
Low Fluence Q-Switched Neodymium-Doped Yttrium Aluminium
Garnet (LFQSNd:YAG 1064nm) versus Combination of LFQSND:
YAG 1064nm and Microneedle Fractionated Radiofrequency
(MFRF) for Treatment of Indonesian Melasma Patients. Which is
Better?
Ary Widhyasti Bandem
1
, Ni Putu Susari Widianingsih
1
, Trisniartami Setyaningrum
1
, Cita Rosita
Sigit Prakoeswa
2
1
Surabaya Skin Centre, Indonesia
2
Departement of Dermato-Venerology Dr Soetomo Teaching Hospital Surabaya, Indonesia
Keywords: melasma, laser, microneedle fractionated radiofrequency, Janus
Abstract: Melasma treatment is still very challenging and cannot definitely be cured, since recurrence are high. Many
modalities used to treat melasma, such as broadspectrum sunscreen, lightening agents, intense pulsed light,
lasers, and a newly microneedle fractionated radiofrequency specially design to treat melasma. In this study,
we enrolled 5 Indonesian melasma patients, Fitzpatricks skin type III-IV, 36-65 years old and given low
fluence Q switched Nd:YAG 1064 nm and other half face added the microneedle fractionated
radiofrequency treatment. Patients were given 4 treatments 2-4 weeks apart. Parameters for the laser
treatment using spot size 6 or 8 mm, 1,6- 1,8 J/cm2, 10 Hz, endpoint slight erythema, and for the
microneedle fractionated radiofrequency, power 3, depth 1-1,5 mm, 100-150 shots The improvement of
pigmentation lesion, skin tone and side effects were evaluated using the Janus imaging system. Conclusion:
Melasma treatment using combination low fluence Q Switched Nd:YAG 1064 nm and microneedle
fractionated radiofrequency was better than low fluence Q Switched Nd:YAG1064 nm alone and no serious
side effects found during both treatment.
1 INTRODUCTION
Melasma is considered one of the most challenging
hyperpigmentation disorder to treat, especially in
Indonesian skin type. Many factors contribute in
developing melasma, such as genetic factors, sun
exposures, pregnancy, oral contraceptives,
phototoxic and photo allergic drugs and cosmetics.
Melasma appears as symmetric facial
hypermelanosis, with irregular light brown to dark
brown macules and patches on face, predominantly
on malar areas, forehead, and chin but until now the
etiology and pathogenesis are not fully understood.
Many treatments modalities are used to cure
melasma in Indonesia, including broad spectrum
sunscreen, topical lightening agents, retinoids,
corticosteroid, chemical peelings, lasers and other
light based energy devices. Unfortunately, there is
no definite cure for melasma. Lasers may worsen the
melasma and cause post inflammatory hyper
pigmentation, but recently laser experts have found
that using the low fluence parameters (laser toning)
give better results (Kim et al., 2012; Fabi et al.,
2014; Trivedi, Yang, and Cho, 2017; Kauvar).
New
treatment for melasma is always awaited.
In 2016, a new device with microneedle
fractionated radiofrequency technology was
specially design to treat melasma, particulary
refracter melasma with the vascular involvement.
5-7
However there is no report on the safety and
effectiveness in Indonesian melasma patients. Aim
of this study is to evaluate the changes in skin tone
and spot pigmentation on the face of melasma
patients, comparing the low fluence Q switched
Nd:YAG 1064 nm versus the combination of low
fluence Q switched Nd:YAG 1064 nm and
microneedle fractionated radiofrequency using the
Janus imaging system.
Bandem, A., Widianingsih, N., Setyaningrum, T. and Prakoeswa, C.
Low Fluence Q-Switched Neodymium-Doped Yttrium Aluminium Garnet (LFQSNd:YAG 1064nm) versus Combination of LFQSND:YAG 1064nm and Microneedle Fractionated Radiofrequency
(MFRF) for Treatment of Indonesian Melasma Patients. Which is Better?.
