
Correlation between Psoriasis Severity and Periodontal Pocket Depth
in Psoriasis Vulgaris
Sofa Inayatullah
1*
, Anita H. Joedo
2
,
Githa Rahmayunita
1
, and Evita Halim Effendi
1
Department of Dermatology and Venereology Faculty of Medicine Universitas Indonesia / Dr. Cipto Mangunkusumo
National General Hospital, Jakarta
2
Department of Dental and Oral Medicine, Dr. Cipto Mangunkusumo National General Hospital, Jakarta
Keywords: Infection, periodontitis, psoriasis
Abstract: Psoriasis is a chronic inflammatory skin disease, characterized by erythematous plaques and scales,
with Koebner phenomenon and Auspitz sign. One of the trigger factors that contributes is infection.
Periodontitis is an infection that occurs in periodontal tissue and can be one of the infection focus. This
research aimed to determine the proportion of periodontitis in patients with psoriasis vulgaris and the
correlation between psoriasis severity and periodontal pocket depth. This cross-sectional study was
conducted in July-November 2017 in Dermatovenereology clinic of dr. Cipto Mangunkusumo National
General Hospital, Jakarta. Anamnesis and physical examination of skin lesions were done by
investigator, dental and oral examination were done by periodontist. Total of 34 subjects were
examined with median age of 37.5 years (range 19-58 years old). The subjects consisted of 20 patients
(58.8%) with mild psoriasis and 14 patients (41.2%) with moderate-severe psoriasis. The result showed
16 patients (47.1%) with periodontitis and 18 patients (52.9%) without periodontitis. Periodontitis was
obtained in 8 patients (23.53%) in each group of mild and moderate-severe psoriasis. There was no
statistically significant correlation between psoriasis severity and periodontal pocket depth (r = 0.126, p
= 0.478). The results might be due to counfounding factors that affect both psoriasis severity and
pocket depth.
1 INTRODUCTION
Psoriasis is a chronic inflammatory skin disease,
characterized by erythematous plaque and scales,
with Koebner phenomenon and Auspitz sign
(Gudjonson et al., 2012).
Trigger factors for
psoriasis are infection, drugs, trauma, stress, obesity,
smoking, and alcohol consumption (Sharma et al.,
2015; Ungprasert et al., 2016).
Recurrence and
persistence of psoriatic lesions may occur and
disrupt patients quality of life. One of the trigger
factors that contributes is infection (Sharma et al.,
2015).
The focus of infection sources are varied,
including oral, ear, and throat infections (Ungprasert
et al., 2016; Brezewski et al., 2013). Management of
infection is one of the keys for achieving skin
remission (Brezewski et al., 2013).
Oral infection in psoriasis patient is common and
may act as a source of focal infection. The
prevalence of periodontal disease in psoriasis
patients in some studies ranged from 24-27%
(Rysstad et al.,2014; Lazaridou et al., 2013).
Periodontitis is a chronic infection and inflammatory
disease of periodontal tissue characterized by gum
bleeding, periodontal pocket formation, periodontal
tissue destruction, and alveolar bone destruction
(Sharma et al., 2015). The periodontal pockets are
assessed by measuring the pocket depth, the distance
measured from gingival edge to pocket base in
millimetres (Page & Eke, 2007).
Both of psoriasis and periodontitis have immune
responses toward microbiota on epithelial surface. It
is suspected that damage or disturbance in
periodontal tissue may associate with psoriasis
exacerbation. On the other side, remission of
psoriasis may correlate with remission of
periodontal tissue destruction (Sharma et al., 2015).
Pocket depth correlate with periodontitis severity
(Page & Eke, 2007). We suspected that psoriasis
severity might be correlated with pocket depth.
Several studies aimed to know the difference
between periodontitis and periodontal status in
78
Inayatullah, S., Joedo, A., Rahmayunita, G. and Effendi, E.
Correlation between Psoriasis Severity and Periodontal Pocket Depth in Psoriasis Vulgaris.
DOI: 10.5220/0008151200780082
In Proceedings of the 23rd Regional Conference of Der matology (RCD 2018), pages 78-82
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

psoriasis patients compared with control group
(Sharma et al., 2015).
Periodontitis was found more
frequently in psoriasis patients than in control group
(Rysstad et al.,2014). Metaanalysis studies reported
that patients with periodontitis had a greater risk of
psoriasis (Ungprasert et al., 2016;Keller et al.,
2012).
Prevalence of psoriasis varies across countries
with range of 0.09-11.4% (Gujonson et al.,
2012;Anonym, 2016).
In developing countries, the
prevalence ranges from 1.5-5% (Anonym, 2016).
The 2013 Indonesian National Health Research
Report (known as RISKESDAS) reported the
population proportion with dental and mouth
problems were 25.9%. The proportion of
Indonesians with proper behavior in teeth brushing
was only 2.3%. Most Indonesian brushed their teeth
every day during morning and afternoon shower
(Anonym, 2013).
