
Correlation of Interpersonal Factors, Situational with Cervical
Cancer Prevention in Woman of Childbearing Age
Ni Ketut Alit Armini, Rista Fauziningtyas and Anneke Widi Prastiwi
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Cervical Cancer, Woman, Childbearing, Prevention.
Abstract: Cancer is the main cause of death and disability in the world, especially in women. Regarding cervical
cancer, women can be pressed to participate in primary and secondary prevention. Cervical cancer
prevention in Indonesia is not a priority for women of childbearing age. This research used a cross-sectional
approach. Simple random sampling was and 159 woman of childbearing age were selected as respondents.
Independent variables involved interpersonal and situational factors. The dependent variable was the
prevention of cervical cancer. Data were collected by questionnaires and analyzed using Spearman's Rho
test with a significant level of α ≤ 0,05. This showed the relationship between interpersonal factors with
cervical cancer prevention at p = 0.000 and situational factors relating to cervical cancer prevention at p =
0.000. Interpersonal factors and situational factors have a significant relationship with the primary and
secondary prevention of cervical cancer. These results can be referenced in future research related to other
factors of HPM theory such as previous experience, urgency, perceived benefits of actions, the perceived
barriers of actions, activity related to effects, and commitment in prevention. Health officers should try to
improve information about cervical cancer prevention methods in a form that people can easily understand.
1 BACKGROUND
Cancer is the leading cause of death and disability
throughout the world, especially in women
(Ginsburg et al., 2016). Cervical cancer that strikes
women should be suppressed by conducting primary
and secondary prevention (Febriani, 2016). Cervical
cancer prevention efforts in Indonesia has still not
given priority to women of childbearing age.
Women have not made efforts to prevent cervical
cancer. This is related to social and cultural factors,
hereditary habits, lack of resources, economic
factors, and inadequate health care facilities
(Ompusunggu & Hill, 2011). The government has
issued a policy on the prevention and early detection
of cervical cancer by using Visual Inspection with
Acetic Acid (VIA). However, some studies suggest
that few women know about the risks and early
detection of cervical cancer (Rosser et al., 2015).
Cervical cancer is still the fourth ranked
affecting women around the world with 527 624
women each year contracting the disease, and 265
672 deaths as a result (Kessler, 2017). There are an
estimated 40,000 new cases of cervical cancer in
Indonesia each year. Indonesia has the highest
number of sufferers of cervical cancer at
approximately 36%. The East Java Province ranked
first for most cases of cervical cancer with a figure
of 21 313 (Ministry of Health, 2015). Data
Lamongan in 2016, positive IVA test data for 169
people, a Pap smear grade II/ III/ IV of 631/8/2 than
2,423 people were examined by the age of 30-50
years (Department of Health, 2016). PHC Data
Lamongan 2016 positive
VIA test data by 73 and the
data pap smear as much as 22 class 1 and class 2 as
many as 65 of the 219 people who checked in with
the number of women of childbearing age by 12 996
people. The Health Promotion Model
by Nola J
Pender focuses on an individual's ability to maintain
its health with the belief that it is better to act to
prevent disease and attempt an action that leads to
the improvement of the condition (Alligod, MR &
Tomey, 2006). Interpersonal factors are sourced
from the family and this group of people is one of
the factors that influences the behavior of women
regarding Pap Smears (Mouttapa et al., 2016).
Situational factors related to access or service may
inhibit or support the behavior of cancer prevention
(Chigbu, Onyebuchi, Ajah, & Onwudiwe, 2013;
Kim et al., 2012). The study (Armini, Kurnia, &
44
Armini, N., Fauziningtyas, R. and Prastiwi, A.
Correlation of Interpersonal Factors, Situational with Cervical Cancer Prevention in Woman of Childbearing Age.
DOI: 10.5220/0008320200440050
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 44-50
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Hikmah, 2016) based on the Health Promotion
Model demonstrates that good personal factors
enhance efforts to prevent cervical cancer. It is
important to follow interpersonal factors and
situational analysis to prevent cervical cancer in
women of childbearing age.
