
Pressure Ulcer Characteristics in Pediatric Patient
Nova Zairina Lubis, Deryne Anggia Paramita, and Khairina
Departement of Dermatology and Venereology, Faculty of Medicine, Universitas Sumatera Utara
Keywords: Pressure ulcer, pediatric, medan
Abstract: Pressure ulcer is a common condition in adult patient. This condition however is not well studied in
pediatric patient. Pressure ulcers commonly formed on tissues located above bony prominences. Continuous
pressure applied on these areas (eg. by mattress surface or medical equipment) may cause tissue damages
that contribute to the ulcers formation. This is a descriptive study using culture test and sensitivity test. This
study was done in the main referral hospital of Sumatera Island, RSUP H. Adam Malik Medan from June to
October 2017. The minimum sample was 20. Steps done in this study include patient sampling, coding, data
analysis and report writing. Subject characteristics discussed in this study include age, gender, ulcer severity
grade, location, onset, and underlying disease. The most common age group found in this study was the 0-3
years old age group at 9 subjects (50%). The most common gender group found in this study was male at 15
subjects (75%). The most common ulcer grade group found in this study was grade 1 ulcer group at 9
subjects (45%). This study also found the occipital region as the most common ulcer region at 6 subjects
(30%). The most common onset found in this study was after 3-5 weeks at 10 subjects (50%). The most
common underlying disease found in this study was hydrocephalus at 5 subjects (25%).
1 INTRODUCTION
Pressure ulcer is a localized injury to the skin and/or
underlying tissue usually over a bony prominence,
as a result of pressure, or pressure in combination
with shear and/or friction (National Pressure Ulcer,
2009).
Pressure ulcer is a common clinical problem
found within hospital inpatients. This problem has
both physical and psychological implications that
may increase morbidity, mortality, and hospital cost
(Schluer, 2016).
Studies on pressure ulcer in pediatric population
has not been done extensively, unlike in adult
population (Baharestami and Ratcliff, 2007).
The
prevalence of pressure ulcer in hospital pediatric
patients ranges from 3% to 35% (Kottner et al.,
2010). From 2011-2016, 53 pediatric pressure ulcer
cases were identified in RSUP Haji Adam Malik
(Rekam Medis, 2017).
Children skins are morphologically and
functionally different to adult skins. Differences in
physiological demands also cause fluid and
electrolyte imbalance to happen more frequently in
pediatric population. Higher body surface area in
children also put them in higher risk for dehydration.
Hypoxia may occur in skin cells with minimal
perfusion. This may cause them to easily break even
under minimal trauma (Rossie, 1996).
Some known risk factors of pressure ulcer in
pediatric population include immobility and
decrease of skin sensitivity (Suddaby et al., 2005).
Communication skills limitations in ill pediatric
population also put them at higher risk to develop
pressure ulcer (Dellinger et al., 2012).
Skin discontinuity such as epidermal peeling or
skin tearing (eg. caused by frictional stress) on
pediatric population especially in critical conditions
may increase risk for developing septicemia and
death (Dellinger et al., 2012).
Secondary infection of pressure ulcer is the most
commonly found complication. Resistant
microorganisms may colonize the pressure ulcer
thus causing local infection and severe bacteremia
may also ensue thereafter (Cataldo et al., 2011).
A
study by Braga et al. found S. aureus (20.7%),
negative Gram bacilli (32.5%) or both (46.8%) as
the three most common etiology of pressure ulcer
secondary infection (Baraga et al., 2013).
Pressure ulcer may cause unpleasant experiences
in pediatric patients and their families, appearance
alterations, treatment time prolongation and
secondary infection. Wound caring may also prove
56
Lubis, N., Paramita, D. and Khairina, .
Pressure Ulcer Characteristics in Pediatric Patient.
DOI: 10.5220/0008150700560059
In Proceedings of the 23rd Regional Conference of Dermatology (RCD 2018), pages 56-59
ISBN: 978-989-758-494-7
Copyright
c
2021 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
to be quite challenging in these patients (Bemabe et
al., 2012).This study aimed to address the lack of
epidemiological studies on pressure ulcer in
pediatric population in Indonesia especially in North
Sumatera. Parameters used in this study include
frequency, microbial pattern, and sensitivity test
result.
