
Leprosy, Syphilis, and Human Immunodeficiency Virus Coinfection:
A Case Report
Mochammad Rifky Luthfiandi, Satiti Retno Pudjiati, Hardyanto Soebono
Departement of Dermatology and Venerology, Faculty of Medicine Universitas Gadjah Mada, Dr.Sardjito General
Hospital, Yogyakarta, Indonesia
Keywords: leprosy, syphilis, HIV, sexually transmitted disease
Abstract: Coinfection between leprosy, syphilis and HIV is very rare, and this association remains unclear. We report
55 years old man from Bantul, Indonesia, who present almost all over the body covered with erytematous
patches and plaques in various sizes, multiple, discrete with ulnaris nerve enlargement. This patient was
diagnosed as BL leprosy, secondary syphilis and HIV infection. Laboratory investigation showed Bacterial
Index 3+ and Morphological Index 43.75%, positive TPHA, VDRL 1/32, and HIV reactive with CD4 count
4. Histologic finding demonstrated as acute viral exanthem. We treated this patient with WHO-multidrug
therapy regimen for MB leprosy, benzathin penicillin 2.4 million unit IM single dose, and triple FDC
(tenofovir, hiviral, and efavirenz) once a day. A month after therapy, VDRL was surprisingly increasing to
1/256 in titer. Hence, we re-treated him with benzatin penicillin 2,4 million unit once a week for 3
consecutive weeks. We conclude that coinfection between these three diseases make the clinical
manifestation and histological become atypical, and it amay influence each other. Treatment of these
diseases combination was the same as the disease separately.
1 INTRODUCTION
Leprosy is a chronic infection of the skin and
peripheral nerves by Mycobacterium leprae (M.
leprae). The clinical spectrum of leprosy depends on
specific host immunity. Patients with tuberculoid
leprosy have good cell-mediated immune responses
to M. leprae, whereas those with lepromatous
disease do not have cell-mediated immune responses
but rather produce high titres of M leprae-specific
antibodies (Britton,2004) (Ustianowski,2006).
Syphilis and human immunodeficiency virus
(HIV) are both transmitted sexually and so it is not
surprising that a substantial number of people are
infected with both agents. HIV has several effects on
the presentation, diagnosis, disease progression, and
therapy of syphilis (Lynn,2004)(Stevenson,2006).
The interaction between syphilis and HIV infection
is complex and remains incompletely understood,
despite there being more than 2 decades of clinical
experience with coinfected patients
(Stevenson,2006).
Prevalence rates of HIV infected persons are also
increasing in many countries where leprosy is
endemic. Although the number of coinfected
patients has not been estimated, the increasing
geographic overlap of these two diseases will result
in increasing number of individuals being dually
infected (Ustianowski,2006). Meanwhile, there are
few number of case reports of leprosy that
association with HIV (T.S. Chandra Gupta, 2007).
Furthermore, the long incubation period and low
incidence of leprosy make it hardly to do studies
about coinfection leprosy and HIV
(Ustianowski,2006).
Clinical manifestasion of leprosy present with
skin lesion from hypopigmented to nodular lesion
and nerve damage (Ustianowski,2006). Likewise
syphilis, the skin lesion can form ulceration,
maculopapullar, to nodular (lynn,2004). Patients
with HIV often have several simultaneous or
sequential cutaneous conditions. In general,
noninfectious cutaneous abnormalities are not
prognostic of rapid progression of
immunosuppression, but it might be specific markers
of the stage of HIV disease (Maurer,1998). All of
them can resembling other diseases and lead
misstaken and delayed diagnosed for the clinician.
Luthfiandi, M., Pudjiati, S. and Soebono, H.
Leprosy, Syphilis, and Human Immunodeficiency Virus Coinfection: A Case Report.
DOI: 10.5220/0008159904690472
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 469-472
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
469
Coinfection between leprosy, syphilis and HIV
are very rare, and their correlation remain unclear.
This report is to present a man of 55 years of age
diagnosed of leprosy with laten syphilis and HIV.
Hopefully, this paper may remind clinicians the
possible co-incidence between these infectious
diseases.
2 CASE
A 55 years old man, lived in Bantul, visited
outpatient clinic of dermatology and venerology, Dr.
Sardjito General Hospital with reddish spot in
almost all over the body. The history of present
illnes had started from 2 months before admitted the
clinic with reddish spots on the face and scalp,
which gradually extended to the whole body. No itch
nor pain were reported. He had seen dermatologist,
and treated as allergy, but no improvement. He was
then refered to our hospital. He frequently applied
hair dyes, and various cosmetics. Beside his wife, he
had multisexual-partners of three other men. , with
last sexual activity was 6 month ago with wife.