2 METHODS
This study used the Desktriptif-analytic design:
Cross-sectional approach. The population of this
study comprised of 271 people. Samples were taken
from 159 people. The sampling technique used in
this study was probability sampling with simple
random sampling. Independent variables in this
study were interpersonal factors (family, peers, and
health workers) and situational (choice, demand
characteristics, and environment). The dependent
variables in this study are the primary and secondary
preventions of cervical cancer in women of
childbearing age. This study used a questionnaire
instrument. This questionnaire, relating to
interpersonal factors, associated domain suggestions
regarding cervical cancer prevention, social support
that comes from family, peers, and health workers,
and the influence of others who are already taking
steps to prevent cervical cancer. The questionnaire
contained 12 closed questions requiring yes and no
answers. The situational factors associated with the
prevention of cervical cancer were the level of
participation of people living around women of
childbearing age in the prevention of cervical
cancer, the environmental conditions for the
prevention of cervical cancer which contained three
questions with a choice of yes and no answers. The
questionnaire investigated cervical cancer
prevention efforts that have been conducted,
containing nine questions with the possible answers
‘never’, ‘rarely’, and ‘frequently’. The research was
conducted in Puskesmas Lamongan in June–July
2017. The results were analyzed using Spearman's
Rho test with significance level α ≤ 0.05.
3 RESULT
Based on reproductive history, results show that
most respondents had been pregnant <3 times at 110
respondents (69.2%). Most respondents used birth
control; a small proportion were not using
contraception. Most respondents were married at
149 respondents (93.7%), while there were 10
(6.3%) respondents who had never married or were
widowed. The most commonly used contraceptive
was the injection at 92 respondents (57.9%).
Respondents who had used family planning within a
period of <5 years and 5–10 years, respectively, was
47 respondents (29.6%). Regarding the respondents’
