
The Effect of Catheter Associated Urinary Tract Infection (CAUTI)
Bundle of Care: A Systematic Review
Wardah Fauziah
1
, Nana Rochana
1
and Achmad Zulfa Juniarto
2
1
Department of Nurse, Faculty of Medicine, Diponegoro University, Semarang, Indonesia
2
Faculty of Medicine, Diponegoro University, Semarang, Indonesia
Keywords: Catheter, Care, CAUTI Bundle.
Abstract: The aim of this paper was to determine the effect of CAUTI bundle of care in reducing and preventing the
incidence of CAUTI. The inclusion criteria of this review were; experimental studies, adult patients as
samples, and urinary catheter installation for a minimum period of 72 hours; while the exclusion criteria was
patients with worsening conditions. The literature search was done through 6 bibliography databases
(CINAHL, Scientdirect, Proquest, Pubmed, Google Scholar and MEDLINE) from 2014 to 2018 in English
language using the keywords; CAUTI, urinary catheter, protocol, guideline, and bundle of care. A total of
171 articles had been identified but after the selection process, only 6 articles met the criteria. The selected
articles then were critically appraised using Critical Appraisal Skill Program (CASP). The result showed
that CAUTI bundle of care had a significant effect to reduce and prevent CAUTI. The CAUTI bundle
consisted of assessment, aseptic technique, catheter care, catheter removal if there was no further indication,
and catheter selection. This review recommends that the CAUTI bundle of care should be implemented in
Indonesia, in which no prior published study reported, for the best evidence of care.
1 INTRODUCTION
The Center of Diseases Control and Prevention
(CDC) defines Catheter Associated Urinary Tract
Infection (CAUTI) as an infection in patients who
have or still use an indwelling catheter. (Fletcher,
Tyszka, Jeanne T. Harrod, Molly. Fowler, Karen E.
Fowle. Saint, Sanjay. Krein, 2016). The biggest risk
factor is the use of catheters exceeding 6 days; it can
be said that CAUTI occurs because of long-term
catheter placement, not in accordance with the
indications and lack of aseptic procedures during
catheterization, both on the device and the medical
staff (Theobald, Resnick, Dittus, & Roumie, 2017).
The impact of CAUTI is the duration of hospital
stay, unnecessary morbidity and motility, and
increased costs for hospital care. Patients taking
catheters have a 3 times greater risk of being
hospitalized for longer periods of time and longer
antibiotic use, even reports say that the organism
that causing Urinary Tract Infection (UTI) due to
catheterization is an organism that has been resistant
to many antibiotics. If it is not immediately treated,
it will cause urosepsis and even death which reaches
9,000 cases per year. It is estimated that 17% - 69%
of UTI due to catheterization can be prevented by
good infection control (Semaradana, 2014).
Lee (2017) states that the incidence of catheter-
related urinary tract infections (CAUTI) was 30% of
the overall incidence of infections in hospitals in
Singapore (Lee, 2017). Catheter use is the most
common cause of urinary tract nosocomial
infections. The risk of bacteriuria is related to the
length of catheterization. The risk of bacteriuria
increases by 5-10% per day after catheter placement.
Bacteria can occur 90-100% in long-term catheter
use. Bacteria that occur are usually asymptomatic
(Tarmono, Renaldo, & Ghinorawa, 2015).
Some evidence based interventions had been
reported to reduce CAUTI incidences (Saint et al.,
2009). These interventions then were developed by
CDC becoming a bundle of care as a guidelines.
This guideliness is called CAUTI bundle of care.
(Josephine Anne Navoa-Nga, Regina Berbab, Victor
D. Rosenthalc,∗, Victoria D. Villanuevaa, María
Corazon V. Tolentinoa, Glenn Angelo S. Genuinob,
Rafael J. Consunjib, 2013)(Josephine Anne Navoa-
Nga, Regina Berbab, Victor D. Rosenthalc, Victoria
D. Villanuevaa, María Corazon V. Tolentinoa,
Fauziah, W., Rochana, N. and Juniarto, A.
The Effect of Catheter Associated Urinary Tract Infection (CAUTI) Bundle of Care: A Systematic Review.
DOI: 10.5220/0008205901230131
In Proceedings of the 1st International Conference of Indonesian National Nurses Association (ICINNA 2018), pages 123-131
ISBN: 978-989-758-406-0
Copyright
c
2020 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
123
Glenn Angelo S. Genuinob, Rafael J. Consunjib,
2013).
Futhermore, some studies showed that CAUTI
bundle of care decreased CAUTI occurence
significanly.(Al-Hameed Fahad, Ahmed Gulam , Al-
Saedi Asim & Al-Hameed Faisal, 2018)(Mody et al.,
2017)(Sushilkumar Satish Gupta; Pavan Kumar
Irukulla; Mangalore Amith Shenoy; Vimbai
Nyemba; Diana Yacoub, 2017)(Josephine Anne
Navoa-Nga, Regina Berbab, Victor D. Rosenthalc,∗,
Victoria D. Villanuevaa, María Corazon V.
Tolentinoa, Glenn Angelo S. Genuinob, Rafael J.
Consunjib, 2013)(Regagnin, , Debora Schettini da
Silva Alves, Ana Maria Cavalheiro, Thiago Zinsly
Sampaio Camargo, Alexandre R. Marra, Victor, &
Edmond, 2015). However, the effect of CAUTI
bundle of care on the CAUTI incidence is still
limited. Therefore, this review aims to determine the
effect of CAUTI bundle of care in reducing and
preventing the incidence of CAUTI.
2 METHODS
The inclusion criteria of this review were;
experimental studies, adult patients as samples, and
urinary catheter installation for a minimum period of
72 hours; while the exclusion criteria were patients
with worsening conditions. The literature search was
done through 6 bibliography databases namely
Cumulative Index to Nursing and Allied Health
Literature (CINAHL), Scientdirect, Proquest,
Pubmed, Google Scholar and Medical Literature
Analysis and Retrieval System (MEDLINE) from
2014 to 2018 in English language The search used
keywords; CAUTI, urinary catheter, protocol,
guidelines, and bundle of care. A total of 171 articles
have been identified but after the selection process,
only 6 articles met the criteria. The selected articles
uses PICO (population, intervention, comparisons,
and outcomes) and were then critically appraised
using the Critical Appraisal Skill Program (CASP).
