
Heat Therapy as an Excellent Adjuvant Treatment for Severe
Chromoblastomycosis: A Case Report
Lusiana, Rizky L. Prayogo, Rahadi Rihatmadja, Sandra Widaty, Sri Linuwih Menaldi, Eliza
Miranda.
Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia / Dr. Cipto Mangunkusumo
General Hospital, Jakarta Indonesia.
Keywords: chromoblastomycosis, heat therapy, itraconazole.
Abstract: Chromoblastomycosis is a subcutaneous infection commonly found in tropical and subtropical areas, caused
by dark-pigmented fungi (Dematiaceae). The disease is most frequently observed in extremities with
previous history of trauma and is associated with agricultural occupation. It is characterized by a clinical
presentation of verrucous nodule or plaque, muriform bodies on direct smear and histopathological
examination and slow growing, black-brown colony on the culture. It has been reported that several
treatment options for chromoblastomycosis are studied with varied cure rate, both physical therapy and
systemic antifungal drugs. Heat therapy was a method that applies heat to the lesion thereby inhibit the
growth of fungi. Here we report a severe chromoblastomycosis case which had combination treatment of
heat therapy and itraconazole and showed favourable outcome.
1 INTRODUCTION
Chromoblastomycosis (CBM) commonly occur in
tropical and subtropical regions, and it is caused by
Dematiaceae such as Fonsecaea pedrosoi,
Phialophora verrucosa and Cladophialophora
carrionii as the most common pathogen species.
(Hay, 2012,Queiroz, 2017) Dematiaceae refers to
fungi containing melanin in their cell walls
microscopically visible by a gross brown,
olivaceous, or black pigmentation. (Queiroz, 2017)
Fungi inoculation exist because of direct
transcutaneous implantation in the lower extremity
as the predilected area, followed by upper extremity
and upper part of the trunk with the history of
trauma and associated with particular occupation in
the farm land or in the agricultural field. (Queiroz,
2015)
The initial lesion may begin with erythematous
macular or squamous papule, and then it may
gradually extended within months or years and
eventually become polymorphic, hyperkeratotic
papules-nodules, cauliflower-like or verrucous
plaques with atrophic scar in the middle part. (Hay,
2012,Queiroz, 2017,Agarwal, 2017,Purim, 2017)
Diagnosis is established based on medical history,
physical examination and identified Dematiceae.
The presence of muriform or sclerotic bodies by
direct examination with potassium hydroxide (KOH)
and histopathological examination and also on the
culture we can find slow-growing, black-brown
colonies with soft hairy surface.
It has been reported that there are several
therapeutic options for CBM, such as physical
therapeutic methods (heat therapy, excisional
surgery, electrosurgery, CO2 laser, heat therapy, and
photodynamic therapy) and systemic antifungal
agent. (Queiroz, 2017,Hiruma, 1993-Hira, 2002)
According to several open and noncomparative
clinical trials, itraconazole is the standard therapy
for CBM, and it is also the most common antifungal
drug used that can be combined with other
modalities. The recovery rate varies, however in the
chronic case and severe lesion it is common to get
insufficient outcome with high rate of disease
reccurence. Heat therapy is a potential therapeutic
option for CBM that is easy to use with good
response. Several complications that is commonly
encountered in CBM are secondary bacterial
infection that may cause lymphatic fibrosis and
extremity elephantiasis. Chronic diseases may also
developed to become squamous cell carcinoma.
(Hira, 2002)
406
Lusiana, ., Prayogo, R., Rihatmadja, R., Widaty, S., Menaldi, S. and Miranda, E.
Heat Therapy as an Excellent Adjuvant Treatment for Severe Chromoblastomycosis: A Case Report.
DOI: 10.5220/0008158504060410
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 406-410
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
2 CASE
A 50-year-old male visited the Dermatology and
Venerology Outpatient Clinic at the Dr. Cipto
Mangunkusumo General Hospital on 7 September
2017 with chief complaint of cauliflower-like
masses with black spots that has spread to the right
lower extremity since 10 years ago. Initially, the
middle finger of the right feet was hurt by knife, and
then red spot appear in the dorsal pedis, above the
wound surface and extended gradually, become
hyperkeratotic papules-nodules, cauliflower-like or
verrucous plaques with atrophic scars in the middle
part. The lump was itch and painful especially after
activities, sometimes bleeding if it is scratched or
traumatized. The patient had several medical
consultations at the Community Health Centre
where he received antihistamine, pain killer, and
topical therapy. However, the symptoms did not
improved. The patient frequently worked at the farm
land, taking care of crops without any foot cover.