age when first experiencing sexual intercourse, 140
respondents (88.1%) were >18 years. The number of
respondents that already knew about cervical cancer
was 107 respondents (67.3%).
There were 37 respondents (23.3%) that had
already done tests, i.e. IVA /Pap smear, while 122
respondents (76.7%) had not done these tests. There
were only two respondents (1.3%) who had been
given the HPV vaccine; this was due to a health pr
program in the workplace.
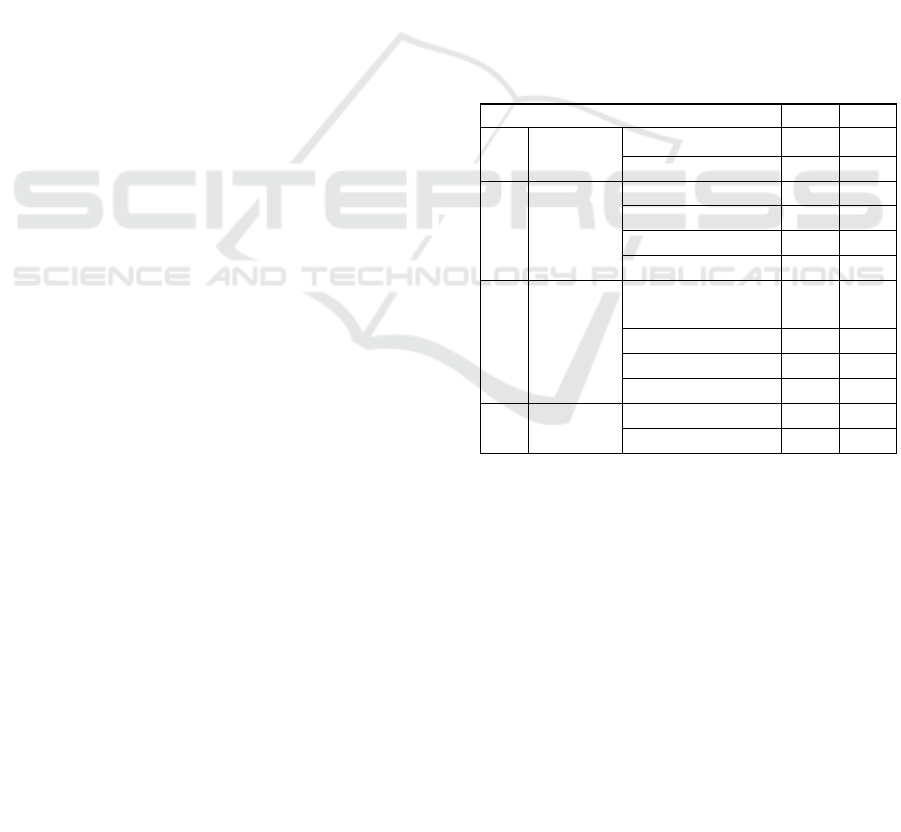
Table 1: Demographic data of respondents (n = 159)
No Demographics f %
1 Age 18–35 years 75 47.2
36–49 years 84 52.8
2 Education Elementary school 17 10.7
Junior high school 23 14.5
Senior high school 85 53.5
College 34 21.4
3 Work Government
officials
6 3.8
Private employees 32 20.1
Traders 23 14.5
Housewives 98 61.6
4 Family
income
<Rp.1.702.780 67 42.1
> Rp.1.702.780 92 57.9
Correlation of Interpersonal Factors, Situational with Cervical Cancer Prevention in Woman of Childbearing Age
45
As many as 78 respondents (49.1%) had low
interpersonal factors and only 37 respondents
(23.3%) were in the high category. Respondents
with situational factors in the medium category were
54 respondents (34%), while 52 respondents
(32.7%) belonged to the higher category. Sufficient
cervical cancer prevention efforts indicated a high
number of 136 respondents (85.5%).
For women of childbearing age, the prevention
of cervical cancer in the ‘sufficient’ category
indicates that 58 people (36.5%) have low
interpersonal relationships. According to the results,
42 people (26.4%) have medium interpersonal
relationships, and only 36 people (22.6%) have high
interpersonal relationships. However, one
respondent (0.6%) showed that a lower level of
cervical cancer prevention efforts proved to
demonstrate high interpersonal relationship factors.
The results from the Spearman rho p = 0.000 H1
indicate that there is a relationship between
interpersonal factors and the prevention of cervical
cancer in women of childbearing age. R = 0.299
indicates an insignificant relationship between the
variables of interpersonal factors and prevention of
cervical cancer in women of childbearing age.
