.D. (2012). African american
men’s belief about mental illness, perception of stigma,
and help seeking barriers. The Counseling
Psychologist, 41(3), pp. 359-391.
Illness Perception of Schizophrenia among Schizophrenic Outpatients
249