The author evaluated the title and abstract of all
references. List of references from articles was
sought manually by searching for research relevant
to other inclusion criteria. Data extraction was done
using Microsoft Word. Information obtained from
each study included the following: title, journal, year
of publication, location, study population, study
design, time of intervention, characteristics of the
intervention and control groups, measurement tools,
and pre and post intervention results was shown on
table 1.
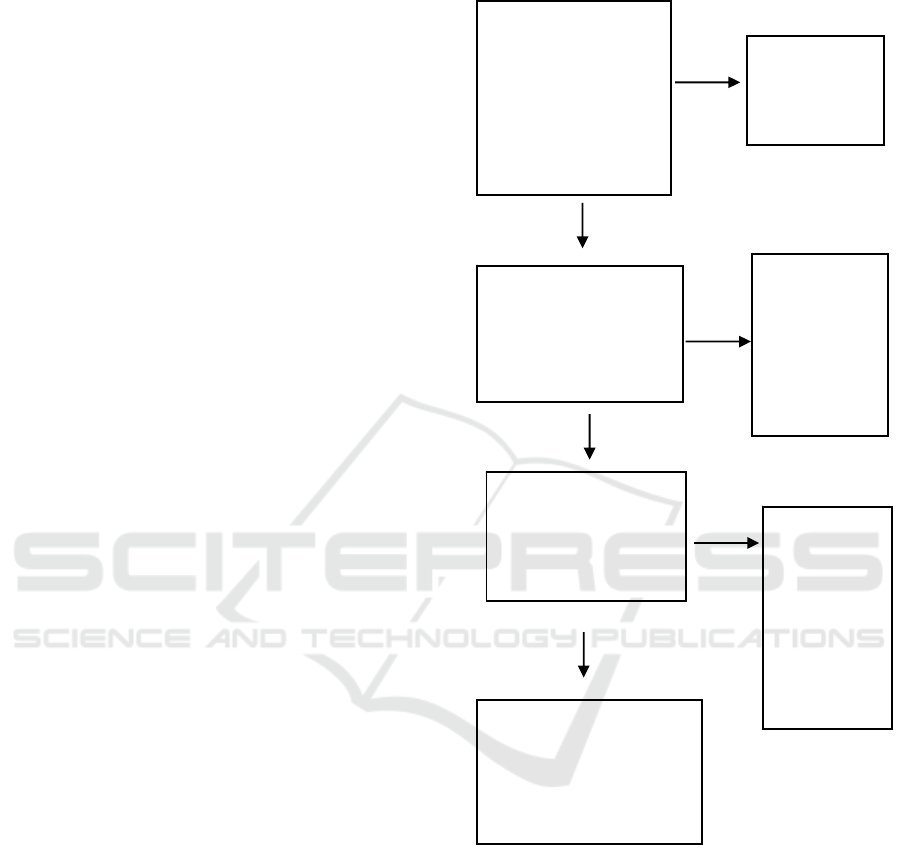
The following figure 1 shows the search strategy
and pre selection process carried out in this study:
Recordidentified
throughdatabase:
CINAHL,MEDLINE,
Scientdirect,
Proquest,Pubmed
andGoogleScholar
(n=171)
Excludedtitle
andabstract
(n=97)
Relevantarticlesforthis
review
(n=74)
Excludedby
inclusionand
exclusion
criteria(n=67)
Protocol
excluded
low‐quality
ornospesific
data(n=2)
IncludeStudies
(n=5)
Relevantarticlesafter
screening(n=7)
Figure 1: Searching Strategy.
3 RESULTS
3.1 Effect of CAUTI Bundle of Care
A total 171 studies were initially identified as
results. After filtered by abstract and title total
studies, excluded by criteria inclusion and exclusion
and Protocol excluded low-quality or no spesific
data total studies were reviewed 5 studies.
The results showed that 3 out 5 of studies had
level II of evidence with good quality and two
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
124

studies had level III with good quality and low
quality data or major flaws. No study had high level
of evidence (level I).
Table 2 described the effect of CAUTI bundle of
care. The CAUTI rate decreased significanly with
the average of rates CAUTI mean pre implemention
7,90%, mean post 1,18% and mean difference 5,
59%. All studies had p value significant effect
CAUTI rates after interventions.
Population and sample performed of studies that
4 out 5 had at ICU and one studies medical surgical.
3.2 CAUTI Bundle of Care
The CAUTI of care Bundle consists of several
interventions that are interrelated with each other,
from several studies reviewed the interventions
carried out include, There bundles were: The use of
a catheter is only for the right indication, The use of
appropriate techniques for catheter placement,
Proper catheter care (antimicrobial urine catheter
can prevent bacteriuria in hospitalized patients
during short-term catheterization, depending on the
antimicrobial layer and several other variables
compared to standard catheters), Noting the use of
catheter material (choosing the right catheter aims to
delay the onset of bacteriuria and to prevent
bacterial attachment and growth), Obstruction
management (there is no consensus regarding the
time at which routine catheter changes must be
made. Shorter periods may be needed if there is
damage or catheter leakage. In general, long-term
catheters must be replaced before blockages occur or
may occur. Time of indwelling catheter use different
for each patient, some patients form deposits on the
lumen of the catheter very quickly), Specimen
Collection (get aseptic urine samples), Small
amounts of fresh urine can be taken from the distal
part of the catheter, or if it is better than the place
where the material is available, and before urine is
aspirated with sterile needles and syringes, the place
of extraction must be disinfected (if a large volume
of urine is needed for special analysis, then the urine
must be taken aseptically from the drainage bag and
routine urine culture in patients with asymptomatic
catheters is not recommended).
4 DISCUSSION
4.1 Effect of CAUTI Bundle of Care
The effect CAUTI of care bundle that has shown
that developing nurse driven protocol interventions
show that interventions has made the decline in
urinary catheter use from 37.6% to 26.3%, and
provide education about the diagnosis and definition
of CAUTI. increasing the right identification ability
so that the given antibiotic therapy is right, and the
last one using the CAUTI prevention bundles, one of
the studies conducted in America states that there
has been a decrease in the average CAUTI incidence
of 50% per month and a decrease from 5.41 to 2.49
per 1000 catheter days (Peter, Devi, & Nayak,
2018). While a study conducted by Al-Hameed
showed the results of the rate of UTI and the use of
urinary catheters during the study decreased the rate
of UTI significantly per 1000 days catheter from 2.3
to 0.3 (Al-hameed et al., 2018). Then another study
conducted by Navoa et al in 2013 showed the effect
of CAUTI of care bundle intervention on the
incidence of CAUTI from 11.0 to 2.66 per 1000
catheter days (Josephine Anne Navoa-Nga, Regina
Berbab, Victor D. Rosenthalc, Victoria D.