The statistical test results from the Spearman
Rho p = 0.000 H1 accepted that there is a
relationship between situational factors and the
prevention of cervical cancer in women of
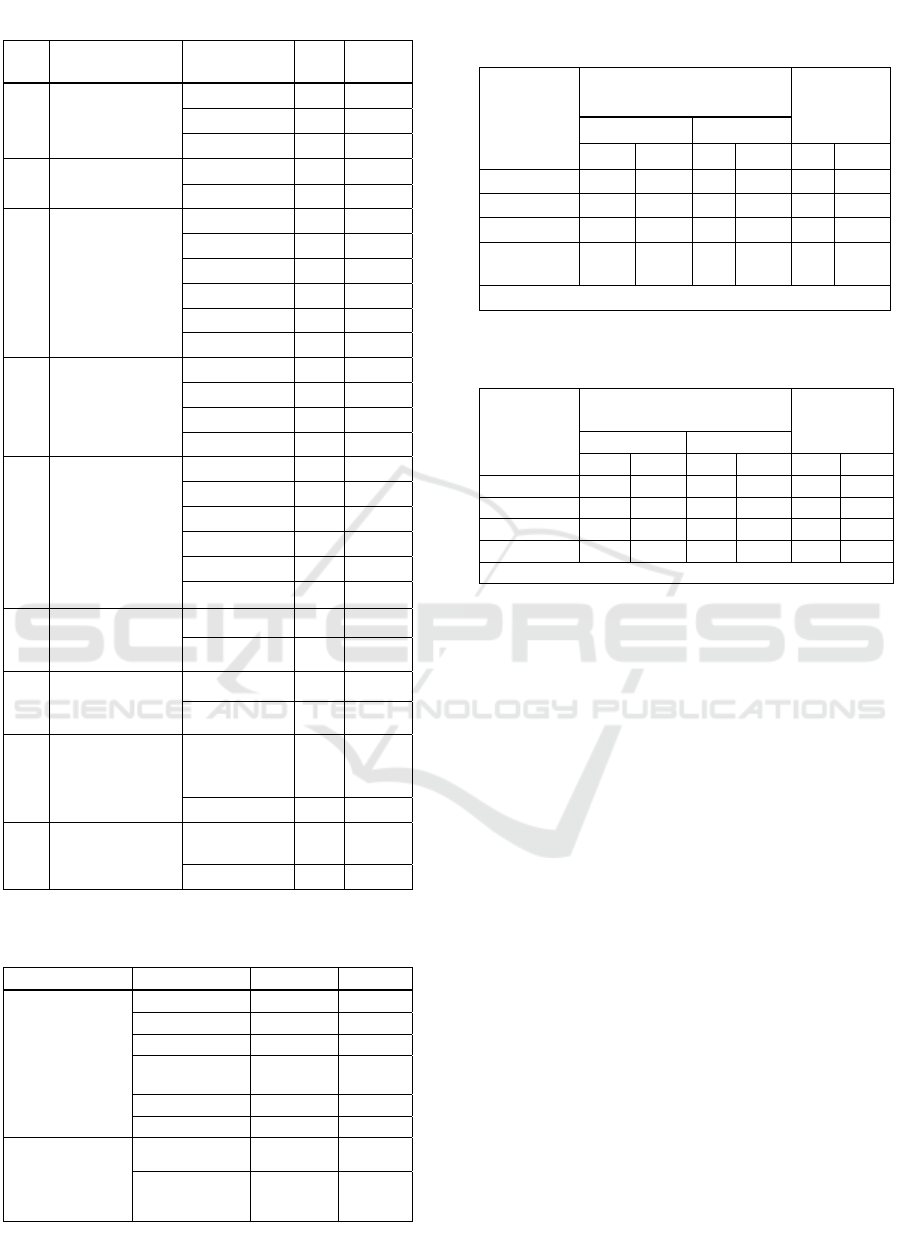
Table 2: Reproductive history (n = 159)
No Characteristics Criteria f %
1. Pregnant
experience
None 7 4.4
<3 times 110 69.2
≥3 times 42 26.4
2. Marital Status married 149 93.7
widowed 10 6.3
3. History of
contraception
used
None 32 20.1
1 type 92 57.9
2 type 26 16.4
3 type 6 3.8
4 type 2 1.3
5 type 1 0.6
4. Period of
contraception
used
None 32 20.1
<5 years 47 29.6
5–10 years 47 29.6
>10 years 33 20.8
5. Type of
Contraception
None 32 20.1
Injection 87 54.7
Oral 21 13.2
Implant 6 3.8
IUD 9 5.7
Tubectomy 4 2.5
6. The first
sexual
intercourse
≤ 18 years 19 11.9
>18 years 140 88.1
7. Knowledge
about cervical
cance
r
Not yet 52 32.7
Knows 107 67.3
8. Assessment
IVA/Pap
Smea
r
Not yet 122 76.7
Yes 37 23.3
9. The HPV
vaccine
Not yet 157 98.7
Yes 2 1.3
Table 3: Interpersonal, situational, and prevention
factors (n = 159)
Variable Criteria f %
Interpersonal
Factors
Low 78 49.1
Mediu
m
44 27.7
Hi
g
h 37 23.3
Situational
Factors
Low 53 33.3
Mediu
m
54 34
High 52 32.7
Cervical
cancer
prevention
efforts
Insufficient 23 14.5
Sufficient 136 85.5
Table 4: Interpersonal relationship factors in the
prevention of cervical cancer (n = 159)
Interperso
nal Factor
Cervical cancer
prevention efforts
Total
Insufficient Sufficient
f % f % ∑ %
Low 20 12.6 58 36.5 78 49.1
Medium 2 1.3 42 26.4 44 27.7
High 1 0.6 36 22.6 37 23.3
Total 23 14.5 13
6
85.5 15
9
100
Spearman rho p = 0.000 r =0.299
Table 5: Relationship of situational factors and the
prevention of cervical cancer (n = 159)
Situational
Factor
Cervical cancer
p
revention efforts
Total
Insufficient Sufficient
f % f %
∑
%
Low 14 8.8 39 24.5 53 33.2
Mediu
m
8 5.0 46 28.9 54 34
Hi
g
h 1 0.6 51 32.1 53 32.7
Total 23 14.5 136 85.5 159 100
S
p
earman rho
p
= 0.000 r =0.283
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
46

childbearing age. R = 0.283 showed that variables in
situational factors and the prevention of cervical
cancer in women of childbearing age have an
insignificant relationship.
