
Skin Manifestations on Radiotherapy Patients in Dr. Moewardi
General Hospital Surakarta
Fiska Rosita, Bobby Febrianto, and Muhammad Eko Irawanto
Dermatovenereology Departement
Dr. Moewardi General Hospital/Faculty of Medicine Sebelas Maret University, Surakarta
Keywords: radiotherapy, acute radiation dermatitis, chronic radiation dermatitis
Abstract:
Radiotherapy is a common treatment modality for cancer and 50% of cancer patients receive radiotherapy as
a preoperative, postoperative and palliative therapy. Radiotherapy treatments cause various reactions to the
skin and cause pain, discomfort, irritation, itching, and burning sensations. Side effects that occur in the skin
due to radiation is classified into two, namely acute radiation dermatitis and chronic radiation dermatitis. This
study aimed to determine the skin manifestations which occur in radiotherapy patients in Dr. Moewardi
General Hospital Surakarta. A retrospective descriptive was conducted in Dr. Moewardi General Hospital
with the patient of radiotheraphy. The data were taken from medical record and direct observation. Thirty two
patients were included in this study, 20 female patients and 12 male patients, with the age ranged from 32 to
78 years old. Nasopharyngeal cancer is the most patients radiotherapy. Of all 32 radiotherapy patients only
1 (3.2%) patient received radiotherapy dose 2.5 Gy per fraction, and 24 (75%) patiens had 66 Gy for total
dose. According to the National Cancer Institute grade 1 acute radiation dermatitis occurred in our
radiotherapy patient was erythematous patch with partial hyperpigmentation 48.3%.
1 INTRODUCTION
Radiotherapy is a common treatment modality for
cancer and 50% of cancer patients receive
radiotherapy as preoperative, postoperative and
palliative therapy (Ali et al., 2014). Radiotherapy
treatments cause various reactions to the skin and
pain, discomfort, irritation, itching, and burning
sensations. Skin-induced changes in radiation can
result in disruption of daily activity and quality of life.
Skin reactions to radiation largely depend on the
technique, total dose, volume, and variety of therapy
in each individual (McQuestion, 2011). Side effects
that occur in the skin due to radiation is classified into
two namely acute radiation dermatitis and chronic
radiation dermatitis. Manifestations of acute radiation
dermatitis include erythema, edema, burning,
pruritus, pigmentation, desquamation, hair loss, loose
nails, bullae, erosion and ulceration. While the
manifestations of chronic radiation dermatitis consist
of excessive wrinkling, skin atrophy,
hyperpigmentation, permanent hair loss, dryness of
the skin and keratosis (Ali et al., 2014).
1.1 Acute Radiation Dermatitis
Acute radiation dermatitis is one of the most common
skin reactions caused by radiotherapy and often
occurs within 90 days of exposure (Bray et al.,
2016).The severity of skin reactions may occur from
mild erythema, desquamation to ulceration. Erythema
can be the first symptom that appears 24 hours after
exposure. Erythema can subside within a few days.
And generalized erythema can occur in the second
week until the fourth week of therapy. Other skin
changes such as dry skin, hair loss, and
hyperpigmentation can also be seen (Hegedus et al.,
2016). During the third week to the sixth week of
treatment, if the cumulative radiation dose reaches 20
Gy, dry desquamation may occur. A more severe
reaction of moist desquamation is seen when the total
radiation dose on the skin is 40 Gy or more. The
severity of the disease can be assessed on a scale of
1-4 according to the National Cancer Institute. First
degree is dry desquamation along with widespread
erythema.
Second degree appears rapid erythema or local
slough. This reaction causes a moist desquamation
confined to the skin fold after the cumulative
Rosita, F., Febrianto, B. and Irawanto, M.
Skin Manifestations on Radiotherapy Patients in Dr. Moewardi General Hospital Surakarta.
DOI: 10.5220/0008152601410145
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 141-145
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
141

radiation dose reaches 40 Gy or more. The presence
of moist desquamation increases the risk of infection.
Patients may experience increased pain due to
exposure to nerve (Bray et al., 2016). Third
degree
occurs dermatitis with confluent desquamation.
Fourth degree is characterized by ulceration, and
necrosis (Hymes et al., 2006).
The classification of acute radiation dermatitis:
Grade 0 - None
Grade 1 - Faint erythema or dry desquamation
Grade 2 - Moderate to brisk erythema or patchy moist
desquamation, mostly confined to skin fold and
creases; moderate erythema
Grade 3 - Moist desquamation other than skin folds;
pitting edema, bleeding from minor trauma and
abrasion
Grade 4 - Skin necrosis or ulceration of full-thickness
epidermis; may have spontaneous bleeding from
affected area.