Villanuevaa, María Corazon V. Tolentinoa, Glenn
Angelo S. Genuinob, Rafael J. Consunjib, 2013)
Bundle CAUTI of care is some of the
interventions conducted to prevent the incidence of
CAUTI, which is a combination of several
interventions based on evidence practice
nursing.(Lona Mody,M Todd Greene, Jennifer
Meddings, Sarah L Krein, Sara E McNamara,
Barbara W Trautner, David Ratz, Nimalie D Stone,
LillianMin, Steven J Schweon, Andrew J Rolle,
RussellN Olmsted, Dale R Burwen, James Battles,
Barbara Edson, 2017)
Other studies show significant results between
bundles CAUTI of care for UTI rates, such as the
research conducted by Lona Mody in 2017, a decline
in UTI rate from 6.78 to 2.63 per 1000 catheter-days
(Mody et al., 2017). The study conducted by
Sushilkumar et al also showed significant results
between interventions carried out on the UTI rate of
5.47 before intervention to 1.08 per 1000 catheter-
days. (Sushilkumar Satish Gupta, Pavan Kumar
Irukulla, Mangalore Amith Shenoy, Vimbai
Nyemba, Diana Yacoub, 2017)
4.2 CAUTI Bundle of Care
An integrative review conducted by Michelle Henry
(2018) to evaluate Evidence Based Practice
preventive measures for infections that occur due to
catheter placement (CAUTI) in critical care settings.
The recommended intervention to prevent the
occurrence of CAUTI is the use of urine samples to
identify CAUTI in patients who have fever, some
studies recommend patient hand hygiene protocols
The Effect of Catheter Associated Urinary Tract Infection (CAUTI) Bundle of Care: A Systematic Review
125
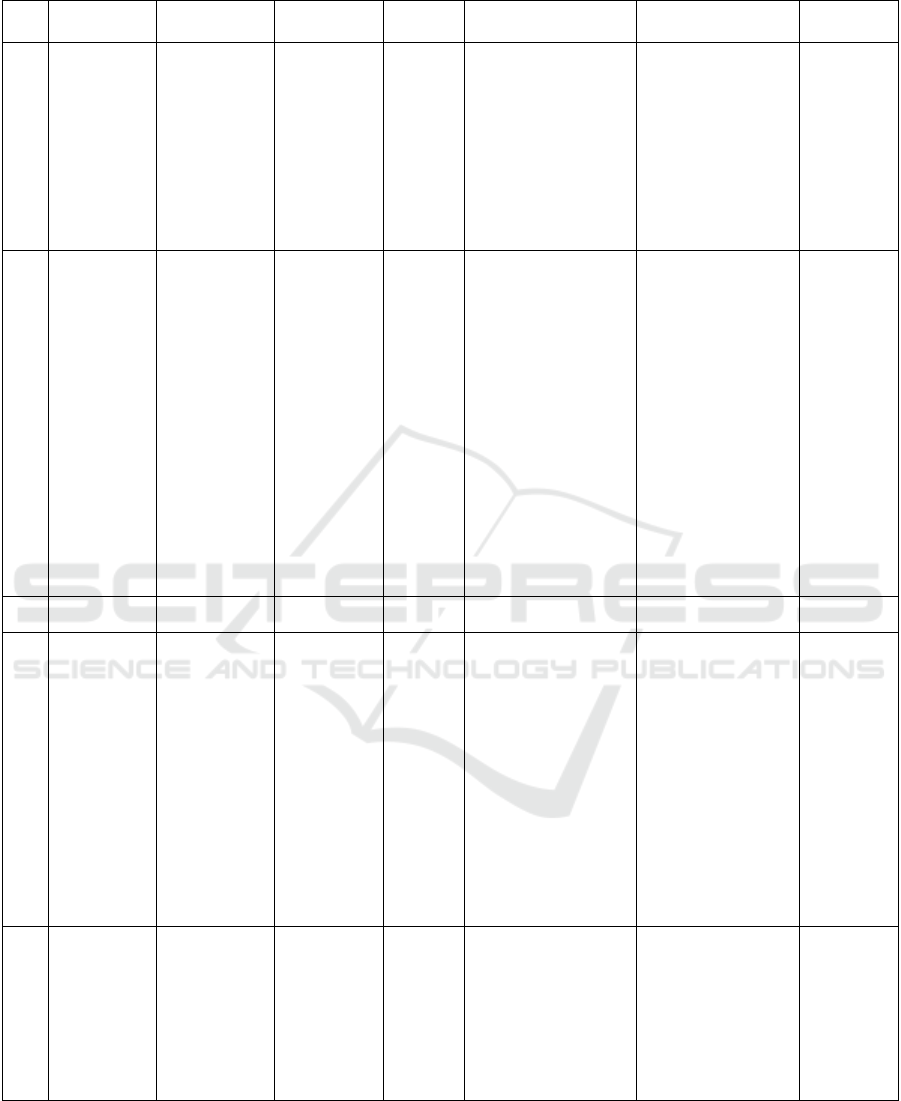
Table 1: Extract Data.
No Author/Year Title
Sample
Population
Reseacrh
Design
Methods Outcome
Level Of
Evidence
1
Fahad M. Al-
Hameed, Gulam
R. Ahmed,
Asim A. AlSaedi,
Muhammad J.
Bhutta,
Faisal
Al-Hameed,
Majid M. Al
Shamrani, 2018
Applying
preventive
measures leading
to significant
reduction of
catheter-
associated urinary
tract infections in
adult intensive
care unit
ICU
quasy
experimental
-retropective
study
The proper use of silicon
catheter, aseptic insertion
technique, emptying bag
three-fourth via close
circuit, the use of
appropriate size catheter,
securing the draining tube
on the thigh to keep catheter
b
ag below patient’s bladder
level and removal of the
catheter as early as possible
were ensured in all patients.
