
Nail Changes in Children Undergoing Chemotherapy
Ardelia Dyah Ayu
1,*
, Reti Anggraeni
1
, Endra Yustin Ellista Sari
1
, Muh. Riza
2
, and Suci Widhiati
1
1
Dermatovenereology Departement, Dr. Moewardi General Hospital/Faculty of Medicine Sebelas Maret University,
Surakarta
2
Pediatric Department, Dr. Moewardi General Hospital/ Faculty of Medicine Sebelas Maret University, Surakarta
Keywords: nail changes, nail disorder, children, chemotherapy
Abstract: Many chemotherapeutic agents used in the management of various malignancies. Nail changes are often under
recognized or attributed to other causes. The anticancer chemotherapeutic agents were known to cause a
damage to the nail. This analytical, cross-sectional study was conducted in Dr. Moewardi General Hospital
Surakarta between December 2017 and January 2018. The subjects were taken by consecutive sampling,
consisting of 30 children undergoing chemotherapy and 30 healthy children as a control. History taking and
physical examination in the form of digital photography as well as dermoscopic examination were conducted
in all subjects. The data obtained were then analyzed using Mann-Whitney test, p < 0.05 was considered
significant statistically. Nail changes were observed in 25/30 ( 83.3%) of the children receiving chemotherapy
and they have a statistical significant difference compared to control group, with the p value 0.000. The nail
changes obtained were trachonychia (22,2%), dyscromia (18.5%), melanonychia (14.8%), and Beau’s lines
(14.8%). Combination of methotrexate and vincristine was the most frequent chemotherapeutic agent used in
the subjects (40%). This study is expected to provide knowledge for dermatologist so that it can improve the
promotive health, preventive, curative and education for the patient.
1 INTRODUCTION
The anticancer chemotherapeutic agents were known
to cause various mucocutaneous side effects,
including nail changes. Nail changes are often under-
recognized or attributed to many causes.
Chemotherapy-induced nail changes, though they not
life threatening, are cosmetically distracting and can
be a source of significant distress to patients.
The anti- cancer chemotherapeutic agents may
cause a damage to the nail matrix or the nail bed and
a variety of changes involving the nail plate, nail bed,
hyponychium or the nail folds may be seen (Chen et
al., 2007). Several chemotherapy agents and their
combinations have been reported to induce nail
changes, including taxoids, cyclophosphamide,
doxorubicin/ daunorubicin, 5-fluorouracil and
vincristine. Cyclophosphamide and doxorubicin are
two agents commonly reported to affect the nails
(Hinds & Thomas, 2008).
The nail changes mostly are the result of acute
toxicity to the nail epithelium. Various symptoms will
occur depend on which nail structure is affected and
the severity of the insult (Piraccini et al., 2003).
Pigmentation changes due to chemotherapeutic
agents involving the nail plate are seen secondary to
the damage of the nail matrix melanocytes. The
damage to the nail bed may be as a consequence of
direct damage due to drugs or an indirect damage to
the underlying blood vessels (Reddy et al., 2017).
Nail growth in children is faster than is in adult,
and it is estimated to be at a rate of 0.12 mm / day
(Chen et al., 2007; Balgord & Pardee, 2008; Robert et
al., 2015). However, nail changes in children
undergoing chemotherapy, in comparison to adult
cases, are less well characterized in the literature.
This study was designed to understand and to find out
the pattern of nail changes in children receiving
various chemotherapies.
2 METHODS
An analytical, cross-sectional study conducted in Dr.
Moewardi General Hospital Surakarta between
December 2017 and January 2018. The subjects were
taken by consecutive sampling, consisting of 30
children undergoing chemotherapy and 30 healthy
children as a control.
History taking and physical examination in the
form of digital photography as well as dermoscopic
118
Ayu, A., Anggraeni, R., Sari, E., Riza, M. and Widhiati, S.
Nail Changes in Children Undergoing Chemotherapy.
DOI: 10.5220/0008152101180121
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 118-121
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
examination were conducted in all subjects. We
excluded children with nail abnormalities which
occur prior to chemotherapy. Potassium hydroxite
(KOH) test was performed if there was a suspicion of
onychomycosis and or its coincidence in the subjects.
The data obtained were then analyzed using Mann-
Whitney test, p < 0.05 was considered significant
statistically.