Previous history of malignancy, lung disease or
chronic cough in the patients and family were
denied.
On physical examination, the general condition
and vital signs were within normal limit. On the
right lower extremity and ventral side of the right
foot, there were multiple erythematous and skin-
colored papules, nodules, vegetative plaques with
black spots. There were hypertrophic scars between
these lesions (Fig.2a). There was no enlargement in
the lymph node. The direct examination with KOH
showed some muriform cells or sclerotic bodies.
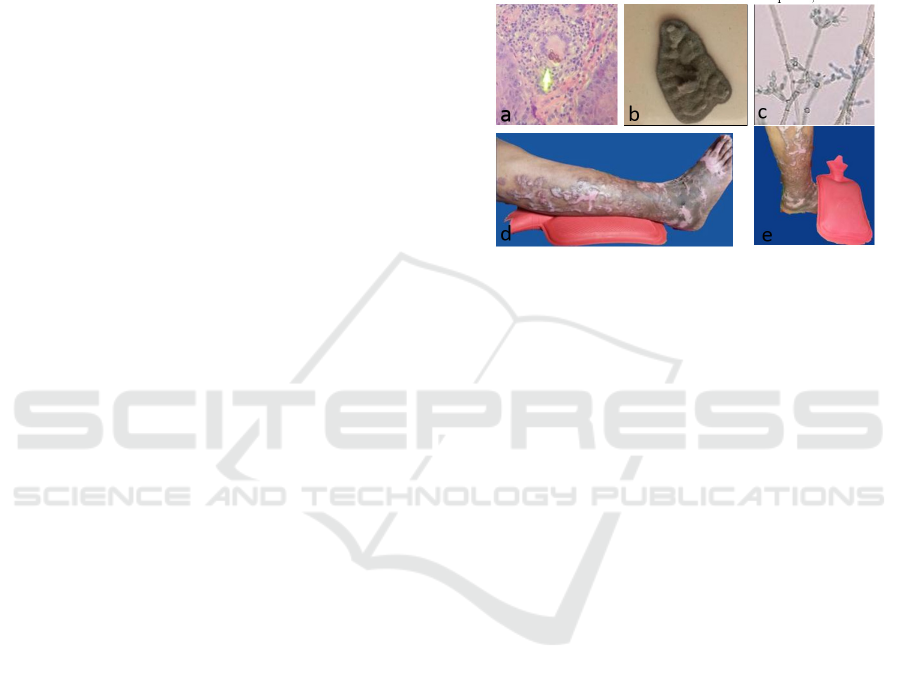
Histopathological examination revealed
hyperplasia pseudoepitheliomatosa appearance, and
in the dermis there were lymphocyte cells
infiltration, histiocytes, plasma cells and
multinucleated and Langhans giant cells. There were
muriform cells with thick wall and brown-coloured
in the cytoplasm of giant cell (Fig.1a). Tissue culture
on Sabouraud's dextrose agar (SDA) medium grown
slow-growing, dark-brown colonies, with slightly
elevated center (Fig.1b). Microscopic examination
with lactophenol cotton blue (LPCB) staining
revealed brown conidiophores, ovoid conidia that
located at the end or at the side of conidiophores
concluded as Foncecaeae pedrosoi (Fig.1c).
All of these examination results supported the
diagnosis of CBM. Patient was given itraconazole
200 mg daily combined with heat therapy. As the
heat therapy, patient used hot water rubber pocket
with temperature around 50–60
0
C for 30-60 seconds,
3 times daily (Fig.1c). Clinical improvement has
been observed within 1 month of therapy. Visually,
the swelling became smaller, black granules were
disappeared, the pain and itch symptoms were
vanished. During 4 months of follow up, most of the
swelling was thinner (Fig.2b). Nodular type lesion
was faster to become small compared to plaque-
shaped lesions and hypertrophic scars. The liver and
kidney functions was routinely examined every
month.
Figure 1. a. Muriform cells, b. Colony of F. pedrosoi
(macroscopic), c. Slide culture of F. pedrosoi
(microscopic, LPCB), d-e. Heat therapy procedure.