The Rate of CAUTI
significant reduction from
2.3 to 0.3 per 1000
catheter days.
II-B
2
Josephine Anne
Navoa-Nga,
Regina Berbab,
Victor D.
Rosenthalc,
Victoria D.
Villanuevaa,
María Corazon
V. Tolentinoa,
Impact of an
International
nosocomial
Infection Control
Consortium
multidimensional
approach on
catheter-associated
urinary tract
infections in
Patients
characteristics
such as UC
duration mean,
surgical stay,
pulmonary
disease,
abdominal
surgery, cancer,
endocrine
metabolic
diseases, renal
quasy
experiment-
Prospektive
Perform hand hygiene (HH)
before insertion and
manipulation of a UC,
Maintain unobstructed urine
flow; i.e., UC on thigh
without strangulating, Keep
the collecting bag below the
level of the bladder at all
times; i.e., UC with
collecting bag hanging and
not allowing urine reflux,
Empty the collecting bag
regularly and to avoid
allowing the draining spigot
to touch the collecting
container and to monitor
CAUTIs using standardized
criteria to identify patients
with CAUTIs and to collect
UC-days as denominators.
Urinary Catheter use mean
0,67. The rate of CAUTI
was 11,0 days per 1000
UC-days at baseline and
decreased 2,66 per UC-
days after interventions.
II-B
No Author/Year Title
Sample/
Population
Reseacrh
Design
Methods Outcome
Level Of
Evidence
3
Glenn Angelo S.
Genuinob, Rafael
J. Consunjib,
Jacinto Blas V
2013
adult intensive
care units in the
Philippines:
International
Nosocomial
Infection Control
Consortium
(INICC) findings
impairment, and
immune-
compromised
condition, were
similar during
both periods.
However,he
mean age of
patients,
proportion of
women, and
presence of
previous
infections were
higher during the
interventions
p
eriods
4
Lona Mody,;
M.Todd Greene,
Jennifer
Meddings
2017
A National
Implementation
Project to Prevent
Catheter
Associated Urinary
Tract Infectionin
Nursing Home
Residents
Older adults
nursing home.
ICUs and SDUs
(Step Down
Units)
experimental
study-
prospective
Catheter removal, aseptic
insertion, using regular
assessments, training for
catheter care, and
incontinence care planning,
as well as a socio adaptive
bundle emphasizing
leadership, resident and
family engagement, and
effective communication.
The rate of CAUTI
decreased from 6.78 to
2.63 infections per 1000
catheter-days.
II-B
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
126
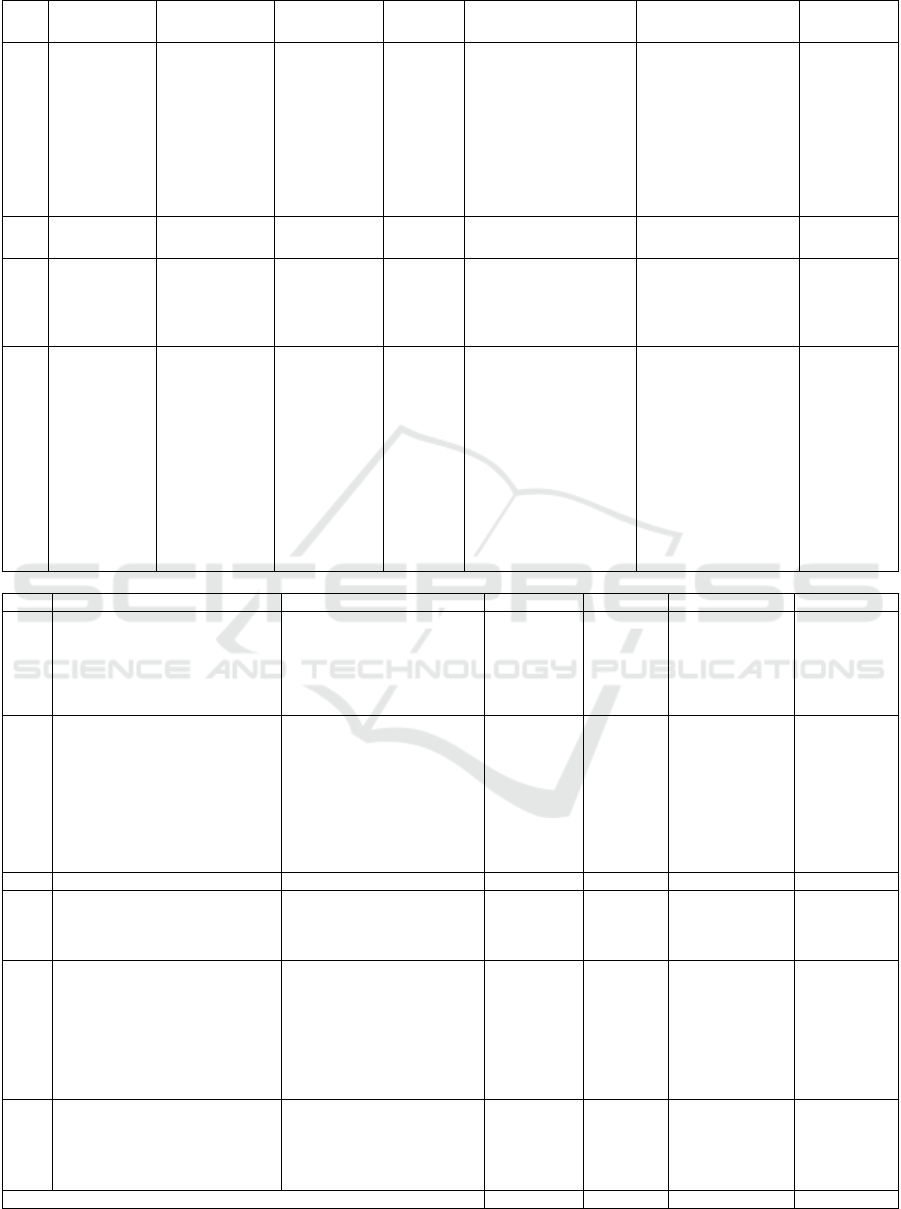
Table 1: Extract Data. (cont.)