According to patient confession, he was forced for
sexual intercourse with three man 5 years ago, then
after that he never had sex except with his wife. He
also reported that he travelled alot due to his
profession. No history of diabetes mellitus,
hypertension, nor were reported
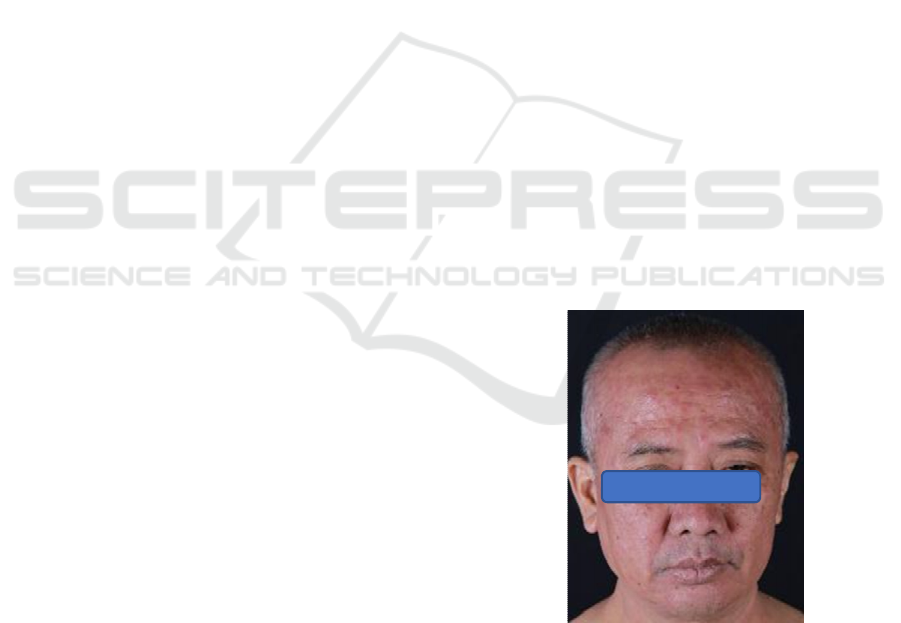
Dermatological status demonstrated erytematous
patches and plaques in various sizes, multiple,
discret distributed all over the body (Fig. 1-3). There
was enlargement of both ulnar nerves but no
sensitibility impairment in lesions, and nor motoric
and sensoric nerve impairment. The differential
diagnosis were made Morbus Hansen-Multi
Bacillary (MH-MB) BL/ LL type, Secondary
Syphilis, HIV/AIDS, and Allergic Contact
Dermatitis (ACD).
Laboratory examinations showed bacterial index
(BI) 3+ and morphological index (MI) 43.75%,
treponema palidum haemaglutination (TPHA)
positif, venereal disease research laboratory (VDRL)
1/32, HIV rapid test positive, and enzym linked
fluouroscent assay (ELFA) test for HIV was 23.31
(normal range <0.25) with CD4 only 4. Biopsy from
right upper arm lesion demonstrated histologially as
acute viral exanthem (Fig.4).
Working diagnosis in this case were MH MB
type BL/LL, latent syphilis, and HIV. We treated
him with MDT-MB regimen, intramuscular
injection of benzatin penicillin 2.4 million units in
single dose, and triple Fixed Drugs Combination
(FDC) (tenofovir 300mg, hiviral 300mg, and
efavirenz 600mg) once a day.
After a month, the skin manifestations were
improved leaving only hyperpigmentation in almost
all over the body. However, VDRL titer was even
higher which was 1/256. And the AFB smear were
+3 for BI and 20% MI. So, unresponsive diagnosis
of syphilis was made. Benzatin penicillin 2.4 million
units injection once a week in consecutive 3 weeks
was performed.. A month followed up showed that
VDRL titer was decreasing to 1/32.
3 DISCUSSION
Diagnosis for leprosy is made when one or more
cardinal sign are present, i.e hypopigmented or
reddish skin lesions with definite loss of sensation,
involvement (thickened) of the peripheral nerve, and
skin smear positif for acid fast bacilli (Britton,2004)
(ILA Technical Forum,2002). According to the
immunity, Ridley and Jopling clasifies the leprosy as
follows; indeterminate (I), tuberculoid tuberculoid
(TT), borderline tuberculoid (BT), borderline
borderline (BB), borderline lepromatous (BL), and
lepromatous leprosy (LL).
8
Which is tuberculoid
pole can be associated with rapid and severe nerve
damage, whereas lepromatous pole is associated
with chronicity and long-term complications.
Borderline disease is unstable and can be
complicated by reactions (Britton, 2004).
Figure 1. patches-plaques on the face
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
470

Figure 2. patches on the palm
Figure 3. patches-plaques on the trunk
Figure 4. A. HE staining 40x. B. HE staining 100x. C. HE
staining 400x. D. FF staining.
In this case, two cardinal sign was appear, i.e
thickened of the ulnaris nerve, and skin smear for
acid fast bacilli was positf 3 for BI and 43.75% for
MI. And there was no sensoric or motoric nerve
impairment. Even though histopathology
examination result was not suitable for leprosy. This
might be because the biopsy sample in the upper
right arm is a lesion from other diseases in this
patient. From this finding, we diagnosed the patient
as leprosy.