DOI: 10.5220/0008156903330337
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 333-337
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
333

2 METHODS
We enrolled 5 Indonesian woman patients with
melasma, age 36-65 years old, Fitzpatricks Skin type
III-IV in this study. Before treatment, patients signed
informed consent and given topical anesthesia using
topical eutectic mixture of 2,5% lidocain and 2,5 %
prilocaine. All patients were treated with low
fluence Q switched Nd:YAG 1064 nm spotsize 6 or
8 mm with fluence 1,6-1,8 J/cm, 10 Hz, with end
point slight erythema, and half face of each patients
received an addition of microneedle fractionated
radiofrequency treatment. The parameters of
microneedle fractionated radiofrequency were:
power 3, depth 1-1,5 mm, 100-150 shots. Interval
treatment was 2-4 weeks and all other treatments
were continued such as broadspectrum sunscreens,
and topical lightening agents. Photographs were
taken using normal light, polarization light and UV
light with the skin analyzer Janus 2 done by the
same technician. Evaluation of data and photographs
was done by another dermatologist.
3 RESULTS
Table 1: Mean value of skin tone and spot pigmentation using Janus imaging system
Area Treatment LFQS1064nm LFQS1064nm & MFRF
Upper chee
k
Before 32.2 ± 2.6 (29-36) 33.6 ± 2.7 (31-38)
Skin Tone Afte
r
32.6 ± 1.5 (30-34) 32.6 ± 2.6 (29-35)
Lower chee
k
Before 32.4 ± 0.5(32-33) 32.9 ± 0.2 (33-32.9)
Afte
r
32.3 ±0.7 (31.5-33) 32.9 ± 0.2 (33-32.9)
Spot Upper chee
k
Before 32.6 ±12.8 (19-46) 38.8 ±10,4 (29-53)
Pigmentation Afte
r
27.8 ±14.9 (10-43) 28.6 ±10.9 (15-40)
Middle
chee
k
Before 33.2 ±7.4 (21-40) 36 ±13.8 (22-52)
Afte
r
31.4 ± 13.1 (10-45) 24.4 ± 11.3 (13-40)
Lower
Chee
k
Before 34.6 ± 9.5 (23-45) 33.8 ±10 (24-47)
Afte
r
39 ± 9.9 (28-51) 19.4 ± 8.4(12-30)
LFQS1064nm : Low fluence Q-Switched Neodymium-Doped Yttrium Aluminium Garnet 1064nm
MFRF: Microneedle Fractionated Radiofrequency
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
334
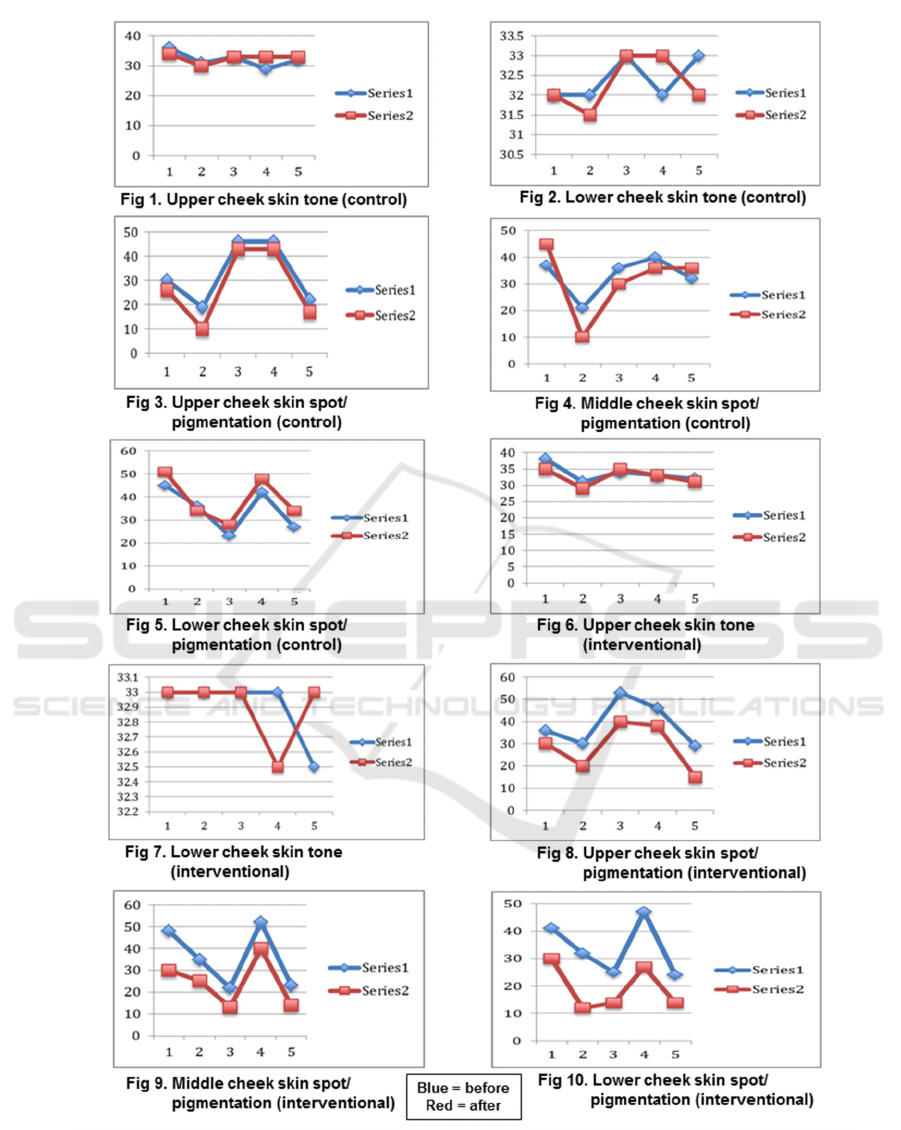
Figure 1: The line graph of skin tone and spot pigmentation (before-after) in split face control and interventional area.