No Author/Year Title
Sample/
Population
Reseacrh
Design
Methods Outcome
Level Of
Evidence
5.
Dejanira A.
Regagnin,
Debora Schettini
da Silva Alves,
Ana Maria
Cavalheiro,
Thiago Zinsly
Sampaio
Camargo,
Alexandre.
Sustainability of a
program for
continuous
reduction of
catheter-associated
urinary tract
infection
Medical-surgical
intensive care
unit and step
down unit.
quasy
experimental
study
ICU nurses and physicians
inserted urinary catheter,
remove made solely by the
patients’s physician,
catheter insertion audited,
process measures audited,
urinary catheter insertion
cart implemented, Nurse
appointed exclusively for
CAUTI prevention,
The rate of CAUTI in the
ICUs was 0,9 per 1,000
catheter days, and the
SDUs the rate was 1,0
UTI per 1,000 catheter
days.
III-B
No Author/Year Title
Population/
Sample
Research
Design
Methods Outcome Mean
6.
Marra, Elivane
da Silva Victor,
Michael B.
Edmond.
2015
intensification of audits, and
catheter insertion team
developed.
7.
Sushilkumar
Satish Gupta,
Pavan Kumar
Irukulla,
Mangalore Amith
Shenoy, Vimbai
Nyemba, Diana
Yacoub, Yizhak
Kupfer
2016
Successful strategy
to decrease
indwelling catheter
utilization rates in
an academic
medical intensive
care unit
ICU
quasy
experimental
-
retrospective
observationa
l study
to permit IUC use only in
the following predetermined
indications, futher narrow
down the criteria for urinary
catheter utilization to
urinary retention and
genitourinary procedures
only, and use sonographic
b
ladder scanning to identify
high-risk patients who may
need indwelling catheters in
the near future.
IUC utilization rasio had a
statistically significant
decrease from 0,92
(baseline) to 0,28 (after 3
interventions) (P <,0001).
The CAUTI rates had a
statistically significant
decrease from 5,47
(baseline) to 1,08 (after 3
interventions) (P=,0134).
III-C
No. Title Author Mean Pre Mean Post Mean Difference P
1.
Applying preventive measures
leading to significant reduction of
catheter-associated urinary tract
infections in adult intensive care
unit
Fahad M. Al-Hameed, Gulam
R. Ahmed,
Asim A. AlSaedi, Muhammad
J. Bhutta,
Faisal Al-Hameed, Majid M. Al
Shamrani,
2,3 % 0,3%
2%
0,001
2.
Impact of an International
Nosocomial Infection Control
Consortium multidimensional
approach on catheter-associated
urinary tract infections in adult
intensive care units in the
Philippines: International
Nosocomial Infection Control
Consortium (INICC) findings
Josephine Anne Navoa-Nga,
Regina Berbab, Victor D.
Rosenthalc, Victoria D.
Villanuevaa, María Corazon V.
Tolentinoa, Glenn Angelo S.
Genuinob, Rafael J. Consunjib,
Jacinto
Blas V
11 % 2,66% 8,34%
0,0001
No. Title Author Mean Pre Mean Post Mean Difference P
3.
A National Implementation Project
to Prevent Catheter Associated
Urinary Tract Infectionin Nursing
Home Residents
Lona Mody, M.Todd Greene,
Jennifer Meddings
6,78% 2,63% 4,15% < ,0001
4.
Sustainability of a program for
continuous reduction of catheter-
associated urinary tract infection
Dejanira A. Regagnin, Debora
Schettini da Silva Alves, Ana
Maria Cavalheiro, Thiago
Zinsly Sampaio Camargo,
Alexandre R. Marra, Elivane da
Silva Victor, Michael B.
Edmond.
ICU :7 %
SDU:14,9%
0,9%
1%
ICU; 6,1 %
SDU; 13,9%
All test of
statistical
significance
were 2-sided,
with the
significance
level set at
P
<,05.
5.
Successful strategy to decrease
indwelling catheter utilization rates
in an academic medical intensive
care unit
Sushilkumar Satish Gupta,
Pavan Kumar Irukulla,
Mangalore Amith Shenoy,
Vimbai Nyemba, Diana
Yacoub, Yizhak Kupfer
5,47% 0,78% 4,69%
< .0001
Average of Mean 7.90 % 1,18% 5,59%
The Effect of Catheter Associated Urinary Tract Infection (CAUTI) Bundle of Care: A Systematic Review
127

(PHHP) as one of the interventions that must be
done to prevent CAUTI, some studies also
recommend strategies for preventing CAUTI
focusing on limiting the use and duration of catheter
installation, the use of aseptic techniques for catheter
insertion and catheter care, then a study (Henry,
2018) only for people in need, ensure that only
competent and experienced people do catheter
installation, use sterile equipment, keep the drainage
system closed, maintain urine flow, maintain hand
hygiene before and after put on a catheter.
(Sushilkumar Satish Gupta; Pavan Kumar Irukulla;
Mangalore Amith Shenoy; Vimbai Nyemba; Diana
Yacoub, 2017). Meanwhile the research conducted
by Vicki Parker etc states that CAUTI bundle care is
divided into several components which are
abbreviated to NOCAUTI namely need for catheter
assessed, Obtain the patient consest, Competency,
Asepsis, Unobstructed flow, Timely catheter,
Infection risk daily periurethal hygiene. (Lona
Mody,M Todd Greene, Jennifer Meddings, Sarah L
Krein, Sara E McNamara, Barbara W Trautner,
David Ratz, Nimalie D Stone, LillianMin, Steven J
Schweon, Andrew J Rolle, RussellN Olmsted, Dale
R Burwen, James Battles, Barbara Edson, 2017)
Then another study stated that bundle care to
prevent CAUTI consisted of Hand hygiene before
catheter placement, maintaining urinary
unobstructed flow, keeping the catheter sac under
the bladder, emptying the bladder, and monitoring
CAUTI using standard criteria to identify patients
with CAUTI. (Josephine Anne Navoa-Nga, Regina
Berbab, Victor D. Rosenthalc, Victoria D.
