
Fishtank Granuloma Treated with Combination of Minocycline and
Rifampicine
Alfonsus Rendy Laksditalia Nugroho
1
, Taufiq Hidayat
1
, Lita Setyowatie
1
, Krisna Ariaputra
1
, Diah
Prabawati Retnani
2
1
Departement of Dermatology and Venereology, Faculty of Medicine, Universitas Brawijaya / dr. Saiful Anwar
Regional General Hospital, Malang, Indonesia
5
Department of Pathology Anatomy, Faculty of Medicine, Universitas Brawijaya / dr. Saiful Anwar Regional General
Hospital, Malang, Indonesia
Keywords: fishtank granuloma, minocycline, rifampicine
Abstract: Fishtank granuloma is atypical mycobacterium infection with Mycobacterium marinum as causative agent,
primary risk of this condition are exposure with aquatic environment. It has no standard therapy, meanwhile
it is imperative to begin therapy as soon as possible before bad prognosis happen due to ascending infection
from skin to tenosynovium.
Men, 40 years old complains from painful bumps in the back of the hand,
ulcerating and indurated. Patient had undergone several therapies, but there were no improvement. Patient
got hobby of nurturing koi fishes, similar lesion found on patient’s fishes. General examination shows pain
score was 6/10. Dermatological examination dorsal manus dextra, with localized distribution, shows
erythematous nodules, well defined, quantity 6, size 0,5–2 cm, with ulcers, crusts and scales.
Histopathological examination shows poorly formed granulation tissues. Epidermis shows acanthosis and
some absent, while dermis shows connective tissue with many blood vessels and sparse inflammatory cells
of neutrophil, lymphocyte and histiocyte. No visible datia cells and caseous necrosis. Blood count shows
limphocytosis and slight increase of ESR. Patient being diagnosed as fishtank granuloma, got minocycline
2x100 mg, rifampicine 1x600 mg for three months. Lesion healed with scar, pain score reduced to zero were
achieved in second month. Therapy continued one month after complete healing. Fishtank granuloma often
misdiagnose and leads to late initial therapy, meanwhile this infection tend to be persistent and unable to
heal spontaneously. Combination of minocycline and rifampicine can increase therapeutical efectivity and
may support establishing diagnosis of fishtank granuloma.
1 INTRODUCTION
Fishtank granuloma is atypical mycobacterial
infection with Mycobacterium marinum as causative
agent, that obtain its name due to primary risk factor
of this condition which are exposure to aquatic
environment or water creatures. (Delphine et al,
2012,Wu et al, 2002) This pathogen exist in both
tropical or sea water. Mycobacterium marinum first
time being isolated by Aronson in 1926 from a dead
sea fish that being obtained from aquarium in
Philadelphia. In 1951, Norden and Linell able to
isolating it from swimmer who swim in the
contagious swimming pool in Sweden. In the year of
1962, Swift and Cohen begin to report two cases of
Mycobacterium marinum infection from tropical
fishes aquarium, and so it begin the term “fishtank
granuloma.” Since that time, the term “swimming
pool granuloma” has rarely being used because
chlorination of this reservoir make this condition
become rare to occur in swimming pool.(Bonamonte
et al, 2013) Mycobacterium marinum infection in
human that has been proved by culture was reported
in 66 patients from 1996 to 1998 in France, with
incidence 0.04 cases per 100,000 inhabitants per
year. According to published study being held in
USA, annual incidence of this ilness is 0.27
confirmed cases per 100,000 inhabitants.
(Bonamonte et al, 2013) In Asia, fishtank granuloma
incidence is not being reported yet in a large publish
study. However in 2012, Wu TS et al in Taiwan
suceed reporting 27 case finding of Mycobacterium
marinum from 1999 to 2010 in Changung memorial
hospital, while in Indonesia, there are only two case
Nugroho, A., Hidayat, T., Setyowatie, L., Ariaputra, K. and Retnani, D.
Fishtank Granuloma Treated with Combination of Minocycline and Rifampicine.
DOI: 10.5220/0008158203930397
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 393-397
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
393
report found from Fauziah SN et al in 2015 and
Barros T et al in 2016 both from RSCM Jakarta,
being treated with combination therapy of
minocycline and rifampicine with good clinical
improvement.(Fauziah et al, 2015,Baros et al, 2015)
Being reported within this case report, one case of
fishtank granuloma in male 40 years old with good
clinical improvement, the lesion healed with scar,
reduction of pain score to zero, after 2 months
therapy with combination rifampicine and
minocycline. Therapy was continued to the third
month to prevent recurrence.
