
Ki-67 Staining as a Tool to Differentiate Verrucous Carcinoma from
Condyloma Acuminatum on Skin Biopsy
Willy Sandhika
Department of Anatomic Pathology Universitas Airlangga Surabaya, Indonesia
Keywords: Ki-67 Staining, Verrucous Carcinoma, Condyloma Acuminatum.
Abstract: Verrucous carcinoma is a variant of well differentiated squamous cell carcinoma that slowly growing and
rarely metastasize. It grows as polypoid mass with verrucous surface. Macroscopically can produce exophytic
appearance that mimic condyloma acuminatum. On skin biopsy specimen that usually tiny tissue, the
microscopic appearance can be similar with condyloma acuminatum because it composed of well
differentiated squamous epithelial cells. Ki-67 staining can label proliferating cell even they are not in mitotic
state. Verrucous carcinoma has high proliferation index while condyloma acuminatum has low index. This
study want to prove whether Ki-67 staining can serve as reliable marker to differentiated verrucous carcinoma
from condyloma acuminatum. Sixteen case are retrieve from archive of Pathologic Department Dr, Soetomo
Hospital consist eight case verrucous carcinoma and condyloma acuminatum respectively.
Immunohistochemical staining with antibody Ki-67 was performed on each case. Squamous epithelial cells
that stain positive were count from each case, and the results were statistically compare between verrucous
carcinoma and condyloma acuminatum. The result of this study shows significant difference in number of Ki-
67 positive cells in verrucous carcinoma compare to condyloma acuminatum. There is also different in
squamous cell layer that expressed Ki-67. It is concluded that Ki-67 staining is a reliable tool that can
differentiate verrucous carcinoma from condyloma acuminatum on skin biopsy specimen.
1 INTRODUCTION
Verrucous carcinoma is a variant of well
differentiated squamous cell carcinoma. It is grow
exophytic with verrucous surface. Unlike squamous
cell carcinoma, it grows slowly with no metastatic
potential and behave as low grade malignancy.
Verrucous carcinoma can arise in anogenital region
and should be distinguished from condyloma
acuminatum (Liu, G., Li, Q., Shang, X., Qi, Z., Han,
C., Wang, Y., Xue, F., 2016). Verrucous carcinoma at
anogenital region can give clinical features
mimicking giant condyloma acuminatum which is
benign proliferative lesion caused by human
papilloma virus (HPV). On microscopic examination,
both disease can give similar features such as
acanthosis with papillomatosis with minimal nuclear
atypia. On the other hand, warty squamous cell
carcinoma can arise in giant condyloma acuminatum
making it more complicated. Therefore, it takes a
reliable test to differentiate verrucous carcinoma from
condyloma acuminatum especially in giant form
(Bambao, C., Nofech-Mozes, S., Shier, M., 2010).
Ki-67 protein are expressed in all proliferating
cells. Since the nature of malignancy is uncontrolled
excessive proliferation, examination of tumor tissue
with Ki-67 theoretically can be used as reliable tool
to detect malignant transformation in condyloma
acuminatum (Li, L. T., Jiang, G., Chen, Q., Zheng, J.
N, 2015). The aims of this study was to prove whether
Ki-67 stain can distinguish verrucous carcinoma from
condyloma acuminatum.
2 METHODS
Blok paraffin from verrucous carcinoma and
condyloma acuminatum each eight case (totally
sixteen case) were retrieved from archive of
Pathology department Dr. Soetomo Hospital
Surabaya. These paraffin blocks were sliced 6 m
thick and were placed in object glass to perform
immunohistochemistry stain with Ki-67 antibody.
Microscopic analysis were made by light microscope
to count Ki-67 positive cells. Only squamous cells
Sandhika, W.
Ki-67 Staining as a Tool to Differentiate Verrucous Carcinoma from Condyloma Acuminatum on Skin Biopsy.
DOI: 10.5220/0008156102990301
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 299-301
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
299
that expressed Ki-67 protein were count as positive.
The number of positive cells were count in area
40.000 m
2
using microscopic graticulae at 400 times
magnification. The number of squamous epithelia
cells that expressed Ki-67 protein were tabulated and
statistically analyzed to assessed is there significance
difference in number from verrucous carcinoma
compare to condyloma acuminatum.