2 METHODS
This was a descriptive observational study using
cross sectional method. The study was done from
July to October 2017. The target population was
pressure ulcer inpatients at RSUP H Adam Malik
Medan. The accessible population was pressure
ulcer inpatients at rindu B, NICU and PICU of
RSUP H Adam Malik Medan. Accessible population
that fulfilled the inclusion and exclusion criteria
became the sample group in this study.
Inclusion criteria in this study include <18 years
old pressure ulcer inpatients without topical
antibiotic treatment on the pressure ulcer location.
Patients without consent to this study were excluded.
20 samples were included in this study using
consecutive sampling method. Variables used in this
study include pressure ulcer, microbial profile and
sensitivity test.
3 RESULT
Subject characteristics discussed in this study
include age, gender, ulcer severity grade, location,
onset, and underlying disease
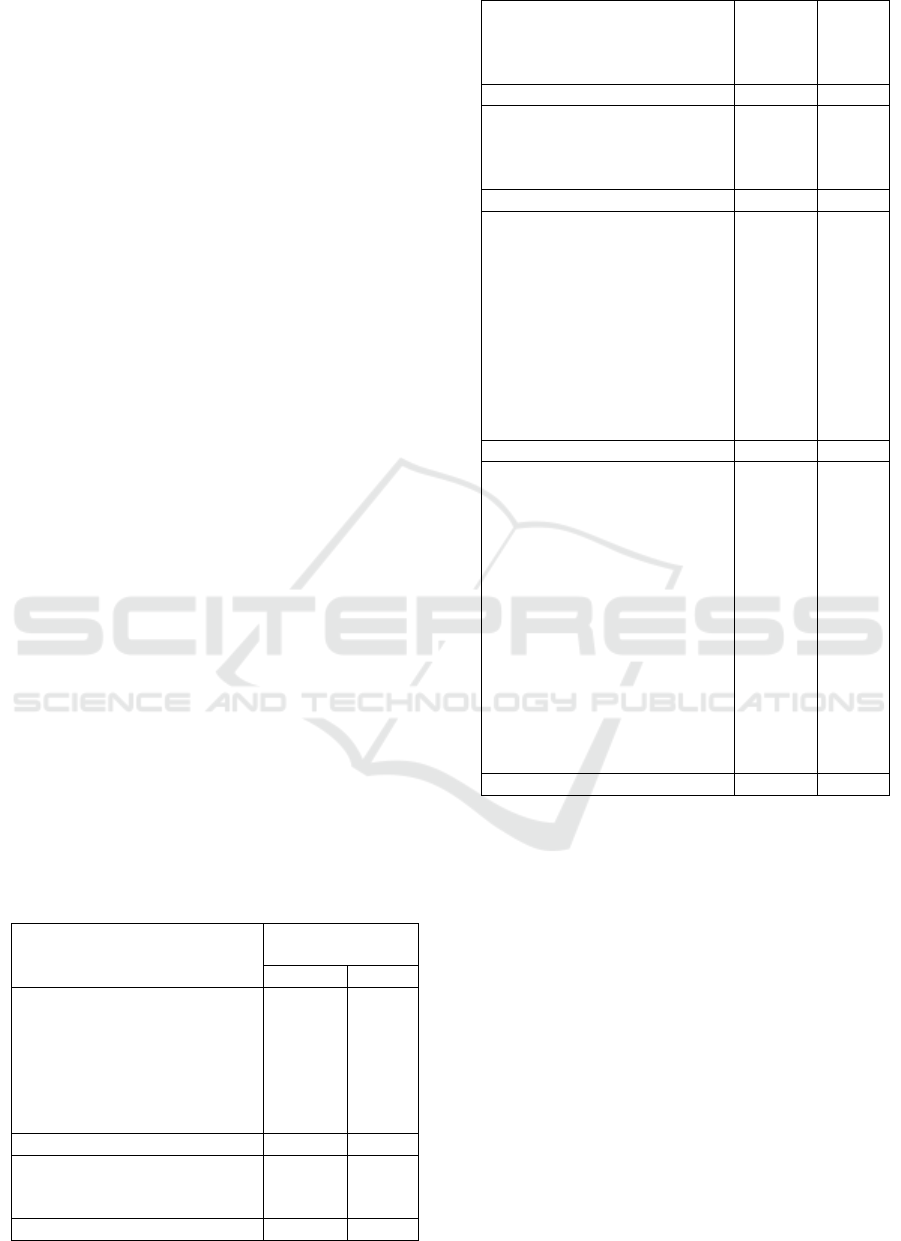
Table 1. Subject distribution accorded to age, gender,
ulcer severity grade, location, onset, and underlying
disease.