2 CASE
Male, 40 years old came to Outpatient
Departement of Dermatology and Venereology
Saiful Anwar General Hospital with main complain
bumps that ulcerate in his hand since five months
before admission. Initially the bump was solitary,
the size was around 1 cm and look like boils and but
a few weeks, it become bigger, indurated and
painful. The bump was not itch, on a scale 0 out of
10, but it more painful on a scale 6 out of 10. After a
few week occur second bumps next to the first bump
and the bump got ulcerate. This past 3 months, occur
new two bumps closer to the wrist, with the same
characteristic as the previous bumps. No history of
punctured or being manipulated with sharp objects,
woods or branch of a plant. No history being bite by
his pets (patient have turtle and koi fishes as pets).
Patient clean the pond once every twice week and
patient never use gloves when cleaning the pond.
Patient recall that before the occurrence of the bump
that he complains, he has small wounds result from
boils in his wrist that breaks that he ignore
previously. Patient never have any history of chronic
cough more than 3 months. No history of losing
weight since this past years. Throughout the year,
the weight were consistent around 59 kg. After the
occurrence of second bumps, taken to General
Practitioner got zalf contains antibiotic but there not
much improvement. Go to dermatovenereologist, got
Injected with intra lesion corticosteroid but there
was not much changes. On May 2017 the
dermatovenereologist command patient to got
FNAB and culture from the ulcers. Because the
culture show growth of bacteria, the
dermatovenereologist give topical antibiotic therapy.
Not much improvement to the lesion. Patient got
history try to find therapy for his ilness to several
dermatovenereologist and follow the instruction
carefuly of topical therapy but there are no
improvement were achieved. Topical therapy that
patient ever got were nadifloxacine, erythromycine,
metronidazole, sulfur, salycilic acid and
dexpanthenol. Patient never apply traditional herbals
or any other substances to his wounds. Patient is
single. Working as computer technician. Patient got
hobbies of nurturing koi fishes in aquarium, ponds
and have turtles. He clean the fishtank and pond
once a week. No history got bite by his turtle or any
wound appear from his hobbies. But according to the
patient he has history of having boils that breaks and
leave a wound in his wrist and that time, he keep
cleaning the fishtanks anyway with the existing
wound. According to the patient some of his fishes
have ulcer in their body part. Patient clean his yard
twice a month by unplug the wild grasses with bare
hands. He do it to make his garden clean. Patient do
not like gardening or nurturing a specific plant.
Physical examination shows patient compos mentis,
with good general condition.
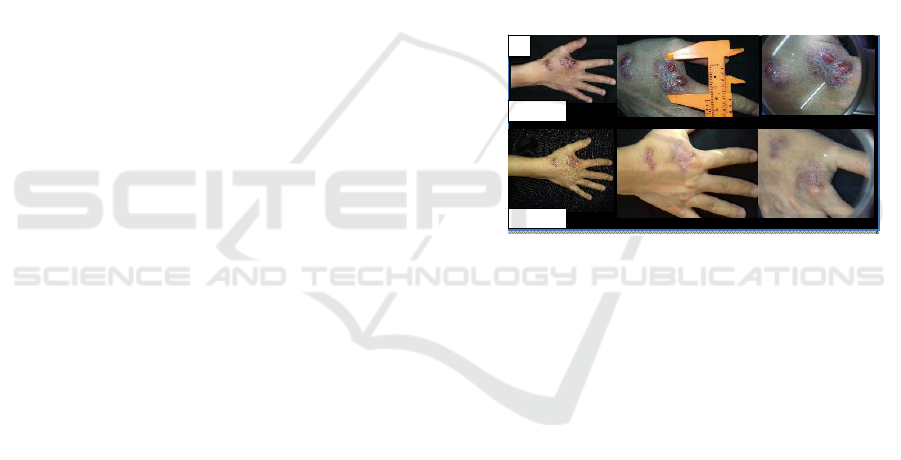
Figure 1. Clinical improvement after 3 month of
rifampicine 1x600mg and minocycline 2x100mg
Dermatological examination from dorsal manus
dextra, with localized distribution, shows
erythematous nodules, well defined, round to oval,
some confluence, quantity 6, size 0,5 cm – 2 cm,
with ulcer, crust and scales. Zeehl Neelsen stain
examination from the lesion did not show acid fast
bacillus. Blood count examination show
limphocytosis and increase of erythrocyte
sedimentation rate. Chest X-ray within normal
limits, no sign of tuberculosis.