3 RESULTS
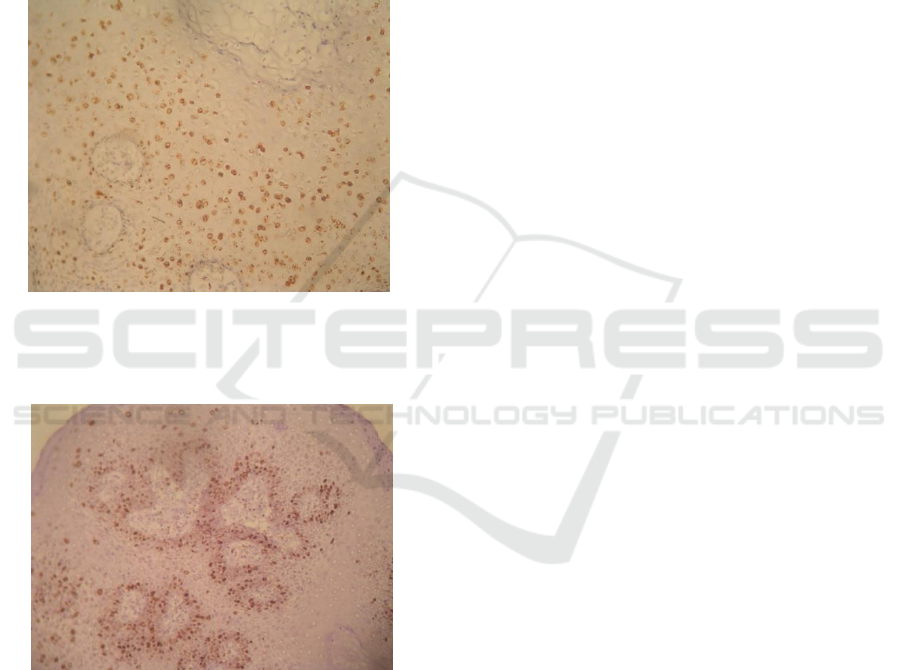
Figure 1: Expression of Ki-67 protein in verrucous
carcinoma specimen. Ki-67 were expressed in all layer of
squamous epithelia cells. (Ki-67 immunohistochemistry
staining 400X magnification).
Figure 2: Expression of Ki-67 protein in condyloma
acuminatum specimen. Ki-67 were expressed mainly at
basal layer of squamous epithelia cells, only few scattered
cell in spinous layer expressed Ki-67. (Ki-67
immunohistochemistry staining, 400X magnification).
On microscopic examination there is significant
difference in Ki-67 positive cell from verrucous
carcinoma (56,75±9,00) compare to condyloma
acuminatum (22,25±4,40) (p=0.000). At cut off value
40 cells per 40.000 m
2
area, Ki-67 staining can
differentiate all case of verrucous carcinoma from
condyloma acuminatum which means 100 percent of
accuracy.
The pattern of Ki-67 positive cells were also differ
on verrucous carcinoma compare to condyloma
acuminatum. On verrucous carcinoma, Ki-67 were
expressed in all layer of squamous epithelia (figure 1)
while in condyloma acuminatum, the Ki-67 were
expressed only in basal layer (figure 2).
4 DISCUSSION
Ki-67 protein were expressed in proliferating cells.
Ki-67 protein can be detected within the nucleus of
proliferating cells during all active phases of the cell
cycle i.e. G
1
, S, G
2
and mitosis, but it is not expressed
in resting cells G
0
. Therefore it an excellent marker
for determining proliferative activity (Scholzen, T.,
Gerdes, J., 2000). Assessment of Ki-67 positive cell
can give different result from mitotic count since Ki-
67 were expressed in all proliferation cycle. Ki-67
index has been used for evaluating prognostic test for
disease progression in several cancer (Jonat W. and
Arnold N, 2011). In skin tumor, Ki-67 evaluation can
be used as a marker indentify a malignant process.
Leblebici has performed immunohistochemical
staining with Ki-67 on keratoacanthoma compare
with squamous cell carcinoma. It gives 81%
sensitivity and 100% specificity in detecting
malignant squamous cell from benign squamous
epithelial cells (Leblebici, C., Pasaoglu, E., Kelten,
C., Darakci, S., Dursun, N., 2017).
This study give different result in number of Ki-
67 positive cells as well as the pattern of Ki-67
positive cells. In verrucous carcinoma, the number
squamous epithelial that expressed Ki-67 is larger
significantly compare to that in condyloma
acuminatum. As it was count on 40.000 m area, the
verrucous carcinoma always have more than 40 Ki-
67 positive cells while squamous epithelia in
condyloma acuminatum consistently give less than 40
positive cells. It means 100 percent of accuracy.