1.2 Chronic Radiation Dermatitis
The skin will look relatively normal for different
durations of time after radiotherapy and chronic
changes will not develop for months or years after
receiving radiotherapy (Bray et al., 2016). Severe
chronic skin reactions develop more than 90 days
after radiotherapy is complete. These skin reactions
include epidermal depletion, dermal atrophy,
vascular damage, fibrosis that develops as a
progressive induration with edema formation, and
thickening of the dermis. Other effects which will
occur later are depigmentation, telangiectasis, and
dermal necrosis with ulceration occurring after
radiotherapy (Hegedus et al., 2016). Chronic
radiation dermatitis is a true late-stage reaction that
develops months to years after exposure to
radiotherapy (Bray et al., 2016).
To determine the degree of skin reaction due to
exposure to radiotherapy requires thorough history
about the length of radiotherapy recieved, the first
appearance of skin reaction and then perform physical
examination. The results are then compared with the
National Cancer Institute classification for acute
radiation dermatitis. Therefore we conducted this
study to determine the skin manifestation in patient
undergoing radiotherapy in Dr. Moewardi General
Hospital Surakarta.
2 METHODS
This retrospective descriptive study was conducted in
the Radiotherapy Division of Dr. Moewardi General
Hospital Surakarta. All of the data were taken from
skin examination and from medical record data. Data
collected were sex, age, type of cancer, common
exposed areas, and dermatological status.
3 RESULTS
Our study obtained 32 subjects, 20 females and 12
males. Most patients receiving radiotherapy started at
the age of 46, this ranged from 46 to 65. Head and
neck (62.5%) were the most common exposed sites,
followed by mamae area (25%). The most cancer type
in our study is nasopharyngeal cancer (40.6%).
Erythematous patches with partial hyperpigmentation
(48.3%) was the most common skin manifestation,
while erythematous patches was less common
(28.1%). Based on national cancer institute all of skin
manifestation was grade 1 acute radiation dermatitis.
Of all 32 radiotherapy patients only 1 (3.2%) patient
received radiotherapy dose 2.5 Gy per fraction. The
most widely accepted total dose of radiotherapy
patients in Dr. Moewardi General Hospital was 66
Gy (Table 1)(Fig.1).
4 DISCUSSION
Intrinsic factors such as general skin condition,
nutritional status, age, comorbid disease (diabetes
mellitus and connective tissue disorders) and
ethnicity all modulate the risk of acute skin reaction (
Hegedus et al., 2016). Skin manifestation can affect
both sexes though in our study they mostly affected
female. According study by Mateusz Spalek in 2016
stated that female sex is still suspected as an
independent predictor of severe skin reactions
(Spalek, 2016). Skin reactions due to radiotherapy
based on the age are related to skin healing ability, as
they decrease with age. It is caused by aging, loss of
collagen, and decreased capillary tissue. Based on
radiotherapy exposure location, the head and neck
area was found to be the largest area affected 62.5%
so that it may cause increased skin reactions more
frequently due to the area having thin epidermal
layers on that area (Ali et al., 2014).
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
142

Table 1. The data of patiens receiving radiotherapy and their skin manifestation
Total
(n=32)
Percentage
(%)
Gender
Male
Female
12
20
37.5
62.5
Age (year)
26-35
36-45
46-55
56-65
>65
2
7
8
8
7
6.3
21.9
25.0
25.0
21.9
Expose area
Head and Neck
Breast
Abdomen
20
8
4
62.5
28.1
9.4
Type of cancer
Breast cancer
Nasopharyngeal cancer
Larynx cancer
Lung cancer
Ear cancer
Palatum cancer
Hypopharynx cancer
Cervix cancer
8
13
3
2
1
1
1
3
25.0
40.6
9.4
6.3
3.1
3.1
3.1
9.4
Skin manisfestation
Patch erythematous
Patch erythematous with partial
hyperpigmentation
Patch hyperpigmentation with crust
No skin manifestation
9
14
2
7
28.1
48.3
6.3
21.9
Degree of acute radiation dermatitis
First degree
Second degree
Third degree
Fourth degree
32
0
0
0
100
0
0
0
Fractional dose
2 Gy
2,5 Gy
31
1
96.8
3.2
Total dose of radiation
40 Gy
50 Gy
60 Gy
66 Gy
3
1
4
24
9.4
3.1
12.5
75.0
Study from Ahmad Ameri and Mona Malekzadeh,
2017 reported that radiation dermatitis is commonly
seen in patients with breast cancer, head and neck
cancer, lung cancer and sarcoma due to the superficial
position of these cancer and higher radiation dose
affect the skin (Ameri & Malekzadeh, 2017).