The high proportion of periodontitis in patients
with psoriasis vulgaris in earlier studies and low
proportion of Indonesian population with proper
behavior in brushing were become our consideration
to determine the proportion of periodontitis in
psoriasis vulgaris. The study was aimed to find the
proportion of periodontitis in patients with psoriasis
vulgaris and report the correlation between psoriasis
severity and periodontal pocket depth. In this study,
patients with smoking habit and alcohol
consumption were excluded
.
2 METHODS
The study was an analytic descriptive study with
cross sectional design. Total subjects were 34
psoriasis vulgaris patients in Dermatovenereology
clinic of dr. Cipto Mangunkusumo National General
Hospital according to inclusion and exclusion
criteria. General physical examination, vital signs,
skin lesions, and determination of psoriasis severity
using psoriasis area and severity index (PASI) scores
were performed by principal investigator. Patients
with PASI score less than 7 were classified as mild
psoriasis and patients with PASI score 7 or greater
were classified as moderate-severe psoriasis.
Patients were assessed by a periodontist to examine
pocket depth, clinical attachment level (CAL),
plaque index, calculus index, and papillary bleeding
index. Periodontitis were assessed based on pocket
depth and CAL. Periodontitis definition in this study
was based on case definition proposed by the
Centers for Disease Control and Prevention (CDC)
and the American Academy of Periodontology
(AAP). Moderate periodontitis was defined as
having ≥2 interproximal sites with CAL ≥4 mm (not
on same tooth), or ≥2 interproximal sites with pocket
depth ≥5 mm (not on same tooth). Severe
periodontitis was defined as having ≥2 interproximal
sites with CAL ≥6 mm (not on same tooth) and ≥1
interproximal site with pocket depth ≥5 mm
(Rysstad et al., 2014; Page & Eke, 2007). Subjects
with certain indications or clinical doubts will be
underwent panoramic radiography.
3 RESULTS
Total subjects were 34 patients during July-
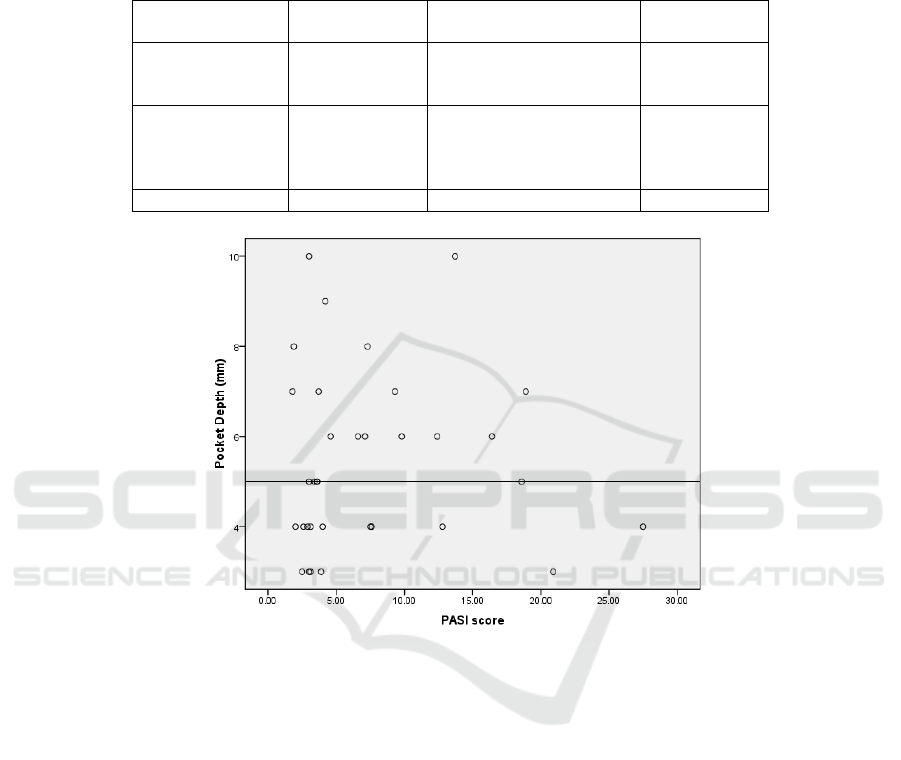
November 2017. The proportion of periodontitis can
be seen in table 1 and correlation between psoriasis
severity and periodontal pocket depth can be seen in
figure 1.
4 DISCUSSION
4.1 Proportion of Periodontitis in Psoriasis
Vulgaris Patients
Total of 34 subjects consist of 20 patients (58.8%)
with mild psoriasis and 14 patients (41.2%) with
moderate-severe psoriasis. Median of PASI scores
was 4.1 (range 1.8-27.5). Median of age was 37.5
years old with range 19-58 years old. Subjects
consist of 27 female (79.4%), and 7 male (20.6%).