Characteristics Decubitus ulcer
patients
n %
Age
0 – 3
>3 – 6
>6 – 9
>9 – 12
>12 – 15
>15 – 18
9
1
0
1
4
5
45
5
0
5
20
25
Total 20 100
Gender
Male
Female
15
5
75
25
Total 20 100
Ulcer Grade
Grade 1
Grade 2
Grade 3
9
6
5
45
30
25
Total 20 100
Onset (weeks)
0 – 2
3 – 5
6 – 8
5
10
5
25
50
25
Total 20 100
Location
Femoral
Iliac
Occipital
Feet
Sacrum
Scrotum
Temporal
Tibial
Knees
Arms
1
1
6
1
5
1
1
1
1
2
5
5
30
5
25
5
5
5
5
10
Total 20 100
Undelying disease
Abscess
Acute lymphoblastic
leukemia
Fracture
Head injury
Hydrocephalus
Burn wounds
Bacterial meningitis
Post appendicitis
Systemic lupus erythematosus
Intracranial space occupying
lesion
Osteomyelitis
Osteosarcoma
1
1
2
4
5
1
1
1
1
1
1
1
5
5
10
20
25
5
5
5
5
5
5
5
Total 20 100
4 DISCUSSION
The most common age group found in this study was
the 0-3 years old age group at 9 subjects (50%). A
study by Schindler et al also found similar result.
They concluded that pressure ulcers can be more
easily formed at an age above 2 years old during
admission to the hospital PICU when compared to
those of older age (Schindler et al., 2011).
A study
by Curly et al also found the mean age of pediatric
pressure ulcer inpatients was at 36 months old
(Curley et al., 2003).
The most common gender group found in this
study was male at 15 subjects (75%) compared to
female at 5 subjects (25%).Several epidemiological
studies done on children pressure ulcer patients also
found similar results. Higher percentage and
Pressure Ulcer Characteristics in Pediatric Patient
57

distribution of adipose tissues in females were
thought to be able to cushion the bony prominence
areas (eg. on sacrum). However, further studies are
needed (Kottner et al., 2010).
The most common ulcer grade group found in
this study was grade 1 ulcer group at 9 subjects
(45%). Similar results were also found on studies
done by Curley et al (2013).
This study also found the occipital region as the
most common ulcer region at 6 subjects (30%).
Pressure ulcers on children usually formed on body
areas that sustain the most pressure. Solis et al found
that within all age groups, occipital region usually
sustain the most pressure followed by sacrum and
scapular region (Solis et al., 1988).
Different patterns
were found in adults where ischial tuberosity,
sacrum, and heels are the most common regions
(Kottner et al., 2010). These differences were
thought to be caused by anatomical developmental
changes. Pressure burdens tend to shift from
occipital to sacrum region as people age (Solis et al.,
1988).
The most common onset found in this study was
after 3-5 weeks at 10 subjects (50%). Similar results
can be found on a study by Manning et al. where
they found 24 days as the mean inpatient treatment
duration of their subjects. They also found that
longer duration of inpatient treatment was associated
with higher risk to develop pressure ulcers (Manning
et al., 2015).
The most common underlying disease found in
this study was hydrocephalus at 5 subjects (25%).
Immobility and sensate loss are some of the main
risk factors for pediatric pressure ulcers (Bernabe,
2012).
Both conditions are known to be common in
patients with hydrocephalus.