4 DISCUSSION
There is a relationship between interpersonal factors
and the prevention of cervical cancer in women of
reproductive age with low levels of relationships in a
category. Most respondents have interpersonal
factors in the low category, but in cervical cancer
prevention efforts in the behavior of respondents is
sufficient. Primary prevention is a healthy behavior
that is generally carried out in everyday life, while
secondary prevention efforts such as IVA
examinations/Pap tests are not done immediately.
Most respondents were educated past high school or
its equivalent, at colleges, or were housewives. A
total of 23 respondents were housewives whose
distance from other houses was great, so the degree
of socialization of such individuals was less and
respondents only gained support from family who
lived at home but did not receive support from
others, such as neighbors or posyandu groups.
According to research by Torres et al. (2013)
communication between group members positively
and negatively affects the screening, encouragement,
and discussion of health problems and can
subsequently influence health-seeking behavior,
causing lower interpersonal factors for prevention
efforts.
Interpersonal factors that are the highest in this
study lie in the domain of social support relating to
family support in the prevention of cervical cancer.
Social support comes from a family able to provide a
positive influence, but the influence of others who
have less impacts prevention efforts. Domain social
support relates to the help given by the family for
the prevention of cervical cancer; husbands are
especially important in influencing the decisions
made by wives or other family members to reduce
the risk of cervical cancer. Some respondents were
health workers who had high interpersonal factors
and can provide information about cancer prevention
efforts.
Interpersonal factors, with the lowest influence
on others who are already making efforts to prevent
cervical cancer, are related to family members who
have previously been tested using IVA /Pap smear.
There were 61 respondents that stated they have
family members who already carry out secondary
prevention and many family members of
respondents who have not done tests using an IVA
/Pap smear.
Regarding marital status, most (149)
respondents are married and the participants’
husbands work as private employees and civil
servants, which facilitates communication between
them. Most husbands can provide support after
knowing the results of the IVA test program (Chigbu
et al., 2013). Families can contribute to the
prevention of cervical cancer by providing support
and motivation (Fallahi, Shahrbabaki, Hashemian, &
Kahanali, 2016). Family support, especially from
female relatives, provides encouragement and
motivation for individuals to perform a pap smear
test (Madhivanan, Valderrama, Krupp, & Ibanez,
2015). Prevention efforts that are sufficient in the
region are supported by the regions' existing
additional service for cervical cancer prevention
conducted by health workers. These are supported
by midwives and assisted by volunteer mothers at
the time of commemorating the cancer world with
lectures. According to research by Rosser, Njoroge
and Huchko (2015), educational interventions to
improve knowledge about cervical cancer can
improve prevention efforts. A total of 140
respondents had sexual intercourse at age >18 years
and 110 respondents have been pregnant <3 times,
reducing the risk of cervical cancer. Being married
and pregnant at an early age means the risk is ≥ 3
times the risk, increasing the incidence of HPV
infection and cervical cancer (Kessler, 2017).
There are several reasons that the 58 respondents
with low interpersonal factors, who make sufficient
effort for the prevention of cervical cancer. These
respondents have the notion that a pap smear
examination is only done when there is a complaint
around the pubic area. Respondents think healthy
conditions do not need to be checked. A total of 107
respondents know about cervical cancer but do not
yet understand fully the information. Thirty-seven
respondents have already done IVA/Pap smear tests,
but the prevention of cervical cancer by respondents
making sufficient efforts rarely pay attention to the
current state of stress and the fact that they rarely
slept for more than eight hours. A total of 37
respondents have already done IVA/Pap smear tests.
This is powered by age, of which most of the
respondents were aged between 21 and 49 years.