According to the National Cancer Institute grade
1 acute radiation dermatitis occurred in our
radiotherapy patients was erythematous patch with
partial hyperpigmentation. The severity of the skin
manifestation is related to both intrinsic and extrinsic
factors. Extrinsic factors include the total dosage of
radiation, fractioned delivery schedules, volume of
irradiated tissue and the radiosensitivity of the
involved tissue (Bray et al., 2016).
Skin Manifestations on Radiotherapy Patients in Dr. Moewardi General Hospital Surakarta
143
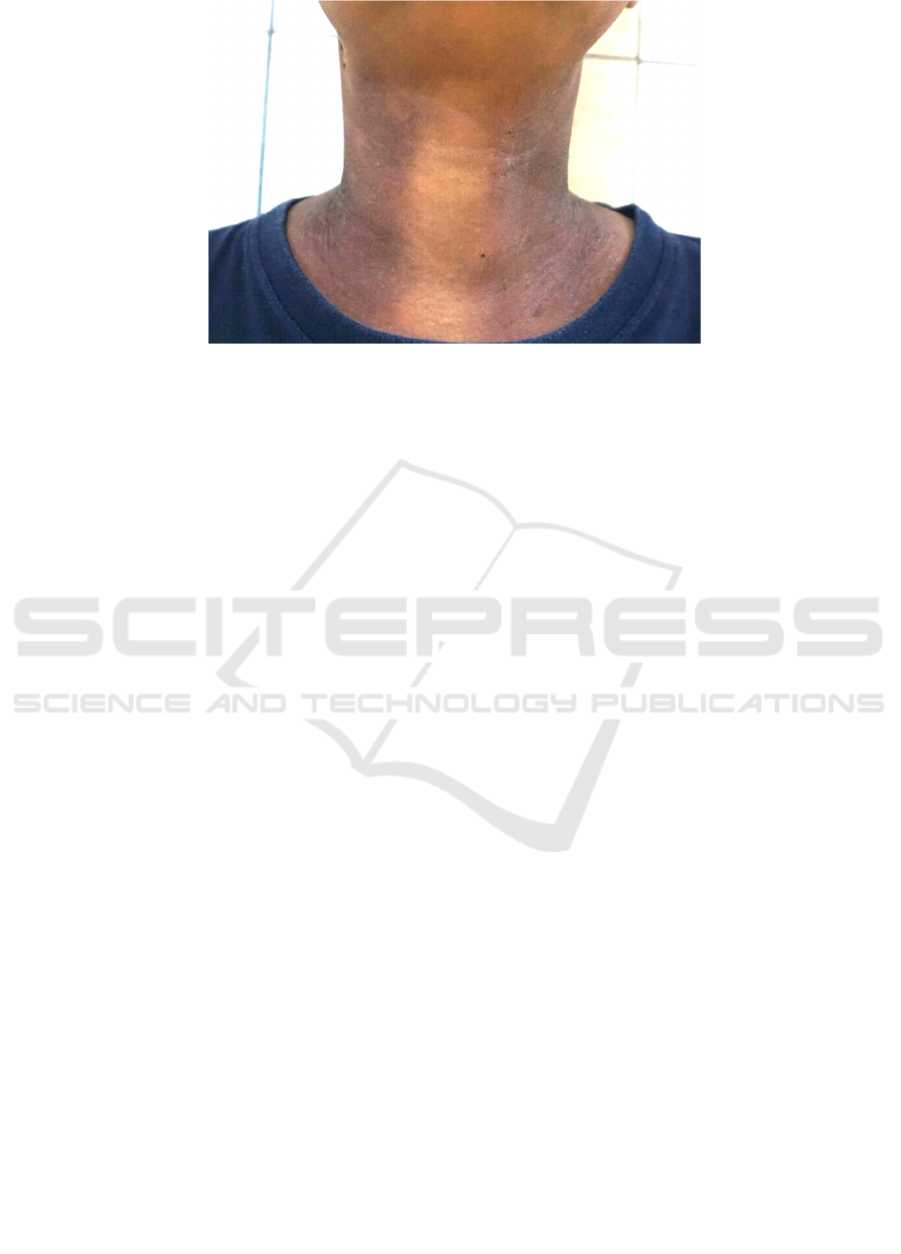
Figure. 1: First degree of acute radiation dermatitis
Among patients received radiotherapy in Dr. Moe-
wardi General Hospital, only 1 (3.2%) patient had
radiotherapy dose of 2,5 Gy per fraction and 24 (75%)