Histopathological examination with HE & PAS
stain shows poorly formed granulation tissues with
no malignancy. Epidermis absent in some part and
acanthosis in the other , while dermis area shows
connective tissue with many blood vessels and
sparse inflammatory cells of neutrophil, lymphocyte
and histiocyte. No visible datia cells and caseous
necrosis. Patient being diagnosed as fishtank
granuloma and being planned for therapy with
rifampicine 1x600 mg and minocycline 2x100 mg
for three months.
B
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
394
3 DISCUSSION
Fishtank granuloma is pathologic condition
causing granulomatous skin and soft tissue lesions in
humans that occur because of Mycobacterium
marinum, aerobic, waterborne atypical
mycobacterium that belongs to Runyon’s
classification Group I photochromogenic non-
tuberculous mycobacteria. This pathogen causing
chronic systemic infections in fish and amphibians,
commonly found in non-chlorinated water
occupying many aquatic environments. In one large
published study by Jernigan et al in 2000, they
observed 193 infections reported from 1962 through
1996 and found that this pathogen were majority
aquarium-related.(Rallis, 2007,Jernigan,
2000,Petrini, 2006 )M. marinum infection occurs
two weeks after direct inoculation of the organism
either from fish fins, bites or from the handling of
aquariums. In 90% of cases, this takes place via
trauma to the upper extremity and do not
transmittable from person to person.(Delphine et al,
2012,Rallis, 2007,Bhatty et al, 2000) In this case
patient got hobby of nurturing koi fishes, and direct
contact with koi fishes and turtle. He also has habit
of cleaning the pond and aquarium without latex
gloves. Patient recall that he has minor lesion few
weeks before the occurrence of the lesion.
Fishtank granuloma begins as a violaceous
papule at the site of a trauma 2-3 weeks after
inoculation. Dermatological examination shows
nodule or psoriasiform or verrucous plaque, usually
occur in hands, feet, elbows or knees.
Infections with
M. marinum can be classified into 4 clinical
categories; Type I (1–3 lesions), Type II: numerous
(> 3) lesions) Type III: deep infections
(tenosynovitis until osteomyelitis), Type IV:
disseminated infection, lung involvement and other
systemic manifestations.(Delphine et al, 2012,Rallis,
2007,Bhatty et al, 2000) Diagnosis is usually
delayed, because most physicians are unfamiliar
with the disease and a failure to establish a history of
exposure to aquatic environments. Therefore, key
diagnostic elements for M. marinum infections are a
high index of suspicion raised by negative bacterial
tissue cultures, poor response to conventional
antibiotic treatments and a history of aquatic
exposure.
4
Bonamonte et al in 2013, report acid-fast
bacilli identification only can be found in 6.7% case
using Ziehl-Neelsen stain, in accordance with the
low detection rates reported in the international
literature.(Bonamonte et al, 2013) In this patient,
regarding the clinical manifestation, Patient suffer
from fishtank granuloma type II with history of poor
response to various antibiotics and and history of
exposure with aquatic environments. Disseminated
distribution from the lungs can be excluded since
there were no history of chronic cough, or lung
tuberculosis an chest X-Ray of this patient was
normal. The diagnosis of fishtank granuloma was
established based on clinical manifestation and was
then confirmed with histopathological examination
of skin tissues.