Villanuevaa, María Corazon V. Tolentinoa, Glenn
Angelo S. Genuinob, Rafael J. Consunjib, 2013)
Other studies say that the bundle technique to
prevent CAUTI is abbreviated with CAUTI which is
a component of Catheter Removal, Aseptic
Insertion, Regular Use Assessment, and Training for
Catheter Care, Incontinence Care Plan, and
Appropriate Indications for Indwelling Urinary
Catheters (Lona Mody,M Todd Greene, Jennifer
Meddings, Sarah L Krein, Sara E McNamara,
Barbara W Trautner, David Ratz, Nimalie D Stone,
LillianMin, Steven J Schweon, Andrew J Rolle,
RussellN Olmsted, Dale R Burwen, James Battles,
Barbara Edson, 2017)The basic principle of using a
catheter is the use of appropriate indications at the
time of installation and removal of the actuator,
when it is an indication such as the following:
Haematuria; Retention; Urology surgery; Decubitus
ulcer; Measurement of inputs and outputs; End of
life care; and Immobility. Other studies suggest that
hematuria does not require a catheter except patients
in retention. (Dawson, Gallo, & Prevc, 2017)
Research conducted by Al Hameed shows that a
multidisciplinary approach, stepwise intervention
strategies and CAUTI bundles, can significantly
reduce the IUC utilization ratio (Indwelling Urinary
Catheter) and CAUTI level. IAD (Intoctenensia
Associated Dermatitis) which is a potential
complication after catheter insertion can be
minimized by a variety of multidisciplinary
strategies, which involve nursing staff, nutritionists,
and care specialist wounds. (Sushilkumar Satish
Gupta; Pavan Kumar Irukulla; Mangalore Amith
Shenoy; Vimbai Nyemba; Diana Yacoub, 2017)
There is no definite definition of CAUTI Bundle
recommended so far, the researchers collected the
best evidence based that could be applied as a
CAUTI intervention. There are eight components
adopted including; screening all admission patients,
using Foley’s silicone catheters, aseptic techniques,
insertions, emptying catheter bags, selecting the
right catheter size, cleaning the catheter ducts in the
patient's thighs, placing a catheter sac lower than the
patient’s bladder and not touching the floor, and
releasing the catheter as soon as possible after the
patient's condition improves and no further catheter
assistance is needed (Al-Hameed Fahad, Ahmed
Gulam , Al-Saedi Asim & Al-Hameed Faisal, 2018)
While the research conducted by Mariam divided
the two phases of the intervention process to prevent
CAUTI, namely the Assessment phase and the
Protocol phase of care. In the assessment phase the
researcher made an assessment of the nurse
regarding nurse’s knowledge and educated the nurse
to carry out the protocol of care. Then in the
protocol of care phase is divided into several parts,
namely first to prepare the object settings (catheter-
mounted patients), then prepare the protocol of care
content that is knowing the anatomy and
pathophysiology of the urinary system, knowing
indications of catheter installation and infection
control in patients who are catheterized know
contraindications to catheter installation, prepare
catheter installation, perform catheter care, and find
out complications related to catheter placement.
After completion, proceed with the planning of
action protocol of care by paying attention to the
patient's condition. Then at the end of the phase an
evaluation was conducted on nurses related to the
protocol of care that had been done. (Shehab, 2017)
Some important things in CAUTI Bundle that
must be considered by nurses are among others: first
the catheter must remain closed and minimize the
duration of catheter use. Second, pay attention to the
risk of cross infection between patients who are
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
128

catheterized also must receive attention. Third,
nurses must also pay attention to the fact that
patients should receive treatment from nurses when
the installation of the catheter includes hand washing
procedures and the use of sterile gloves in the
catheter installation must also be considered by the
nurse. Furthermore, patients should receive enough
fluids orally to maintain urine flow of 50-100 ml /
hour. Then, systemic prophylactic antibiotics are not
recommended for catheter placement or intermittent
catheterization. There is no benefit from antibiotic
irrigation through a catheter and bladder. When
changing catheters regularly depending on the
catheter material used. Take into account
alternatives for sedentary catheterization which often
causes symptomatic infections. In certain cases,
suprapubic catheters, catheter condoms and
intermittent catheterization are more recommended
than permanent catheters. (Tarmono et al., 2015)
Meanwhile other studies make programs to
prevent infection due to catheter placement. The
program was divided into 3 phases, namely phase 1
including ICU Nurse installing a catheter,
determining the discussion to remove the catheter,
and auditing catheter insertion consisting of
determining the type of catheter, Hand hygiene
before catheter placement, perineal hygiene using
antimicrobial soap, hand washing, prior connection
between catheters and catheter sacs, using aqueous
chlorhexidine antisepsis, introducing opportunities
for catheter placement as a unique opportunity and
hand washing after catheter placement. Then phase 2
consists of the audit process, and the implementation
of catheter installation is then followed by the third
phase, namely the appointment of nurses who are in
charge of preventing CAUTI, then looking at the
feedback to what has been done. (Josephine Anne
Navoa-Nga, Regina Berbab, Victor D. Rosenthalc,
Victoria D. Villanuevaa, María Corazon V.
Tolentinoa, Glenn Angelo S. Genuinob, Rafael J.
Consunjib, 2013) While other studies state that
interventions to reduce CAUTI by installing
catheters
Then Systematic Review conducted by Dinah
Gould et al entitled Implementing clinical guidelines
to prevent catheter-associated urinary tract infections
and improve catheter care in nursing homes using
the Systematic search method and critical appraisal.
The total studies reviewed and analyzed were 8
studies which included the study conducted by
Gokula and Gaspar which used guidelines for
prevention of CAUTI and carried out in a population
of 14 patients with long-term catheter use and used a
comparison for control groups using the SOP in
hospital and carried out for 3 months with the results
of the study saying there was no difference between
the application of the CAUTI guidelines and the
standard SOP carried out. Whereas 2 studies were
conducted by Galeon and Romero and the research
of Abraham and Debakey using the Uncontrolled
Before and After Study research methods. The study
was carried out by implementing a complete
guideline for CAUTI Prevention, stating that there
were significant differences after the CAUTI
prevention guidelines were implemented. While 5
other studies evaluated one part of the CAUTI
Prevention guidelines showing significant results.