Low Fluence Q-Switched Neodymium-Doped Yttrium Aluminium Garnet (LFQSNd:YAG 1064nm) versus Combination of LFQSND:YAG
1064nm and Microneedle Fractionated Radiofrequency (MFRF) for Treatment of Indonesian Melasma Patients. Which is Better?
335

Figure 2: Photograph using Janus Imaging System: left side of patient: combination LFQSNd:YAG1064nm and
Microneedle Fractionated Radiofrequency. right side: LFQSNd:YAG1064nm.
4 DISCUSSION
Janus imaging system take images in 3 different
lights, normal light for evaluating wrinkles and
pores, polarized light for evaluating spot and
pigmentation while UV light to evaluate sebum and
porphyrin (p.acnes). In the polarized imaging of the
Janus system we found that the skin tone for our
patients in this study did not improve consistently in
both treatments, the LFQS1064nm and the
combination LFQS1064nm and microneedle
fractionated radiofrequency (figure 1,2,6,7). Skin
tone is level of darkness of the overall skin. The skin
tone can be uneven due to excessive workload,
stress, pigmentation, sunburn, keratin and skin
problems. Janus imaging system record that
melasma patients have poor skin tone before and
after treatment. We conclude in this study that skin
tone in Janus imaging system is not a realible
parameter to evaluate the efficacy of melasma
treatment. These findings were similar to research
done by Prakoeswa CRS, Pratiwi FD, et al. Skin
tone was found not significant to evaluate the
improvement in photoaging before and treatment
using amniotic membrane stem cell conditioned
medium (AMSC-CM) (Prakoeswa, nd).
Evaluation of the skin pigmentation and spots of
melasma decrease on both sides of the face, except
two patients (the middle cheek), and three patients
(the lower cheek) that were only given LFQS1064
nm. These areas showed an increase value of
pigmentation (figure 2,4). These findings may be
due to that the lesion had more intense pigmentation,
darkening effect post laser treatment or the lesions
were refracter to LFQS 1064nm treatment. Spots
and pigmentation in the upper, middle, and lower
cheeks with combination treatment, we found that
the pigmentation consistently decreased after
treatment (figure 8,9,10). This may due to the
proposed mechanism of the microneedle fractionated
radiofrequency, where the microneedle fractionated
radiofrequency may work through modes of action,
including enhancing permeability of topical
lightening agents and increasing degradation of
dermal vasculature (Choi and Choi; Choi, et al.,
2015). The therapeutic topical lightening agents are
known to be limited by their poor transepidermal
penetration, so maybe the microneedle
radiofrequency creates micro channels to enhance
transdermal drug delivery. This micro environment
altered by the microneedle fractionated
radiofrequency may caused the reversal of solar
elastosis, causing decrease melanogenesis and
lightening of the melasma. Not like the fractionated
lasers which cause more crusting, the microneedle
fractionated radiofrequency did not show any
obvious microcrusting or increased epidermal
Splitface:
Before treatment
After 4 treatments
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
336

shedding. The effectiveness combination treatment
of microneedle fractionated radiofrequency and
topical lightening agents reported by Choi et al,
showed good improvement in melasma lesion (Choi
and Choi; Choi, et al., 2015).