3 RESULTS
Table 1. Clinical features of the enrolled subjects
Total
(chemotherapy
group, n = 30)
(control group, n
= 30)
Percentage
(%)
Age (year)
0 – 5
6 – 11
12 - 16
15
41
4
25
68.3
6.7
Gender
Male
Female
28
32
46.7
53.3
Nail changes in
chemotherapy
group
Yes
No
25
5
83.3
16.7
Nail changes in
control group
Yes
No
3
27
10
90
The data obtained were than analyzed using
Mann-Whitney test. It is showed that there was a
statistically significant difference in nail changes
between children undergoing chemotherapy and
healthy control group, with the p value 0.016. The age
of most subject is between 6 – 11 years old. The
number of men and women in this study was
proportional.
4 DISCUSSION
Nail dermoscopy (onychoscopy) has initially been
used for the assessment of nail pigmentation, but its
exertion has expanded for the diagnosis of all nail
disorders and it becomes a routine diagnostic
instrument, as it reveals helpful information.
Dermoscopy can be applied to all visible parts of the
nail unit, and even the nail matrix can be studied.
Many nail signs can be magnified by dermoscopy and
combined with clinical examination to establish the
diagnosis (Piraccini et al., 2012). In this study we
used dermoscopy examination to asses the diagnosis
of the nail changes, combining with history taking
and other physical examination.
Numerous mucocutaneous effects result from
inflammatory disorder, systemic drugs, trauma, viral
infection, macronutrient and micronutrients
deficiency, and even product used on the nails
(Kristien, 2015). Three out of 30 children in control
group had nail changes, in the forms of Beau’s lines
and leukonychia. These may occur due to nutritional
deficiency in children, espesially micronutrient
deficiency.
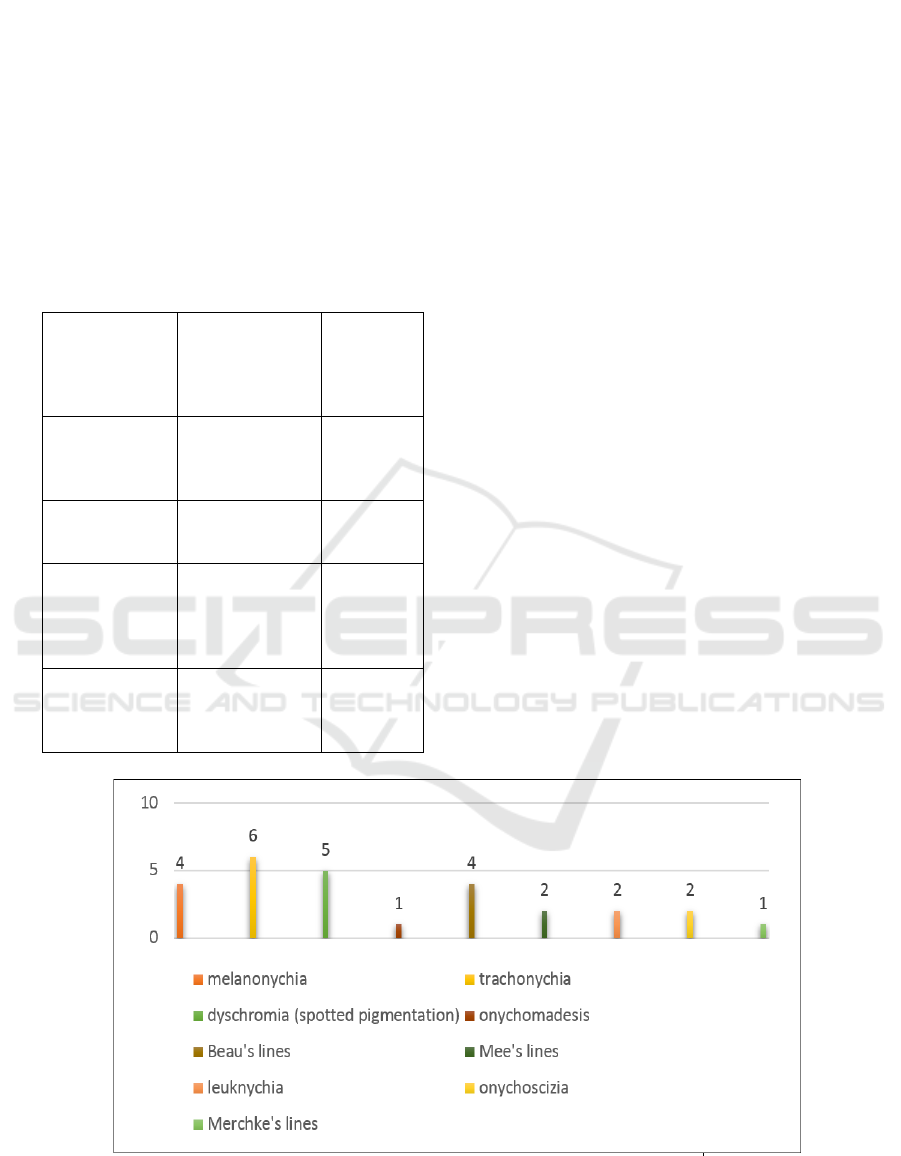
Figure 1. Pattern of nail changes in chemotherapy group
Nail Changes in Children Undergoing Chemotherapy
119

Figure 2. A. Trachonychia, change in nail plate. B. Melanonychia, change in nail pigmentation.