What should be a concern in the application of the
CAUTI prevention guideline is the challenge that
comes from nurses to be able to properly implement
the guideline that has been made by the consensus
for the prevention of CAUTI (Gould, Gaze, Ba,
Cooper, & Cadwaladr, 2017)
Meanwhile another study conducted by Parker et
al. (2017) conducted a study using the intervention
study pre-post control method. The study was
conducted at 2 Health Districts with the population
being adult patients in several acute spaces in 4
hospitals (acute setting) and in NSW, Australia. The
study began by educating nurses on NOCAUTI
Interventions bundles consisting of guidelines for
IDC insertion, indications for collection of urine
specimens, guidelines for IDC removal and
education for nurses to implement CAUTI
prevention interventions. Saint Have made the
concept of NOCAUTI bundles through pilot
projects in Australia. The concept of NOCAUTI
consists of Need for catheter assessed (Assessment
is done for patients with appropriate indications for
catheter placement), Obtain patient consent and
Offer Patient Education (Giving informed consent
and education to patient / patient families),
Competency (Ensuring only nurses have competence
and experienced who put on a catheter), Asepsis
(Using asepsis technique), Unobstructed (Keeping
urine flow in the hose not having obstruction),
Timely Cateteher removal (Determining the time of
catheter up based on indications and medical needs
needed), and Infection (Performing care catheter and
taking urine specimen with asepsis technique). The
results of the research carried out can improve
patient safety through strong implementation and
evaluation of clinical practice and changes in
practice that will contribute to improving patient
experience and the results obtained by the hospital.
Research conducted adds evidence based practice
through increasing understanding of interventions to
reduce CAUTI. (Lona Mody,M Todd Greene,
The Effect of Catheter Associated Urinary Tract Infection (CAUTI) Bundle of Care: A Systematic Review
129

Jennifer Meddings, Sarah L Krein, Sara E
McNamara, Barbara W Trautner, David Ratz,
Nimalie D Stone, LillianMin, Steven J Schweon,
Andrew J Rolle, RussellN Olmsted, Dale R Burwen,
James Battles, Barbara Edson, 2017)
Interventions are targeted at nurses who have the
task of installing a urine catheter in the hospital and
are designed to reduce the use of inappropriate urine
catheters and improve the necessary catheter care.
The interventions consisted of education with lecture
methods from videos, installing reminders in the
room, and weekly infection prevention lectures by
the head of the room. (L. Gayani Tillekeratne,
Darren R. Linkin, Mariah Obino, Wanjiku,
Holtzman, & Cohn, 2014) Nurses must understand
indications of catheter placement namely acute
urinary obstruction or retention, the need for
measurement accurate from input and output in
critically ill patients, the presence of open sacrum or
perineal ulcers in patients with urinary incontinence,
prolonged immobilization, the need for continuous
urinary discharge during perioperative care and
increased comfort in patients who are near death (L.
Gayani Tillekeratne, Darren R. Linkin, Mariah
Obino et al., 2014)
Another intervention the researchers obtained
was that the interventions used in nursing home
implementation projects, which depend on technical
and social adaptive interventions, reduce the level of
ISTI associated with catheter installation in settings
where utilization is low but catheter use lasts longer.
Although this project focuses on reducing catheter-
related UTIs, an approach similar to evidence based
can be used to address the security issues of other
residents in community-based nursing homes. (Lona
Mody,M Todd Greene, Jennifer Meddings, Sarah L
Krein, Sara E McNamara, Barbara W Trautner,
David Ratz, Nimalie D Stone, LillianMin, Steven J
Schweon, Andrew J Rolle, RussellN Olmsted, Dale
R Burwen, James Battles, Barbara Edson, 2017)
Another study conducted on resident students
produced two important points, the first was the
simulation of providing optimal facilities for
evaluating clinical decision making and the second
the participants had experience and training in a
catheterization scenario that would be their
responsibility in the future. This information allows
opportunities for change in surgical education that
will emphasize important clinical topics, ongoing
assessment, and the method of feedback. Thus will
improve the performance of trainees and ensure
competency for independent practice (Nathwani,
Law, Witt, Ray, & Dimarco, 2017)
5 CONCLUSSION
Interventions that have been designed to reduce
initially high levels of CAUTI indicate that there is a
decrease in unnecessary use of urinary catheters and
a decrease in CAUTI levels. And the costs for
interventions are more affordable. (Tillekeratne et
al., 2014) CAUTI incidence has decreased
significantly after the implementation of strategies
and interventions to prevent CAUTI levels being
carried out in adult ICU patients. (Al-hameed et al.,
2018) Interventions apply a variety of approaches
including the following are: bundles of infection
control interventions, education, supervision of
CAUTI levels, feedback on CAUTI, supervision of
the nurse's performance feedback process (Josephine
Anne Navoa-Nga, Regina Berbab, Victor D.
Rosenthalc, Victoria D. Villanuevaa, María Corazon
V. Tolentinoa, Glenn Angelo S. Genuinob, Rafael J.
Consunjib, 2013)
CAUTI incidence declined significantly after the
adoption of strategies and interventions to prevent
CAUTI levels being carried out in adult ICUs by
implementing eight components adopted in patient
care (Al-Hameed Fahad, Ahmed Gulam , Al-Saedi
Asim & Al-Hameed Faisal, 2018)
The results of the research discussed above show
that the CAUTI of care bundle can prevent and
reduce CAUTI so that it can help nurses to improve
effective and efficient health services for patients.
This Systematic review recommends that the
CAUTI bundle can significantly reduce CAUTI
incidence and become the basis for the study of the
effect of the CAUTI bundle in Indonesia.
ACKNOWLEDGEMENTS
We would like to acknowledge Diponegoro
University in supporting this work.
REFERENCES
Al-Hameed Fahad, Ahmed Gulam , Al-Saedi Asim, B. M.,
& Al-Hameed Faisal, S. M. (2018). Brief
Communication, 39(1), 97–103.
https://doi.org/10.15537/smj.2018.1.20999
Dawson CH, Gallo M, Prevc K. TWOC around the clock :
a multimodal approach to improving catheter care.
2017;
Fletcher, K. E., & Tyszka, Jeanne T. Harrod, Molly.
Fowler, Karen E. Fowle. Saint, Sanjay. Krein, S. L. K.
(2016). Qualitative validation of the CAUTI Guide to
ICINNA 2018 - The 1st International Conference of Indonesian National Nurses Association
130

Patient Safety assessment tool. American Journal of
Infection Control, 44(10), 1102–1109.
https://doi.org/10.1016/j.ajic.2016.03.051
Ghinorawa T. Penatalaksanaan Infeksi Saluran Kemih dan
Genitalia Pria 2015.