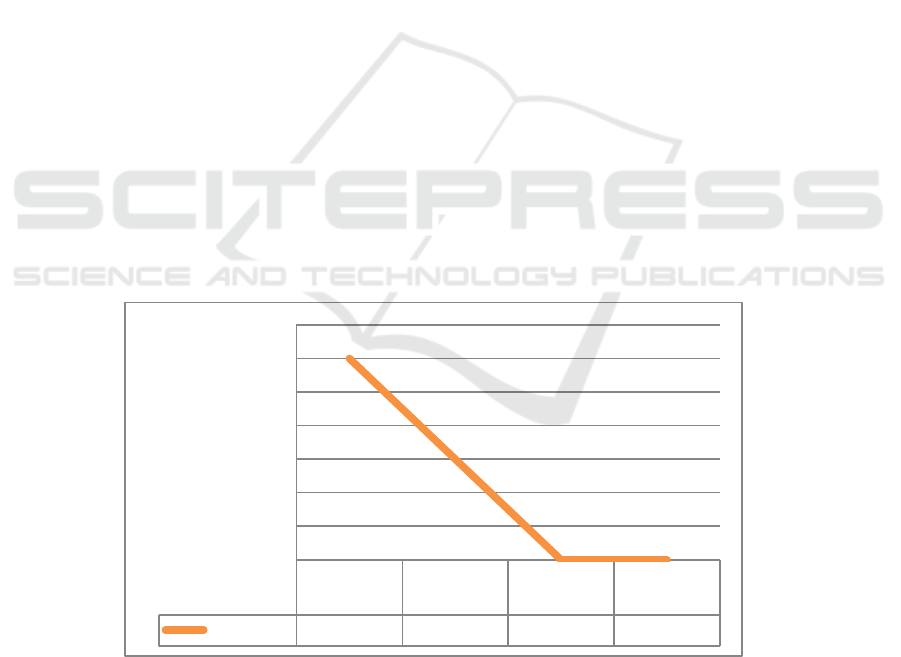
Figure 2. Pain score reduce from 6 to 3 on 1st month, completely zero in second month and the third month
There is no standard regimen for therapy of
choice for fishtank granuloma because low
incidence of this infection, and M. marinum is
naturally multi-drug resistant species and treatment
is based primarily on the personal experience and
preference of individual investigators, without any
large studies or randomized controlled trial. In
superficial cutaneous infections, minocycline,
clarithromycin, doxycycline and trimethoprim-
sulfamethoxazole being reported as effective
Before
therapy
1stmonth
2nd
Month
3rdmonth
Painscore
6300
0
1
2
3
4
5
6
7
PainScore
Fishtank Granuloma Treated with Combination of Minocycline and Rifampicine
395

monotherapy, but drug resistance varies and thereby
combination therapy using two drugs may be
required.(Rallis, 2007,Doug et al, 2012
)
Like other
atypical mycobacteria, patients suspected of having
atypical mycobacterial skin infections are generally
treated empirically.(Rallis, 2007,Jernigan, 2000)
Minocycline, The second-generation tetracyclines
are the most frequently reported effective treatments.
It inhibits bacterial protein synthesis by preventing
the association of aminoacyl-tRNA with the
bacterial ribosome.(Delphine et al, 2012,Jernigan,
2000)
Cummins et al 2005 describe a case of M.
marinum that improved rapidly with minocycline
despite a lack of response to doxycycline after 6
weeks. Recent in vitro studies with wild-type M.
marinum Strains have shown minocycline to be
more potent than doxycycline. In addition, at least
one minocycline-sensitive strain has shown
resistance to doxycycline.(Cummins et al,
2005,edelstein et al, 1994) Bonamonte et al 2013
collecting 15 case report from 1987 to 2011 and
found 13 cases effectively treat by minocycline 200
mg per day with clinical improvement after 2-3
months.(Bonamonte et al, 2013) Rifampicine in a
dose of 600 mg daily, has been used effectively in
fishtank granuloma either alone or in combination
with other agent. Inhibit RNA synthesis and result in
termination of bacterial replications.(Bonamonte et
al, 2013,Cummins et al, 2005) Speight et al in 1997
has suceed giving rifampicine as single therapy for
fishtank granuloma in 14 month old girl, the patient
got rifampicine as single therapy because
ethambutol and minocycline were contraindicated
due to the patient’s age. In 1994 Elstein et al
collected 31 case report of fishtank granuloma and
conclude that among other treatment, rifampin in
combination with other antimycobacterial appeared
to be more successful and in the next best for fish
tank granuloma therapy is minocycline
treatment.(edelstein et al, 1994,Speight et al,1997)
Duration of therapy that consider effective for
management of atypical mycobacteria is ranging
from four to thirty eight weeks , depends on how the
lesion reponse clinically. It is suggest that the
treatment is continued for next four week after
lesion has resolved to prevent recurrence of illness.