Table 3. The frequency of nail changes based on chemotherapy agents.
Agents of Chemotherapy Frequency Percentage (%)
Methotrexate + vincristine
Etoposide+ carboplatin
Doxorubicin + vincristine + cyclophosphamide
Cyclophosphamide
Cyclophosphamide + metilprednisolone
Vincristine
Cisplatin + bleomycine + vincristine
10
8
1
3
1
1
1
40
32
4
12
4
4
4
Nail changes were observed in 25/30 ( 83.3%) of
the children receiving chemotherapy and have a
statistically significance difference to control group.
MEDLINE and EMBASE (1966–2008) databases
reported that nail changes were caused by nail toxicity
which is the adverse effect linked to a number of
chemotherapeutic agents. The continuously dividing
nail matrix cells are easily perturbed by antimitotic
activity so that chemotherapy agents become easier to
affect the nails (Gilbar et al., 2009). Nail changes are
usually temporary and resolve with the cessation of
this therapy , but some may persist (Gupta et al.,
2008).
Chemotherapy-induced nail changes can classified
into nail color changes, changes in the surface of the
nail plate, disruption between the nail plate and the
underlying nail bed, and damage to soft tissue
structures surrounding the nail (Ranawaka, 2009). In
this study, nail color changes occur in 40.7% subjects
and the rest are nail plate changes. The three most
common nail changes found in our study were
trachonychia, dyscromia, and melanonychia.
Trachyonychia is defined as roughness of the nails.
Trachyonychia has been grouped into 2 types: shiny
trachyonychia and opaque trachyonychia, as seen in
Figure 2.A; this likely represent the spectrum of
disease severity. The clinical features of
trachyonychia include a sandpaperlike appearance of
the nails, longitudinal ridging, brittleness, and nail
pitting (Chu & Rubin, 2014).
Rough and brittle nails are caused by decrease in
the nail growth rate, which is common in
chemotherapy course. Trachonycia also have been
suggested to be caused by underlying poor metabolic
or nutritional health of patients with advanced cancers,
but this suggestion has not been formally proven
(Robert et al., 2015).
Nail hyperpigmentation can be brown or black
(melanonychia) or other colours. It commonly
presents as a longitudinal streak (longitudinal
melanonychia) as seen in Figure 2.B, but can also
present as a transverse band (transverse
melanonychia), spotted pigmentation or involve the
entire nail plate (total melanonychia) (Chu & Rubin,
2014). The exact mechanism of chemotherapy-
induced hyperpigmentation is not clearly understood.
But it is postulated that the accumulation of the drug
in the nails can have a direct toxic effect on the
melanocyte causing increased melanin production, or
there may be an associated increase in the
adrenocorticotropic hormone or the melanocyte
stimulating hormone.
13
Praveen Kumar et all in their
study stated that the statistically significant changes
observed were nail matrix melanocyte changes
including longitudinal pigmentary bands as the most
common change in 67.7% of cases, following
administration of chemotherapy agents with an
average onset of 6 weeks from the start of the course
(Reddy et al., 2017).
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
120

Beau’s lines are transverse linear depressions in
the dorsum nail plate that emerge from beneath the
proximal nail fold, and are due to a transitory decrease
in mitotic activity of the nail matrix keratinocytes.
Drug- induced Beau’s lines are usually dose related
and reproducible with readministration of the drug
(Piraccini et al., 2003).
Most of the children (80%) in our chemotherapy
group have undergone 0-6 month course duration.
Drug-induced nail changes could develop within 3-4
weeks after the initiation of chemotherapy and
sometimes they does not need specific treatment,
because they show only past damage to the matrix and
the changes generally resolve as the nails grow out
(Robert et al., 2015). This also explains why in some
subjects who have undergone a long course of
chemotherapy may not develop any nail changes.