Gould, D., Gaze, S., Ba, N. D., Cooper, T., & Cadwaladr,
B. (2017). American Journal of Infection Control
Implementing clinical guidelines to prevent catheter-
associated urinary tract infections and improve
catheter care in nursing homes : Systematic review.
AJIC: American Journal of Infection Control, 45(5),
471–476. https://doi.org/10.1016/j.ajic.2016.09.015
Ikatan Urologi Indonesia. Diagnosis dan Penatalaksanaan.
2014;41(10):737–40.
Josephine Anne Navoa-Nga, Regina Berbab, Victor D.
Rosenthalc,∗, Victoria D. Villanuevaa, María Corazon
V. Tolentinoa, Glenn Angelo S. Genuinob, Rafael J.
Consunjib, J. B. V. M. I. b. (2013). Impact of an
International Nosocomial Infection Control
Consortium multidimensional approach on catheter-
associated urinary tract infections in adult intensive
care units in the Philippines : International Nosocomial
Infection Control Consortium ( INICC ). Journal of
Infection and Public Health, 6(5), 389–399.
https://doi.org/10.1016/j.jiph.2013.03.002
L. Gayani Tillekeratne, Darren R. Linkin, Mariah Obino,
A. O., Wanjiku, M., Holtzman, D., & Cohn, J. (2014).
A multifaceted intervention to reduce rates of catheter-
associated urinary tract infections in a resource-limited
setting. American Journal of Infection Control, 42(1),
12–16. https://doi.org/10.1016/j.ajic.2013.07.007
Lee EK. Incidence of CAUTI in a new integrated ICU /
HD in Singapore over 1 year. 2017;20(3):53–60.
Lona Mody,M Todd Greene, Jennifer Meddings, Sarah L
Krein, Sara E McNamara, Barbara W Trautner, David
Ratz, Nimalie D Stone, LillianMin, Steven J Schweon,
Andrew J Rolle, RussellN Olmsted, Dale R Burwen,
James Battles, Barbara Edson, S. Saint. (2017).
Avoiding inappropriate urinary catheter use and
catheter-associated urinary tract infection ( CAUTI ): a
pre-post control intervention study, 1–10.
https://doi.org/10.1186/s12913-017-2268-2
Mody, L., Greene, M. T., Meddings, J., Krein, S. L.,
Mcnamara, S. E., Ascp, M. T., … Saint, S. (2017). A
National Implementation Project to Prevent Catheter-
Associated Urinary Tract Infection in Nursing Home
Residents, 48109(8), 1154–1162. https://doi.org/
10.1001/jamainternmed.2017.1689
Maria A, Rn C, Zinsly T, Camargo S, Marra AR, Victor S,
et al. catheter-associated urinary tract infection.
2015;14–8. Available from: http://dx.doi.org/10.1016/
j.ajic.2015.11.07
Nathwani JN, Law KE, Witt AK, Ray RD,Dimarco SM.
SC. Am J Surg [Internet]. 2017; Available
from:http://dx.doi.org/10.1016/j.amjsurg.2017.01.007
Navoa-ng JA, Berba R, Rosenthal VD, Villanueva VD,
Corazon M, Tolentino V, et al. Impact of an
International Nosocomial Infection Control
Consortium multidimensional approach on catheter-
associated urinary tract infections in adult intensive
care units in the Philippines : International Nosocomial
Infection Control Consortium ( INICC ) findings. J
Infect Public Health [Internet]. 2013;6(5):389–99.
Available from:
http://dx.doi.org/10.1016/j.jiph.2013.03.002
Prevention I, Island L, Forest J, Health N, Hills F. an
academic medical intensive care unit. AJIC Am J
Infect Control [Internet]. 2017; Available from:
http://dx.doi.org/10.1016/j.ajic.2017.06.020
Parker V, Giles M, Graham L, Suthers B, Watts W, Brien
TO, et al. Avoiding inappropriate urinary catheter use
and catheter-associated urinary tract infection (
CAUTI ): a pre-post
control intervention study. 2017;1–10.
Regagnin, D. A., , Debora Schettini da Silva Alves, Ana
Maria Cavalheiro, Thiago Zinsly Sampaio Camargo,
Alexandre R. Marra, E. da, Victor, S., & Edmond, M.
B. (2015). catheter-associated urinary tract infection,
14–18. https://doi.org/10.1016/j.ajic.2015.11.037
Saint, S., Olmsted, R. N., Fakih, M. G., Kowalski, C. P.,
Watson, S. R., Sales, A. E., & Krein, S. L. (2009).
Translating health care-associated urinary tract
infection prevention research into practice via the
bladder bundle. Joint Commission Journal on Quality
and Patient Safety, 35(9), 449–455. https://doi.org/
10.1016/S1553-7250(09)35062-X
Shehab, M. S. (2017). Impact of Protocol of Care of
Patients Undergoing Urinary Catheterization,
10(August), 1013–1021.
Sushilkumar Satish Gupta; Pavan Kumar Irukulla;
Mangalore Amith Shenoy; Vimbai Nyemba; Diana
Yacoub. (2017). Successful strategy to decrease
indwelling catheter utilization rates in an academic
medical intensive care unit. AJIC: American Journal
of Infection Control. https://doi.org/10.1016/j.ajic.
2017.06.020
Tarmono, K. P. S., Renaldo, B. S. N. C. A. M. I. W. J., &
Ghinorawa, A. R. A. H. H. I. W. Y. T. (2015).
Guidelines Penatalaksanaan Infeksi Saluran Kemih
dan Genitalia Pria 2015. Jakarta: Ikatan Ahli Urologi
Indonesia (IAUI).
Tillekeratne LG, Linkin DR, Obino M, Omar A, Wanjiku
M, Holtzman D, et al. American Journal of Infection
Control A multifaceted intervention to reduce rates of
catheter-associated urinary tract infections in a
resource-limited setting. Am J Infect Control
[Internet]. 2014;42(1):12–6. Available from:
http://dx.doi.org/10.1016/j.ajic.2013.07.007
The Effect of Catheter Associated Urinary Tract Infection (CAUTI) Bundle of Care: A Systematic Review
131