According to research by Hajializadeh et al., (2013)
the age range of 21–49 years is associated with Pap
smear test completion.
There were 36 respondents who had a high
degree of interpersonal factors and prevention.
Counseling by health officials and information from
Correlation of Interpersonal Factors, Situational with Cervical Cancer Prevention in Woman of Childbearing Age
47

neighbors who have used the IVA/Pap smear tests
for cervical cancer encourages the respondents to
maintain health so that women of childbearing age
can take steps to prevent cervical cancer early.
Neighboring women can provide a source of social
support for healthcare associated with a Pap smear
examination (Luque, Opoku, Ferris, & Guevara
Condorhuaman, 2016). Level of education also
motivates respondents to take precautions; as many
as 85 respondents were educated past high school or
equivalent and 34 were college educated. Education
has a positive impact on the perception of cervical
cancer in relation to the HPV vaccine (Kwan, Tam,
Lee, Chan, & Ngan, 2011). Levels of education, at
high school level or equivalent, encourage people to
receive new knowledge (Vamos, Calvo, Daley,
Giuliano, & López Castillo, 2015).
Two respondents had the HPV vaccine because
they had a family history of cervical cancer and
experienced reproductive problems. This was
supported by the family income >Rp.1,702,780. The
respondents’ husbands worked as civil servants.
Respondents’ prevention efforts were in the
‘sufficient’ category because many respondents
carried out primary prevention and behavior in
everyday life. Secondary prevention of cervical
cancer is to do tests such as IVA /Pap smear, but
these are rarely done by the respondents; only 37
respondents conducted the IVA/Pap smear tests.
There were respondents who had a low
interpersonal factors but cervical cancer prevention
efforts because respondents obtain information from
mass media and the Internet. Mass media is a useful
tool for encourage testing IVA/Pap smear (De Vito
et al., 2014).
There is a relationship between situational
factors and the prevention of cervical cancer in
women of childbearing age. Situational factors that
have a relationship in this study relate to of
environmental conditions for the prevention of
cervical cancer in the region where there are
community health clinics and health centers within
the region tersebuat Lamongan ± 2 km. Factors that
influence is less domain the level of participation of
people living around women of childbearing age in
the prevention of cervical cancer because some
respondents were confused when filling out
questionnaires on these domains because they did
not know many women who had already had the
IVA/Pap smear test.
Some respondents already knew about cervical
cancer prevention program. Some were told by
family members, or volunteers when filling out the
questionnaire. Situational factors were included in
the low category because most respondents hesitated
when answering whether neighbors or mothers in the
residential area already had IVA/Pap smear tests.
There were 51 respondents who had sufficient
situational factors and prevention. This was because
respondents knew that there are programs such as
the IVA test/Pap smear close to the residence of
respondents. When experiencing reproductive
problems, respondents immediately went to visit the
healthcare center, but inside the house, there are
family members who smoke, thus affecting cervical
cancer prevention efforts. Healthcare providers can
influence and educate the reduction of incidences of
cervical and breast cancer (Schoenberg, Kruger,
Bardach, & Howell, 2013). The higher the
situational factors, the higher the prevention of
cervical cancer. Improved healthcare facilities will
have a major impact on the prevention of cervical
cancer (Rosser et al., 2015).
Some respondents (53) hesitated when filling in
the level of participation of people living around
women of childbearing age in the prevention of
cervical cancer. Some respondents were confused
when filling out the questionnaires in these areas
because they did not know the information regarding
women of childbearing age in the neighborhood that
had taken the IVA/Pap smear tests.
There were 39 respondents that had low
situational factors and take steps to prevent cervical
cancer in the ‘sufficient’ category. Making an effort
to prevent cervical cancer is a behavior that is often
performed in daily life but lower situational factors
of respondents means that if there are health
problems that are not life-threatening, they do not
need to check with the health clinic and are only
given herbal medicine. When experiencing vaginal
discharge or itching in the area around the genitals,
respondents did not check into the health clinic
because of their perception of it being a natural
condition. Beliefs, behaviors, and stressors affect
individuals in the prevention of cervical cancer
(Daley et al., 2011).