The results showed that 16 patients (47.1%) with
periodontitis and 18 patients (52.9%) without
periodontitis. There were 8 patients (23,53%) with
mild psoriasis and 8 patients (23,53%) with
moderate-severe psoriasis diagnosed with
periodontitis.
The proportion of periodontitis in psoriasis
vulgaris patients in this study is higher than previous
studies conducted by Lazaridou et al. (2013), Fadel
et al.
(2013), and Rysstad et al. (2014). Lazaridou et
al. (2013) showed the proportion of periodontitis in
psoriasis patients were 27%, which is 46% of the
patients were active smokers. In our study, smokers
were excluded. There was no age restriction in
Lazaridou’s study, while in our study the age was
limited at 18-59 years old. Fadel et al. (2013)
showed the proportion of periodontitis in psoriasis
vulgaris patients were 24%. The results showed that
patients with psoriasis have lower pH of saliva,
fewer teeth number, and lower level of alveolar bone
compared to control group (p <0.05). Rysstad et al.
Correlation between Psoriasis Severity and Periodontal Pocket Depth in Psoriasis Vulgaris
79
(2014) showed the proportion of moderate-severe
periodontitis in psoriasis patients were 24%, while
68% of subjects were in immunosuppressant
therapy. Patients with systemic therapy and smoking
habit still be included in Rysstad’s study, while in
our study those patients were excluded.
Table 1. Proportion of periodontitis in subjects (n = 34)
Periodontitis
n (%)
Without periodontitis
n (%)
Total
n (%)
Mild psoriasis
8 (23.5)
12 (35.3)
20 (58.8)
Moderate-severe
psoriasis
8 (23.5)
6 (17.6)
14 (41.2)
Total n (%) 16 (47.1) 18 (52.9) 34 (100)
Figure 1. Correlation between PASI score and periodontal pocket depth (n = 34)
The reports of 2013 RISKESDAS showed that
proportion of Indonesian population with dental and
mouth problems were 25.9%. Proper behavior in
teeth brushing is the habit of brushing every day
after breakfast and before bedtime. Almost all
population with age ≥10 years brushed their teeth
every day (93.8%), Jakarta was the highest
proportion (98.1%) and Papua was the lowest
(49.6%). Most of them actually brushed their teeth
during morning and afternoon shower. Improper
behavior of teeth brushing were found in almost all
age groups, while the proper behavior were only
2.3% (Anonym, 2013). These might be the cause of
high proportion of periodontitis in this study
compared with other researches
.
4.2 Correlation between Psoriasis Severity
and Periodontal Pocket Depth
This study showed no significant and very weak
correlation (r = 0.126; p = 0.478) between PASI
score and pocket depth (figure 1). This results
showed that increase in pocket depth were not
followed by an increase in PASI score. Although
this study found that there were no correlation
between psoriasis severity and periodontal pocket
depth, but there was positive correlation between
them. We assumed that pocket depth was not
enough to affect psoriasis severity. This result may
be caused by confounding factors that affect both
pocket depth and psoriasis severity.
There were many factors that can affect both
PASI score and pocket depth. The characteristics of
subjects were heterogeneous, with wide age range
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
80

(18-59 years old). Emotional stress and diabetes
mellitus may also be the cause of the absence of
significant correlation.
Wide age range (18-59 years old) could be a
counfounding factor for correlation between
psoriasis severity and periodontal pocket depth in
this study. Brown et al.
(1990) reported 5.7%
subjects with 4-6mm pocket depth in the age group
of 18-24 years old. This proportion was increased
three fold (18.1%) in the age group of 55-64 years
old.
This study did not evaluate stress factors.
Lakshmy et al. (2015) reported psychiatry morbidity
in psoriasis vulgaris and the correlation with
psoriasis severity. The results showed that 71
patients (78.9%) have depression and 69 patients
(76.7%) have anxiety disorders. There was positive
correlation between psoriasis severity and
psychological variables (depression, anxiety, and
stress). Psoriasis severity correlated significantly
with depression (r = 0.465, p = 0.000), anxiety (r =
0.515, p = 0.000), and stress (r = 0.544, p = 0.000).
Rosania et al.
14
(2009) reported there were positive
correlation between the score of stress and pocket
depth (r = 0.23, p = 0.06) and also with number of
missing teeth (r = 0.54, p <0.001).
Diabetes mellitus is a frequent comorbid in
psoriasis and periodontitis patients (Anonym, 2016;
Holmstrup et al., 2017).
There were 5 patients
(14.7%) with history of diabetes mellitus. Diabetes
mellitus could act as a counfounding factor between
psoriasis severity and periodontal pocket depth in
this study.