Monotherapy with antimycobacterial agent reported
to be effective but since there are variety in drug
resistency in M. marinum, combination therapy of
usually two drugs were strongly suggested.(Rallis,
2007,Fauziah et al, 2015,Baros et al, 2015) Fauziah
et al in 2016 was reported Mycobacterium marinum
infection that successful being treated with
combination of rifampicine and minocycline, after 2
months.(Fauziah et al, 2015)
4 CONCLUSIONS
Clinical, histopathological feature and clinical
response to minocycline and rifampicine support
establishing diagnosis of fishtank granuloma. There
are clinical improvement, the lesion healed with scar
and reduction of pain score to zero after two months
giving rifampicine 600 mg daily and minocycline
200 mg twice daily, and application of wet gauze
(Na Cl 0,9%) twice daily in this patient. Therapy
were being continued 1 month after resolved of
lesion and pain, to prevent recurrence (Baros et al,
2015) Laboratory examination after release from
treatment shows no elevated liver and renal enzyme,
normal erythrocyte sedimentation rate (ESR) and
other normal laboratory counts. Blue black
discoloration, as side effect of minocycline in the
lesion appear after 3 months therapy but subside
after 1 months release from treatment.
ACKNOWLEDGEMENTS
If any, should be placed before the references
section without numbering.
REFERENCES
Adams, R. M., Remington, J. S., Steinberg, J., & Seibert,
J. S., 1970. Tropical fish aquariums: a source of
Mycobacterium marinum infections resembling
sporotrichosis. JAMA, 211(3), pp. 457-461.
Barros, T., Legiawati, L., Yusharyahya, S. N., Sularsito, S.
A., & Wihadi, I., 2015. Atypical mycobacterial
infection mimicking carbuncle in an elderly patient: A
case report. Journal of General-Procedural
Dermatology & Venereology Indonesia, 32-35.
Bonamonte, D., De Vito, D., Vestita, M., Delvecchio, S.,
Ranieri, L. D., Santantonio, M., & Angelini, G.,2013.
Aquarium-borne Mycobacterium marinum skin
infection. Report of 15 cases and review of the
literature. European Journal of Dermatology, 23(4),
510-516.
Bhatty, M. A., Turner, D. P., & Chamberlain, S. T., 2000.
Mycobacterium marinum hand infection: case reports
and review of literature. British journal of plastic
surgery, 53(2), pp. 161-165.
Cummins, D. L., Delacerda, D., & Tausk, F. A., 2005.
Mycobacterium marinum with different responses to
second-generation tetracyclines. International journal
of dermatology, 44(6), pp. 518-520.
Delphine, J. Lee., Thomas, H. Rea., & Robert, L. Modlin.,
2012. Leprosy. Dalam: Wolff Klaus, Goldsmith
Lowell A, Katz Stephen I, Gilchrest Barbara A, Paller
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
396

Amy S, Leffel David J, penyunting. Fitzpatrick’s
Dermatology in General Medicine. Edisi ke 8. New
York. McGraw-Hill; 2012. h.2253-63 /6.
Dong, D., Wang, D., Li, M., Wang, H., Yu, J., Wang, C.,
... & Gao, Q., 2012. PPE38 modulates the innate
immune response and is required for Mycobacterium
marinum virulence. Infection and immunity, 80(1), pp.
43-54.
Edelstein, H., 1994. Mycobacterium marinum skin
infections: report of 31 cases and review of the
literature. Archives of Internal Medicine, 154(12), pp.
1359-1364.
Fauziah, S. N., Legiawati, L., Sularsito, S. A.,
Yusharyahya, S. N., Rihatmadja, R., Sirait, S. P., ... &
Widyasari, I., 2016. Atypical mycobacterial infection
resembles sporotrichosis in elderly patient. Journal of
General-Procedural Dermatology & Venereology
Indonesia, pp. 62-67.
Jernigan, J. A., & Farr, B. M., 2000. Incubation period and
sources of exposure for cutaneous Mycobacterium
marinum infection: case report and review of the
literature. Clinical infectious diseases, 31(2), pp. 439-
443.
Petrini, B., 2006. Mycobacterium marinum: ubiquitous
agent of waterborne granulomatous skin
infections. European Journal of Clinical Microbiology
and Infectious Diseases, 25(10),pp. 609-613.
Rallis, E., 2007. Koumantaki-Mathioudaki E. Treatment
of Mycobacterium marinum cutaneous infections.
Expert Opin Pharmacother 8, pp. 2965-2978.
Speight, E. L., & Williams, H. C., 1997. Fish Tank
Granuloma in a 14-Month-Old Girl. Pediatric
dermatology, 14(3), pp. 209-212.
Wu, T. S., Chiu, C. H., Yang, C. H., Leu, H. S., Huang, C.
T., Chen, Y. C., ... & Chia, J. H., 2012. Fish tank
granuloma caused by Mycobacterium marinum. PloS
one, 7(7), e41296.
Fishtank Granuloma Treated with Combination of Minocycline and Rifampicine
397