5 CONCLUSION
The most common age group found in this study was
the 0-3 years old age group at 9 subjects (50%). The
most common gender group found in this study was
male at 15 subjects (75%). The most common ulcer
grade group found in this study was grade 1 ulcer
group at 9 subjects (45%). This study also found the
occipital region as the most common ulcer region at
6 subjects (30%). The most common onset found in
this study was after 3-5 weeks at 10 subjects (50%).
The most common underlying disease found in this
study was hydrocephalus at 5 subjects (25%).
ACKNOWLEDGMENT
This research was supported by Research
Foundation of Universitas Sumatera Utara Budget
Period of 2017. We thank our colleagues from
Department of Dermatology and Venereology,
Faculty of Medicine, Universitas Sumatera Utara,
Haji Adam Malik General Hospital, and
Microbiology Laboratory who provided insight and
expertise that greatly assisted the research.
REFERENCES
Baharestami, M., Ratliff, C., 2007. Pressure Ulcers in
Neonates and Children: An NPUAP White Paper.
Advance in Skin & Wound Care, 20(4), pp. 208-220.
Bernabe, K., 2012. Pressure Ulcers in The Pediatric
Patient. Current Opinion in Pediatric. 24(3), pp. 352-
356.
Braga I., Pirett C., Ribas R., Gontijo Filho P., Diogo
Filhoa., 2013. Bacterial Colonization of Pressure
Ulcers: Assessment of Risk for Bloodstream
Infection and Impact on Patient Outcomes. The
Journal of Hospital Infection, 83(4), pp. 314-20.
Cataldo, C., Bonura, C., Caputo, G., et al, 2011.
Colonization of Pressure Ulcers By Multidrug-
Resistant Microorganism In Patients Receiving Home
Care. Scandinavian Journal of Infectious Disease,
43(11-12), pp. 947-952.
Curley, MA., Razmus, IS., Roberts, KE., Wypij, D.,
2003. Predicting pressure ulcer risk in pediatric
patients the Braden Q scale. Nursing Research, 52(1),
pp. 22-33.
Dellinger, RP., Levy, MM., Rhodes, A., Annane, D.,
Gerlach, H., Opal, SM., et al., 2012. Surviving Sepsis
Campaign: International Guidelines for Management
of Severe Sepsis and Septic Shock. Intensive Care
Medicine. 39: 165-228.
Kottner, J., Wilborn, D. and Dassen, T., 2010. Frequency
of pressure ulcers in the paediatric population: a
literature review and new empirical
data. International journal of nursing studies, 47(10),
pp.1330-1340.
Manning, M., Gauvreau, K., Curley, M., 2015. Factors
Associated With Occipital Pressure Ulcers in
Hospitalized Infants and Children. American
Association of Critical Care, 24(4), pp. 342-348.
National Pressure Ulcer Advisory Panel and European
Pressure Ulcer, 2009. Prevention and Treatment of
Pressure Ulcers: Clinical Practical Guideline.
National Pressure Advisory Panel, Washington, DC.
Rekam Medis RS Umum Pusat Haji Adam Malik, 2017.
Rossie, E., 1996. Padiatrie 3
rd
edition. Stuttgart, New
York, Thieme.
Schindler, C.A., Mikhailov, T.A., Kuhn, E.M.,
Christopher, J., Conway, P., Ridling, D., Scott, A.M.
and Simpson, V.S., 2011. Protecting fragile skin:
RCD 2018 - The 23rd Regional Conference of Dermatology 2018
58

nursing interventions to decrease development of
pressure ulcers in pediatric intensive care. American
Journal of Critical Care, 20(1), pp.26-35.
Schluer, AB., 2016. Pressure Ulcer in Maturing Skin – A
Clinical Perspective. Journal of Tissue Viability,
26(1), pp. 2-5.
Solis, I., Krouskop, T., Trainer, N. and Marburger, R.,
1988. Supine interface pressure in children. Archives
of physical medicine and rehabilitation, 69(7),
pp.524-526.
Suddaby, E., Barneu, S., Facteau, L., 2005. Skin
Breakdown in Acute Care Pediatrics. Pediatric
Nursing, 31(2): 132-138.
Pressure Ulcer Characteristics in Pediatric Patient
59