3 DISCUSSION
Chromoblastomycosis is more common in
male, with male-to-female ratio of 4:1, and
predominantly between 30-50 years of age
because risk of trauma was higher in these
groups of population. (Santos,2007) Disease
transmission was due to inoculation of non-
intact skin with fungi Dematiceae from soil or
contaminated crops. The patient was a 50-year-
old male, works at farm and seldomly use foot
protector. Patient had a history of cutting
wound on his foot 10 years ago. Several months
later there were red spots on the surface above
the cut wound. From the medical history, the
patient demographic status was consistent with
epidemiology characteristic of CBM, such as
gender, age, and occupation type. (Santos,
2007) History of trauma surrounding the lesion,
history of occupation, and infrequent use of
foot protector, were the risk factors that may
create a port d’entrée for the fungi and
eventually resulted in subcutaneous mycosis
infection. (Santos, 2007)
Heat Therapy as an Excellent Adjuvant Treatment for Severe Chromoblastomycosis: A Case Report
407

Figure 2. a. Before treatment, cauliflower-like lesions, b. After 4 month combination therapy, the lesions smaller, thinner,
black spots dissapear.
Diagnostic techniques of CBM are based on
physical and direct examination, culture and
histopathology.Queiroz,2009 From direct scrap of
KOH and skin biopsy in the lesion surface
containing black spots, we could find the disease
hallmark of CBM or pathognomonic fungi structure:
muriform cell or sclerotic bodies or fumagoid cells
or copper pennies.(Queiroz, 2017;Queiroz, 2015;
Queiroz,2009) Muriform cells had thick wall like
chestnut, round-shaped, brown color with cross
chamber, tranversal and longitudinal, and this is as
result of fungi adaptation in order to survive in the
host tissue. (Queiroz, 2017; Queiroz, 2015) The
sensitivity of direct examination with KOH for CBM
was 90-100%. (Queiroz, 2017) Therapy may be
started upon the demonstration of muriform cells,
however, culture identification is important because
Fonsecaea species may be less sensitive to
antifungals. (Queiroz, 2017) From all the signs,
symptoms and examinations results in this patient
we concluded the diagnosis was CBM and
categorized as severe degree based on the lesion size
of more than 15 cm2.13
Therapy of CBM consists of several modalities,
such as systemic antifungal medication, physical
therapy, surgical or combination of these modalities.
(Queiroz, 2017; Hiruma,1993) Options and outcome
of treatment were dependent by the etiological
pathogen, size of lesion, and the degree of the
disease, complication, like dermis fibrosis and
edema that can reduce the drug concentration in the
tissue. The most effective systemic antifungal drugs
is itraconazole (200-400 mg/day) or terbinafine
(500-1000 mg/day) minimally 6-2 months therapy.
In the refractory cases, both drugs could be given
simultaneously. F. pedrosoi was said to be
insensitive to systemic antifungal drugs compared to
C. carrionii and P. verrucosa and there was a report
of resistance to itraconazole. (Hira, 2002, Andrade,
2004) In this case, itraconazole was still sensitive
with rapid clinical improvement. Heat therapy was a
method that applies heat so that the lesion
temperature reach 42-45oC. (Queiroz, 2015)The
mechanism of action relies on fungal intolerance to
high temperature. (Queiroz, 2017) Yanase et al.
reported that maximal temperature of F. pedrosoi for
growth was 390C.(Yanase, 1978) Heat therapy has
particularly been applied in Japan, with several
methods. Application of a chemical pocket warmer
occluded with a bandage over the lesions on 24 h per
2a
2b
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
408

day, or local heat therapy for 2 h perday combined
with the administration of posaconazole, or
combination of heat therapy for 12 h perday and
terbinafin, resulted in an improvement of lesions and
negative microscopic examination and culture
results within 2-8 months. (Queiroz, 2017; Yanase,
1978)
In this case the combination of itraconazole 200
mg/day with heat therapy, using rubber pocket water
warmer, about 50-600C for only 30-60 minutes,
showed good response within one month, as it was
faster than previous reports. During evaluation after
four months of treatment, the response was
excellent, the swelling became smaller and thinner,
and the surface became smoother. The itch and pain
were vanished. Itraconazole is planned to be given
for 12 months with monthly follow up.
Treatment of CBM needs to be monitored and
evaluated clinically, mycologicaly,
hystopathologically every three or four months.
(Queiroz, 2017) The disease can be assessed as
clinically cured if the lesion resolution was obtained
completely, with sclerotic scar without subjective
symptoms such as pain or pruritus. (Queiroz,
2017,Hira, 2002) Mycological cure is defined by the
negative results of direct microscopic and culture.