There is also difference in staining pattern of
squamous cells that express Ki-67 protein. In
condyloma acuminatum, cells that express Ki-67
mostly on basal layer. Only a few scattered cells in
upper layer express Ki-67 whereas in verrucous
carcinoma, squamous cells from all layer express Ki-
67 protein.
Distinguishing condyloma acuminatum from
verrucous carcinoma are not always give clear-cut
criteria, since giant condyloma acuminatum can give
similar feature both macroscopic and microscopically
with verrucous carcinoma. Condyloma acuminatum
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
300

usually behave as benign proliferative lesion with no
malignant potential but in a few circumstances it can
undergo malignant transformation. Papapanagiotou
has reported malignant transformation of giant
condyloma at perianal area (Papapanagiotou, I.K.,
Migklis, K., Ioannidou, G., Xesfyngi, D., Kalles, V.,
Mariolis-Sapsakos, T., Terzakis, E., 2017). The
coexistence of condyloma with verrucous carcinoma
make it more complicated in diagnosis since the
benign process can contain focus of some malignant
cells making malignant marker was strongly required
for benign looking cases (ErmanVlahovic, M., Vlahovic,
J., Mrcela, M., Hrgovic, Z., 2017).
Sometimes microscopic examination with
hematoxylin-eosin staining cannot detect malignant
transformation. Huang has reported a giant
condyloma acuminatum with benign microscopic
feature give recurrent lesion with malignant feature
(Huang SM, Leung WH and Chen BF, 2007).
Therefore it need an additional staining to detect
microscopic malignancy that involve a few epithelial
cells.
Ki-67 protein which expressed in proliferating
cells has been used to determine tumor grade in many
cancer has potential ability to differentiate
malignancy from benign process and also useful for
detection focus of malignant transformation that arise
in benign lesion (Jonat W. and Arnold N, 2011).
5 CONCLUSION
Ki-67 staining is useful tool for differentiate
verrucous carcinoma from condyloma acuminatum
with 100 percent accuracy.
REFERENCES
Bambao, C., Nofech-Mozes, S., Shier, M., 2010. Giant
condyloma versus verrucous carcinoma: A case report.
Journal of Lower Genital Tract Disease 14, 230–233.
doi:10.1097/LGT.0b013e3181c945ed
ErmanVlahovic, M., Vlahovic, J., Mrcela, M., Hrgovic, Z.,
2017. Coexistence of Condylomata Acuminata with
Warty Squamous Cell Carcinoma and Squamous Cell
Carcinoma. Medical Archives 71, 72.
doi:10.5455/medarh.2017.71.72-75
Huang SM, Leung WH and Chen BF, 2007. Malignant
Transformation of Perianal Giant Condyloma
Acuminatum. J Soc Colon Rectal Surgeon (Taiwan)
18:23-30
Jonat W. and Arnold N, 2011. Is the Ki-67 labelling index
ready for clinical use? Annals of Oncology 22(3):500–
502.
Leblebici, C., Pasaoglu, E., Kelten, C., Darakci, S., Dursun,
N., 2017. Cytokeratin 17 and Ki-67:
Immunohistochemical markers for the differential
diagnosis of keratoacanthoma and squamous cell
carcinoma. Oncology Letters 13, 2539–2548.
doi:10.3892/ol.2017.5793
Li, L. T., Jiang, G., Chen, Q., Zheng, J. N, 2015. "Ki67 is a
promising molecular target in the diagnosis of cancer
(Review)". Molecular Medicine Reports 11:1566-1572.
Liu, G., Li, Q., Shang, X., Qi, Z., Han, C., Wang, Y., Xue,
F., 2016. Verrucous Carcinoma of the Vulva: A 20 Year
Retrospective Study and Literature Review. Journal of
Lower Genital Tract Disease 20, 114–118.
doi:10.1097/LGT.0000000000000164
Papapanagiotou, I.K., Migklis, K., Ioannidou, G., Xesfyngi,
D., Kalles, V., Mariolis-Sapsakos, T., Terzakis, E.,
2017. Giant condyloma acuminatum-malignant
transformation. Clinical Case Reports 5, 537–538.
doi:10.1002/ccr3.863
Scholzen, T., Gerdes, J., 2000. The Ki-67 protein: from the
known and the unknown. Scholzen T1, Gerdes J. J Cell
Physiol Mar, 311–322. doi:10.1002/(SICI)1097-
4652(200003)182:3<311::AID-JCP1>3.0.CO;2-9
Ki-67 Staining as a Tool to Differentiate Verrucous Carcinoma from Condyloma Acuminatum on Skin Biopsy
301