Regarding available options in the prevention of
cervical cancer, there were 96 respondents that never
check their health with the health services. Some
respondents had health problems related to
reproductive issues. Types of birth control used by
the respondents, as many as 87 types of injections
and a history of contraceptive use many types of
birth control use 1 as much as 92 response.
Injections have side effects if used for a long time.
Forty-seven respondents used contraception <5 years
and 47 respondents used contraception for 5–10
years. Hormonal contraception can cause adverse
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
48

effects on reproductive disorders and weight-gain
issues, pushing the respondents to make visits to the
healthcare service (Simmons & Edelman, 2016;
Wiebe, Brotto, & MacKay, 2011).
5 CONCLUSIONS
Most women of childbearing age have low
interpersonal factors; the family/husband, neighbors,
close friends and health workers still offer little
support in the prevention of cervical cancer in
Puskesmas, Lamongan. Various situational factors
show almost an equal number of available options:
the level of community participation and
environmental conditions. Cancer prevention efforts
are mostly in the category of pretty. Almost all have
done to prevent cervical cancer primary prevention
of secondary, but many are not doing. Low
interpersonal factors that will inhibit cancer
prevention efforts. Situational factors are almost
balanced by the options available: the level of
community participation and environmental
conditions will support efforts to prevent cervical
cancer in women of childbearing age, in the working
area of Puskesmas Lamongan.
ACKNOWLEDGEMENT
The researchers would like to thank the Faculty of
Nursing, Universitas Airlangga for the publication
and all the women of childbearing age who devoted
their time and willingness to participate.
REFERENCES
Alligod, M.R & Tomey, A. (2006). Nursing Theorist and
Their Work. 6th. Missouri: Mosby.
Chigbu, C. O., Onyebuchi, A. K., Ajah, L. O., &
Onwudiwe, E. N. (2013). Motivations and preferences
of rural Nigerian women undergoing cervical cancer
screening via visual inspection with acetic acid.
International Journal of Gynecology & Obstetrics,
120(3), 262–265.
http://doi.org/10.1016/j.ijgo.2012.10.011
Daley, E., Alio, A., Anstey, E. H., Chandler, R., Dyer, K.,
& Helmy, H. (2011). Examining barriers to cervical
cancer screening and treatment in florida through a
socio-ecological lens. Journal of Community Health,
36(1), 121–131. http://doi.org/10.1007/s10900-010-
9289-7
De Vito, C., Angeloni, C., De Feo, E., Marzuillo, C.,
Lattanzi, A., Ricciardi, W., … Boccia, S. (2014). A
large cross-sectional survey investigating the
knowledge of cervical cancer risk aetiology and the
predictors of the adherence to cervical cancer
screening related to mass media campaign, 2014.
http://doi.org/10.1155/2014/304602
Dinkes. (2016). Rekapitulasi deteksi dini kanker payudara
dan kanker leher rahim puskesmas se-kabupaten
Lamongan. Lamongan.
Fallahi, A., Shahrbabaki, B. N., Hashemian, M., &
Kahanali, A. A. (2016). The needs of women referring
to health care centers for doing pap smear test, 19(6).
Febriani, C. A. (2016). Faktor-faktor yang berhubungan
dengan deteksi dini kanker leher rahim di kecamatan
gisting kabupaten tanggamus lampung, VII, 228–237.
Ginsburg, O., Bray, F., Coleman, M. P., Vanderpuye, V.,
Eniu, A., Kotha, S. R., … Message, U. S. G. (2016).
The global burden of women’s cancers: a grand
challenge in global health. The Lancet, 0(0), 743–800.
http://doi.org/10.1016/S0140-6736(16)31392-7
Hajializadeh, K., Ahadi, H., Jomehri, F., & Rahgozar, M.
(2013). Psychosocial predictors of barriers to cervical
cancer screening among Iranian women: the role of
attachment style and social demographic factors.
Journal of Preventive Medicine and Hygiene, 54(4),
218–22.
Kemenkes. (2015). Stop Kanker. infodatin-Kanker.
Jakarta.