(Queiroz, 2017) In this case direct examinations
with KOH showed negative result during four
months therapy. Histopathological cure is achieved
if there are no muriform cells, microabscesses and
granulomas, and are being replaced by the
appearance of chronic inactive inflammation and
fibrosis. (Queiroz, 2017) The variable cure rate of
CBM is 15%–80% depending on the severity of the
disease, and it will increase when two or more
modalities were used in combination. (Queiroz,
2015,Agarwal, 2017)
4 CONCLUSION
There is a risk of treatment failure and
recurrence in CBM. In a patient with severe and
extended lesion, the aim of treatment are to
reduce the lesion size and control the state of
the disease so that there will be no complication
and to improve patient quality of life.
Hira, 2002
Heat therapy is a potential therapeutic option
for CBM that is easy to use, affordable prices,
and combination with itraconazole showed
good clinical response in this case.
REFERENCES
Agarwal, R., Singh, G., Ghosh, A., Verma, K. K., Pandey,
M., & Xess, I., 2017. Chromoblastomycosis in India:
review of 169 cases. PLoS neglected tropical
diseases, 11(8), 1-13, e0005534.
Andrade, T. S., Castro, L. G., Nunes, R. S., Gimenes, V.
M., & Cury, A. E., 2004. Susceptibility of sequential
Fonsecaea pedrosoi isolates from
chromoblastomycosis patients to antifungal
agents. Mycoses, 47(5‐6), pp. 216-221.
Ameen, M., 2009. Chromoblastomycosis: clinical
presentation and management. Clinical and
Experimental Dermatology: Clinical
dermatology, 34(8), pp. 849-854.
Hay R.J., 2012. Deep fungal infections. In: Goldsmith
LA, Katz SI, Gilchrest BA, Paller AS, Leffel JD,
Wolff K, editor. Fitzpatrick’s dermatology in general
medicine. 8
th
Edition. New York: McGraw-Hill, 2312-
2317.
Hira, K., Yamada, H., Takahashi, Y., & Ogawa, H., 2002.
Successful treatment of chromomycosis using carbon
dioxide laser associated with topical heat
applications. Journal of the European Academy of
Dermatology and Venereology, 16(3), pp. 273-275.
Hiruma, M., Kawada, A., Yoshida, M., & Kouya, M.,
1993. Hyperthermic treatment of chromomycosis with
disposable chemical pocket
warmers. Mycopathologia, pp. 122(2), 107-114.
Hu, Y., Huang, X., Lu, S., Hamblin, M. R., Mylonakis, E.,
Zhang, J., & Xi, L., 2015. Photodynamic therapy
combined with terbinafine against
chromoblastomycosis and the effect of PDT on
Fonsecaea monophora in
vitro. Mycopathologia, 179(1-2),pp. 103-109.
Purim, K. S. M., Peretti, M. C., Fillus Neto, J., &
Olandoski, M., 2017. Chromoblastomycosis: tissue
modifications during itraconazole treatment. Anais
Brasileiros de Dermatologia, 92(4), pp. 478-483.
Queiroz-Telles, F., Esterre, P., Perez-Blanco, M., Vitale,
R. G., Salgado, C. G., & Bonifaz, A., 2009.
Chromoblastomycosis: an overview of clinical
manifestations, diagnosis and treatment. Medical
mycology, 47(1), pp. 3-15.
Queiroz-Telles, F., 2015. Chromoblastomycosis: a
neglected tropical disease. Revista do Instituto de
Medicina Tropical de São Paulo, 57, 46-50.
Queiroz-Telles, F., de Hoog, S., Santos, D. W. C.,
Salgado, C. G., Vicente, V. A., Bonifaz, A., ... & Pana,
Z. D., 2017. Chromoblastomycosis. Clinical
microbiology reviews, 30(1), pp. 233-276.
Santos, A. L., Palmeira, V. F., Rozental, S., Kneipp, L. F.,
Nimrichter, L., Alviano, D. S., ... & Alviano, C. S.,
2007. Biology and pathogenesis of Fonsecaea
pedrosoi, the major etiologic agent of
chromoblastomycosis. FEMS microbiology
reviews, 31(5), pp. 570-591.
Shantala, G.B., Rudresh, S.M., Nagarathnamma, T, 2011.
Chromoblastomycosis: A Case Report. JCDR, 5(4),
pp. 864-866.
Heat Therapy as an Excellent Adjuvant Treatment for Severe Chromoblastomycosis: A Case Report
409

Yanase, K., & Yamada, M., 1978.. Pocket-warmer'therapy
of chromomycosis. Archives of dermatology, 114(7),
pp.1095-1095.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
410