Laser toning using low fluence Q Switched
Nd:YAG 1064 nm for melasma treatment has gain
popularity since a few years ago. It is an addition
treatment to previous treatment such as topical
lightening agents, broadspectrum sunscreens, and
chemical peelings. The exact mechanism of laser
toning on the improvement of melasma is still
unclear. It has been proposed that melanin granules
are fragmented and dispersed into the cytoplasm
without destruction by repetitive laser energy with a
subphotothermolytic fluence over large spot size
known as subcellulear selective photothermolysis.
Effectiveness of this treatment various and melasma
lesions can recur or get darkened and rebound
hyperpigmentation can occur. Common side effects
were physical urticaria, acneiform eruption, minute
petechiae, whitening of fine facial hair, herpes
simplex reactivation, leukoderma and mottled
hyperpigmentation (Sim et al., 2014). In this study
patients tolerated the laser toning and the
microneedle fractionated radiofrequency and found
no serious side effect, only slight erythema which
subside after few hours.
Future studies to evaluate effectiveness treatment
of melasma may easily done using Janus imaging
system by evaluating spot pigmentation, and for
generalization of the treatment effectiveness still
need larger subjects, more treatment sessions, and
long term follow up to monitor recurrences.
5 CONCLUSION
Patients recieving low fluence Q switched
Nd:YAG1064nm laser and microneedle fractionated
radiofrequency showed better improvement in spots
pigmentation of melasma compared to only using
low fluences QSNd:YAG 1064nm laser. Treatments
were well tolerated and no serious side effects notice
during both treatments.
ACKNOWLEDGEMENT
The work was supported by Surabaya Skin Centre
and PT Regenesis
DECLARATION OF INTEREST
The authors report no conflicts of interest. The
authors alone responsible for the content and
writing of the paper.
REFERENCES
Choi, M., Choi, S., Successful treatment of melasma
resistent to low fuence QSNY laser and topical
medication using fractional radiofrequency needle
device.
Choi, M., Choi, S., Kang, J.S., Cho, S.B.. Successful
treatment of refractory melasma using invasive micro-
pulsed electrical signal device, 2015. Med Laser, 4(1),
pp.39-44.
Fabi, S.G., Friedmann, D.P., Massaki, A.B.N., Goldman,
M.P., 2014. A randomized split face clinical trial of
low fluence Q switched Neodynium-Doped Yttrium
Aluminum Garnet (1,064 nm) Laser versus low
fluence Qswitched Alexandrite laser (755nm) for the
treatment of facial melisma. Lasers in Surgery and
Medicine, 46, pp.531-537.
Kauvar, A., The evolution of melasma therapy: Targeting
melanosomes using low fluence Q switched
Neodymium-doped yttrium aluminium garnet lasers.
Semin Cutan Med Surg, 31, pp.126-132.
Kim, J.E., Chang, S.E., Yeo, U.C., Haw, S., Kim, L.H.,
Histopathological study of treatment of melasma
lesions using a low fluence Q switched 1064nm
neodymium yttrium aluminium garnet laser, 2012.
Clinical and experimental dermatology, 38, pp.167-
171.
Na, J., Zheng, Z., Dannaker, C., Lee, S.E., Kang, J.S.,
Cho, S.B., Electromagnetic initiation and propagation
of bipolar radiofrequency tissue reactions via invasive
non insulated micro-needle electrodes.
Prakoeswa, C.R.S., Pratiwi, F.D., Murtiastutik, D.,
Citrashanty, I., Indramaya, D.M., Sukanto, H., and
Rantam, F.A., Photoaging: Effect of amniotic
membrane stem cell-conditioned medium (AMSC-
CM).
Sim, J.H., Park, Y.L., Lee, J.S., Choi, W.B. et al., 2014.
Treatment of melasma by low fluences 1064nm Q-
switched Nd:YAG laser. Journal of Dermatological
Treatment, 25, pp.212-17.
Trivedi, M.K., Yang, F.C., Cho, B.K., A review of laser
and light therapy in melisma, 2017. Internasioal
Journal of women’s Dermatology.
Low Fluence Q-Switched Neodymium-Doped Yttrium Aluminium Garnet (LFQSNd:YAG 1064nm) versus Combination of LFQSND:YAG
1064nm and Microneedle Fractionated Radiofrequency (MFRF) for Treatment of Indonesian Melasma Patients. Which is Better?
337