In our study methothrexate and vincristine were
the most common combinations of chemotherapeutic
agents used on the subjects (40%) and also the most
frequent agents caused the nail abnormality. Loose
toenails, thickened and discolorization, as well as
onycholysis and nail shedding will occur correspond
to chemotherapeutic cycles of methotrexate. In the
other hand, vincristine has been reported to produce
leukonychia, Beau’s lines, Mees’ lines, and
onychodermal bands (Gilbar et al., 2009).
The evaluation of nail changes in children
undergoing chemotherapy was hampered by some
confounding factors, such as a combination of
multiple agents in most regimens made it difficult to
determine the main culprit drug, opportunistic
infection during chemotherapy, and symptoms often
resolve with or without drug withdrawal.
5 CONCLUSION
This study was conducted in Dr. Moewardi General
Hospital Surakarta between December 2017 and
January 2018. The statistical analysis revealed that
there was a significant difference in nail changes
between children undergoing chemotherapy and
healthy control group, with the p value < 0.05. The
most common nail changes was trachonychia. The
combination of methotrexate and vincristine was the
most frequent chemotherapeutic agent used in the
subjects. The relationship between exposure time of
chemotherapy agents or its combination with the
onset of nail changes cannot be determined yet due to
limited observation of time time research. Research
with a larger number of subjects and longer
observation time is needed to obtain more
representative results and causative relationships
between each parameters.
REFERENCES
Balgord, S., & Pardee, T., 2008. Chemotherapy-Induced
Fingernail Changes. Indian J Dermatol [Internet],
53(4):204–205.Available from:
http://www.ncbi.nlm.nih.gov/pubmed/24795111.
Chen, W., Yu, Y. S., Liu, Y. H., Sheen, J. M., & Hsiao, C.
C., 2007. Nail changes associated with chemotherapy in
children. Journal of the European Academy of
Dermatology and Venereology, 21(2), pp. 186-190.
Chu, D. H., & Rubin, A. I., 2014. Diagnosis and
management of nail disorders in children. Pediatric
Clinics, 61(2), pp. 293-308, Available from:
http://linkinghub.elsevier.com/retrieve/pii/S003139551
3002083.
Gilbar, P., Hain, A., & Peereboom, V. M., 2009. Nail
toxicity induced by cancer chemotherapy. Journal of
Oncology Pharmacy Practice, 15(3), pp. 143-155.
Gupta, A., Parakh, A., & Dubey, A. P., 2008. Chemotherapy
induced nail changes. Indian journal of
dermatology, 53(4),pp. 204.
Hinds, G., & Thomas, V. D., 2008. Malignancy and cancer
treatment-related hair and nail changes. Dermatologic
clinics, 26(1), pp. 59-68.
Issaivanan, M., & Khairkar, P. H., 2003. Doxorubicin
induced melanonychia. Indian pediatrics, 40(11), pp.
1094-1096.
Kristien Hoffman., 2015. When vitamin and nutritional
deficiencies cause skin and nail changes. Podiatry
Today. [cited 29 January 2018]. Available from:
https://www.podiatrytoday.com/when-vitamin-and-
nutritional-deficiencies-cause-skin-and-nail-changes
Piraccini, B. M., Bruni, F., & Starace, M., 2012.
Dermoscopy of non‐skin cancer nail
disorders. Dermatologic therapy, 25(6), pp. 594-602.
Piraccini, B. M., Iorizzo, M., & Tosti, A., 2003. Drug-
induced nail abnormalities. American journal of clinical
dermatology, 4(1), pp. 31-37.
Ranawaka, R. R., 2009. Patterns of chromonychia during
chemotherapy in patients with skin type V and outcome
after 1 year of follow‐up. Clinical and Experimental
Dermatology: Clinical dermatology, 34(8), e920-e926.
Reddy, P. K. S., Prasad, A. L. S., Sumathy, T. K., & Reddy,
R. V., 2017. Nail changes in patients undergoing cancer
chemotherapy. International Journal of Research in
Dermatology, 3(1), pp. 49-54, Available from:
http://www.ijord.com/index.php/ijord/article/view/96.
Robert, C., Sibaud, V., Mateus, C., Verschoore, M., Charles,
C., Lanoy, E., & Baran, R., 2015. Nail toxicities induced
by systemic anticancer treatments. The Lancet
Oncology, 16(4), e181-e189, Available from:
http://dx.doi.org/10.1016/S1470-2045(14)71133-7.
Nail Changes in Children Undergoing Chemotherapy
121