patients with total dose of 66 Gy. Radiation doses of
more than 2 Gy per fraction are linked with the
development of more severe delayed skin reactions
(Hegedus et al., 2016). The level of damage received
equates directly to the amount of radiation exposure
(Maddocks-Jennings,. et al., 2005). Based on the
Fanni Hegedus study, Laju M, Matthew, and Robert
Schwartz stated that a total of 40 Gy or more dose can
cause severe skin manifestations such as moist
desquamation. This is also supported by studies
conducted by Fleta N. Bray, Brian J. Simmons, Aaron
H. Wolfson, and Keyvan Nouri who also support it.
This is evidenced in a study by Rodrigo Mosca et al
in 2013 how the effect of total dose and dose
fractional affects the appearance of skin
manifestations in mice, whereas at 2 Gy fractional
dosage has caused transient erythematous. However,
in that study it was found that lower doses ranged
from 1 - 43.5 Gy, 2 - 58 Gy, 3 - 72.5 Gy did not result
in severe dermatitis reaction (Mosca et al., 2013). In
acute radiation dermatitis does not require immediate
treatment. The healing occurs about 28-40 days after
the peeling and can recover within 3-6 months after
exposure (Jaschke et al., 2017).
5 CONCLUSIONS
Based on our finding, it is necessary to have a
thorough examination when we have cancer patient
so that we can give better management for the skin
problem.
REFERENCES
Ali, S., Reddy, M., & Hussain, S., 2014. Cutaneous effect
of radiotherapy- a review article. Innovative Journal of
Medical and Science, 4, pp. 341-9.
Ameri, A., & Malekzadeh, M., 2017. Radiation dermatitis
[Internet]. September 8 [Cited 2018 Jan 13]. Available
from: https://oncohemakey.com/radiation-dermatitis/
Bray, F. N., Simmons, B. J., Wolfson, A. H., & Nouri, K.,
2016. Acute and chronic cutaneous reactions to
ionizing radiation therapy. Dermatology and
therapy, 6(2), pp. 185-206.
Hegedus, F., Mathew, L. M., & Schwartz, R. A., 2016.
Radiation dermatitis: an overview. International
journal of dermatology, 56(9), pp. 1-5.
Hughes, A., Mitchel, A., Bianchini, J., Goodwin, F.,
Guidote, N., & Gunderson, R., 2013. Symptoms and
management guidelines: Radiation dermatitis. BC
Cancer Agency, pp. 1-11.
Hymes, S. R., Strom, E. A., & Fife, C., 2006. Radiation
dermatitis: clinical presentation, pathophysiology, and
treatment 2006. Journal of the American Academy of
Dermatology, 54(1), pp. 28-46.
Jaschke, W., Schmuth, M., Trianni, A., & Bartal, G., 2017.
Radiation-induced skin injuries to patients: what the
interventional radiologist needs to
know. Cardiovascular and interventional
radiology, 40(8), pp. 1131-1140.
Maddocks-Jennings, W., Wilkinson, J. M., & Shillington,
D., 2005. Novel approaches to radiotherapy-induced
skin reactions: a literature review. Complementary
therapies in clinical practice, 11(4), pp. 224-231.
McQuestion, M., 2011. Evidence-based skin care
management in radiation therapy: clinical update.
In Seminars in oncology nursing, 27(2), pp. e1-e17),
WB Saunders.
Mosca, R. C., Ferreira, D. C., Napolitano, C. M., Santin, S.
P., Dornelles, L. D. P., Alvarenga, E. O., & Mathor, M.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
144

B., 2013. An athymic mouse model to mimic cobalt-60
cutaneous radiation injury. International Nuclear
Atlantic Conference. Brazil: INAC.
Sharp, L., 2016. Radiotheraphy-related skin reaction
[Internet]. June 21 [Cited 2018 Jan 5]. Available from:
http://cancerworld.net/e-grandround/radiotherapy-
related-skin-reactions/
Spałek, M., 2016. Chronic radiation-induced dermatitis:
challenges and solutions. Clinical, cosmetic and
investigational dermatology, 9, pp. 473-482.
Skin Manifestations on Radiotherapy Patients in Dr. Moewardi General Hospital Surakarta
145