Syphilis is diagnosed using serological test, with
treponemal and non treponemal test. In majority, this
serological test can be accurately to diagnose
syphilis. However, direct testing methods, such as
dark-field microscopic examination, direct
fluorescent antibody-treponema pallidum (DFA-TP),
and polymerase chain reaction (PCR), should be
considered when the diagnosis of syphilis cannot be
confirmed (Stevenson,2006). In this case,
serological test with TPHA was positive, and VDRL
was positif with 1/32 in titer. With the manifestasion
rash almost all over the body and also found in
palms and soles, at the beginning we diagnosed with
secondary syphilis. But as the histopathology result
did not demonstrate skin lesion of syphilis, hence,
latent syphilis was considered. This was also
supported by the fact he might get the syphilis was
around 5 years ago, and that a month after treatment
with benzathin penicilin, the titer of VDRL was
increasing to 1/256 in titer.
Human immunodefiency virus were diagnosed
using rapid test with immunochromatographic (ICT)
and ELFA, which is the result was positif. With the
sensitivity 100% and specificity 98% for ELFA, we
can confirm the diagnosis for HIV (Ortiz,1996). In
this case, rapid test using ICT was done,with the
result was positive. Then we confirmed the result
with ELFA, and the result was positif. So, we
diagnosed this patient as HIV infection.
The therapy for leprosy with syphilis and HIV
coinfection is still the same with leprosy without
coinfection. HIV infection might affect the efficacy
of multidrug therapy for leprosy, with HIV-positive
patients potentially taking longer to clear
mycobacteria from lesions or experiencing a higher
relapse rate, but some published data suggest that
leprosy-HIV coinfected patients respond equally
well to multidrug therapy without the need for
prolonged treatment.
1
relapses are rare after
multidrug therapy, being about 1 per 1000 person-
years for tuberculoid patients and 0–20.4 per 1000
person-years for multibacillary patients
(Britton,2004)(Ustianowski,2006).
Penicillin remains the main therapy for all stages
and sites of syphilis and in all patient groups
(Lynn,2004)(US Centers for Disease Control and
Prevention,2002). the difference from syphilis
patients with and without HIV are in early phase of
the disease (< 2 years), where are patients without
HIV are treated with intramuscular benzatin
penicillin 2,4 million units in single dose. In
coinfetion with HIV, early disease can be treated
A
B
C
D
Leprosy, Syphilis, and Human Immunodeficiency Virus Coinfection: A Case Report
471

same as with non-HIV patient, but some clinician
recommend 3 dose at weekly interval (US Centers
for Disease Control and Prevention,2002).
4 CONCLUSION
We reported a case of 55 years old man with BL/ LL
leprosy, with latent syphilis, and HIV infection. The
skin manifestation and histopathological were
atypical, but these were supported by the laboratory
examinations which were acid fast bacilli,
serological test for syphilis and HIV serology. From
this case, we demonstrate that coinfection between
these three diseases is apparently possible, make the
clinical and histological features may be atypical, as
interactions each other between them. . In general,
the therapy is the same as the disease was separately.
REFERENCES
Britton, W.J, Lockwood, D.N.J., 2004. Leprosy. Lancet,
363(9416), 1209–1219.
ILA Technical Forum., 2002. Diagnosis and classification
of leprosy. Leprae Rev, 72, pp. 17–26.
Lynn, W. A., & Lightman, S., 2004. Syphilis and HIV: a
dangerous combination. The Lancet infectious
diseases, 4(7), pp. 456-466.
Maurer, T.A., & Berger, T.G., 1998. Dermatologic
Manifestations of HIV. HIV insite, University of
California San Francisco.
De Lejarazu Ortiz, R., Eiros-Bouza, J. M., Martínez, P.,
Reguera, J. I., & Rodríguez-Torres, A., 1996.
Comparison of 2 ELFA methods for the automatized
diagnosis of HIV infection. Enfermedades infecciosas
y microbiologia clinica, 14(3), pp. 150-154.
RIDÉEY, D., & Jopling, W. H., 1966. Classification of
leprosy according to immunity. A five-group
system. International journal of leprosy, 34(3), pp.
255-273.
Stevenson, J., & Heath, M., 2006. Syphilis and HIV
infection: an update. Dermatologic clinics, 24(4), pp.
497-507.
Gupta, T. C., Sinha, P. K., Murthy, V. S., & Kumari, G.
S., 2007. Leprosy in an HIV-infected person. Indian
Journal of Sexually Transmitted Diseases and
AIDS, 28(2), 100-102.
US Centers for Disease Control and Prevention., 2002.
Sexually transmitted diseases treatment guidelines.
MMWR Recomm Rep. 51, pp. 1–78.
Ustianowski, A. P., Lawn, S. D., & Lockwood, D. N.,
2006. Interactions between HIV infection and leprosy:
a paradox. The Lancet infectious diseases, 6(6), pp.
350-360.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
472