5 CONCLUSION
The high proportion of periodontitis was found in
psoriasis vulgaris patients and there was no
statistically significant correlation between psoriasis
severity and periodontal pocket depth. In the
management of psoriasis vulgaris, all trigger factors
should be eliminated so that psoriatic lesions do not
get worse and recurrent. Although this study found
that there was no correlation between psoriasis
severity and periodontal pocket depth, but the high
proportion of periodontitis in psoriasis vulgaris
patients should increase the physician awareness to
identify and treat the focus of infection properly.
ACKNOWLEDGEMENT
The author thanks to the patients for their
participation in this study. And also special thanks to
dr. Windy Keumala Budianti, SpKK, dr. Endi
Novianto, SpKK, drg. Cut Intan Safitri, Sp.Perio,
and drg. Siti Marhamah, Sp.Perio for their help in
data collection. The author also thanks to dr. Rompu
Roger Aruan, SpKK from Koja District Hospital
who had participated in referring his patients for this
study.
REFERENCES
Anonym, 2016. Global report on psoriasis. World Health
Organization.
Anonym, 2013. Riset Kesehatan Dasar 2013. Badan
penelitian dan pengembangan kesehatan Kementerian
Kesehatan RI.
Brezewski, PL., Spalkowska, M., Podblelska, M.,
Chmlelewska, J., Wolek, M., Malec, K., Malec, K., &
Wojas-Pelc, A., 2013. The role of focal infections in
the pathogenesis of psoriasis and chronic
urticaria. Advances in Dermatology and
Allergology/Postȩpy Dermatologii I
Alergologii, 30(2), 77.
Brown, L. J., Oliver, R. C., & Loe, H., 1990. Evaluating
periodontal status of US employed adults. Journal of
the American Dental Association (1939), 121(2),
pp.226-232.
Fadel, H. T., Flytström, I., Calander, A. M., Bergbrant, I.
M., Heijl, L., & Birkhed, D, 2013. Profiles of dental
caries and periodontal disease in individuals with or
without psoriasis. Journal of periodontology, 84(4),
pp. 477-485.
Gudjonson, JE., Elder, JT, 2012. Psoriasis.
In: Goldsmith
LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ,
Wolff K, editors. Fitzpatrick’s dermatology in general
medicine. 8th Edition. New York: McGraw-Hill;
p.169-93.
Holmstrup, P., Damgaard, C., Olsen, I., Klinge, B.,
Flyvbjerg, A., Nielsen, C.H. and Hansen, P.R., 2017.
Comorbidity of periodontal disease: two sides of the
same coin? An introduction for the clinician. Journal
of oral microbiology, 9(1), p.1332710.
Keller, J. J., & Lin, H. C. 2012. The effects of chronic
periodontitis and its treatment on the subsequent risk
of psoriasis. British Journal of Dermatology, 167(6),
pp.1338-1344.
Lakshmy, S., Balasundaram, S., Sarkar, S., Audhya, M., &
Subramaniam, E., 2015. A cross-sectional study of
prevalence and implications of depression and anxiety
in psoriasis. Indian journal of psychological
medicine, 37(4),pp. 434.
Lazaridou, E., Tsikrikoni, A., Fotiadou, C., Kyrmanidou,
E., Vakirlis, E., Giannopoulou, C., ... & Ioannides, D.,
2013. Association of chronic plaque psoriasis and
Correlation between Psoriasis Severity and Periodontal Pocket Depth in Psoriasis Vulgaris
81

severe periodontitis: a hospital based casecontrol
study. Journal of the European Academy of
Dermatology and Venereology, 27(8),pp. 967-972.
Page, R. C., & Eke, P. I., 2007. Case definitions for use in
population-based surveillance of periodontitis. Journal
of periodontology, 78(7S), pp. 1387-1399.
Rosania, A. E., Low, K. G., McCormick, C. M., &
Rosania, D. A., 2009. Stress, depression, cortisol, and
periodontal disease. Journal of periodontology, 80(2),
pp. 260-266.
Sharma, A., Raman, A., Pradeep, AR., 2015. Association
of chronic periodontitis and psoriasis: Periodontal
status with severity of psoriasis. Oral diseases, 21(3),
pp. 314-319.
Skudutyte-Rysstad, R., Slevolden, E. M., Hansen, B. F.,
Sandvik, L., & Preus, H. R, 2014. Association
between moderate to severe psoriasis and periodontitis
in a Scandinavian population. BMC Oral
health, 14(1), pp. 139.
Ungprasert, P., Wijarnpreecha, K., Wetter, DA., 2016.
Periodontitis and risk of psoriasis: A systematic
review and meta-analysis Journal of the European
Academy of Dermatology and Venereology, 31(5), pp.
857-862.
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
82