Kessler, T. A. (2017). Cervical Cancer: Prevention and
Early Detection. Seminars in Oncology Nursing.
http://doi.org/10.1016/j.soncn.2017.02.005
Armini, N. K. A., Kurnia, I. D., & Hikmah, F. L. (2016).
Personality Factor , Self Efficacy and Prevention of
Cervical Cancer among Childbearing Age Women.
Jurnal Ners, 11(2), 294–299.
Kim, Y.-M., Ati, A., Kols, A., Lambe, F. M., Soetikno, D.,
Wysong, M., … Lu, E. (2012). Influencing Women’s
Actions on Cervical Cancer Screening and Treatment
in Karawang District, Indonesia. Asian Pacific Journal
of Cancer Prevention, 13(6), 2913–2921.
http://doi.org/10.7314/APJCP.2012.13.6.2913
Kwan, T. T. C., Tam, K. fai, Lee, P. W. H., Chan, K. K.
L., & Ngan, H. Y. S. (2011). The effect of school-
based cervical cancer education on perceptions
towards human papillomavirus vaccination among
Hong Kong Chinese adolescent girls, 84(1), 118–122.
http://doi.org/10.1016/j.pec.2010.06.018
Luque, J. S., Opoku, S., Ferris, D. G., & Guevara
Condorhuaman, W. S. (2016). Social network
characteristics and cervical cancer screening among
Quechua women in Andean Peru, 16(1).
http://doi.org/10.1186/s12889-016-2878-3
Madhivanan, P., Valderrama, D., Krupp, K., & Ibanez, G.
(2015). Family and cultural influences on cervical
cancer screening among immigrant Latinas in Miami-
Dade County, USA, 18(6), 710–722.
http://doi.org/10.1080/13691058.2015.1116125
Mouttapa, M., Park Tanjasiri, S., Wu Weiss, J., Sablan-
Santos, L., DeGuzman Lacsamana, J., Quitugua, L.,
… Vunileva, I. (2016). Associations Between
Women’s Perception of Their Husbands’/Partners’
Correlation of Interpersonal Factors, Situational with Cervical Cancer Prevention in Woman of Childbearing Age
49

Social Support and Pap Screening in Pacific Islander
Communities. Asia Pacific Journal of Public Health,
28(1), 61–71.
http://doi.org/10.1177/1010539515613412
Ompusunggu, F., & Bukit, E. K. (2011). Karkteristik,
hambatan wanita usia subur melakukan pap smear di
puskesmas kedai durian, 20–24.
Rosser, J. I., Njoroge, B., & Huchko, M. J. (2015).
Knowledge about cervical cancer screening and
perception of risk among women attending outpatient
clinics in rural Kenya. International Journal of
Gynecology and Obstetrics, 128(3), 211–215.
http://doi.org/10.1016/j.ijgo.2014.09.006
Schoenberg, N. E., Kruger, T. M., Bardach, S., & Howell,
B. M. (2013). Appalachian women’s perspectives on
breast and cervical cancer screening., 13(3), 2452.
Simmons, K. B., & Edelman, A. B. (2016). Hormonal
contraception and obesity. Fertility and Sterility,
106(6), 1282–1288.
http://doi.org/10.1016/j.fertnstert.2016.07.1094
Torres, E., Erwin, D. O., Treviño, M., & Jandorf, L.
(2013). Understanding factors influencing Latina
women’s screening behavior: A qualitative approach,
28(5), 772–783. http://doi.org/10.1093/her/cys106
Vamos, C. A., Calvo, A. E., Daley, E. M., Giuliano, A. R.,
& López Castillo, H. (2015). Knowledge, Behavioral,
and Sociocultural Factors Related to Human
Papillomavirus Infection and Cervical Cancer
Screening Among Inner-City Women in Panama.
Journal of Community Health, 40(6), 1047–1056.
http://doi.org/10.1007/s10900-015-0030-4
Wiebe, E. R., Brotto, L. A., & MacKay, J. (2011).
Characteristics of Women Who Experience Mood and
Sexual Side Effects With Use of Hormonal
Contraception. Journal of Obstetrics and Gynaecology
Canada, 33(12), 1234–1240.
http://doi.org/10.1016/S1701-2163(16)35108-8
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
50
